Abstract
The purpose of this study was to describe the demographic characteristics of low-income parents who perceive financial burden in managing their child’s asthma and related associations with their children’s asthma outcomes and clinical characteristics. We hypothesized that (1) identifiable differences between parents who do and do not report burden; (2) regardless of access to care, asthma outcomes would be worse for children whose parents perceive financial burden in obtaining care for their child’s condition. Baseline data from a randomized trial evaluating the effect of a school-based asthma intervention were analyzed for this research. Eight hundred thirty-five parents were interviewed by telephone regarding their child’s asthma management. Associations between demographic and clinical factors and perception of financial burden were examined using bivariate analysis. Multivariate regression analyses were used to examine associations between perceptions of financial burden and asthma outcomes, including emergency department visits, hospitalizations, and missed school days. Perceived financial burden was evident in 10 % (n = 79) of parents. Female heads of household (χ2(3) = 7.41; p < 0.05), those at the lowest income levels (χ2(3) = 12.14; p < 0.01), and those whose child’s asthma was poorly controlled (χ2(2) = 49.42; p < 0.001) were most likely to perceive financial burden. In models controlling for level of asthma control, income, and having a usual source of asthma care, parents who perceived financial burden were more likely to have children who had at least one emergency department visit (OR = 1.95; 95 % CI = 1.15 to 3.29), hospitalization (OR = 3.99; 95 % CI = 2.03 to 7.82), or missed school days due to asthma (OR = 3.26; 95 % CI = 1.60 to 6.67) in the previous year. Our results supported our hypotheses. Among low-income parents of children with asthma, the majority do not perceive financial burden to obtaining care. However, among parents that do perceive burden, urgent care use and missed school days due to asthma for their child were significantly higher, regardless of family income and having a usual source of asthma care. Mothers and grandmothers heading families and those caring for children with uncontrolled asthma were most likely to report burden. These findings have implications for clinical practice in that health care providers may be able to take simple actions to determine patients’ financial-related perceptions, correct misconceptions, and help patients consider their full range of options to manage their child’s asthma.
Keywords: Childhood asthma, Low income, Urban children, Outcomes, Barriers to care, Asthma
Introduction
Asthma is the most prevalent pediatric chronic illness, affecting seven million children in the U.S. and is the main reason children use urgent care services for a chronic condition.1 Living in urban inner-city environments has been identified as a risk factor for asthma prevalence, along with low socioeconomic status, and less access to primary care.2,3 Children living in low-income areas have above-average rates of emergency department (ED) visits and hospitalizations.4 The National Asthma Education and Prevention Program (NAEPP) has described health services utilization as an important proxy measure of disease morbidity and an independent measure of asthma outcomes.5
Advances in the evidence base for the treatment and management of asthma over the last several decades have provided solid evidence that asthma can be effectively managed by individuals and their families, but to accomplish this end, families need support from health systems and an effective ongoing therapeutic regimen.6 With rising health care costs more frequently shifted to patients in the form of co-pays, deductibles, and higher health insurance premiums, routine management may be perceived by some as financially burdensome. For children with asthma, family financial burden has been raised as a concern by a number of observers.7,8
Even in groups classified as low-income, there is variation in availability of financial resources for addressing health problems. People with similar individual- or household-level socioeconomic characteristics can live in very different local service environments.9 Anderson and colleagues have shown that, regardless of individual-level characteristics, a low-income child who resides in a metropolitan statistical area with more federally funded community health centers and a less equal distribution of income has better access to medical care.10 This access is thought to be based on the fact that greater community wealth and its distribution provide greater support for expanding health resources to low-income individuals.10 Furthermore, annual income is used as measure of relative poverty in the U.S.,11 however, accumulated wealth varies dramatically across social groups.12 Data show that, in the lowest income quintile, households headed by whites have on average more than 400 times as much wealth as those headed by African Americans.9
Given these community and individual differences, there is reason to believe that perceptions of financial burden may not always be synonymous with a family’s financial situation as viewed by others, or an external assessment of their ability to pay for health care. National data have shown that 87 % of adults with asthma report having health insurance coverage, yet 30 % of this group report facing financial barriers in obtaining care.13 Although expansions of Medicaid and State Children’s Health Insurance Programs have provided more coverage for essential medicines and preventive services for children, data suggest that even minimal levels of cost-sharing can be burdensome to insured, low-income families,14 while other work has shown that cost concerns are more often mentioned by families with private or no health insurance coverage.15,16
The potential impact of a parent’s perceptions about cost barriers to obtaining asthma care for their children is not well understood. Work with children with asthma living in inner-city Baltimore has shown no associations between perception of financial burden and underuse of medications,17 while other work has shown that children with asthma from families with high out-of-pocket expenditures for health care use less medicine18,19 and are more likely to be hospitalized.19 In the adult literature, individuals with work-related asthma who reported at least one financial barrier to asthma care were more likely to experience adverse asthma outcomes compared with individuals who did not report financial barriers.20
Although several studies have shown associations between measures of socioeconomic status and asthma outcomes, it is not clear whether parent perceptions of families’ financial situation is related to outcomes for children. Since evidence suggests that access to care alone may not predict which families are most vulnerable to perceiving financial burden with care, there may be other demographic and clinical characteristics of patients that accompany these perceptions. Understanding factors associated with parent perceptions of financial burden in low income families may help clinicians better anticipate which patients are most concerned with financial burden and need help to clarify their perceptions and/or help to understand their options better.
