Abstract
Minocycline is a tetracycline derivative antibiotic commonly prescribed for acne, rosacea, and other inflammatory skin disorders. Minocycline turns black when oxidized, leading to discoloration of the skin, nails, bulbar conjunctiva, oral mucosa, teeth, bones, and thyroid gland. Hyperpigmentation has been reported after long-term minocycline therapy with at least 100 mg/day. Three types of minocycline-induced cutaneous hyperpigmentation can result. Type I is the most common, and is associated with blue-black discoloration in areas of previous inflammation and scarring. Type II most commonly affects the legs and is characterized by blue-gray pigmentation of previously normal skin. Type III is the least common and is characterized by diffuse muddy-brown discoloration predominantly on sun exposed skin. Minocycline-induced hyperpigmentation may be cosmetically disfiguring and prompt identification is essential. Without treatment, symptoms may take several months, to years to resolve, after discontinuation of the drug. However, the pigmentation may never completely disappear. In fact, there have been few reports of complete resolution associated with any therapeutic intervention. We report a case of a patient on long-term minocycline therapy utilized as an anti-inflammatory agent to control symptoms of rheumatoid arthritis, which led to minocycline-induced hyperpigmentation of the face. To remove the blue-gray cutaneous deposits, 3 Q-switched lasers (Neodymium: yttrium aluminum garnet (Nd:YAG) 1064 nm, Alexandrite 755 nm, and Ruby 694 nm) were used in test areas. The Alexandrite 755 nm laser proved to provide effective clearing of the minocycline hyperpigmentation requiring just 2 treatments, with minimal treatment discomfort and down time.
Keywords: rheumatoid arthritis, discoloration, antibiotic, inflammatory disease, tetracycline, wavelength
Introduction
Diffuse blue-gray skin discoloration has been reported in several conditions such as Addison’s disease, argyria, hemochromatosis and polycythemia vera.1 Riehl melanosis is characterized by brown-violet pigmentation on sun-exposed areas, erythema, and pruritus.2 Erythema dyschromicum perstans is either idiopathic or acquired, typically occurs in those younger than 40 years, and first presents with erythematous macules that slowly turn slate gray resulting in gray-blue hypermelanosis.2 Finally, end-stage metastatic melanoma can produce a blue-gray to brown hue to the body.2 In addition, drugs including minocycline, amiodarone, zidovudine, and bleomycin have been reported to cause cutaneous darkening (Table 1).
Table 1.
Drugs associated with cutaneous darkening and special attributes
| Drug | Description |
|---|---|
| Minocycline12 | Type I: blue-grey pigmentation of normal skin Type II: blue-black pigmentation of inflamed/scarred skin Type III: muddy brown pigmentation with sun-exposure |
| Amiodarone13 | Slate-colored, blue-gray to purple discoloration of sun-exposed skin |
| Bleomycin14 | Dark brown flagellate (band-like) hyperpigmentation on areas of trauma, especially trunk and proximal extremities |
| Zidovudine15 | Melanonychia and mucosal hyperpigmentation (more common in dark-skinned individuals) |
Minocycline is a semi-synthetic tetracycline antibiotic that turns black when oxidized, and can produce discoloration of the skin, nails, oral mucosa, conjunctiva, teeth, bones, and thyroid gland.3 Three types of minocycline-induced cutaneous hyperpigmentation have been described:3
Type I is the most common, and is associated with blue-black discoloration in areas of previous inflammation and scarring.
Type II most commonly affects the legs and is characterized by blue-gray pigmentation of previously normal skin.
Type III is the least common and is characterized by diffuse muddy-brown discoloration predominantly on sun-exposed skin.
