Abstract
Objective
To examine gender differences in the association between beliefs in heart disease preventability and 10-year incidence of coronary heart disease (CHD) in a population-based sample.
Methods
2,688 non-institutionalized Nova Scotians without prior CHD enrolled in the Nova Scotia Health Study (NSHS95) and were followed for 10 years. Risk factors, health behaviors and incident CHD were assessed. Participants responded “yes” or “no” to a question about heart disease preventability.Survival models, adjusted for age, income,total and high density lipoprotein (HDL) cholesterol, and systolic blood pressure, were used to estimate the relation between health belief and incident CHD. Gender differences in the relation between health beliefs and health behaviors were assessed.
Results
Gender was a significant moderator of the relation between belief and CHD incidence;specifically,women who believed heart disease could be prevented were less likely to have incident CHD events compared to women who believed heart disease could be not prevented (HR=0.36, 95% CI0.24-0.55, p <.001). This relation was not found for men. Belief was also related to smoking behavior for women (β = −0.70, OR= 0.50, 95% CI = 0.33-0.74, p =.001), but not men. Smoking significantly mediated the relation between health beliefs and incident CHD for women (z = −1.96, p =.05), but not for men.
Conclusion
Health belief in prevention and subsequent smokingwas an important independent predictor of incident coronary heart disease in women, but not men.
Keywords: health beliefs, gender differences, cardiovascular disease
Introduction
Coronary heart disease (CHD) is the leading cause of death among women and men in the United States, accounting for about 1 of every 5 deaths (Lloyd-Jones et al., 2010). It is well documented that certain health behaviors and lifestyle choices, such as smoking, eating high fat foods, lack of exercise, and exposure to stress, influence the development of CHD (Yusuf et al., 2004). However, previous studies have also shown that knowledge about CHD risk factors correlatesonly weakly with participation in physical activity andmaintenance of a healthy diet, and does not have a significant influence on smoking cessation or adherence to blood pressure and cholesterol-lowering treatments (Alm-Roijer, Stagmo, Uden, & Erhardt, 2004).
There are a number of prominent theories concerning people’s tendency to engage in positive health behaviors. These include the health belief model (M.H. Becker, 1974), protection motivation theory (Rogers, 1975), theory of reasoned action (Ajzen & Fishbein, 1977), social learning theory (Bandura, 1986) and the theory of planned behavior (Ajzen & Madden, 1986), with each theory highlighting a particular determinant of health behavior such as motivation, behavior enactment, or multi-stage processes (Armitage & Conner, 2000). Although these theories concern a range of different predictors of health behaviors, none take into account people’s fundamental belief in preventability of disease as a factor in motivation or behavior change. While much of the current literature discusses risk perception(Byrne, Walsh, & Murphy, 2005; DiMatteo, Haskard, & Williams, 2007; Hay, Coups, & Ford, 2006),overall beliefin disease preventabilitymay also be adeterminant of health behaviors and as such may inform our ability to conduct health education and prevention strategies.
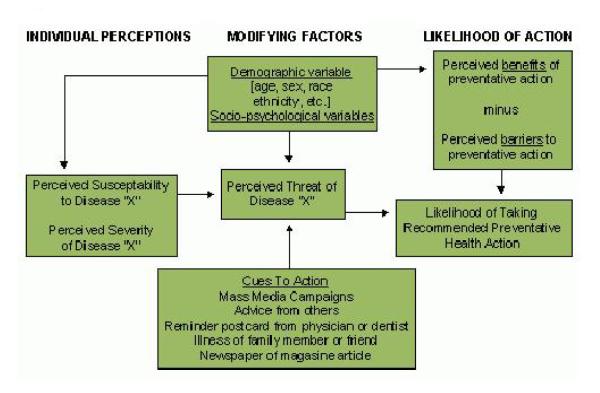
This study was guided by the health belief model, and specifically examined whether people’s perceived preventability of disease would impact their preventive health behaviors and their health outcomes. The original health belief model proposed by Becker (1974) suggested that some people use preventative health behaviors to avoid disease whereas others do not, depending on their perceived threat of disease, their perceived susceptibility, their perceived severity of disease, and their perceived benefits of health-seeking action countered against the inherent barrier (Figure 1). Although the health belief model does not directly include perceived preventability of disease in its conceptual framework, we chose this model as we viewed beliefs in prevention to be proxies for beliefs about susceptibility and threat and as having the same fundamental relation to behavior and outcomes. Other models do not containconstructs for which prevention beliefs could serve as a reasonable proxy.
Figure 1.