We could not locate studies that have specifically examined which parents are most likely to perceive financial burden nor whether such perceptions are associated with poor asthma outcomes in their children. Exploring these questions in families where children are most vulnerable to poor asthma outcomes is important given the extent of asthma-related morbidity in communities experiencing economic deprivation.21,22
The purpose of this study was to describe the demographic characteristics of low-income parents who perceive financial burden in managing their child’s asthma and related associations with their children’s asthma outcomes and clinical characteristics. Families were recruited from Detroit, Michigan, a city facing severe economic problems and a high prevalence of asthma.23 We hypothesized that (1) parents who perceive financial burden with their child’s asthma management exhibit identifiable differences compared with those where no burden is reported; (2) regardless of access to care, asthma outcomes are worse for children whose parents perceive financial burden in obtaining care for their child’s condition.
Methods
Data
We conducted a cross-sectional analysis of data from parents of urban elementary school children in Detroit, Michigan. The data used in this analysis came from the baseline assessment for a randomized trial evaluating a school-based asthma program described elsewhere.24 The study protocol was approved by the University of Michigan Institutional Review Board and the Detroit Public Schools system.
Sample
Participants were parents of school-aged children with asthma symptoms enrolled in grades 2–5 at 14 Detroit elementary schools. The participating schools were located in low-income neighborhoods in Northwest Detroit. More than 40 % of the families of the children enrolled in these elementary schools met federal guidelines for poverty. Parents of all children in grades 2 to 5 (n = 6,351) were provided a survey form designed to identify asthma cases, and 4,576 parents returned the survey with sufficient data for analysis, of which 1,217 children were identified for participation in the randomized trial.24 Of 1,217 children fitting initial criteria, parents or caretakers of 835 children agreed to participate and provided baseline data. Parents provided written informed consent for themselves and their minor child prior to the collection of any information. Parents were given small monetary incentives for their participation in the study.
Data Collection
One hour, parent baseline interview data were collected over the telephone by trained interviewers. The interview captured self-reported data related to the parent’s experience with the child’s asthma and demographic information.
Measures
Perception of Financial Burden
The main independent variable was perception of financial burden. To evaluate perceived financial burden in obtaining asthma care for the child, parents were asked the following question: “Has your child’s asthma caused any financial problems for the family?” Similar measures have been used in national surveys to measure perception of financial burden.25
Asthma Outcomes—Health Services Use and Missed School Days
The dependent variables in this study were health services use and missed school days. Frequency of health care use (ED visits, hospitalizations, ICU stays) and missed school days in the past 12 months due to the child’s asthma were assessed through parent self-report. Self-report of health care events such as ED visits and hospitalizations have been shown to be highly correlated with medical records of such events.26
Asthma Medications
We assessed which asthma medications, both controller and quick relief forms, were prescribed to the child by obtaining the names of medications through open-ended responses from the parent who were asked to assemble medicines to refer to during the interview.
Asthma Control and Frequency of Symptoms
Asthma control and frequency of symptoms were assessed based on self-report of the presence of daytime and nighttime symptoms in the previous month, which is the recommended assessment period based on the NAEPP Guidelines for the Diagnosis and Management of Asthma.5
Usual Source of Care for Asthma
To evaluate whether the child with asthma had a usual source of care, parents were asked the following question: “Not including the emergency room, does your child have a regular family doctor or health care provider that you usually go to for his/her health care?”
Demographic Characteristics
Data regarding family and household demographic data including gender of child, age of child, head of household, parent education, child and parent race, and annual household income were also collected.
Analysis
All data were analyzed using SAS 9.2. Frequencies were computed for each of the categorical variables (child gender, head of household, child and parent race, parent education, annual income, usual source of care for asthma, perceived financial burden, frequency of symptoms, asthma control, and asthma medication prescription). Asthma medications were re-coded into the child taking quick relief medication or controller medication. Asthma control was calculated by taking the worst impairment category of day or night symptoms. This technique and rationale has been used in other studies and is recommended in the NAEPP asthma guidelines.5,27 The NAEPP asthma guidelines were used to classify asthma control into three categories: poorly controlled, not well controlled, or well controlled, and four categories for frequency of symptoms: ≤2 days/week, >2 days/week but not daily, daily, and throughout the day.5
Student’s t-test and chi-squared analyses with Fisher’s exact test were used to examine differences in demographic and child clinical characteristics between parents who did and did not report perception of financial burden.