Minocycline-induced hyperpigmentation is associated with long-term use of this drug. Any patient receiving more than 100 grams of minocycline can develop discoloration.4 The pigment deposition is the result of a drug metabolite-protein complex chelated with calcium, or an insoluble minocycline-melanin complex.5 Minocycline hyperpigmentation occurs in 2.4% to 14.8% of patients on chronic treatment, most commonly for acne and rosacea.5 In a study of 700 patients on high-dose long-term minocycline treatment for acne (100 mg daily, 100/200 mg on alternate days, or 200 mg daily for 10.5 months), the only side effect that was significantly greater in patients taking higher doses (cumulative dose greater than 70 g) compared with lower doses was pigmentation (P < 0.01).6 Its anti-inflammatory effects are helpful for rheumatoid arthritis, immunobullous disease and other inflammatory diseases.3 The incidence of minocycline pigmentation is higher in patients treated for autoimmune diseases and may be more common with increasing age.3
Q-switched lasers use high energy, nanosecond pulsing and are available in 3 wavelengths for drug-induced pigmentation, including the Ruby 694 nm, the Alexandrite 755 nm, and the Nd:YAG infrared 1064 nm.7 There have been reports of the Alexandrite laser leading to the resolution of Type II minocycline induced hyperpigmentation.6 Other reports have shown efficacy of the Ruby laser for minocycline facial and leg pigmentation.8,9 A single study compared the YAG and Ruby lasers in the treatment of minocycline pigmentation and the Ruby laser was found to be more effective.9 However, there are no studies comparing the 3 Q-switched lasers for effectiveness and patient comfort in the treatment of minocycline-induced hyperpigmentation.
Case
A 70-year-old caucasian male presented with a one-year history of progressive worsening blue-gray discoloration of the face. There were no associated symptoms and no history of previous gold therapy. Physical examination revealed macular, non-blanching, diffuse blue-gray hyperpigmentation on the forehead, temples, cheeks, nose, and chin sparing the oral mucosa. The patient was taking 100 mg of minocycline orally twice daily for 3 years (total 219 grams) to suppress symptoms of rheumatoid arthritis. The patient noticed increased darkening of the face over the past year. Minocycline was discontinued to prevent further pigmentation. A 0.4 × 0.3 × 0.3 cm punch biopsy demonstrated mild perivascular lymphocytic infiltrates with increased pigment deposition in the basal layers of the epidermis (Figure 1). Iron stain was negative (Figure 2).
Figure 1.
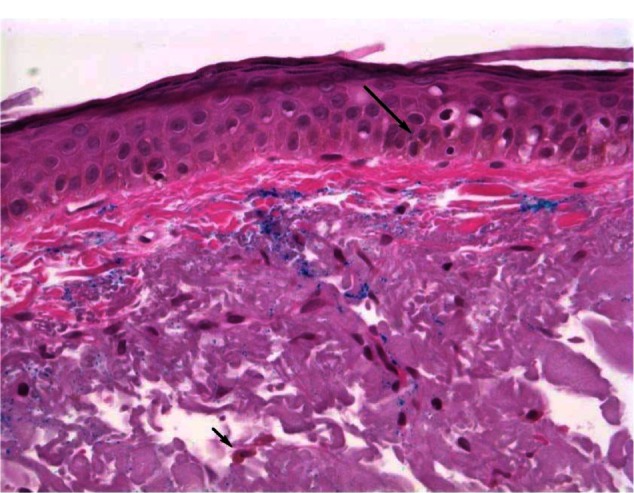
Minocycline-induced hyperpigmentation.
Notes: There is increased faintly visible light brown pigment (melanin) within the basal keratinocytes (long arrow) and dermal dendocytes (short arrow). The blue pigment within the papillary dermis is the ink used for margins.
Figure 2.
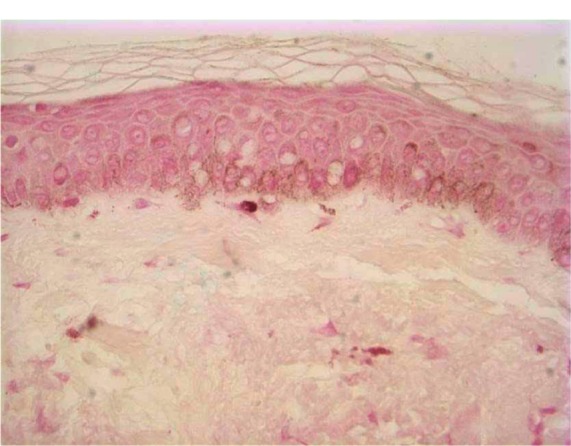
Iron stain.