Becker’s Health Belief Model
Research generated by the health belief model has often found that women behave more consistently in relation to their health attitudes and beliefs than do men (Armitage, Norman, & Conner, 2002; Courtenay, Mccreary, & Merighi, 2002; Tarrant & Cordell, 1997; Weijzen, de Graaf, & Dijksterhuis, 2009). Evidence suggests that men and women differ in their beliefs about vulnerability to disease and their subsequent engagement in preventative health behaviors. Gender socialization influences health behavior, including men and women’s perceptions of and use of their bodies, and their psychosocial adjustment to illness(Sabo, 2000). Overall, men are more likely to adopt attitudes and beliefs that undermine their health and well-being, including being less likely to perceive themselves as vulnerable to disease (Courtnenay, 2000; Eisler, 1995; Sabo, 2000; Tarrant & Cordell, 1997; Williams, 2003). This can be seen as a consequence of gender socialization, as men and adolescent males who adopt traditional or stereotypic beliefs about masculinity have greater health risks than their peers with less traditional beliefs. (Courtnenay, 2000; Eisler, 1995; Lippa, 2000).As a result, men often engage in riskier behaviors such as smoking, maintaining a poor diet, failing to exercise, and abusing alcohol, whereaswomen tend to engage in health protective behaviors (Courtenay, et al., 2002; Kaplan & Marks, 1995; Nicholas, 2000). This gender specific perception of health risk and subsequent health behavior is seen in nearly every racial and ethnic group(Courtenay, et al., 2002).
Although there arewell documented gender differences in attitude-behavior consistency, the influence of this gender difference on disease outcomes is less well-established. For example,although one ecological study showed that up to 40% of the gender differences in cardiovascular risk mortality can be attributed to differences in five health behaviors(Jackson et al., 1997), there are no longitudinal, population-based studies that have demonstrated that gender differences in the attitude-behavior link are consequential, particularly in heart disease.
Accordingly, the primary goal of this study was to test the hypothesis that gender moderates the relation between belief in CHD preventability and CHD incidence in a large, population-based sample of participants from Nova Scotia, Canada. That is, we examined whether the magnitude of the association between belief in CHD preventability and CHD incidence varied for men versus women. We further examined whether differential participation in health behaviorsby men and women mediates the relation between health beliefs and incident CHD outcomes.Specifically, we examined whether a specific health behavior (i.e., smoking) could bea mechanism by which health belief confers increased risk of CHD incidence. We chose to examine smoking as it is a well-known behavioral risk factor for CHD that is monolithically negative (there are no good reasons to smoke) and is largely a matter of choice (there are no mitigating factors where a physician might encourage a patient to keep smoking).
We used a large population-based sample to understand how these theories play out in a more naturalistic setting. Additionally, as our dataset includes 10-year ischemic cardiac disease outcomes, we were able to test not only the effect of health beliefs on health behaviors, but also its subsequent implications on long-term disease outcomes. Given that data were collected in Canada, we were able to link participants’ baseline survey data with their medical records. The universal structure of the Canadian healthcare system further removed participants’ barriers to health care, which may have been a confounder if we had considered at the association of prevention beliefs and health outcomes in a cohort from the United States. Thus, we were able to test how health beliefs and subsequent health behaviors actually affected CHD incidence, which allows us to make some causal inferences that would not be possible cross-sectionally or in nations without universal health coverage.
Methods
The Nova Scotia Health Study (NSHS95) was a population-based survey implemented by Heart Health Nova Scotia in partnership with the Nova Scotia Department of Health to estimate the distributions of selected health indicators and preventive practices of Nova Scotians. The sample was selected in 1995 based on a probability-sampling frame designed by Statistics Canada, the national statistical agency and census bureau, to be representative of the Nova Scotia population by age, gender and geographic location. Those who were ineligible due to pregnancy, breastfeeding, ill-health, or disability were screened out as their CHD risk factors (e.g. weight, blood pressure, and diabetes) were not considered stable at entry.
In 1995, 3,217 study participants were enrolled in NSHS95; 2,688 of these participants provided consent for follow-up and did not have a previous CHD. The targeted population consisted of all non-institutionalized Nova Scotians, ages 18 and above, whose names were listed in the Medical Service Insurance register (MSI), the government-sponsored, universal health insurance plan. At the time of enrollment, participants completed a survey ascertaining CHD risk factors and health behaviors. During a 10-year follow-up period, information on CHD incidence was extracted from two national health registries for CHD incidence and linked to participants’ NSHS95 data. The province provides universal healthcare coverage for all its residents, thus assuring that all survey participants had access to the same level of health care and that events were recorded using a full-capture surveillance system. The overall recruitment percentage (72%) is comparable to other large health surveys, and weights applied from propensity score analyses to test for response bias revealed no meaningful biases(Lawson, 1999).
Survey Procedure
A group of 29 public health nurses completed a 5-day training session to learn the techniques for contacting participants and collecting data. From March through November of 1995, participants responded to a questionnaire thatincluded questions regarding their health beliefs and that took approximately 90 minutes to complete. Participants also attended a health care clinic for assessment of fasting lipid levels, blood pressure, and anthropometric measures.