Models were then created to examine relationships between perceived burden and the outcomes of interest: ED visits, hospitalizations, and missed school days during the past 12 months. Outcomes were analyzed as both categorical and continuous variables. Both multivariate logistic and negative binomial distribution regression analyses were used for three separate models to assess whether parent perceived financial burden to obtaining asthma care was associated with ED visits, hospitalizations, and missed school days for their child. Based on the distribution of responses, ED visits, hospitalizations, and missed school days were each dichotomized into either “none” or “one or more” for logistic regression analyses. Negative binomial distribution regression was used since the outcome variables were count data, and overdispersion between the mean and variance of each of the outcomes was present.28 In all models, we controlled for level of asthma control, usual source of care for asthma, and annual household income based on the rationale that uncontrolled asthma, not having a usual source of care, and annual household income have all been shown to be associated with greater urgent care use in previous literature.29–31 Alpha values of 0.05 or less were considered significant.
Results
Demographic Characteristics
Table 1 describes demographic characteristics of the sample. Ten percent (n = 79) of parents in this sample perceived financial burden in obtaining asthma care for their child, and 90 % (n = 755) did not perceive financial burden. The mean age of the children was 8.40 years (SD = 1.29), and 53 % were male. Parents and children in this sample were predominantly African American (97 %). Among heads of household, 75 % were mothers to the child with asthma; 15 % were fathers; 6 % were grandmothers, and 4 % were “other,” consisting of step-parents, grandfathers, aunts or uncles, or another relationship to the child. Fifty-eight percent of the sample had an annual household income of less than $20,000, 24 % between $20,001 and $40,000, 12 % between $40,001 and $60,000, and 6 % had an annual household income above $60,001. Ninety-two percent of children were reported to have a usual source of care for asthma. Seventy-seven percent of parents achieved an educational level of high school or above.
TABLE 1.
Demographic characteristics of parents who do and do not experience financial burden from managing their child’s asthma
| Variable | Total sample (n = 835), % | Perception of financial burden (n = 79), % | No perception of burden (n = 755), % | p value, T, or χ2 |
|---|---|---|---|---|
| Child age (mean (SD)) | 8.40 (1.29) | 8.44 (1.28) | 8.40 (1.29) | T = 0.26; NS |
| Child sex (% male) | 53 % | 54 % | 53 % | χ2 = 0.17; NS |
| Child race | χ2 = 3.11; NS | |||
| White | 1 % | 0 % | 1 % | |
| Black | 97 % | 95 % | 97 % | |
| Other | 2 % | 5 % | 2 % | |
| Parent race | χ2 = 4.97; NS | |||
| White | 1 % | 0 % | 1 % | |
| Black | 96 % | 94 % | 97 % | |
| Other | 3 % | 6 % | 2 % | |
| Head of household | χ2 = 7.41* | |||
| Mother | 75 % | 81 % | 75 % | |
| Father | 15 % | 6 % | 16 % | |
| Grandmother | 6 % | 10 % | 5 % | |
| Other | 4 % | 3 % | 4 % | |
| Household income | χ2 = 12.14** | |||
| <20,000 | 58 % | 76 % | 57 % | |
| 20,001–40,000 | 24 % | 17 % | 25 % | |
| 40,001–60,000 | 12 % | 5 % | 12 % | |
| >60,000 | 6 % | 2 % | 6 % | |
| Parent education | χ2 = 3.35; NS | |||
| <High school | 13 % | 13 % | 13 % | |
| High school | 33 % | 34 % | 33 % | |
| 2-year college | 36 % | 33 % | 36 % | |
| College grad | 14 % | 13 % | 14 % | |
| Grad school | 4 % | 7 % | 4 % | |
| Usual source of care for asthma (% yes) | 92 % | 92 % | 92 % | χ2 = 0.001; NS |
Student’s t-test and chi-square tests were performed on demographic variables of interest to identify differences between the groups
NS not significant
*p < 0.05, **p < 0.01, as levels of significance reported
Demographic factors associated with burden were found for heads of household (χ2(3) = 7.41; p < 0.05), with a greater proportion of mothers and grandmothers perceiving financial burden; and household income (χ2(3) = 12.14; p < 0.01), with a greater proportion of those at the lowest income levels perceiving financial burden.
Clinical Characteristics
Table 2 describes frequency of symptoms, having prescribed medications, and asthma control among children in the sample. Seventy percent of children were found to be on quick-relief medication, while 24 % were on controller medication. Based on NAEPP classification for frequency of symptoms, 85 % of all children in the sample were found to have symptoms ≤2 days/week, while 5 % had symptoms 2 days/week; 8 % had daily symptoms, and 2 % of children reported symptoms throughout the day. Based on NAEPP classification for asthma control, 76 % of all children in the sample had well-controlled asthma; 17 % had not well-controlled asthma, and 7 % had poorly controlled asthma. Among children prescribed controller medication, 57 % had well-controlled asthma; 33 % had not well-controlled asthma, and 10 % had poorly controlled asthma. Nineteen percent of the sample needed controller medication based on symptom frequency but had not received a prescription.
