Abstract
Context
Disulfiram has emerged as a promising treatment for cocaine dependence, but it has not yet been evaluated in general populations of cocaine users.
Objectives
To compare the effectiveness of disulfiram therapy with that of a placebo condition in reducing cocaine use and to compare the effectiveness of 2 active behavioral therapies—cognitive behavior therapy (CBT) and interpersonal psychotherapy (IPT)—in reducing cocaine use.
Design
Randomized, placebo-controlled, double-masked (for medication condition), factorial (2×2) trial with 4 treatment conditions: disulfiram plus CBT, disulfiram plus IPT, placebo plus CBT, and placebo plus IPT.
Setting
A community-based outpatient substance abuse treatment program.
Patients
A total of 121 individuals meeting the criteria for current cocaine dependence.
Interventions
Patients received either disulfiram (250 mg/d) or placebo in identical capsules. Medication compliance was monitored using a riboflavin marker procedure. Both behavioral therapies (CBT and IPT) were manual guided and were delivered in individual sessions for 12 weeks.
Main Outcome Measures
Random regression analyses of self-reported frequency of cocaine use and results of urine toxicology screens.
Results
Participants assigned to disulfiram reduced their cocaine use significantly more than those assigned to placebo, and those assigned to CBT reduced their cocaine use significantly more than those assigned to IPT (P<.01 for both). Findings were consistent across all study samples (eg, intention to treat, treatment initiators, and treatment completers). Benefits of disulfiram use and CBT were most pronounced for participants who were not alcohol dependent at baseline or who fully abstained from drinking alcohol during treatment. Adverse effects experienced by participants who received disulfiram were mild and were not considerably different from those experienced by participants who received placebo.
Conclusions
Disulfiram and CBT are effective therapies for general populations of cocaine-dependent individuals. Disulfiram seems to exert a direct effect on cocaine use rather than through reducing concurrent alcohol use.
The past 10 years have been marked by important advances in the development of effective treatments for cocaine dependence.1 Disulfiram has recently emerged as one of a few promising pharmacotherapeutic approaches. Given clinical observations of high rates of alcohol dependence among cocaine-dependent outpatients,2–8 the initial rationale for disulfiram therapy was as a strategy to reduce alcohol use among cocaine users.9,10 Reduced alcohol use was hypothesized to concomitantly reduce patients’ exposure to alcohol, which can be a potent cue for cocaine use; lessen alcohol-related impairments in judgment and in the ability to resist cravings and offers of drugs11; and reduce exposure to cocaethylene, a pharmacologically active metabolite of cocaine and alcohol when they are used concurrently.5,12
An initial randomized trial13 of disulfiram therapy in individuals who were cocaine and alcohol dependent supported the effectiveness of disulfiram therapy for cocaine dependence. However, that study was not masked because it used a no-medication comparison to control for patients’ expectations of the ethanol-disulfiram reaction.14 Two subsequent randomized trials15,16 of cocaine-dependent individuals undergoing agonist therapies (either methadone hydrochloride or buprenorphine hydrochloride) suggested that disulfiram may be an effective treatment for cocaine dependence regardless of whether patients are concurrently alcohol dependent. These findings suggest that disulfiram may have some direct effects on cocaine dependence, which seems to be consistent with new evidence from laboratory studies17–19 suggesting that disulfiram may affect subjective and physiologic responses to cocaine.
The present study was conducted to address several gaps in knowledge regarding the effects of disulfiram therapy on cocaine use by being the first to (1) evaluate a large general outpatient sample, (2) include a placebo condition to control for medication expectancies, (3) include alcohol-dependent and non–alcohol-dependent cocaine abusers to evaluate possible effects of alcohol on the effects of disulfiram, and (4) to combine disulfiram therapy with either a highly structured coping skills treatment or a less structured behavioral approach to evaluate the impact of concomitant behavioral treatments with very different rationales.
Regarding behavioral therapies, cognitive behavior therapy (CBT) has been demonstrated to be effective in cocaine-dependent samples.13,20 There is also some evidence21–27 suggesting that CBT may be more effective when combined with medication and that it often has a delayed main effect that grows stronger at posttreatment follow-up of up to a year. However, studies evaluating the effectiveness of CBT have often compared it with non-specific control conditions. The present study was also designed to build on previous literature by comparing CBT with another active behavioral approach, interpersonal psychotherapy (IPT). Moreover, the initial study13 evaluating disulfiram therapy in cocaine- and alcohol-dependent individuals provided some evidence to suggest that disulfiram was more effective when delivered in conjunction with behavioral therapies that focused on facilitating abstinence (eg, CBT or 12-step facilitation) compared with a supportive clinical management control condition. Thus, the present study was also designed to extend those findings by comparing CBT with a less structured behavioral therapy (IPT).
In this article, we present findings from a 2×2 factorial trial evaluating 2 medication conditions (disulfiram and placebo) and 2 types of behavioral therapy (CBT and IPT) in a general outpatient sample of cocaine-dependent individuals. We hypothesized that (1) disulfiram therapy is more effective than placebo use in reducing cocaine use, regardless of whether patients also use alcohol, and (2) CBT is more effective than IPT in reducing cocaine use. Secondary, exploratory hypotheses included the following: (1) disulfiram therapy is effective without reference to alcohol intake among cocaine abusers who do not drink alcohol, (2) disulfiram therapy is effective through reduction of alcohol use among cocaine abusers who are concurrently alcohol dependent, (3) medication compliance improves the efficacy of disulfiram therapy, and (4) disulfiram therapy is more effective when combined with CBT than with IPT.
METHODS
PARTICIPANTS
Participants were recruited from individuals seeking treatment at the Central Treatment Unit of the APT Foundation, a nonprofit outpatient substance abuse treatment center in New Haven, or from respondents to newspaper advertisements. Individuals who met DSM-IV criteria for current cocaine dependence were included. Individuals were excluded if they (1) were currently physically dependent on opiates or barbiturates or if their principal drug of dependence was not cocaine, (2) met lifetime DSM-IV criteria for a psychotic or bipolar disorder or expressed strong current suicidal or homicidal ideation, (3) had a current medical condition that would contraindicate disulfiram treatment (eg, hepatic or cardiac problems, hypertension, or pregnancy), or (4) had been treated for substance use during the previous 2 months. Individuals who were physically dependent on alcohol were eligible for the protocol after they completed alcohol detoxification.
Participants were administered the Structured Clinical Interview for DSM-IV28 and underwent a physical examination, including electrocardiography, urinalysis, and laboratory blood work. A total of 121 of the 154 individuals screened were determined to be eligible for the study, provided informed consent, and were randomized. Primary reasons for ineligibility were (1) failure to complete the pretreatment evaluation (n=14), (2) liver or heart conditions that contraindicated disulfiram treatment (n=8), (3) unwillingness to take disulfiram (n=4), (4) severe polysubstance dependence that required inpatient treatment (n=2), (5) work conflicts (n=2), (6) failure to meet current cocaine dependence criteria (n=1), (7) concurrent opioid dependence (n = 1), and (8) pregnancy (n = 1). Urn randomization29 was used to balance treatment groups with respect to baseline severity of cocaine dependence, sex, and race.