Measures
Demographics and traditional CHD risk factors
Participants’ age and sex were recorded from the provincial medical registry, and then verified by the nurse interviewer during the home session. Smoking, physical activity level, alcohol consumption, family history, and presence of diabetes were gathered during the home interview. Smoking status was coded such that those who reported that they had never smoked or had not smoked over the past year were defined as non-smokers and those who reported currently smoking or having quit within the past year were defined as active/recent smokers. Other traditional cardiovascular risk factors, including total cholesterol,LDL cholesterol, HDL cholesterol, and blood pressure were ascertained either during the home visit or a clinic visit approximately one-week later. Income was recorded in one of 15 ordinal categories.
Health beliefs
All participants were asked, “Based upon what you have heard or read, do you believe that heart disease can be prevented?” Participants answered “yes” or “no” to this question.
Incident CHD events
Our primary outcome was hospitalization or death by any CHD event based upon ICD -9 codes. Incident CHD hospitalizations and deaths for the 10 years following NSHS95 administration were determined from the provincial health care registry. A hospitalization was considered to be a CHD event if one of the discharge codes was for ischemic heart disease (International Classification of Diseases [ICD] -9 codes 410.x,411.x, 413.x, and 414.x and ICD-10 codes I21.x, I23.x, I24.x, and I25.x). This included acute myocardial infarction (MI) and other forms of acute ischemic heart disease, but excluded old or previous MIs (codes 412 and I22/I25.2).All hospitals submit discharge information to the provincial health care registry for reimbursement. Furthermore, reimbursements for hospitalizations that occur outside Nova Scotia are paid by the provincial plan. Thus, the provincial health care registry captures all hospitalizations for which the government-sponsored plan makes payment. The dates of all CHD events were obtained.To limit the analyses to incident events, we excluded participants with a CHD diagnosis prior to their baseline survey by searching for documentation of a CHD event in the 5 years prior to their survey date using the data sources described above. Additionally, participants who had multiple outcomes were censored in survival analyses at the time of their first event, thus there are no multiple events for participants.
All deaths are reported to provincial offices, which in turn notify the national census bureau, Statistics Canada, which applies a nationally consistent process of determining the underlying cause of death. Specifically, these data were converted to the ICD codes by staff at Statistics Canada, and only those codes listed above qualified as fatal CHD. Data was extracted by Population Health Unit of Dalhousie University. Participants were observed for up to 10 years, from the date of their initial visit in 1995 until the earliest of the following: 10-year anniversary of their initial visit date, March 2005, date of emigration, death from causes other than CHD, or documented incident CHD.
Analysis
Means and frequencies were calculated for descriptive purposes, with t-tests and chi-squares calculated to test for differences between genders and health beliefs. Cox proportional hazards models were constructed to determine whether health belief predicts incident CHD over and above traditional cardiovascular risk factors. Specifically, we estimated the hazard ratios (HR) of health belief for incident CHD, adjusted for age at baseline to control for cohort and healthy survivor effects,income as a marker for socioeconomic status, and used a decomposed Framingham risk score to control for traditional cardiovascular risk factors (total and HDL cholesterol, systolic blood pressure) because we were interested in the possible mediating effects of health behaviors such as smoking. We entered a cross-product gender-by-health belief interaction term in our Cox proportional hazards modelsto test whether gender moderates the relation between belief in CHD preventability and actual CHD incidence
If we found a significant moderator effect, we would thenstratify the sample by genderto testwhether smokingmediates the relation between health belief and incident CHD for men or women. We used Baron and Kenny’s definition of mediation (1986), where the independent variable is associated with the dependent variable, the independent variable is associated with the mediator, and the mediator is associated with the dependent variable with the independent variable in the model. Thus, we initially established that health belief was associated with incident CHD in women but not men using Cox proportional hazard models, we then used moderated logistic regression, to test the relation between health belief and smoking, controlling for each of the aforementioned covariates. Finally we used a Cox proportional hazard model in which smoking predicted incident CHD, controlling for belief in CHD preventability and the other covariates for men and women separately. We used a Sobel test to test the significance of mediation found using the classic Baron and Kenny mediation criteria (Baron & Kenny, 1986; Preacher & Leonardelli, 2001; Sobel, 1982). Our decision to use the classic Baron and Kenny approach rather than bootstrapping was based on the need to use a different analytic framework (survival and logistic regression) models to test the different hypothesized relations.
All analyses were performed using Statistical Package for Social Science (SPSS) software version 18 (SPSS, 2010).
Results
Descriptive statistics for the participants included in the analysis are presented in Table 1, as are significant differences between genders and health beliefs. There were 235 (8.7%) incident CHD events (226 nonfatal, 9 fatal) during 26,570 person-years of observation (incidence rate = 8.84 events/1000 person-years). As seen in Table 1, many standard risk factors were associated with both health beliefs and gender, such as cholesterol and systolic blood pressure. We then adjusted for age, cholesterol, systolic blood pressure, and income as they were possible confounders.
Table 1.