TABLE 2.
Clinical characteristics of parents who do and do not experience financial burden from managing their child’s asthma
| Variable | Total sample (n = 835), % | Perception of financial burden (n = 79), % | No perception of burden (n = 755), % | p value, χ2 |
|---|---|---|---|---|
| Currently prescribed asthma medication (% yes) | 72 % | 71 % | 41 % | χ2 = 5.18* |
| Quick-relief medication (% yes) | 70 % | 68 % | 40 % | χ2 = 4.41* |
| Controller medication (% yes) | 24 % | 32 % | 13 % | χ2 = 7.52** |
| Frequency of symptoms | χ2 = 37.79*** | |||
| ≤2 days/week | 85 % | 61 % | 87 % | |
| >2 days/week | 5 % | 10 % | 4 % | |
| Daily | 8 % | 21 % | 7 % | |
| Throughout the day | 2 % | 8 % | 2 % | |
| Asthma control | χ2 = 49.42*** | |||
| Well-controlled | 76 % | 44 % | 80 % | |
| Not well-controlled | 17 % | 38 % | 15 % | |
| Poorly controlled | 7 % | 18 % | 5 % | |
| Asthma control of children currently prescribed controller medication (n = 513) | χ2 = 3.27, NS | |||
| Well-controlled | 57 % | 42 % | 61 % | |
| Not well-controlled | 33 % | 42 % | 31 % | |
| Poorly controlled | 10 % | 16 % | 8 % | |
| Need controller medication and has not been prescribed by physician | 19 % | 34 % | 17 % | χ2 = 7.37** |
Chi-square tests were performed on clinical variables of interest to identify differences between the groups
NS not significant
*p < 0.05, **p < 0.01, ***p < 0.001, as levels of significance reported
Clinical factors associated with burden were found for parents of children who were prescribed both quick relief (χ2(1) = 4.41; p < 0.05) and control (χ2(1) = 7.52; p < 0.01) forms of asthma medications, reported more frequent asthma symptoms (χ2(3) = 37.79; p < 0.001), had not well and poorly controlled asthma (χ2(2) = 49.42; p < 0.001), and a need of controller medication but had not received a prescription by their doctor (χ2(1) = 7.37; p < 0.01).
Asthma Outcomes
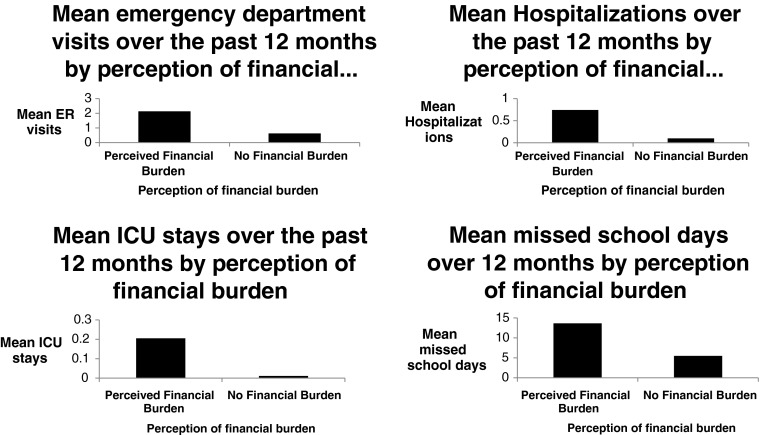
Table 3 and Figure 1 show both means and proportions of ED visits, hospitalizations, ICU stays, and missed school days for the total sample, stratified by parent perception of financial burden. Children of parents who perceived financial burden had higher means and proportions of greater than one ED visits (t = 4.87, p < 0.001; χ2(1) = 21.58; p < 0.001), hospitalizations (t = 4.75, p < 0.001; χ2(1) = 38.73; p < 0.001), ICU stays (t = 4.47, p < 0.001; χ2(1) = 24.92; p < 0.001), and missed school days (t = 5.44, p < 0.001; χ2(1) = 23.88; p < 0.001), compared with children of parents who did not perceive financial burden.
TABLE 3.
