Abstract
Objectives
The purpose of this study is to investigate emergency department (ED) providers’ knowledge of the life-time cancer risk attributable to radiation (LAR) from commonly performed CT scans and its association with the ordering providers’ risk/benefit analysis prior to ordering the exam. It further explores factors that may influence provider selection of a particular diagnostic imaging study in an ED setting.
Materials and Methods
Sixty-seven ED providers at the University of Rochester Medical Center completed a multiple choice questionnaire. The questions were derived to assess individual provider’s awareness of LAR from a diagnostic CT scan of the abdomen/pelvis and their behavior towards risk/benefit analysis before ordering the exam.
The association between the questions and years since completion of clinical training was determined using the Spearman correlation test. Univariate logistic regression analysis was employed for the same questions to predict the knowledge of LAR.
Results
Less than 30% of ED providers possessed accurate knowledge of LAR (p-value .025). Providers with greater clinical experience, although lacking in the knowledge of LAR, were more likely to consider patients’ radiation dose history, conduct risk/benefit analysis, and less likely to order a CT scan unnecessarily. Clinical experience was negatively correlated with perceived unnecessary use of CT scans (p-value .01).
Conclusion
A large proportion of ED providers are unaware of the life-time risk of carcinogenesis from commonly performed CT scans. The clinical experience, not the knowledge of LAR, is significantly associated with beneficial behavior toward the use of CT scanning.
INTRODUCTION
Many diagnostic imaging examinations involve exposure to ionizing radiation from radioactive materials or X-rays. The primary risk associated with ionizing radiation is cancer (1–4). The exposure from medical radiation is, by far, the greatest man-made source of radiation to the general population (5). Per capita radiation dose from medical exposures in the United States increased from 0.67 millisievert (mSv)/year in 1980 to over 3 mSv/year in 2005. CT (computerized tomography) scans are largely responsible for this dramatic increase (6–11). From 1980 to 2005 CT scan usage increased from 3 million to 60 million. This is out of proportion to population growth; a 50% growth in the US population is accompanied by a 600% increase in medical exposure to radiation (5). Although the risk for any one person is not large, increased radiation exposure for a population is a public health concern as the radiation-induced cancers typically do not occur until 1–2 decades or longer after radiation (12,13). It is now generally accepted that approximately 30% of all CT scans could be avoided altogether or replaced by a different diagnostic tool (6,10,14). Yet the current utilization trends are headed in the opposite direction.
Approximately 70 million CT scans were performed in the USA in the year 2007, which are predicted to cause 29,000 future cancers (15). Understanding the reasons contributing to over-utilization of CT scans in clinical practice is exceedingly important. Many probable factors contributing to CT over utilization include inadequate knowledge and awareness of the referring providers of the amount of radiation exposure and potential risk of inducing a fatal cancer from each of the commonly performed diagnostic CT scans, malpractice concerns, availability, accuracy, and the speed with which a test can be performed and results obtained. The emergency department (ED) of a hospital is one such setting where providers tend to over utilize CT scans. The providers are under strict time constraint and constant pressure for a quick turnaround of patients to prevent backlog. Consequences of a missed or wrong diagnosis and a potential malpractice lawsuit weigh heavily on their minds. Since CT technology can be accessed quickly, is readily available, provides pictures of pathological processes occurring in the body/organ system in exquisite detail, it is often relied upon to confirm or exclude a diagnosis, (16,17). Individual health risks are small, not immediate, and the risk/benefit assessment for CT imaging is usually considered to be in the patient’s favor.
The purpose of this study was to assess ED providers’ awareness of the cancer risk over a person’s lifespan attributable to radiation from commonly performed CT scans and to explore its associations with providers’ behavior/attitude toward risk/benefit analyses inherent to CT scanning before ordering one. Furthermore, this study intends to identify the factors that may influence provider selection of a particular imaging study in a busy ED setting.
METHODS
Data Collection
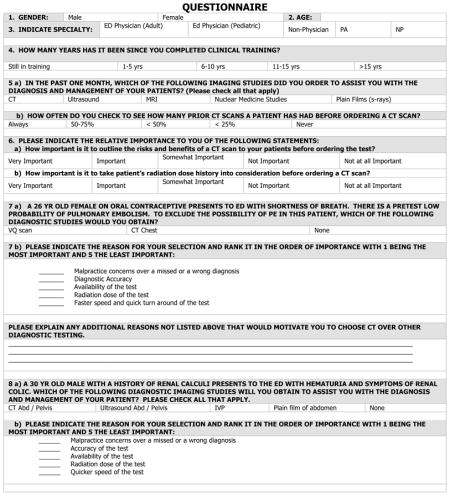
This was a cross sectional study to assess ED providers’ awareness of life-time cancer risk attributable to radiation (LAR) from a commonly performed CT scan of the abdomen and pelvis (CTAP). This was accomplished through deployment of an original multiple choice questionnaire (Appendix A) comprised of a total of 12 questions. The respondents were instructed to check the correct answer for each question. Pretesting the questionnaire amongst 10 referring providers from various medical specialties determined that the time to complete the survey was less than 10 minutes. The instrument was designed to assess the following areas:
Section A
Demographic information, including gender, age, current position, number of years elapsed since completion of clinical training, and the type of diagnostic imaging studies ordered within the past one month.