Characteristics for consented participants (N = 2,688) – mean and standard deviation unless noted otherwise.
| Characteristics | By gender |
P | By belief |
P | |||
|---|---|---|---|---|---|---|---|
| Total sample N = 2,688 |
Women n =1,306 |
Men n = 1,382 |
CHD can be prevented n = 2,227 |
CHD cannot be prevented n = 461 |
|||
| Age at baseline (years) | 46.6 ± 19.0 | 47.2 ± 19.4 | 46.0 ± 18.9 | .11 | 44.8 ± 18.5 | 55.1 ± 18.8 | <.0001 |
| CHD events, n (%) | 235 (8.8) | 101 (7.4) | 134 (10.3) | <.001 | 168 (7.6%) | 67 (14.7%) | <.0001 |
| Belief CHD cannot be prevented, n (%) |
461 (17.2) | 229 (16.6) | 232(17.8) | .41 | -- | -- | |
| Family history of CHD, n (%) | 1226 (45.6) | 667 (48.3) | 559 (42.8) | < .01 | 530 (23.8) | 103 (23.9) | .55 |
| Diabetes, n (%) | 107 (4.0) | 52 (3.8) | 55 (4.2) | .55 | 82 (3.7) | 25 (5.4) | .08 |
| High density lipids (mg/dL) | 1.3 ± 0.3 | 1.4 ± 0.4 | 1.2 ± 0.3 | < .001 | 1.2 ± .3 | 1.3 ± .4 | .003 |
| Low density lipids (mg/dL) | 3.2 ± 0.9 | 3.2 ± 1.0 | 3.3 ± 0.9 | < .05 | 3.4 ± 1.0 | 3.2 ± .9 | <.001 |
| SBP (mmHg) | 125.0 ± 17.9 | 122.1 ± 18.5 | 128.1 ± 16.7 | < .001 | 129.1 ± 18.6 | 124.1 ± 16.8 | <.001 |
| DBP (mmHg) | 76.5 ± 9.9 | 74.5 ± 9.5 | 78.7 ± 9.8 | < .001 | 77.6 ± 9.6 | 76.5 ± 9.7 | .06 |
| BMI (kg/m2) | 27.0 ± 5.6 | 26.8 ± 6.1 | 27.2 ± 5.1 | .10 | 27.0 ± 5.6 | 27.3 ± 5.6 | .32 |
| Framingham risk score | 1.4 ± 9.4 | 1.2 ± 9.3 | 4.1 ± 5.06 | < .001 | 0.6 ± 9.5 | 5.2 ± 7.8 | <.001 |
| Active smokers, n (%) | 835 (31.2) | 397 (28.9) | 438(33.7) | < .01 | 674 (30.4) | 161 (35.1) | .06 |
| High Alcohol Drinkers, n (%) | 905 (36.8) | 581 (48.4) | 324 (25.8) | <.001 | 755 (37.0) | 150 (36.1) | .74 |
| Low income, n (%) | 1344 (50.0) | 674 (51.6) | 670 (48.5) | .105 | 833 (37.4) | 219 (47.5) | <.001 |
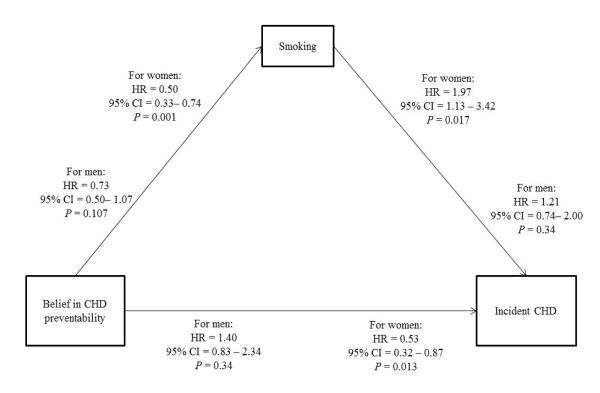
Gender significantly moderated the relation between belief in CHD preventability and CHD incidence (HR= 0.48, 95% CI = 0.27-0.86, p =.013) as hypothesized (Figure 2). This moderating effect remained after adjustment for age, total and HDL cholesterol, systolic blood pressure, and income (HR=0 .38, 95% CI = 0.19-0.78, p = .008).
Figure 2.
Model linking belief in coronary heart disease (CHD) preventability, gender, and incident CHD outcomes
As seen in Table 2, we next stratified the sample by gender, and found that women who answered that they believed in the preventability of CHDwere significantly less likely to have an incident CHD event within 10 years follow-up than women who did not believe in heart disease preventability (HR = 0.36, 95% CI = 0.24-0.55, p<.001) in a Cox regression model. After adjusting for covariates, findings for women were still significant (HR =0.53, 95% CI =0.32 - 0.87, p=.013). While the association was significant for men in the unadjusted model (HR =0.64, 95% CI = 0.44-0.95, p=.028), the association was no longer significant after adjusting for the covariates (HR= 1.34, 95% CI = 0.83-2.34, p=.20).