Health care use and missed school days of children with asthma whose parents do and do not perceive financial burden in managing their child’s asthma
| Variable | Total sample (n = 835), % | Perception of financial burden (n = 79), % | No perception of burden (n = 755), % | p value, T, or χ2 |
|---|---|---|---|---|
| Emergency room visits (mean (SD)) | 0.76 (2.62) | 2.12 (5.51) | 0.62 (2.07) | T = 4.87* |
| χ2 = 21.58* | ||||
| 0 | 73 % | 51 % | 75 % | |
| ≥1 | 26 % | 48 % | 24 % | |
| ICU stays (mean (SD)) | 0.02 (0.36) | 0.20 (1.15) | 0.01 (0.10) | T = 4.47* |
| χ2 = 24.92* | ||||
| 0 | 98 % | 90 % | 99 % | |
| ≥1 | 2 % | 9 % | 1 % | |
| Hospital stays (mean (SD)) | 0.15 (1.15) | 0.74 (3.44) | 0.09 (0.47) | T = 4.75* |
| χ2 = 38.73* | ||||
| 0 | 92 % | 73 % | 94 % | |
| ≥1 | 8 % | 25 % | 6 % | |
| Missed school days (mean (SD)) | 6.26 (12.87) | 13.64 (20.33) | 5.50 (11.58) | T = 5.44* |
| χ2 = 23.88* | ||||
| 0 | 40 % | 14 % | 42 % | |
| ≥1 | 60 % | 86 % | 58 % | |
Student’s t-test and chi-square tests were performed on clinical variables of interest to identify differences between the groups
NS not significant
*p < 0.001, as level of significance reported
FIGURE 1.
Outcomes of interest of children with asthma whose parents do and do not perceive financial burden in managing their child’s asthma.
Multivariate logistic regression resulted in three different models and examined the association between parent perception of financial burden and the likelihood of their child having one or more ED visits, one or more hospitalizations, and one or more missed school days due to asthma in the past 12 months (Table 4). When adjusting for level of asthma control, usual source of care for asthma, and annual household income, it was found that parents who perceive financial burden in obtaining asthma care for their children were more likely to have a child with at least one ED visit (OR = 1.95; 95 % CI = 1.15 to 3.29; p < 0.01), at least one hospitalization (OR = 3.99; 95 % CI = 2.03 to 7.82; p < 0.001), and at least one missed school day (OR = 3.26; 95 % CI = 1.60 to 6.67; p < 0.01) due to asthma in the previous year.
TABLE 4.
Adjusted multivariate models of perceived financial barriers in obtaining child’s asthma care predicting emergency department visits, hospitalizations, and missed school days due to asthma
| Variable | Emergency department visits | Hospitalizations | Missed school days | |||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| OR [95 % CI] | RR [95 % CI] | OR [95 % CI] | RR [95 % CI] | OR [95 % CI] | RR [95 % CI] | |
| Perceived financial burden in obtaining care for child’s asthma | *1.95 [1.15 to 3.29] | **1.22 [0.71 to 1.73 | **3.99 [2.03 to 7.82] | **2.30 [1.44 to 3.17] | *3.26 [1.60 to 6.67] | **0.92 [0.52 to 1.32] |
All models were adjusted for usual source of care for asthma, household income, and asthma control; estimates for control variables not displayed. Model 1 is a multivariate logistic regression model predicting more than one emergency department visit, hospitalizations, or missed school days. Model 2 is a negative binomial distribution regression model predicting emergency department visits, hospitalizations, or missed school days as continuous variables
*p < 0.01; **p < 0.001
Results from the negative binomial distribution models showed that the dispersion parameters for ED visits, hospitalizations, and missed schools day were 3.57, 9.43, and 2.66, respectively, which demonstrates overdispersion with the observed variance greater than the mean and confirmation for the use of negative binomial distribution. When adjusting for level of asthma control, usual source of asthma care, and annual household income, it was found that relationships between parent perception of financial burden and child asthma outcomes demonstrated similar relationships.
Given that 19 % of the sample had need for controller medication but had not received a prescription, perceived burden may be biased because a large percent of the sample were not receiving necessary treatments that may be the source of burden. We computed additional models that adjusted for not receiving necessary treatment. The findings concerning parent perception of financial burden with their children’s asthma management, and child asthma outcomes continued to be significant when also adjusting for this factor.
Discussion
This study of low-income urban children at risk for problems with asthma is unique in that it is the first we are aware of to examine in a pediatric population, demographic, clinical factors, and asthma outcomes related to perceived asthma-related financial burden. We found that 10 % of parents in this study reported perceptions of financial burden with their child’s asthma, and children of parents in this group were more likely to use urgent care and miss school. Our hypothesis concerning identifiable differences among parents who do and do not perceive burden was supported. Female heads of household, those at the lowest income levels, and those whose children had poorly controlled asthma were most likely to perceive financial burden. These findings support work demonstrating that there are differences among adults in perceptions of financial barriers to asthma management20 and illustrate that such perceptions vary even within a low-income population where children have asthma.
Our hypothesis concerning relationships between parent perceptions of financial burden and worse asthma outcomes for their children regardless of access to care was supported. Our analysis controlling for income and usual source of care for asthma suggest that the association between perceptions of financial burden and asthma outcomes is not solely a function of a family’s externally determined financial status or access to care. Children were more likely to use urgent care and miss school if their patients reported perceptions of financial burden even while having a usual source of care. Furthermore, the majority of children in this study were potentially eligible for the statewide MiChild or Healthy Kids health insurance programs administered through Medicaid. Objectively, insurance options were available for almost all.