Section B
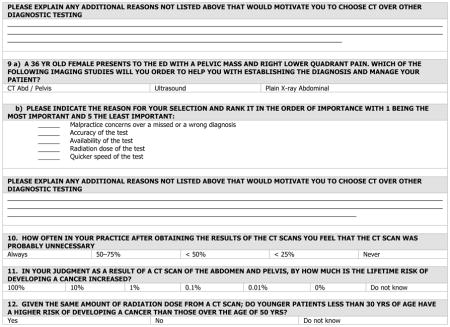
Providers’ behaviors and attitudes towards risk/benefit analysis prior to ordering a CT scan in the evaluation and management of their patients. The providers were asked how often they check the patient’s prior CT scan history before ordering one and how important it was for them to take a patient’s radiation dose history into consideration and to explain the risk and benefits of a CT scan before ordering one. The providers were also presented with three commonly encountered classic clinical scenarios that occur in an ED setting. These included cases in which pulmonary embolism (PE), renal colic, and right lower quadrant female pelvic pain were in the potential differential diagnosis list. The clinical Scenario 1 comprised of a hypothetical case of a 26 year-old-female on oral contraceptives presenting with shortness of breath with a clinical low probability of PE; Scenario 2 was a hypothetical case of a 36-year-old male with a history of renal calculi presenting with hematuria and renal colic and Scenario 3 was a hypothetical case of a 36-year-old female presenting with a pelvic mass and right lower quadrant pain. The providers were asked to choose among the diagnostic studies he/she would order for each of the clinical scenarios to diagnose and manage the patient and rank them in the order of importance. We used clinical evidence-based practice guidelines to assess the appropriate use of diagnostic imaging studies for management of each clinical presentation. (19–22).
Section C
The ED providers’ perception of the unnecessary use of a CT scan after reviewing the results of the test.
Section D
Providers’ knowledge and awareness of radiation exposure health risks. Providers were asked about the approximate increase in life-time cancer risk from a CT scan of the abdomen and pelvis (CTAP) and whether younger patients have a higher risk of developing cancer from radiation associated with a CT scan than their older counterparts. CTAP was selected because it is the most frequently performed CT scan.
Study Population
The study sample for this investigation was drawn from ED providers who work in the ED of the Strong Memorial Hospital and the Highland Hospital (SMH/HH) of the University of Rochester. This included physicians (MD), and midlevel providers (MLP) comprising physician assistants and nurse practitioners. Both adult and the pediatric ED providers were included. The providers were requested to complete the original anonymous questionnaire on a voluntary basis and it was electronically mailed with a cover letter to all the ED providers. In addition, an attempt was made to administer the survey questionnaire at prescheduled ED faculty meetings. There are a total of 96 ED providers who work in the SMH/HH ED including 40 ED attending physicians (MD), 36 ED residents (MD) and 20 midlevel providers (MLP).
Statistical Analyses
Descriptive statistics including frequency analysis were used to evaluate the frequency of provider’s awareness of LAR, participants’ demographics, pattern of risk/benefit analysis, and perceived unnecessary use of CT scans. The criteria for statistical significance level was p < 0.05. Binomial test was applied to the data to test the hypothesis that less than 30% of ED providers will possess accurate knowledge of the LAR from CTAP. Spearman correlation coefficient was used to analyze the association between the provider’s behavior and attitude toward risk/benefit analysis, perceived unnecessary use of CT scans, and years lapsed since the completion of clinical training. Univariate logistic regression analysis was employed to assess the association between the provider’s accuracy of the knowledge of LAR and questions pertaining to providers’ behavior and attitude toward risk/benefit analysis, years lapsed since the completion of clinical training (4), and the perceived unnecessary use of CT scans (10). Hottellings’ T-square test was applied to assess differences in providers ranking of the reasons for various diagnostic choices in the three different clinical scenarios. Fisher exact test was applied to test the difference in the knowledge of LAR between physician and MLP.