| WOMEN | MEN | ||
|---|---|---|---|
| Pathway | Unit of change | Regression parameter (95% CI) |
Regression parameter (95% CI) |
| Health belief→CHD | Per yes/no (0=yes,1=no) |
−1.02** HR= 0.36 (0.24 - 0.55) |
−0.44* HR = 0.64 (0.44 - 0.95) |
| Health belief→CHD adjusted 1 | −0.63* HR = 0.53 (0.32 - 0.87) |
0.34 HR =1.34 (0.83 - 2.34) |
|
| Health belief→Smoking | Per yes/no (0=yes,1=no) |
−0.23 OR= 0.80 (0.59 - 1.08) |
−0.19 OR = 0.83 (0.62 - 1.10) |
| Health belief→Smoking adjusted 1 | −0.70** OR= 0.50 (0.33 - 0.74) |
−0.31 OR = 0.73 (0.50 - 1.07) |
|
| Smoking→ CHD | −0.043 HR = 0.96 (0.62 - 1.48) |
−0.23 HR = 0.79 (0.55 - 1.16) |
|
| Smoking→ CHD adjusted 1 | 0.76** HR = 2.13 (1.23 - 3.67) |
0.16 HR =1.16 (0.72 - 1.91) |
|
| Health belief→Smoking→ CHD | Per yes/no (0=yes,1=no) |
−0.08 HR = 0.92 (0.60 - 1.43) |
−0.24 HR = 0.78 (0.54 - 1.14) |
|
Health belief→Smoking→ CHD
adjusted 1 |
0.68* HR = 1.97 (1.13 - 3.42) |
0.19 HR = 1.21 (0.74 - 1.99) |
Adjusted for age at baseline, total cholesterol, systolic blood pressure, and income
p<.05
p<.01
To further examine the relation between health belief and incident CHD, we next considered ifsmoking was a mediator in the relation of health beliefs and incident CHD for men and women separately. We first established that health belief in preventability predictedless smoking in a logistic regression for women (β =−0.70, odds ratio [OR] =0.50, 95% CI = 0.33-0.74, p=.001), but not for men (β =−0.31, OR = 0.73, 95%CI =0.50-1.07, p =.11) after adjusting for covariates. Smoking also significantly predictedincreased risk for incident CHDfor women (β = 0.68, HR= 1.97, 95%CI =1.13-3.42, p=.017), but not for men (β = 0.19, HR= 1.21, 95%CI =0.74-1.99, p =.44), after adjusting for health belief and the additional covariates in a Cox regression model, thus meeting the classic Baron and Kenny criteria of a mediator(Baron & Kenny, 1986). We tested the significance of the mediated relation with a Sobel test and found that smoking was a significant mediator of the relation between health belief and incident CHD for women (z = −1.96, p=.05). This model can be seen in Figure 3.
Figure 3.
Model linking belief in coronary heart disease (CHD) preventability, smoking, and incident CHD outcomes by gender.
Discussion
We found that gender was a significant moderator in the relation between health belief and incident CHD in this large, randomly-selected population-based sample. Although belief in CHD preventability was associated with lesser risk of incident CHD for women, the same was not true for men.We further found that women who believed heart disease can be prevented were significantly less likely toengage in CHD behavioral risk factors such a smoking, leading to a lower incidence rate of CHD in this sample. For men who believed that heart disease can be prevented, engagement in smoking was affected to a lesser extent than it was among women. Support for our hypotheses lend support to the literature suggesting the importance of accounting for patients’ gender in formulating treatment and prevention protocols (Brown & Bond, 2008; Von Bothmer & Fridlund, 2005; Wardle et al., 2004) as well as demonstrate the consequences of gender differences in attitude-behavior consistency.
We also found that age was a contributing factor to how people perceived the preventability of heart disease. Older people tended to believe that heart disease cannot be prevented and had higher cardiovascular risk factors. Our findings suggest that as people age, and they are more susceptibleto cardiovascular risk factors, they become more fatalistic about their ability to prevent heart disease.
This finding adds to literature on the health belief model, given that this literature has traditionally not considered the importance of the perception of preventability.Our study suggests that the belief that a disease is preventable, in and of itself, is an important predictor of long-term health outcome for women. Most studies that have tested health behavior theories have relied on cross-sectional correlational designs with no prospective data to corroborate findings (Weinstein, 2007). Moreover, although some studies have examined the effect of health beliefs on CHD recurrence and lifestyle change after an acute coronary event (Byrne, et al., 2005; Stafford, Jackson, & Berk, 2008), few prospective studies that have examined the effects of health beliefs on CHD incidence. Thus, our findings add valuable insight into how health beliefs affect long term health outcomes.
Gender, health beliefs, and prevention
Our findings match those of previous studies that have reported gender differences in health beliefs and preventive health behavior adherence. Studies have consistently shown a gender difference in attitude-behavior consistency, with women’s intentions more highly correlated with behavior (Nigg, Lippke, & Maddock, 2009; Weijzen, et al., 2009)compared to men. Men within nearly every racial and ethnic group are more likely than women to engage in behaviors and adopt beliefs that are detrimental to their health (Courtenay, et al., 2002). Our study shows that although both men and women tend to believe that heart disease can be prevented, for women, this translates more strongly into a direct change in their preventive health behavior.