There may be several reasons families’ perceived financial burden is greater than their options objectively suggest, for example, lack of information. Discussion of cost of care between health care professionals and patient in the clinical encounter is frequently lacking, although studies have shown that both patients and providers believe these discussions are important.32 A national survey of physicians treating children with asthma found that 50 % of physicians do not ask their patients about medication costs before prescribing a regimen.33 Furthermore, families may not always be aware of their out-of-pocket costs. A qualitative study conducted with families in urban, low-income communities found that parents of children with asthma frequently cited confusion regarding health care plans and medications covered by their plan.34 In addition, in a study examining adult patients' knowledge of their copayments, Benedetti et al. found that patients have limited knowledge of copayments and make decisions about how and when to seek care in response to perceived costs with very limited discussion with their health care providers.35 Parents who perceive financial burden with their child’s asthma management may not have had opportunities to address these concerns and alternative solutions with their providers.
This exploratory study has several strengths. First, it focuses on a population subgroup vulnerable to poor asthma outcomes. Findings suggest that there are clinical and demographic differences in low-income families for parents who perceive financial burden managing their child’s asthma despite access to care. Second, the study illustrates the association of these perceptions with the health of children. Perceived financial burden was strongly associated with poor asthma outcomes and urgent care use.
Addressing perceptions of financial burden may not be frequent in clinical care, however, there are ways health care professionals can help their patients by doing so.36 Cost of medications and health services are generally not within the control of individual practitioners. However, simple actions might be taken to reduce concerns for parents, especially low-income families. Health care providers can routinely ask parents if they experience specific financial barriers. They can ascertain the perceived greatest cost with obtaining medicine and asthma devices and provide suggestions toward alleviating these. Clinical recommendations can be adjusted accordingly, for example, prescribing generics or accessing local programs that provide assistance with pharmaceutical and medical devices. Health care professionals might inquire if the family has explored routine options for insurance coverage (e.g., through child health insurance programs) and provide information regarding access to these and the types of services covered. Under-enrollment in child health insurance programs is not uncommon. For example, although over 40,000 children are enrolled in the MiChild program for Michigan children, an additional 10,000 are eligible but not enrolled.37 Health care professionals might also refer patients to community organizations assisting families with health and economic concerns. None of these are time-consuming actions and may both assist families to manage better and reflect for patients the provider’s desire to be a full partner in asthma care.
There are limitations to this research that should be noted. Because the study was cross-sectional, causal direction in associations between perceptions and outcomes cannot be determined, that is, do perceptions of burden produce more urgent care use or does urgent care use produce greater perceptions of burden. Parents were asked to recall healthcare utilization and missed school days due to their child’s asthma over the last 12 months. Errors in recall may have affected the accuracy of the numbers reported. However, recall of signal health care events such as ED visits and hospitalizations have been shown to correlate highly with medical records of such events.26,38 Access to health care does not mean access to quality of care.20,39 It may be that deficiencies in quality in this sample produced need for more health care use. However, quality was likely variable across the many providers represented in the population studied and, as such, would not account for findings regarding any one or small group of children. We did not have data available to assess whether health care providers in fact offered alternative options to their patients. Future studies may consider assessing the presence of these actions. The study participants were predominately low-income African Americans residing in Detroit, therefore findings may not be generalizable to other populations, however, may have relevance to low-income groups. Additionally, we did not have data available to examine asthma among multiple children in the household or other chronic conditions that children in the sample may have. These factors may influence parent perceptions of financial burden, and future studies may consider further examination. Lastly, since these data are self-reported, social desirability may have also contributed to the small number of families reporting financial burden, therefore, burden could be greater than represented in data presented here, that is, be underestimated.
Study findings have implications for future research. The need to understand psychological stress as a mediator between factors of socioeconomic status and lung-related health outcomes has been described in the literature.40 Research might explore the mechanisms through which perceptions of financial burden lead to asthma outcomes and urgent care use. Additionally, future studies might more directly collect data regarding specific aspects of perceived financial burden in obtaining asthma care for children, that is, what costs related to medicines, devices, services, and supports are most likely to produce financial stress. How much does loss of work time, transportation costs, child care expenses, or extent of or confusion about copayments for care produce perceptions of burden? Further inquiry into responses to perceptions of financial burden by individuals may help to inform interventions for families living with asthma and improve communication between health care professionals and their patients.