Notes: This high power view shoes the pigment within the basal keratinocytes and dermal macrophages is negative for iron. the pigment is slightly better visualized here than routine hematoxyline and eosin in Figure 1.
The patient was spot-treated with 3 Q-switched lasers (1064 nm, [Palomar Spectrum RD1200] 755 nm, and 694 nm [both Syneron-Candela Alex Trivantage]) to evaluate which laser would achieve the best results in removing pigmentation with minimal discomfort. No topical anesthetic was used. The 1064 nm laser was set at 1.6 joules (J) with a 5 mm spot size. The 755 nm laser used a fluence of 5.5 J with a 4 mm spot size. The 694 nm was set at 4 J with a 6.5 mm spot size. The results of the trial therapy after 1 week are shown in Figure 3. The 1064 nm revealed minimal to no change in pigment. The 755 nm showed a 50% improvement with minimal discomfort. The 694 nm showed 90% improvement, however was uncomfortable for the patient. We chose the 755 nm laser for treatment based on its significant improvement with minimal pain, discomfort, and downtime for the patient. The patient received two full-face treatments spaced 2 weeks apart with the 755 nm at 5.5 J and 4 mm spot size and one follow-up spot treatment. These treatments led to complete resolution of hyperpigmentation and the patient was completely satisfied with the result (Figure 4). Sun protection was encouraged following treatments.
Figure 3.
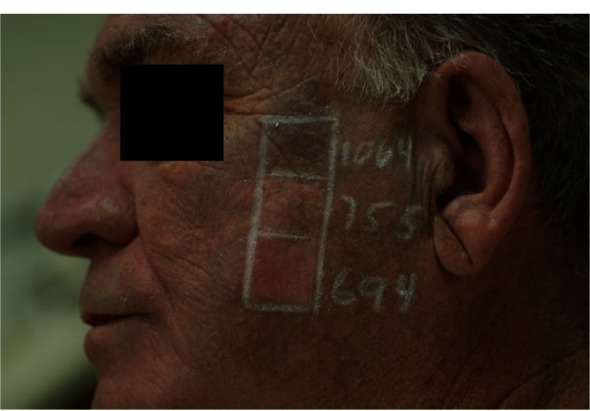
Diffuse blue-black darkening after prolonged minocycline use.
Notes: Spot-treatment trialed with 3 Q-switched lasers (Neodynium: YAG 1064 nm, Alexandrite 755 nm, and Ruby 694 nm).
Figure 4.
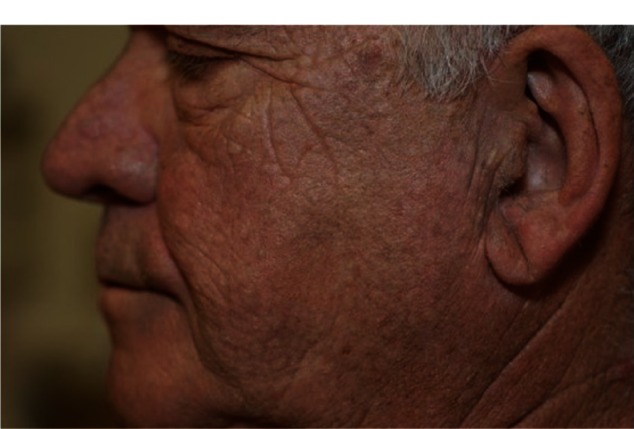
Results after 2 sessions with the Q-switched Alexandrite (755 nm) laser.