RESULTS
A total of 67 ED providers responded to the questionnaire by partially or completely answering the questions. Demographic characteristics of responders are shown in Table 1.
TABLE 1.
Demographic characteristics of Participating Providers
| AGE | Range 23–65 yrs Mean Age 37.6 yrs |
Frequency | Percent |
|---|---|---|---|
| GENDER | Male | 33 | 50% |
| Female | 32 | 50% | |
| YEARS SINCE COMPLETION OF CLINICAL TRAINING | Still in training | 25 | 38% |
| < 10 years | 21 | 31% | |
| > 10 years | 21 | 31% | |
| SPECIALTY | ED Physicians | 51 | 83% |
| MLP | 16 | 20% |
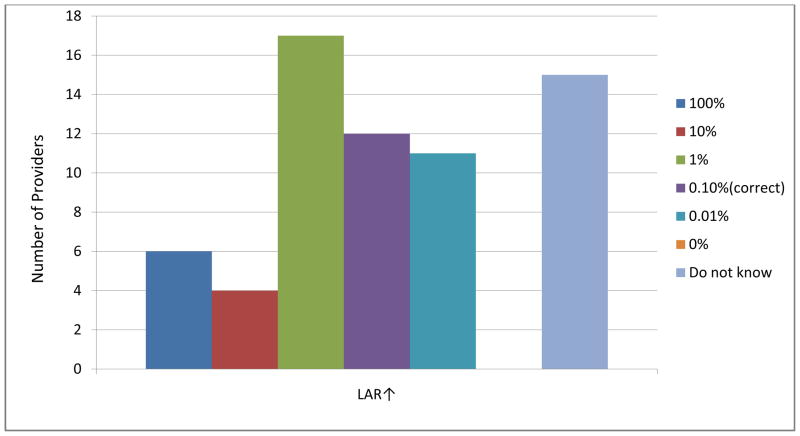
Knowledge of LAR and Hypothesis Testing
Sixty-six responders completed the question assessing the knowledge of LAR from a CTAP. One provider incorrectly checked two boxes and therefore was excluded from analysis. A total of 65 responses were included in the final analysis. Answers to the questions are shown in Figure 1. Only 12 of the 65 responders (18%) had accurate knowledge of LAR from a CTAP, 27 providers (42%) overestimated the radiation risk, 11 (17%) underestimated the risk and 15 (23%) did not know. Significantly less than 30% of ED providers had adequate knowledge of LAR (p-value 0.025). Interestingly, of the 12 responders with accurate knowledge of LAR, 11 (92%) were physicians and 1 (8%) an MLP but the association was not found to be statistically significant (p-value 0.14).
Figure 1. Frequencies of Estimated Lifetime Increased Risk from One CTAP.
QUESTION: IN YOUR JUDGMENT AS A RESULT OF A CT SCAN OF THE ABDOMEN AND PELVIS, BY HOW MUCH IS THE LIFETIME RISK OF DEVELOPING A CANCER INCREASED?”
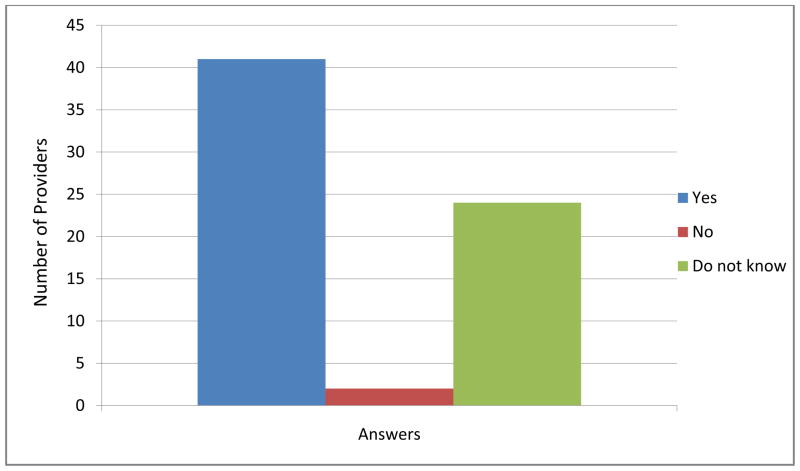
Awareness of Difference in Radiation Risk by Age
When asked if the risk of developing cancer from radiation exposure to CT scan was greater in younger patients, 41 (62%) providers believed it was greater and 24 (36%) did not know and only 1 (2%) thought that the risk was less than in the older patients (Fig 2). Of the 24 providers checking the “do not know” box 11, 69%, were a MLP.