Conclusion
Among low-income parents of urban elementary school children with asthma participating in this study, the majority did not perceive financial burden in managing their child’s asthma. However, among parents that did perceive burden, children were more likely to visit the ED, be hospitalized, and miss school days due to asthma. Female heads of household, those at the lowest income level, and those whose children had poorly controlled asthma were most likely to perceive burden. Externally determined financial status of the family or having a usual source of asthma care did not fully explain perceptions of burden. Addressing financial-related perceptions of parents may be an opportunity for health care professionals to help their patients more fully explore options. Simple actions by the healthcare provider to address perceptions of financial burden could be of benefit to patients and enhance their ability to control asthma. Such communication would also reflect the intention of the health care provider to be sensitive to patient needs.
Acknowledgments
The study described in this article was supported by grant 1 R01 HR-56028 of the Lung Division of the National Heart, Lung, and Blood Institute. The authors would like to thank Michael Cabana and Melissa Valerio for their feedback on an initial draft and Katherine Faiver and Megan Jensen for their assistance with preparation of the manuscript.
References
- 1.Centers for Disease Control and Prevention. Asthma-fast-stats web site. http://www.cdc.gov/asthma/faststats.html. Updated April 27, 2009. Accessed April 17, 2012.
- 2.von Maffei J, Beckett WS, Belanger K, et al. Risk factors for asthma prevalence among urban and nonurban African American children. J Asthma. 2001;38(7):555–564. doi: 10.1081/JAS-100107120. [DOI] [PubMed] [Google Scholar]
- 3.LaVeist T. Minority populations and health: an introduction to health disparities in the U.S. San Francisco, CA: Jossey-Bass; 2005. [Google Scholar]
- 4.National Heart, Lung, and Blood Institute. What is asthma web site. http://www.nhlbi.nih.gov/health/dci/Diseases/Asthma/Asthma_WhoIsAtRisk.html Updated February 1, 2011. Accessed April 17, 2012.
- 5.National Asthma Education and Prevention Program (NAEPP). Guidelines for the diagnosis and management of asthma. Expert Panel Report 3. US Dept of Health and Human Services; 2007.
- 6.Lara M, Rosenbaum S, Rachelefsky G, Nicholas W, et al. Improving childhood asthma outcomes in the United States: a blueprint for policy action. Pediatrics. 2002;109(5):919–930. doi: 10.1542/peds.109.5.919. [DOI] [PubMed] [Google Scholar]
- 7.O'Connell EJ. The burden of atopy and asthma in children. Allergy. 2004;59(78):7–11. doi: 10.1111/j.1398-9995.2004.00563.x. [DOI] [PubMed] [Google Scholar]
- 8.Mailick MD, Holden G, Walther VN. Coping with childhood asthma: caretakers' views. Heal Soc Work. 1994;19(2):103–111. doi: 10.1093/hsw/19.2.103. [DOI] [PubMed] [Google Scholar]
- 9.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 10.Andersen RM, Yu H, Wyn R, Davidson PL, Brown ER, Teleki S. Access to medical care for low-income persons: how do communities make a difference? Med Care Res Rev. 2002;59(4):384–411. doi: 10.1177/107755802237808. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Department of Health & Human Services. 2012 HHS poverty guidelines web site. http://aspe.hhs.gov/poverty/12poverty.shtml#thresholds. Published January 26, 2012. Accessed April 17, 2012.
- 12.Kochhar, R, Fry, R, Taylor, P. Pew Research Center. Wealth gaps rise to record highs between Whites, Blacks, Hispanics. http://pewresearch.org/pubs/2069/housing-bubble-subprime-mortgages-hispanics-blacks-household-wealth-disparity. Published July 26, 2011. Accessed April 17, 2012.
- 13.King M. Cost barriers to asthma care—a comparison by insurance status: national Health Interview Survey and National Asthma Call-Back Survey 2009. Presented at the American Public Health Association Annual Meeting; 2011; Washington, D.C.
- 14.Selden TM, Kenney GM, Pantell MS, Ruhter J. Cost sharing in Medicaid and CHIP: how does it affect out-of-pocket spending? Health Aff (Project Hope) 2009;28(4):w607–w619. doi: 10.1377/hlthaff.28.4.w607. [DOI] [PubMed] [Google Scholar]
- 15.Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;5(6):511–518. doi: 10.1370/afm.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shrank WH, Fox SA, Kirk A, et al. The effect of pharmacy benefit design on patient–physician communication about costs. J Gen Intern Med. 2006;21(4):334–339. doi: 10.1111/j.1525-1497.2006.00402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eggleston PA, Malveaux FJ, Butz AM, et al. Medications used by children with asthma living in the inner city. Pediatrics. 1998;101(3 Pt 1):349–354. doi: 10.1542/peds.101.3.349. [DOI] [PubMed] [Google Scholar]
- 18.Ungar WJ, Kozyrskyj A, Paterson M, Ahmad F. Effect of cost-sharing on use of asthma medication in children. Arch Pediatr Adolesc Med. 2008;162(2):104–110. doi: 10.1001/archpediatrics.2007.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karaca-Mandic P, Jena AB, Joyce GF, Goldman DP. Out-of-pocket medication costs and use of medications and health care services among children with asthma. JAMA. 2012;307(12):1284–1291. doi: 10.1001/jama.2012.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knoeller GE, Mazurek JM, Moorman JE. Work-related asthma, financial barriers to asthma care, and adverse asthma outcomes: asthma call-back survey, 37 states and District of Columbia, 2006 to 2008. Med Care. 2011;49(12):1097–1104. doi: 10.1097/MLR.0b013e31823639b9. [DOI] [PubMed] [Google Scholar]
- 21.United States Census. Poverty web site. http://www.census.gov/hhes/www/poverty/. Updated on December 14, 2011. Accessed April 17, 2012.