TREATMENTS
Each of the study psychotherapies was manual guided and was delivered to participants in weekly individual sessions offered over 12 weeks. Participants also met weekly with an independent clinical evaluator who collected urine and breath specimens, assessed recent cocaine use, and monitored other clinical symptoms. Methods previously demonstrated to be comparable in effectiveness to standard medication masking procedures30 were used to maintain single masking for the psychotherapy condition.
Disulfiram and Placebo
Participants assigned to disulfiram treatment were prescribed 250 mg of the drug daily; participants assigned to the placebo group received identical capsules. Participants were cautioned not to drink alcohol, and breathalyzer samples were collected at each contact and before dispensing of medication each week (results of all breathalyzer samples collected were negative). Adverse events were monitored weekly. Medication compliance was monitored via a riboflavin marker procedure31 and was assessed by a commercial laboratory that evaluated whether each urine specimen collected was positive for the riboflavin marker.
Cognitive Behavior Therapy
Cognitive behavior therapy was based on the relapse prevention model of Marlatt and Gordon32 and adapted for use with cocaine users. The goal of this treatment was abstinence from cocaine and other substances through functional analysis of high-risk situations for substance use and the development of effective coping strategies through skills training. As described in the manual,33 skill training addressed (1) understanding patterns of drug use through functional analyses, (2) identifying and coping with cravings, (3) managing thoughts about drugs and alcohol, (4) developing effective drug-refusal skills, (5)developing problem-solving skills, (6) developing emergency coping plans, (7) improving decision-making skills, and (8) using strategies to reduce the risk of human immunodeficiency virus.
Interpersonal Psychotherapy
Interpersonal psychotherapy34 adapted for use with cocaine abusers35 has 4 basic characteristics: (1) adherence to a medical model of psychiatric disorders, (2) a focus on patient difficulties in current interpersonal functioning, (3) brevity and consistency of focus, and (4) use of an exploratory stance by the therapist that is similar to that of supportive and expressive therapies. The goals of IPT include the cessation of cocaine use and the development of more productive strategies for dealing with social and interpersonal problems associated with the onset and perpetuation of cocaine dependence.
Therapists
The 16 doctoral-level therapists (7 in IPT and 9 in CBT) who delivered the study treatments were experienced in and committed to the type of treatment they delivered in the trial and in treating substance users. Therapists had a mean (SD) of 9.6 (8.4) years of postdoctoral experience and received training that included (1) a didactic seminar and (2) completion of at least 1 closely supervised training case. To promote adherence to manual guidelines, therapists in each condition met regularly with supervisors to discuss case materials and review session videotapes.
ASSESSMENT
Participants were assessed before treatment, weekly during treatment, and at the 12-week treatment termination point by an independent clinical evaluator who was masked to treatment condition. Primary outcome measures were frequency of cocaine use (operationalized for the random regression analyses as the number of days per week the participant reported using cocaine) and results of urine toxicology screens (operationalized as the likelihood of submitting a cocaine-positive urine sample each week). The Substance Abuse Calendar, similar to the Timeline Followback method,36,37 was administered weekly during treatment to collect detailed day-by-day self-reports of cocaine use, alcohol use, other drug use, and medication compliance throughout the 84-day treatment and for the 28 days before randomization.
Participant self-reports of cocaine use were verified through urine toxicology screens obtained at every visit. Of 851 urine specimens collected during the treatment phase, 713 (84%) were consistent with self-report, 27 (3%) were negative for cocaine although the participant reported recent cocaine use, and 111 (13%) were positive for cocaine in cases in which the participant had denied use. This rate compares favorably with previous studies37–39 of cocaine-dependent samples, which have supported the accuracy of self-report data using the methods described herein.
DATA ANALYSES
The principal analytic strategy was the use of random regression models40 for the 2 primary outcome variables, with time as a log-transformed variable to represent the greater slope anticipated in the early weeks of treatment. Baseline frequency of cocaine use (operationalized as the number of days of cocaine use in the 28 days before randomization) was used as a covariate for these analyses. In addition to the principal analysis conducted on the 121 participants randomized to treatment (intention-to-treat sample), supplemental analyses also evaluated treatment effects for the 112 participants who initiated treatment, the 87 who completed 3 or more weeks of treatment, and the 53 who completed all treatment sessions. Results were highly consistent across analysis samples; therefore, results from only the intention-to-treat sample are presented (a full report of all analyses is available from Dr Carroll).
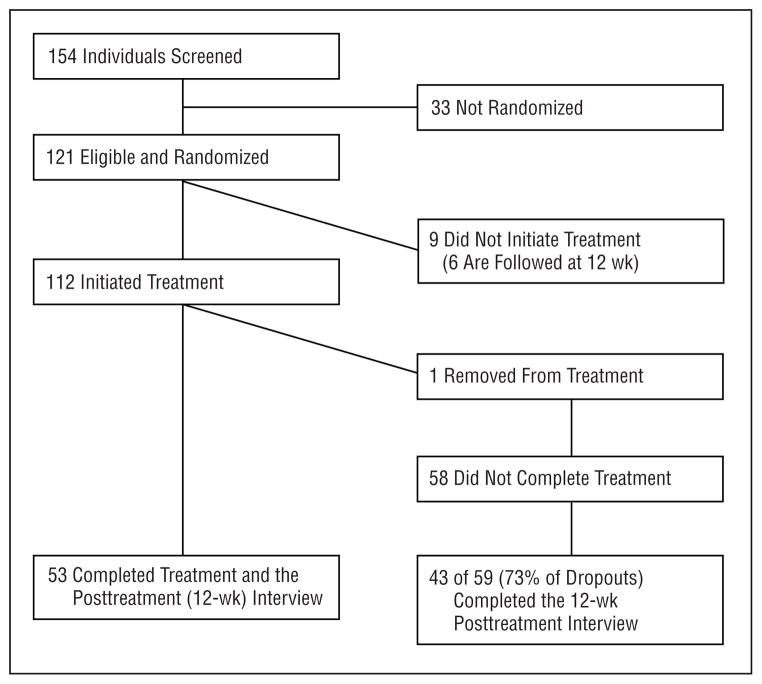
Randomized participants who did not initiate treatment or who dropped out of treatment were followed and interviewed at the 12-week termination point. Of these 68 participants, 49 (72%) were successfully tracked and interviewed. Thus, complete self-report outcome data were available for 84% of the randomized sample (Figure 1).
Figure 1.
Diagram of participant recruitment, retention, and follow-up.
RESULTS
SAMPLE DESCRIPTION
Of the 121 participants randomized to treatment, 26% were female, 63% were white, 31% were African American, and 6% were Hispanic (Table 1). Seventy-seven percent of the participants were single or divorced, and 55% were working full- or part-time. The mean age of the participants was 34.6 years. Mean monthly cocaine use at baseline was 16.6 g, and participants reported using cocaine a mean of 13.0 days in the previous 28 days. Participants reported drinking alcohol a mean of 9.4 days in the previous 28 days. Fifty-four percent of the participants met DSM-IV criteria for a lifetime diagnosis of alcohol dependence, and 26% met the criteria for a lifetime diagnosis of alcohol abuse. Fifty-two percent of the patients met DSM-IV criteria for current alcohol abuse or dependence. Analyses of variance and χ2 tests revealed a statistically significant difference between medication groups on rates of current alcohol abuse or dependence at baseline (disulfiram vs placebo, 63% vs 41%; ; P =.01) but no other statistically significant differences by treatment group for any other baseline variables.