Figure 2. Frequency distribution of awareness of difference in radiation risk by age.
QUESTION: GIVEN THE SAME AMOUNT OF RADIATION DOSE FROM A CT SCAN; DO YOUNGER PATIENTS LESS THAN 30 YRS OF AGE HAVE A HIGHER RISK OF DEVELOPING A CANCER THAN THOSE OVER THE AGE OF 50 YRS?
Behavior and Attitude Toward Risk / Benefit Analysis and its Association with the Knowledge of LAR
Table 2 shows the frequency distribution for answers to the questions addressing risk/benefit analysis. Further analysis yielded no significant association between the knowledge of LAR and the risk/benefit analysis and perceived unnecessary CT scan usage (Table 3), but as shown in Table 4 answers to the questions addressing providers behavior and attitude toward risk/benefit analysis were significant related (p-value <0.05). Although the association between the LAR and the risk/benefit analysis was not found to be statistically significant there are certain trends that are worth mentioning. Note as shown in Table 3 the odds ratio for years lapsed since completion of clinical training is less than one, thus indicating an inverse relationship between the knowledge of LAR and the clinical experience, providers with a longer time elapsed since completion of clinical training were less likely to possess accurate knowledge of the LAR. Similarly the odds ratios for questions addressing the behavior and attitude toward risk/benefit analysis is also less than one, again indicating a reverse relationship between the knowledge of LAR and providers’ likelihood of conducting a risk/benefit analysis prior to ordering a CT scan.
TABLE 2.
Frequency distribution of Behavior/Attitude toward Risk/Benefit Analysis
| Question | Always | 50–75% | < 50% | < 25% | Never |
|---|---|---|---|---|---|
| How often do you check to see how many prior CT scans a patient has had before ordering a CT scan | 26 (40%) | 19 (20%) | 10 (18%) | 8 (12%) | 4 (6%) |
| Question | Very Important | Important | Somewhat Important | Not Important | Not at all Important |
| How important is it to outline the risks and benefits of a CT scan to your patients before ordering the test | 24 (36%) | 25 (37%) | 8 (12%) | 7 (11%) | 3 (4%) |
| How important is it to take patient’s radiation dose history into consideration before ordering a CT scan? | 22 (33%) | 27 (40%) | 13 (20%) | 2 (3%) | 3 (4%) |
TABLE 3.
Univariate Logistic regression analysis of 5 questions and the knowledge of LAR
| Predictors | Odds Ratio Estimations | Odds Ratio Confidence Intervals | P-values | |
|---|---|---|---|---|
| Q4 | 0.80 | 0.52 | 1.24 | 0.32 |
| Q5 | 0.71 | 0.44 | 1.14 | 0.16 |
| Q6a | 0.73 | 0.43 | 1.22 | 0.23 |
| Q6b | 0.83 | 0.46 | 1.48 | 0.52 |
| Q10 | 1.03 | 0.49 | 2.18 | 0.94 |
TABLE 4. The association analysis between 5 questions 4, 5, 6a, 6b and 10.
Spearman correlation coefficients and calculated p-values for the 5 questions:
| Association | Spearman correlation coefficients | p-values |
|---|---|---|
| Q4 vs. Q5 | 0.01 | 0.95 |
| Q4 vs. Q6a | −0.20 | 0.11 |
| Q4 vs. Q6b | −0.16 | 0.21 |
| Q4 vs. Q10 | −0.31 | 0.01 |
| Q5 vs. Q6a | 0.24 | 0.05 |
| Q5 vs. Q6b | 0.42 | 0.00 |
| Q5 vs. Q10 | −0.19 | 0.13 |
| Q6a vs. Q6b | 0.74 | 1.06 |
| Q6a vs. Q10 | 0.06 | 0.61 |
| Q6b vs. Q10 | −0.02 | 0.87 |
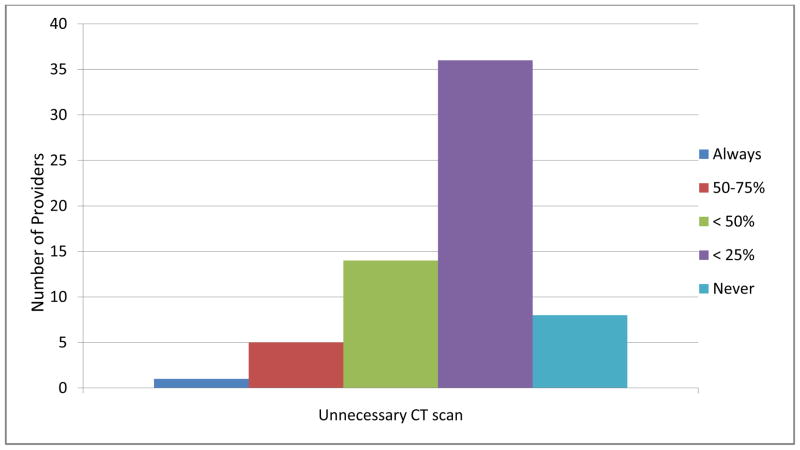
Perceived Unnecessary use of CT Scans
Figure 3 displays the responses to the question addressing how often in their practice after obtaining the results of a CT scan providers’ felt that the CT scan was probably unnecessary. Sixty-four of the 67 responders completed this question; 8 providers (13%) mentioned that this never occurred and 50 (78%) providers felt that between <25 – <50% of the time the CT scans they ordered were probably unnecessary. Providers with more clinical experience were less likely to believe that the CT scan he/she ordered was probably unnecessary (p-value 0.01).