- 22.Schulz AJ, Williams DR, Israel BA, Lempert LB. Racial and spatial relations as fundamental determinants of health in Detroit. Milbank Q. 2002;80(4):677–707. doi: 10.1111/1468-0009.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Michigan Department of Community Health. Asthma. http://www.michigan.gov/mdch/0,1607,7-132--13055--,00.html. Accessed April 17, 2012.
- 24.Clark NM, Brown R, Joseph C, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- 25.Tseng CW, Dudley RA, Brook RH, et al. Elderly patients' preferences and experiences with providers in managing their drug costs. J Am Geriatr Soc. 2007;55(12):1974–1980. doi: 10.1111/j.1532-5415.2007.01445.x. [DOI] [PubMed] [Google Scholar]
- 26.Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on patient outcomes. Pediatric. 2006;117(6):2149–2157. doi: 10.1542/peds.2005-1055. [DOI] [PubMed] [Google Scholar]
- 27.Sharma HP, Matsui EC, Eggleston PA, Hansel NN, Curtin-Brosnan J, Diette GB. Does current asthma control predict future health care use among black preschool-aged inner-city children? Pediatric. 2007;120(5):e1174–e1181. doi: 10.1542/peds.2007-0206. [DOI] [PubMed] [Google Scholar]
- 28.Heeringa SG, West BT, Berglund PA. Applied survey data analysis. Boca Raton, FL: Chapman & Hall; 2010. [Google Scholar]
- 29.Wasilewski Y, Clark NM, Evans D, Levison MJ, Levin B, Mellins RB. Factors associated with emergency department visits by children with asthma: implications for health education. Am J Public Health. 1996;86(10):1410–1415. doi: 10.2105/AJPH.86.10.1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright K. Disparities and predictors of emergency department use among California's African American, Latino, and White children, aged 1–11 years, with asthma. Ethn Dis. 2009;19(1):71–77. [PubMed] [Google Scholar]
- 31.Kim H, Kieckhefer GM, Greek AA, Joesch JM, Baydar N. Health care utilization by children with asthma. Prev Chronic Dis. 2009;6(1):A12. [PMC free article] [PubMed] [Google Scholar]
- 32.Alexander GC, Casalino LP, Tseng CW, McFadden D, Meltzer DO. Barriers to patient–physician communication about out-of-pocket costs. J Gen Intern Med. 2004;19(8):856–860. doi: 10.1111/j.1525-1497.2004.30249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel MR, Coffman JM, Tseng CW, Clark NM, Cabana MD. Physician communication regarding cost when prescribing asthma medication to children. Clin Pediatr (Phila) 2009;48(5):493–498. doi: 10.1177/0009922808330110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Laster N, Holsey CN, Shendell DG, Mccarty FA, Celano M. Barriers to asthma management among urban families: caregiver and child perspectives. J Asthma. 2009;46(7):731–739. doi: 10.1080/02770900903082571. [DOI] [PubMed] [Google Scholar]
- 35.Benedetti NJ, Fung V, Reed M, et al. Office visit copayments: patient knowledge, response, and communication with providers. Med Care. 2008;46(4):403–409. doi: 10.1097/MLR.0b013e31815c3192. [DOI] [PubMed] [Google Scholar]
- 36.Alexander GC, Tseng CW. Six strategies to identify and assist patients burdened by out-of-pocket prescription costs. Cleve Clin J Med. 2004;71(5):433–437. doi: 10.3949/ccjm.71.5.433. [DOI] [PubMed] [Google Scholar]
- 37.Riba M, Ehrlich N, Udow-Phillips M, Clark K. Cover Michigan survey 2011. Ann Arbor, MI: Center for Healthcare Research & Transformation; 2011. [Google Scholar]
- 38.Martin LM, Leff M, Calonge N, et al. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–218. doi: 10.1016/S0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 39.Baicker K, Chandra A. Myths and misconceptions about U.S. health insurance. Health Aff (Project Hope) 2008;27(6):w533–w543. doi: 10.1377/hlthaff.27.6.w533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wright RJ. Psychological stress: a social pollutant that may enhance environmental risk. Am J Respir Crit Care Med. 2011;184:752–754. doi: 10.1164/rccm.201106-1139ED. [DOI] [PMC free article] [PubMed] [Google Scholar]