Table 1.
Baseline Demographic, Substance Use, and Psychiatric Characteristics by Treatment Group
| Variable | Treatment Condition
|
Total (N = 121) | F or χ2 | df | P Value | |||
|---|---|---|---|---|---|---|---|---|
| CBT + Disulfiram (n = 30) | IPT + Disulfiram (n = 30) | CBT + Placebo (n = 30) | IPT + Placebo (n = 31) | |||||
| Demographic characteristics | ||||||||
| Age, mean (SD), y | 36.0 (8.3) | 34.1 (7.9) | 34.1 (5.9) | 34.1 (5.8) | 34.6 (7.0) | 0.53 | 3,117 | .66 |
| Female, No. (%) | 8 (27) | 7 (23) | 8 (27) | 9 (29) | 32 (26) | 0.26 | 3,117 | .97 |
| Race, No. (%) | ||||||||
| African American | 8 (27) | 7 (23) | 10 (33) | 13 (42) | 38 (31) | |||
| Hispanic | 0 | 2 (7) | 5 (17) | 0 | 7 (6) | |||
| White | 22 (73) | 21 (70) | 15 (50) | 18 (58) | 76 (63) | |||
| Single or divorced, No. (%) | 21 (70) | 22 (73) | 24 (80) | 26 (84) | 93 (77) | 2.03 | 3 | .57 |
| Unemployed, No. (%) | 11 (37) | 15 (50) | 14 (47) | 14 (45) | 54 (45) | 1.17 | 3 | .76 |
| Admission prompted by criminal judgment, No. (%) | 3 (10) | 4 (13) | 7 (23) | 4 (13) | 18 (15) | 2.35 | 3 | .50 |
| On probation/parole, No. (%) | 4 (13) | 5 (17) | 12 (40) | 6 (19) | 27 (22) | 7.41 | 3 | .06 |
| Education, No. (%) | ||||||||
| Less than high school | 4 (13) | 4 (13) | 10 (33) | 7 (23) | 25 (21) | 5.40 | 6 | .49 |
| High school graduate | 12 (40) | 11 (36.7) | 8 (26.7) | 9 (29) | 40 (33) | |||
| Some education after high school | 14 (47) | 15 (50) | 12 (40) | 15 (48) | 56 (46) | |||
| Current drug use | ||||||||
| Days of cocaine use in previous 28 d | 14.7 (8.4) | 9.5 (6.9) | 14.0 (9.4) | 13.5 (9.1) | 13.0 (8.7) | 2.30 | 3,117 | .08 |
| Days of alcohol use in previous 28 d | 11.0 (10.1) | 9.7 (8.5) | 6.9 (8.8) | 10.0 (10.3) | 9.4 (9.5) | 1.03 | 3,117 | .38 |
| Days of opioid use in previous 28 d | 0 (0) | 0 (0) | 0.7 (3.6) | 0.10 (.6) | 0.19 (1.8) | 0.90 | 3,117 | .44 |
| Days of marijuana use in previous 28 d | 3.3 (7.7) | 2.1 (6.1) | 2.3 (5.4) | 5.3 (8.5) | 3.3 (7.0) | 1.32 | 3,117 | .27 |
| Regular cocaine use, y | 11.3 (8.5) | 9.8 (5.4) | 12.02 (7.49) | 9.1 (7.1) | 10.6 (7.2) | 1.03 | 3,117 | .39 |
| Regular alcohol use, y | 14.9 (10.3) | 14.6 (7.5) | 13.0 (6.9) | 13.0 (8.4) | 13.8 (8.3) | 0.45 | 3,117 | .72 |
| Freebase users, No. (%) | 24 (80) | 20 (67) | 24 (80) | 22 (71) | 90 (74) | 6.49 | 9 | .69 |
| Any previous drug treatment, No. (%) | 14 (47) | 15 (50) | 18 (60) | 19 (61) | 66 (54) | 1.93 | 3 | .59 |
| Lifetime psychiatric diagnoses, No. (%) meeting lifetime DSM-IV criteria | ||||||||
| Cocaine dependence | 30 (100) | 30 (100) | 30 (100) | 31 (100) | 121 (100) | |||
| Alcohol abuse or dependence | 27 (90) | 27 (90) | 19 (63) | 23 (74) | 96 (79) | 9.35 | 3 | .03 |
| Any affective disorder | 12 (40) | 9 (30) | 11 (37) | 12 (39) | 44 (36) | 0.77 | 3 | .86 |
| Any anxiety disorder | 6 (20) | 4 (13) | 8 (27) | 5 (16) | 23 (19) | 1.96 | 3 | .58 |
| Antisocial personality disorder | 12 (40) | 16 (55) | 13 (50) | 7 (25) | 48 (41) | 7.61 | 3 | .06 |
| Other Axis II disorder | 17 (57) | 14 (47) | 14 (47) | 18 (58) | 63 (52) | 0.67 | 3 | .88 |
| Current psychiatric diagnoses, No. (%) meeting current DSM-IV criteria | ||||||||
| Cocaine dependence | 30 (100) | 30 (100) | 30 (100) | 31 (100) | 121 (100) | |||
| Alcohol abuse or dependence | 19 (63) | 19 (63) | 9 (30) | 16 (52) | 63 (52) | 8.91 | 3 | .03 |
| Any affective disorder | 6 (20) | 8 (27) | 7 (23) | 9 (29) | 30 (25) | 0.76 | 3 | .86 |
| Any anxiety disorder | 4 (13) | 3 (10) | 6 (20) | 1 (3) | 14 (12) | 4.36 | 3 | .23 |
Abbreviations: CBT, cognitive-behavioral therapy; IPT, interpersonal psychotherapy.
TREATMENT IMPLEMENTATION
Participants reported taking their medication on 76% of treatment days, and 72% of all urine specimens were positive for the urine riboflavin marker. Of 825 urine specimens collected during treatment that were matched to a participant self-report of medication compliance, 94% were consistent with the participant’s self-report. Medication compliance was not significantly different across psychotherapy conditions (CBT mean [SD], 0.76 [0.26]; IPT mean [SD], 0.70 [0.32]; F1,99=1.1; P =.30) or across medication conditions (disulfiram mean [SD], 0.72 [0.28]; placebo mean [SD], 0.73 [0.30]; F1,99=0.04; P =.85).