Discussion
This patient had Type III minocycline-induced hyperpigmentation on the sun-exposed skin of the face after taking 219 grams of minocycline over 3 years. Of the 3 Q-switched lasers tested, the 755 nm laser was effective in reversing pigmentation with minimal patient discomfort after 2 treatments. Type III minocycline-induced hyperpigmentation is less likely to respond than Types I and II.3 It is not known exactly how laser therapy removes the pigment associated with minocycline use, but is thought to result from fragmentation of the intracellular and extracellular pigmentation and drainage through the lymphatic system.2
The recommended minocycline dose for acne is 100–200 mg daily. Many patients treated for a year or two will reach a cumulative dose of over 100 g. According to the US Food and Drug Administration (FDA), there is a manufacturing delay of tetracycline leading to a shortage of the drug.10 As a result, physicians are forced to use alternative medications such as doxycycline.10 Therefore, we may see a greater incidence of minocycline-induced hyperpigmentation as minocycline prescribing increases. Fortunately, we can utilize the Alexandrite 755 nm laser to remove pigmentation associated with the use of this drug. A recent case reported successful treatment with the Alexandrite laser, with the patient deciding to continue minocycline therapy and returning 3 years later with recurrence to receive another laser treatment.11
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Merchant F, Carpenter T. Blue-gray discoloration of the skin. Am Fam Physician. 2011 Oct 1;84(7):821–8222. [PubMed] [Google Scholar]
- 2.Kalia S, Adams SP. Dermcase. Minocycline-induced pigmentation. Can Family Physician. 2006 May;52:595–596. [PMC free article] [PubMed] [Google Scholar]
- 3.Pecina JL, Pittelkow MR. Hyperpigmentation – a case study. Aust Fam Physician. 2011 Sep;40(9):701–702. [PubMed] [Google Scholar]
- 4.Eisen D, Hakim MD. Minocycline-induced pigmentation: Incidence, prevention, and management. Drug Saf. 1998 Jun;18(6):431–440. doi: 10.2165/00002018-199818060-00004. [DOI] [PubMed] [Google Scholar]
- 5.Mouton RW, Jordaan HF, Schneider JW. A new type of minocycline-induced cutaneous hyperpigmentation. Clin Exp Dermatol. 2004 Jan;29(1):8–14. doi: 10.1111/j.1365-2230.2004.01421.x. [DOI] [PubMed] [Google Scholar]
- 6.Green D, Friedman KJ. Treatment of minocycline-induced cutaneous pigmentation with the Q-switched Alexandrite laser and a review of the literature. J Am Acad Dermatol. 2001 Feb;44(Suppl 2):342–347. doi: 10.1067/mjd.2001.103036. [DOI] [PubMed] [Google Scholar]
- 7.Goulden V, Glass D, Cunliffe WJ. Safety of long-term high-dose minocycline in the treatment of acne. Br J Dermatol. 1996 Apr;134(4):693–695. doi: 10.1111/j.1365-2133.1996.tb06972.x. [DOI] [PubMed] [Google Scholar]
- 8.Knoell KA, Milgraum SS, Kutenplon M. Q-switched ruby laser treatment of minocycline-induced cutaneous hyperpigmentation. Arch Dermatol. 1996 Oct;132(10):1251–1253. [PubMed] [Google Scholar]
- 9.Tsao H, Busam K, Barnhill RL, Dover JS. Treatment of minocycline-induced hyperpigmentation with the Q-switched ruby laser. Arch Dermatol. 1996 Oct;132(10):1250–1251. [PubMed] [Google Scholar]
- 10.Ruth C. Running on empty. FDA, Congress working to mitigate drug shortages. Derm World. 2012 Jul; [Google Scholar]
- 11.Samalonis LB. Q-switched lasers effective for treating drug-induced hyperpigmentation. Dermatology Times. 2012 Mar 1; [Google Scholar]
- 12.Holm AN, Nelson WK. Images in clinical medicine. Minocycline-induced hyperpigmentation. N Engl J Med. 2006 Nov 16;355(20):e23. doi: 10.1056/NEJMicm053666. [DOI] [PubMed] [Google Scholar]
- 13.Wiper A, Roberts DH, Schmitt M. Amiodarone-induced skin pigmentation: Q-switched laser therapy, an effective treatment option. Heart. 2007 Jan;93(1):15. doi: 10.1136/hrt.2006.091462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta LK, Tanwar RK, Khare AK, Jain SK. Bleomycin induced flagellate pigmentation. Indian J Dermatol Venereol Leprol. 2002 May-Jun;68(3):158–159. [PubMed] [Google Scholar]
- 15.Greenberg RG, Berger TG. Nail and mucocutaneous hyperpigmentation with azidothymidine therapy. J Am Acad Dermatol. 1990 Feb;22(2 Pt 2):327–330. doi: 10.1016/0190-9622(90)70039-k. [DOI] [PubMed] [Google Scholar]