A recent meta-analysis has shown smoking is more predictive of CHDfor women than for men(Huxley & Woodward, 2011). Our findings shed further insight into this association, suggesting that perhaps for women, smoking is an indicator of a belief that heart disease cannot be prevented. This underlying belief may have some unmeasured effect in overall CHD health and engagement in preventive health behaviors.
Women and perceived cardiovascular risk
Additionally, this study contributes to previous literature that has shown that women do not recognize that CHD can be prevented (Christian, Rosamond, White, & Mosca, 2007; Mosca, Ferris, Fabunmi, & Robertson, 2004; Mosca et al., 2005). Research has shown that women in particular are more likely to attribute their CHD to positive family history than to other major modifiable risk factors(Mosca et al., 2006; Murphy et al., 2005). Although the majority of a sample of 1,024 women in one study recognized that engaging in certain activities such as exercise, weight loss, and reducing dietary intake of cholesterol and salt may reduce the risk of heart disease, only 38% actually had a discussion about heart disease with their physician (Mosca, et al., 2004). Thus, our findings highlight the importance of patients’ beliefs in preventability when considering their engagement in preventative behaviors, treatment adherence, and long-term cardiac outcomes.
Clinical and public health implications
These results support the critical need to understand and test the mechanisms by which belief in the preventability of CHD confers increased risk of incident CHD. This program of research has important public health implications for health education, and reinforces the need to tailor our health promotion efforts to each gender. Understanding which health beliefs lead people to engage in health seeking behavior will allow for more tailored and targeted health education and cognitive interventions. Our results suggest that such interventions may be particularly effective for women. For men, however, our results suggest that strategies to strengthen the link between health beliefs and health behaviors may be more important, through better health education and community outreach.
Our study shows that the first step to any intervention or prevention program could include anassessment of what people believe about their health or about their specific health behaviors. Thus, a health practitionercould focus not only on identifying health behaviors that need to be modified but also the patient’s beliefs about the preventability of disease and health consequence. Our results suggest that effective education about the control patients may have over their health may be particularly important.Targeted public health campaigns to address this issue could also be useful, as well as physician education on this matter.
Study limitations
In addition to the lack of well measured health behaviors, other than smoking, further limitations of this study include the reliance upon one question to measure health beliefs. A more comprehensive structured interview with a validated health belief instrument (e.g., Multidimensional Health Locus of Control scale (Wallston, Wallston, & DeVellis, 1978)may have yielded a more reliable and valid assessment of health beliefs, although it may have demanded more time of participants and interviewers.
Although our primary independent variable was reliant on a single question, it was straightforward and directly measured how people felt about the preventability of heart disease. Other studies measuring health beliefs and perceived susceptibility have also used similar questions, such as Courtenay et al. (2002)’s use of three items such as “I believe I have control over my future health.”Indeed, the fact that we were able to detect differences in gender, even after adjusting for possible confounders, attests to the strength of this study measure, despite its limitations.
An additional limitation of our study was a reliance on smoking as a health behavior to measure mediation. The finding that smoking was related to women’s beliefs but not men’sshould be consideredin the context of the addictive nature of smoking(Bruijnzeel, 2012; Castañé, Berrendero, & Maldonado, 2005; Dani & De Biasi, 2001). While also had crude measures of alcohol consumption and physical activity, we do not believe that either of these measures were reliable or valid. Additionally, neither of these variables was related to health beliefs in supplemental analyses (not shown), thus not passing the initial test of mediation.
As the data we have presented here is for 10-year CHD outcomes, and the average age at baseline is 46 (with participants as young as 18 included), much of what we are capturing is early heart events. Given that women tend to have events later than men, our study is limited as we are not able to show the full scope of heart disease outcomes in women.
Another weakness of our findings is theunknown generalizabilityfrom Canada to the United States. Yet, the nationalized Canadian health care system allowed us to retrieve and link healthcare utilization data in a manner that would have been considerably more difficult in the United States.
Conclusion
Health belief in the preventability of illness was found to be an important independent predictor of incident coronary heart disease in women, but not for men. Risky health behaviors, such as smoking, in turn mediatedthe effect of health beliefs on incident CHD for women but not for men.