All psychotherapy sessions were videotaped for supervision and assessment of fidelity to manual guidelines. To evaluate the discriminability of the 2 types of behavioral therapy, 508 session videotapes (randomly selected early, middle, and late sessions for all participants who completed ≥1 session) were rated by evaluators who were masked to the patient’s treatment condition. The Yale Adherence/Competence Scale, which has been demonstrated to have excellent reliability and concurrent and factorial validity in several previous studies,41,42 was used for the process ratings. Estimates of interrater reliability were made based on a sample of 20 videotapes rated by all 11 raters. The model of Shrout and Fleiss43 for random effects indicated a mean intraclass correlation coefficient estimate of 0.96, suggesting that the ratings were highly reliable. Random regression analyses suggested that study treatments were highly discriminable in that (1) CBT therapists used significantly more CBT interventions than IPT therapists (z=12.4; P<.001) and (2) IPT therapists used significantly more IPT interventions than CBT therapists (z=10.1; P<.01).
Moreover, to evaluate the potential effect of therapist effects on findings reported in the following subsections, we conducted a 1-way analysis of variance on continuous measures of outcome, including treatment retention, self-reported cocaine use, urine test results, and medication compliance. No significant effects for therapist were found for any of these variables, even using liberal P values (P<.25).44
RETENTION BY TREATMENT CONDITION
Of the 121 participants randomized, 112 (93%) initiated treatment. The mean (SD) number of sessions completed was 8.0 (5.1). One participant was withdrawn from the trial because of continued high levels of substance use that required inpatient treatment. Fifty-three participants remained in treatment for the full 12 weeks. Participants who remained in treatment for the full 12 weeks did not differ from those who did not initiate treatment or who dropped out in terms of sex, race, route of administration, and the presence of lifetime affective disorder or antisocial personality disorder. However, participants who were employed at baseline were more likely to complete treatment (54% vs 31%; ; P =.04), and those diagnosed as having a lifetime anxiety disorder were more likely to drop out of treatment (27% vs 9%; ; P =.01). There were no significant effects of psychotherapy ( ; P =.79) or medication condition ( ; P =.32) on treatment completion.
OVERALL EFFECTS OF STUDY TREATMENTS ON COCAINE USE
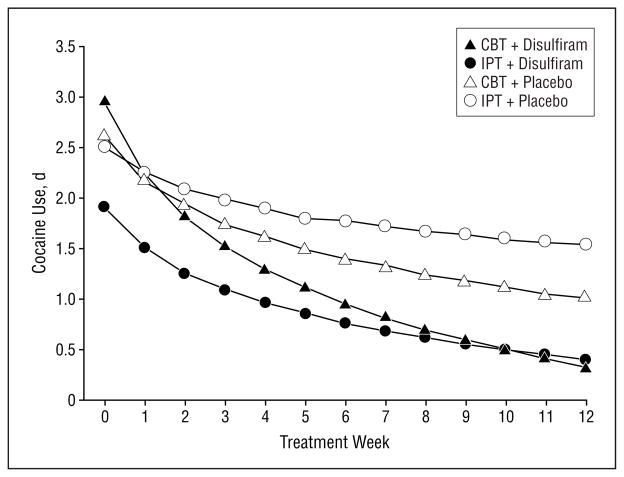
Random-effects regression models evaluating the effects of the study treatments on the frequency of self-reported cocaine use are presented in Table 2 and Figure 2. The overall effect for time was significant, indicating a general reduction in the frequency of cocaine use over time for the participants as a group (z=−7.48; P<.01). Participants assigned to disulfiram treatment reduced their cocaine use significantly more than those assigned to the placebo condition (medication×time, z=−2.82; P<.01). Participants assigned to CBT reduced their frequency of cocaine use significantly more than those assigned to IPT (psychotherapy×time, z=−3.06; P<.01). The interaction of medication and psychotherapy was not statistically significant (medication×psychotherapy×time, z=−1.12; P=.26). When postattrition data from individuals who dropped out of treatment were included in the analyses, all effects were consistent with the analyses limited to data collected before dropout (Table 2).
Table 2.
Effects of Study Treatments on Cocaine Use*
| Self-report Data
|
Urine Data
|
|||
|---|---|---|---|---|
| z | P Value | z | P Value | |
| All Participants Randomized (N = 121, Observations = 917 760) | ||||
| Intercept | 3.43 | <.001 | −1.50 | .13 |
| Med | 0.19 | .85 | 0.71 | .48 |
| Psych | 0.95 | .34 | 0.44 | .66 |
| Med × psych | 0.80 | .42 | 1.57 | .12 |
| Slope | −7.48 | <.001 | −3.74 | <.001 |
| Med × time | −2.82 | <.001 | −2.06 | .04 |
| Psych × time | −3.06 | <.001 | −1.78 | .07 |
| Med × psych × time | −1.12 | .26 | −0.96 | .34 |
| Covariate | 8.65 | <.001 | 3.81 | <.001 |
|
| ||||
| All Participants Randomized, Including Postattrition Data for All Dropouts (n = 121, Observations = 1325) | ||||
| Intercept | 2.96 | <.001 | NA | NA |
| Med | −0.11 | .91 | NA | NA |
| Psych | 0.55 | .58 | NA | NA |
| Med × psych | 0.61 | .54 | NA | NA |
| Slope | −7.81 | <.001 | NA | NA |
| Med × time | −2.61 | .01 | NA | NA |
| Psych × time | −2.57 | .01 | NA | NA |
| Med × psych × time | −1.39 | .16 | NA | NA |
| Covariate | 7.20 | <.001 | NA | NA |
|
| ||||
| All Randomized Participants Who Began Treatment (n = 112, Observations = 908 753) | ||||
| Intercept | 3.34 | <.001 | −1.86 | .06 |
| Med | −0.06 | .95 | 0.75 | .45 |
| Psych | 1.30 | .19 | 0.45 | .65 |
| Med × psych | 0.89 | .37 | 1.30 | .19 |
| Slope | −7.25 | <.001 | −3.48 | <.001 |
| Med × time | −2.65 | .01 | −2.03 | .04 |
| Psych × time | −3.23 | <.001 | −1.79 | .07 |
| Med × psych × time | −1.14 | .25 | −0.76 | .45 |
| Covariate | 8.24 | <.001 | 3.95 | <.001 |
Abbreviation: NA, not applicable.
Definitions: Med, main effect for medication condition (disulfiram vs placebo); Psych, main effect for psychotherapy condition (cognitive-behavioral therapy vs interpersonal psychotherapy); Med × psych, main effect of interaction; Slope, main effect for time; Med × time, effect of study medication across time (negative z value indicates greater slope for disulfiram); Psych × time, effect of psychotherapy condition across time (negative z value indicates greater slope for cognitive-behavioral therapy); Covariate, effect for baseline severity of cocaine use.
Frequency of cocaine use by week (self-reported) and likelihood of submitting a cocaine-positive urine sample by week; results of random-effects regression, with baseline severity of cocaine use as a covariate (days of cocaine use in the previous 28 days).
Figure 2.
Frequency of cocaine use by treatment week. Effects are estimates from random regression analyses. CBT indicates cognitive behavior therapy; IPT, interpersonal psychotherapy.
Results of urine toxicology screens were consistent with the findings based on self-report data. For the full randomized sample, there was a significant decrease in the frequency of cocaine-positive urine specimens submitted over time (z=−3.74; P<.01). There was a significant medication×time effect (z=−2.06; P=.04), suggesting a greater reduction in the likelihood of submitting a cocaine-positive urine specimen for participants assigned to disulfiram treatment vs placebo use. The psychotherapy condition×time effect failed to reach statistical significance for the urine results (z=−1.78; P=.07), but it was in the same direction as the self-report data. Again, there was no evidence of a statistically significant psychotherapy×medication interaction (z=−0.96; P=.34).
EFFECTS OF STUDY TREATMENTS IN ALCOHOL-DEPENDENT VS NONALCOHOLIC SUBGROUPS
As noted previously herein, approximately half of the sample met the criteria for current alcohol abuse or dependence at baseline. To evaluate the significance of current alcohol dependence with respect to treatment response, we conducted supplemental analyses using the same model as described previously herein to evaluate outcomes for (1) participants who met the current criteria for alcohol abuse or dependence (n=63) and (2) participants who did not have a current alcohol diagnosis at baseline (n=58). For the subgroup that met the criteria for alcohol abuse or dependence at baseline, the overall effect of time on cocaine use was statistically significant (z=−8.74; P<.001), as was the psychotherapy×time effect (z=−2.60; P=.01); however, the medication×time effect was not significant (z=−1.29; P<.20) (Table 3).
Table 3.
Effects of Study Treatments on Frequency of Cocaine Use During Treatment by the Presence of Current DSM-IV Alcohol Abuse or Dependence at Baseline: Results of Random Regression Analyses
| Cocaine Use
|
||
| z | P Value | |
| Participants Who Met the Criteria for Alcohol Abuse or Dependence at Baseline (n = 63) | ||
| Intercept | 4.30 | <.001 |
| Med | 0.11 | .91 |
| Psych | 0.67 | .50 |
| Med × psych | 1.14 | .26 |
| Slope | −8.74 | <.001 |
| Med × time | −1.29 | .20 |
| Psych × time | −2.60 | .01 |
| Med × psych × time | 0.70 | .48 |
| Covariate | 6.04 | <.001 |
|
| ||
| Participants Who Did Not Meet the Criteria for Alcohol Abuse or Dependence at Baseline (n = 58) | ||
| Intercept | 4.11 | <.001 |
| Med | 0.50 | .62 |
| Psych | 0.49 | .63 |
| Med × psych | 0.18 | .85 |
| Slope | −7.15 | <.001 |
| Med × time | −2.10 | .04 |
| Psych × time | −2.33 | .03 |
| Med × psych × time | −1.97 | .05 |
| Covariate | 6.29 | <.001 |
Definitions: See Table 2.
For the subgroup that did not meet the criteria for alcohol dependence (n=58), there was a significant overall effect of time on frequency of cocaine use (z=−7.15; P<.001), a significant medication×time effect (z=−2.10; P = .04), a significant psychotherapy × time effect (z=−2.33; P=.03), and a significant 3-way interaction (z=−1.97; P=.05). The latter suggested that the placebo plus IPT condition was significantly less effective than each of the other 3 treatment conditions.
Similarly, whether a participant used any alcohol at all during treatment was strongly associated with the effectiveness of disulfiram treatment in reducing cocaine use. That is, for the 66 individuals who did not drink alcohol on any treatment days, the medication×time effect was significant (z=−4.2; P=.01), as was the psychotherapy×time effect (z=−4.4; P=.01) for frequency of cocaine use. However, for the 35 participants who reported drinking alcohol on 1 or more days during treatment, the medication×time and psychotherapy×time effects were not statistically significant, and neither were the overall effects of time. This suggests that the benefits of CBT and disulfiram use in reducing cocaine use were most pronounced in participants who abstained from alcohol during treatment. Although individuals who abstained from alcohol during treatment reported using alcohol on significantly fewer days in the 28 days before treatment initiation than those who used alcohol during treatment (6.1 vs 15.4 days; F1,103=30.6; P<.001), those who were abstinent during treatment were not significantly different from participants who used alcohol during treatment in terms of whether they met the criteria for current alcohol abuse or dependence at baseline (53% vs 47%; χ2=1.1; P=.29).
Additional exploratory analyses of variance evaluating compliance by treatment condition and whether the participant reported any alcohol use during the trial suggested that individuals who were assigned to disulfiram treatment and who used alcohol had lower rates of medication compliance (61% of urine specimens positive for riboflavin) than those assigned to the placebo condition who did not drink alcohol (71%), those assigned to placebo use who did drink alcohol (76%), and those assigned to disulfiram treatment who did not drink any alcohol during the trial (79%) (medication condition×alcohol use effect, F1,95=3.6; P =.06).
MEDICATION COMPLIANCE AND OUTCOME
To evaluate the impact of medication compliance on cocaine use during treatment, compliance with medication was added as a time-varying covariate to the random regression model described previously herein. The covariate was significant, suggesting that medication compliance was a significant predictor of greater reductions in cocaine use over time (z=−12.6; P=.001). Nevertheless, the medication ×time (z = −2.4; P = .02) and psychotherapy ×time (z = −3.6; P = .01) effects remained statistically significant when controlling for medication compliance.
EFFECTS OF TREATMENT ON ALCOHOL USE
As noted previously herein, all participants were cautioned not to drink alcohol during the study because of the possibility of the ethanol-disulfiram reaction, and 66 participants reported no alcohol use during the trial. For participants who reported drinking alcohol on 1 or more days, mean (SD) alcohol use during the 84-day trial was 4.7 (6.3) days (range, 1–33 days). Random-effects regression models evaluating effects of the study treatments on alcohol use indicated that as a group, participants reported reducing the frequency of their alcohol use over time (z=−0.53; P<.01). For the randomized sample (N=121) and the sample that initiated treatment (n=112), there were no statistically significant effects of medication, psychotherapy, or their interaction on frequency of alcohol use×time. However, for the subgroup that remained in treatment for 3 or more weeks (n=87), there was a statistically significant effect for disulfiram (medication×time, z=−2.68; P=.01). Moreover, when all postattrition data were included in the analyses, there was a significant medication×time effect for the full randomized sample (z=−2.33; P=02).
ADVERSE EFFECTS OF MEDICATION
Adverse effects were mild, and there were no significant differences in rates of adverse effects by medication condition. The most frequently reported adverse effect, headaches, was reported once or more during treatment by 33% of those assigned to placebo use and 34% of those assigned to disulfiram use. Rates of fatigue (28% for placebo vs 34% for disulfiram), nausea (26% vs 26%), and diarrhea (22% vs 21%) also were not significantly different by medication condition. There also were no significant differences in reported adverse effects among the subgroups of participants who drank any alcohol or who used any cocaine during treatment. There were no participant deaths or serious cardiac events during the protocol.
COMMENT
The results of this randomized controlled trial of psychotherapies and pharmacotherapies for cocaine dependence suggest that (1) disulfiram treatment was more effective than the placebo condition in reducing the frequency of cocaine use and the frequency of cocaine-positive urine samples over time and (2) CBT was more effective than IPT in reducing cocaine use during treatment.