References
- Ajzen I, Fishbein M. Attitude-behavior relations: A theoretical analysis and review of empirical research. Psychological Bulletin. 1977;84(5):888–918. doi: 10.1037/0033-2909.84.5.888. [Google Scholar]
- Ajzen I, Madden TJ. Prediction of goal-directed behavior: Attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology. 1986;22(5):453–474. [Google Scholar]
- Armitage CJ, Conner M. Social cognition models and health behaviour: A structured review. Psychology & Health. 2000;15(2):173–189. [Google Scholar]
- Armitage CJ, Norman P, Conner M. Can the Theory of Planned Behaviour mediate the effects of age, gender and multidimensional health locus of control? [Article] British Journal of Health Psychology. 2002;7:299. doi: 10.1348/135910702760213698. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall Inc.; Englewood Cliffs, NJ: 1986. [Google Scholar]
- Baron RM, Kenny DA. The moderator and mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Becker MH. The Health Belief Model and Personal Health Behavior. Health Education Monograph. 1974;2:324–508. [Google Scholar]
- Becker MH, Haefner DP, Kasl SV, Kirscht JP, Maiman LA, Rosenstock IM. Selected psychosocial models and correlates of individual health-related behaviors. Med Care. 1977;15(5 SUPPL):27–46. doi: 10.1097/00005650-197705001-00005. [DOI] [PubMed] [Google Scholar]
- Brown L, Bond M. An Examination of the Influences on Health-Protective Behaviours among Australian Men. [10.3149/jmh.0703.274] International Journal of Men’s Health. 2008;7(3):274–287. [Google Scholar]
- Bruijnzeel AW. Tobacco addiction and the dysregulation of brain stress systems. Neuroscience & Biobehavioral Reviews. 2012 doi: 10.1016/j.neubiorev.2012.02.015. E published. doi: 10.1016/j.neubiorev.2012.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne M, Walsh J, Murphy AW. Secondary prevention of coronary heart disease: Patient beliefs and health-related behaviour. Journal of Psychosomatic Research. 2005;58(5):403–415. doi: 10.1016/j.jpsychores.2004.11.010. [DOI] [PubMed] [Google Scholar]
- Castañé A, Berrendero F, Maldonado R. The role of the cannabinoid system in nicotine addiction. Pharmacology Biochemistry and Behavior. 2005;81(2):381–386. doi: 10.1016/j.pbb.2005.01.025. doi: 10.1016/j.pbb.2005.01.025. [DOI] [PubMed] [Google Scholar]
- Christian AH, Rosamond W, White AR, Mosca L. Nine-year trends and racial and ethnic disparities in women’s awareness of heart disease and stroke: an American Heart Association national study. Journal of Womens Health. 2007;16(1):68–81. doi: 10.1089/jwh.2006.M072. doi: 10.1089/jwh.2006.M072. [DOI] [PubMed] [Google Scholar]
- Courtenay WH, Mccreary DR, Merighi JR. Gender and Ethnic Differences in Health Beliefs and Behaviors. J Health Psychol. 2002;7(3):219–231. doi: 10.1177/1359105302007003216. doi: 10.1177/1359105302007003216. [DOI] [PubMed] [Google Scholar]
- Courtnenay WH. Behavioral Factors Associated with Disease, Injury, and Death among Men: Evidence and Implications for Prevention. Journal of Men’s Studies. 2000;9(1):81. [Google Scholar]
- Dani JA, De Biasi M. Cellular mechanisms of nicotine addiction. Pharmacology Biochemistry and Behavior. 2001;70(4):439–446. doi: 10.1016/s0091-3057(01)00652-9. doi: 10.1016/s0091-3057(01)00652-9. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR, Haskard KB, Williams SL. Health Beliefs, Disease Severity, and Patient Adherence: A Meta-Analysis. Medical Care. 2007;45(6):521–528. doi: 10.1097/MLR.0b013e318032937e. 510.1097/MLR.1090b1013e318032937e. [DOI] [PubMed] [Google Scholar]
- Eisler RM. The relationship between masculine gender role stress and men’s health risk: The validation of a construct. In: Pollack RFLWS, editor. A new psychology of men. BasicBooks; New York: 1995. pp. 207–225. [Google Scholar]
- Hay J, Coups E, Ford J. Predictors of Perceived Risk for Colon Cancer in a National Probability Sample in the United States. Journal of Health Communication. 2006;11(sup001):71–92. doi: 10.1080/10810730600637376. doi: 10.1080/10810730600637376. [DOI] [PubMed] [Google Scholar]
- Huxley RR, Woodward M. Cigarette smoking as a risk factor for coronary heart disease in women compared with men: a systematic review and meta-analysis of prospective cohort studies. Lancet. 2011 doi: 10.1016/S0140-6736(11)60781-2. doi: S0140-6736(11)60781-2 [pii] [DOI] [PubMed] [Google Scholar]
- Jackson R, Chambless LE, Higgins M, Kuulasmaa K, Wijnberg L, Williams OD. Gender differences in ischemic heart disease mortality and risk factors in 46 communities: an ecological analysis. Journal of Cardiovasc Risk. 1997;7:43–54. [Google Scholar]
- Kaplan M, Marks G. Appraisal of health risks: The roles of masculinity, femininity, and sex. Sociology of Health and Illness. 1995;17:206–221. [Google Scholar]