This is the first placebo-controlled trial, to our knowledge, to demonstrate that disulfiram therapy is effective in nonalcoholic cocaine-dependent outpatients. Moreover, these findings suggest that disulfiram therapy is especially effective for nonalcoholic cocaine users, as the effects of disulfiram treatment were most pronounced in participants who did not meet the criteria for current alcohol abuse or dependence and in those who abstained from alcohol during the trial. The findings disconfirm our hypothesis that disulfiram treatment is equally effective in alcoholic and nonalcoholic patients but confirm our hypothesis that medication compliance is associated with better outcomes in the disulfiram group. However, the effect of medication compliance on outcome was seen in the placebo group as well, and the effect of disulfiram treatment on reducing cocaine use remained statistically significant even after controlling for medication compliance.
The unexpected findings regarding the effects of disulfiram treatment on the alcoholic subgroup might be explained by the differential compliance in the good vs poorer outcome alcoholic participants. Alcoholic participants who drank while taking disulfiram were somewhat less likely to be compliant and seemed unable to refrain from continued alcohol use. When those patients discovered a disulfiram reaction, they effectively broke the medication masking and either discontinued taking disulfiram entirely or discontinued it when they wanted to drink alcohol or use cocaine. The patients who did not drink alcohol did not break the medication masking and thus may have complied with the medication treatment sufficiently to experience the anticocaine effect.
Paradoxically, this finding confirms (but in an opposite direction) our hypothesis that the effect of disulfiram treatment on alcoholic cocaine abusers is mediated by its impact on alcohol use. Instead of reducing cocaine use through first stopping drinking, the powerful antidipsotropic effect of disulfiram led drinkers to stop taking disulfiram instead. These findings further suggest that disulfiram treatment reduces the attractiveness of cocaine in the same way for alcoholic and non-alcoholic cocaine abusers. This interpretation (ie, that the effect of disulfiram treatment on cocaine use is not mediated by stopping alcohol use) is further supported by the finding that the disulfiram/placebo differences were greater in participants who did not drink alcohol. If disulfiram exerted its effect on cocaine use by reducing the use of alcohol, a smaller difference would be expected between disulfiram and placebo in the subgroup that did not drink alcohol during the trial. Also, disulfiram treatment seemed to be safe in this population, and levels of reported adverse events were mild and comparable to those reported by patients in the placebo condition.
This study also adds to the growing body of work supporting CBT as a treatment for cocaine dependence and extends it in 2 ways, first by comparing it with another active psychotherapy and second by findings that suggest that the effects of CBT, when delivered with placebo, were not statistically significantly different from CBT or IPT delivered in conjunction with disulfiram. The former finding is compelling in that IPT was conceived and implemented as an active control condition and was delivered and supervised by investigators who were adherents of IPT.45,46 That the effectiveness of CBT relative to that of IPT was robust across analysis samples and the alcoholic/nonalcoholic groups is also notable, given findings from the general psychotherapy literature47–49 that comparisons of 2 active behavioral conditions often result in comparable effects. Regarding the former finding (the lack of evidence of a CBT-disulfiram interaction effect), Figure 2 and the analysis of the non–alcohol-dependent subgroup suggested a pattern of findings that was consistent with additive50,51 effects of the study treatments. That is, results suggest poorest outcomes for the group assigned to IPT plus placebo, and offering either CBT or disulfiram was associated with optimal outcomes in this sample; combining the two provided little additional incremental benefit.
Limitations of the present study include that, as in other trials in cocaine-dependent populations, 50% of individuals who began treatment did not complete it (although, on average, patients attended 67% of sessions offered). Although this underlines that available treatments could, and should, be made more attractive to patients, it is also important that attrition was unlikely to undercut the validity of the conclusions that may be drawn from the study because (1) differential attrition by treatment condition was not seen, (2) statistical methods were used that are less sensitive to missing data and allow use of all data collected from all participants, (3) postattrition data were collected from 73% of the dropouts, and (4) analyses that included data collected after dropout were highly consistent with analyses limited to data collected from participants while they were in treatment.52
In summary, this study provides the strongest evidence to date regarding the effectiveness of disulfiram treatment in reducing cocaine use in that it was the first to be placebo controlled and to include a comparatively large outpatient sample of cocaine-dependent individuals. Furthermore, by including alcohol-dependent and non–alcohol-dependent cocaine abusers, the results of this trial strongly suggest that the effect of disulfiram treatment on cocaine use was not related to cessation of concurrent alcohol use because its superiority to the placebo condition was greater in those who did not drink. Disulfiram treatment was efficacious in patients without a current diagnosis of alcohol abuse or dependence or who refrained from drinking alcohol but was not statistically significantly different from placebo among patients who drank alcohol during the trial. Hence, the use of disulfiram in alcoholic cocaine abusers should be combined with efforts to enhance patient commitment to alcohol abstinence. Alcohol use during treatment was strongly related to cocaine use,6 independent of the patient’s medication condition.
Moreover, if research continues to support the efficacy of disulfiram treatment in varied samples of cocaine abusers, it is important to remember that even the most powerful pharmacotherapies for substance use disorders can be rendered ineffective unless delivered with adequate psychosocial treatment (eg, McLellan et al53) and that carefully targeted behavioral therapies can dramatically enhance pharmacotherapy compliance and effectiveness.54,55 Although the effects of disulfiram treatment were comparable when delivered with CBT or IPT, both approaches were active behavioral therapies delivered by experienced clinicians. Disulfiram treatment compliance and hence outcome might be lower when used in combination with less structured behavioral approaches.56
Acknowledgments
This study was supported by grants R01-DA10679, KO5-DA00089 (Dr Rounsaville), K05-DA 00457 (Dr Carroll), and P50-DA09241 from the National Institute on Drug Abuse, Bethesda, Md.
We thank Joanne Corvino, MPH, John Cecero, PhD, Sarah Church, PhD, Celeste Milligan, PhD, Robert Chang, MD, Meghan Biro, Sarah Fitzsimmons, Kia Samuels, Lorraine Myers, Lance Barnes, and the staff of the Central Medical Unit of the APT Foundation.
References
- 1.National Institute on Drug Abuse. Principles of Drug Abuse Treatment: A Research-Based Guide. Bethesda, Md: National Institute on Drug Abuse; 2000. [Google Scholar]
- 2.Carroll KM, Rounsaville BJ, Bryant KJ. Alcoholism in treatment-seeking cocaine abusers: clinical and prognostic significance. J Stud Alcohol. 1993;54:199–208. doi: 10.15288/jsa.1993.54.199. [DOI] [PubMed] [Google Scholar]
- 3.Brady KT, Sonne S, Randall CL, Adinoff B, Malcolm RJ. Features of cocaine dependence with concurrent alcohol dependence. Drug Alcohol Depend. 1995;39:69–71. doi: 10.1016/0376-8716(95)01128-l. [DOI] [PubMed] [Google Scholar]
- 4.Heil SH, Badger GJ, Higgins ST. Alcohol dependence among cocaine dependent outpatients: demographics, drug use, treatment outcome and other characteristics. J Stud Alcohol. 2001;62:14–22. doi: 10.15288/jsa.2001.62.14. [DOI] [PubMed] [Google Scholar]
- 5.McCance-Katz EF, Price LH, Kosten TR, Jatlow PM. Cocaethylene: pharmacology, physiology, and behavioral effects in humans. J Pharmacol Exp Ther. 1995;274:215–223. [PubMed] [Google Scholar]
- 6.McKay JR, Alterman AI, Rutherford MJ, Cacciola JS, McLellan AT. The relationship of alcohol use to cocaine relapse in cocaine dependent patients in an after-care study. J Stud Alcohol. 1999;60:176–180. doi: 10.15288/jsa.1999.60.176. [DOI] [PubMed] [Google Scholar]
- 7.Schmitz JM, Bordnick PS, Kearney ML, Fuller SM, Breckenridge JK. Treatment outcome of cocaine-alcohol dependent patients. Drug Alcohol Depend. 1997;47:55–61. doi: 10.1016/s0376-8716(97)00069-0. [DOI] [PubMed] [Google Scholar]
- 8.Grant BF, Harford TC. Concurrent and simultaneous use of alcohol and cocaine: results of a national survey. Drug Alcohol Depend. 1990;25:97–104. doi: 10.1016/0376-8716(90)90147-7. [DOI] [PubMed] [Google Scholar]
- 9.Higgins ST, Budney AJ, Bickel WK, Hughes JR, Foerg F. Disulfiram therapy in patients abusing cocaine and alcohol. Am J Psychiatry. 1993;150:675–676. doi: 10.1176/ajp.150.4.675b. [DOI] [PubMed] [Google Scholar]
- 10.Carroll KM, Ziedonis D, O’Malley SS, McCance-Katz E, Gordon LT, Rounsaville BJ. Pharmacologic interventions for abusers of alcohol and cocaine: a pilot study of disulfiram versus naltrexone. Am J Addict. 1993;2:77–79. [Google Scholar]
- 11.Higgins ST, Roll JM, Bickel WK. Alcohol pretreatment increases preference for cocaine over monetary reinforcement. Psychopharmacology (Berl) 1996;123:1–8. doi: 10.1007/BF02246274. [DOI] [PubMed] [Google Scholar]
- 12.Jatlow PM, Ellsworth JD, Bradberry CW, Winger G, Taylor R, Roth RK. Cocaethylene: a neuropharmacologically active metabolite associated with concurrent cocaine-ethanol ingestion. Life Sci. 1991;48:1787–1794. doi: 10.1016/0024-3205(91)90217-y. [DOI] [PubMed] [Google Scholar]
- 13.Carroll KM, Nich C, Ball SA, McCance-Katz E, Rounsaville BJ. Treatment of cocaine and alcohol dependence with psychotherapy and disulfiram. Addiction. 1998;93:713–728. doi: 10.1046/j.1360-0443.1998.9357137.x. [DOI] [PubMed] [Google Scholar]
- 14.Fuller RK, Branchey L, Brightwell DR, Derman RM, Emrick CD, Iber FL, James KE, Lacoursiere RB, Lee KK, Lowenstam I. Disulfiram treatment of alcoholism: a Veterans Administration cooperative study. JAMA. 1986;256:1449–1455. [PubMed] [Google Scholar]
- 15.George TP, Chawarski MC, Pakes JA, Carroll KM, Kosten TR, Schottenfeld RS. Disulfiram versus placebo for cocaine dependence in buprenorphine-maintained subjects: a preliminary trial. Biol Psychiatry. 2000;47:1080–1086. doi: 10.1016/s0006-3223(99)00310-8. [DOI] [PubMed] [Google Scholar]
- 16.Petrakis IL, Carroll KM, Gordon LT, Nich C, McCance-Katz E, Rounsaville BJ. Disulfiram treatment for cocaine dependence in methadone-maintained opioid addicts. Addiction. 2000;95:219–228. doi: 10.1046/j.1360-0443.2000.9522198.x. [DOI] [PubMed] [Google Scholar]
- 17.McCance-Katz EF, Kosten TR, Jatlow PM. Chronic disulfiram treatment effects on intranasal cocaine administration: initial results. Biol Psychiatry. 1998;43:540–543. doi: 10.1016/S0006-3223(97)00506-4. [DOI] [PubMed] [Google Scholar]
- 18.McCance-Katz EF, Kosten TR, Jatlow PM. Disulfiram effects on acute cocaine administration. Drug Alcohol Depend. 1998;52:27–39. doi: 10.1016/s0376-8716(98)00050-7. [DOI] [PubMed] [Google Scholar]
- 19.Hameedi FA, Rosen MI, McCance-Katz EF, McMahon TJ, Price LH, Jatlow PM, Woods SW, Kosten TR. Behavioral, physiological, and pharmacological interaction of cocaine and disulfiram in humans. Biol Psychiatry. 1995;37:560–563. doi: 10.1016/0006-3223(94)00361-6. [DOI] [PubMed] [Google Scholar]
- 20.Carroll KM, Rounsaville BJ, Gordon LT, Nich C, Jatlow PM, Bisighini RM, Gawin FH. Psychotherapy and pharmacotherapy for ambulatory cocaine abusers. Arch Gen Psychiatry. 1994;51:177–197. doi: 10.1001/archpsyc.1994.03950030013002. [DOI] [PubMed] [Google Scholar]
- 21.Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin FH. One year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: delayed emergence of psychotherapy effects. Arch Gen Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- 22.Carroll KM, Nich C, Ball SA, McCance-Katz EF, Frankforter TF, Rounsaville BJ. One year follow-up of disulfiram and psychotherapy for cocaine-alcohol abusers: sustained effects of treatment. Addiction. 2000;95:1335–1349. doi: 10.1046/j.1360-0443.2000.95913355.x. [DOI] [PubMed] [Google Scholar]
- 23.Rawson RA, Huber A, McCann MJ, Shoptaw S, Farabee D, Reiber C, Ling W. A comparison of contingency management and cognitive-behavioral approaches during methadone maintenance for cocaine dependence. Arch Gen Psychiatry. 2002;59:817–824. doi: 10.1001/archpsyc.59.9.817. [DOI] [PubMed] [Google Scholar]
- 24.McKay JR, Alterman AI, Cacciola JS, O’Brien CP, Koppenhaver J, Shepard DS. Continuing care for cocaine dependence: comprehensive 2-year outcomes. J Consult Clin Psychol. 1999;67:420–427. doi: 10.1037//0022-006x.67.3.420. [DOI] [PubMed] [Google Scholar]
- 25.McKay JR, Alterman AI, Cacciola JS, Rutherford MJ, O’Brien CP, Koppenhaver J. Group counseling versus individualized relapse prevention aftercare following intensive outpatient treatment for cocaine dependence. J Consult Clin Psychol. 1997;65:778–788. doi: 10.1037//0022-006x.65.5.778. [DOI] [PubMed] [Google Scholar]
- 26.Maude-Griffin PM, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, Hall SM. Superior efficacy of cognitive-behavioral therapy for crack cocaine abusers: main and matching effects. J Consult Clin Psychol. 1998;66:832–837. doi: 10.1037//0022-006x.66.5.832. [DOI] [PubMed] [Google Scholar]