- Lawson B. Evaluation of non-response bias in the Nova Scotia Health Survey 1995. Dalhousie University; Halifax, Nova Scotia, Canada: 1999. [Google Scholar]
- Lippa RA. Gender-related traits in gay men, lesbian women, and heterosexual men and women: the virtual identify of homosexual-heterosexual diagnosticity and gender diagnosticity. J Pers. 2000;68(5):899–926. doi: 10.1111/1467-6494.00120. [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Stroke Statistics Subcommittee Heart Disease and Stroke Statistics--2010 Update: A Report From the American Heart Association. Circulation. 2010;121(7):e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. doi: 10.1161/circulationaha.109.192667. [DOI] [PubMed] [Google Scholar]
- Mosca L, Ferris A, Fabunmi R, Robertson RM. Tracking women’s awareness of heart disease: an American Heart Association national study. Circulation. 2004;109(5):573–579. doi: 10.1161/01.CIR.0000115222.69428.C9. doi: 10.1161/01.CIR.0000115222.69428.C9. [DOI] [PubMed] [Google Scholar]
- Mosca L, Linfante AH, Benjamin EJ, Berra K, Hayes SN, Walsh BW, Simpson SL. National study of physician awareness and adherence to cardiovascular disease prevention guidelines. Circulation. 2005;111(4):499–510. doi: 10.1161/01.CIR.0000154568.43333.82. doi: 111/4/499 [pii] 10.1161/01.CIR.0000154568.43333.82. [DOI] [PubMed] [Google Scholar]
- Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, Simpson SL. Cardiovascular disease in women: National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–534. doi: 10.1161/CIRCULATIONAHA.105.588103. [DOI] [PubMed] [Google Scholar]
- Murphy B, Worcester M, Higgins R, Le Grande M, Larritt P, Goble A. Causal attributions for coronary heart disease among female cardiac patients. J Cardiopulmonary Rehabilitation. 2005;25(3):135–143. doi: 10.1097/00008483-200505000-00002. quiz 144-135. doi: 00008483-200505000-00002 [pii] [DOI] [PubMed] [Google Scholar]
- Nicholas DR. Men, Masculinity, and Cancer: Risk-factor Behaviors, Early Detection, and Psychosocial Adaptation. [Article] Journal of American College Health. 2000;49:27. doi: 10.1080/07448480009596279. [DOI] [PubMed] [Google Scholar]
- Nigg CR, Lippke S, Maddock JE. Factorial invariance of the theory of planned behavior applied to physical activity across gender, age, and ethnic groups. Psychology of Sport and Exercise. 2009;10(2):219–225. [Google Scholar]
- Preacher KJ, Leonardelli GJ. Calculation for the Sobel test. 2001 from http://people.ku.edu/~preacher/sobel/sobel.htm. [Google Scholar]
- Rogers RW. A protection motivation theory of fear appeals and attitude change. Journal of Psychology. 1975;91:93. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Sabo D. Men’s Health Studies: Origins and Trends. [Article] Journal of American College Health. 2000;49:133. doi: 10.1080/07448480009596295. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic Confidence Intervals for Indirect Effects in Structural Equation Models. Sociological Methodology. 1982;13:290–312. [Google Scholar]
- SPSS . SPSS for Windows. SPSS Inc.; Chicago: 2010. [Google Scholar]
- Stafford LP, Jackson HJP, Berk MMDP. Illness Beliefs About Heart Disease and Adherence to Secondary Prevention Regimens. Psychosomatic Medicine. 2008;70:942–948. doi: 10.1097/PSY.0b013e318187e22e. [DOI] [PubMed] [Google Scholar]
- Tarrant MA, Cordell HK. The Effect of Respondent Characteristics on General Environmental Attitude-Behavior Correspondence. Environment and Behavior. 1997;29(5):618–637. doi: 10.1177/0013916597295002. [Google Scholar]
- Von Bothmer MIK, Fridlund B. Gender differences in health habits and in motivation for a healthy lifestyle among Swedish university students. Nursing & Health Sciences. 2005;7(2):107–118. doi: 10.1111/j.1442-2018.2005.00227.x. doi: 10.1111/j.1442-2018.2005.00227.x. [DOI] [PubMed] [Google Scholar]
- Wallston KA, Wallston BS, DeVellis R. Development of the Multidimensional Health Locus of Control (MHLC) Scales. Health Educ Monogr. 1978;6(2):160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- Wardle J, Haase A, Steptoe A, Nillapun M, Jonwutiwes K, Bellisie F. Gender differences in food choice: The contribution of health beliefs and dieting. Annals of Behavioral Medicine. 2004;27(2):107–116. doi: 10.1207/s15324796abm2702_5. doi: 10.1207/s15324796abm2702_5. [DOI] [PubMed] [Google Scholar]
- Weijzen PLG, de Graaf C, Dijksterhuis GB. Predictors of the consistency between healthy snack choice intentions and actual behaviour. Food Quality and Preference. 2009;20(2):110–119. [Google Scholar]
- Weinstein ND. Misleading Tests of Health Behavior Theories. Annals of Behavioral Medicine. 2007;33:1–10. doi: 10.1207/s15324796abm3301_1. [DOI] [PubMed] [Google Scholar]
- Williams DR. The Health of Men: Structured Inequalities and Opportunities. [Article] American Journal of Public Health. 2003;93:724–731. doi: 10.2105/ajph.93.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]