- 27.Rohsenow DJ, Monti PM, Martin RA, Michalec E, Abrams DB. Brief coping skills treatment for cocaine abuse: 12-month substance use outcomes. J Consult Clin Psychol. 2000;68:515–520. doi: 10.1037//0022-006x.68.3.515. [DOI] [PubMed] [Google Scholar]
- 28.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV, Patient Edition. Washington, DC: American Psychiatric Press; 1995. [Google Scholar]
- 29.Stout RL, Wirtz PW, Carbonari JP, DelBoca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol. 1994;(suppl 12):70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 30.Carroll KM, Rounsaville BJ, Nich C. Blind man’s bluff? effectiveness and significance of psychotherapy and pharmacotherapy blinding procedures in a clinical trial. J Consult Clin Psychol. 1994;62:276–280. doi: 10.1037//0022-006x.62.2.276. [DOI] [PubMed] [Google Scholar]
- 31.Del Boca FK, Kranzler HR, Brown J, Korner PF. Assessment of medication compliance in alcoholics through UV light detection of a riboflavin tracer. Alcohol Clin Exp Res. 1996;20:1412–1417. doi: 10.1111/j.1530-0277.1996.tb01142.x. [DOI] [PubMed] [Google Scholar]
- 32.Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York, NY: Guilford Publications; 1985. [Google Scholar]
- 33.Carroll KM. A Cognitive-Behavioral Approach: Treating Cocaine Addiction. Rockville, Md: National Institute on Drug Abuse; 1998. [Google Scholar]
- 34.Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal Psychotherapy of Depression. New York, NY: Guilford Publications; 1984. [Google Scholar]
- 35.Rounsaville BJ, Gawin FH, Kleber HD. Interpersonal psychotherapy adapted for ambulatory cocaine abusers. Am J Drug Alcohol Abuse. 1985;11:171–191. doi: 10.3109/00952998509016860. [DOI] [PubMed] [Google Scholar]
- 36.Fals-Stewart W, O’Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 37.Hersh D, Mulgrew CL, Van Kirk J, Kranzler HR. The validity of self-reported cocaine use in two groups of cocaine abusers. J Consult Clin Psychol. 1999;67:37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- 38.Zanis DA, McLellan AT, Randall M. Can you trust patient self-reports of drug use during treatment? Drug Alcohol Depend. 1994;35:127–132. doi: 10.1016/0376-8716(94)90119-8. [DOI] [PubMed] [Google Scholar]
- 39.Ehrman RN, Robbins SJ. Reliability and validity of 6-month timeline reports of cocaine and heroin use in a methadone population. J Consult Clin Psychol. 1994;62:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- 40.Gibbons RD, Hedeker D, Elkin I, Waternaux C, Kraemer HC, Greenhouse JB, Shea MT, Imber SD, Sotsky SM, Watkins JT. Some conceptual and statistical issues in analyses of longitudinal psychiatric data. Arch Gen Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 41.Carroll KM, Nich C, Sifry R, Frankforter T, Nuro KF, Ball SA, Fenton LR, Rounsaville BJ. A general system for evaluating therapist adherencer and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- 42.Carroll KM, Connors GJ, Cooney NL, DiClemente CC, Donovan DM, Longabaugh RL, Kadden RM, Rounsaville BJ, Wirtz PW, Zweben A. Internal validity of Project MATCH treatments: discriminability and integrity. J Consult Clin Psychol. 1998;66:290–303. doi: 10.1037//0022-006x.66.2.290. [DOI] [PubMed] [Google Scholar]
- 43.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–429. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 44.Crits-Christoph P, Mintz J. Implications of therapist effects for the design and analysis of comparative studies of psychotherapies. J Consult Clin Psychol. 1991;59:20–26. doi: 10.1037//0022-006x.59.1.20. [DOI] [PubMed] [Google Scholar]
- 45.Luborsky L, Diguer L, Seligman DA, Rosenthal R, Krause ED, Johnson S, Halperin G, Bishop M, Berman JS, Schweizer E. The researcher’s own therapy allegiances: a “wild card” in comparison of treatment efficacy. Clin Psychol Sci Pract. 1999;6:95–106. [Google Scholar]
- 46.Robinson LA, Berman JS, Neimeyer RA. Psychotherapy for the treatment of depression: a comprehensive review of controlled outcome research. Psychol Bull. 1990;108:30–49. doi: 10.1037/0033-2909.108.1.30. [DOI] [PubMed] [Google Scholar]
- 47.Luborsky L, Rosenthal R, Diguer L, Andrusyna TP, Berman JS, Levitt JT, Seligman DA, Krause ED. The dodo bird verdict is alive and well—mostly. Clin Psychol Sci Pract. 2002;9:2–12. [Google Scholar]
- 48.Kazdin AE. Comparative outcome studies of psychotherapy: methodological issues and strategies. J Consult Clin Psychol. 1986;54:95–105. doi: 10.1037//0022-006x.54.1.95. [DOI] [PubMed] [Google Scholar]
- 49.Luborsky L, Singer B, Luborsky L. Comparative studies of psychotherapies: is it true that “everyone has won and all must have prizes?”. Arch Gen Psychiatry. 1975;32:995–1008. doi: 10.1001/archpsyc.1975.01760260059004. [DOI] [PubMed] [Google Scholar]
- 50.Uhlenhuth EH, Lipman RS, Covi L. Combined psychotherapy and pharmacotherapy. J Nerv Ment Dis. 1969;148:52–64. doi: 10.1097/00005053-196901000-00006. [DOI] [PubMed] [Google Scholar]
- 51.Rounsaville BJ, Klerman GL, Weissman MM. Do psychotherapy and pharmacotherapy for depression conflict? empirical evidence from a clinical trial. Arch Gen Psychiatry. 1981;38:24–29. doi: 10.1001/archpsyc.1981.01780260026002. [DOI] [PubMed] [Google Scholar]
- 52.Nich C, Carroll KM. Intention to treat meets missing data: implications of alternate strategies for analyzing clinical trials data. Drug Alcohol Depend. 2002;68:121–130. doi: 10.1016/s0376-8716(02)00111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.McLellan AT, Arndt IO, Metzger D, Woody GE, O’Brien CP. The effects of psychosocial services in substance abuse treatment. JAMA. 1993;269:1953–1959. [PubMed] [Google Scholar]
- 54.Carroll KM, Ball SA, Nich C, O’Connor PG, Eagan D, Frankforter TL, Triffleman EG, Shi J, Rounsaville BJ. Targeting behavioral therapies to enhance naltrexone treatment of opioid dependence: efficacy of contingency management and significant other involvement. Arch Gen Psychiatry. 2001;58:755–761. doi: 10.1001/archpsyc.58.8.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Preston KL, Silverman K, Umbricht A, DeJesus A, Montoya ID, Schuster CR. Improvement in naltrexone treatment compliance with contingency management. Drug Alcohol Depend. 1999;54:127–135. doi: 10.1016/s0376-8716(98)00152-5. [DOI] [PubMed] [Google Scholar]
- 56.Carroll KM. Manual-guided psychosocial treatment: a new virtual requirement for pharmacotherapy trials? Arch Gen Psychiatry. 1997;54:923–928. doi: 10.1001/archpsyc.1997.01830220041007. [DOI] [PubMed] [Google Scholar]