Figure 3. Frequency Distribution of Perceived Unnecessary Use of CT Scan.
QUESTION: HOW OFTEN IN YOUR PRACTICE AFTER OBTAINING THE RESULTS OFTHE CT SCANS YOU FEEL THAT THE CT SCAN WAS PROBABLY UNNECESSARY?
Results of the Clinical Case Scenarios
Scenario 1
A total of 62 responses were included in the analysis. Five respondents (7%) incorrectly checked more than two options. Thirty (48%) providers appropriately chose to order no imaging study and explained that they would order a “D-dimer” test, and if the D-dimer was positive, they would proceed with a VQ scan; 26 (42%) selected CT scan as their first approach. Those selecting a CT scan ranked the accuracy of the test as the most important factor in their decision. Surprisingly, malpractice concerns achieved lower ranking in the overall decision-making process. The providers with longer clinical experience gave radiation dose a higher rank (p-value 0.04).
Scenario 2
Of the 67 responders, 11 were excluded from analysis for inappropriate selection of multiple options or no options. Of the 56 responders included, 22 (39%) appropriately selected either no test or a plain film of the abdomen. Only 3 (<1%) responders selected an ultrasound examination of the abdomen. Five (9%) selected an IVP and 26 (46%) providers selected a CT scan of the abdomen/pelvis. Diagnostic accuracy and availability of an imaging study were cited as important factors in determining a provider’s choice of a given diagnostic test. Those selecting no test or a test with the least amount of radiation exposure explained in their comments that clinical observation followed by plain x-ray of the abdomen and/or US examination would be their approach in the given clinical scenario. They further explained that the only reason for ordering a CT scan would be if there were clinical concerns for appendicitis or diverticulitis. Some of the providers who selected a CT scan as their first choice indicated unavailability of ultrasound as a factor leading to a decision favoring a CT scan.
Scenario 3
Ten of the 67 responders were excluded because of inappropriate selection of multiple tests or no tests at all. A majority of the providers, 37 (64%) selected appropriately ultrasound (US), 19 (33%) selected CT scan and 2 (3%) selected no test at all. Again, among the reasons given for using the CT scan, accuracy scored the highest rank. It should also be noted that the providers who selected US, also gave accuracy the highest rank. Some of the providers who selected CT scan indicated that US is the test of choice, but difficult to obtain in the ED at all times. Some said that they would obtain an US if available.
DISCUSSION
Several scientific publications have explored the referring physician’s knowledge of radiation exposure from a chest X-ray and certain commonly performed CT scans along with their associated cancer risk (18, 23–25). Overall the findings indicated that many physicians don’t grasp or explain to patients the radiation exposure involved from diagnostic imaging studies. Actual awareness level of radiation risks among physicians was surprisingly low. Some studies found no correlation with the level of training or seniority while a few found that the performance was inversely related to seniority. None of these studies address the issue if the referring providers consider potential risks and benefits of a diagnostic study before ordering a CT scan. Nor did these studies explore factors, other than the knowledge of patient radiation exposure that could have influenced a physician’s selection of a particular diagnostic imaging study. Moreover, prior studies have not investigated provider’s knowledge of LAR from commonly performed diagnostic CT scans. These studies limit their investigation to provider knowledge of patient radiation exposure and/or perceived cancer risk. While accurate knowledge of radiation exposure from commonly performed diagnostic CT is important, it is even more important to precisely understand the estimated LAR. It is the latter that provides the framework and the underpinnings for an adequate risk/benefit analysis.
Our findings indicate that a majority of the ED providers in our study group lack accurate knowledge and awareness of the increase in life time risk of developing cancer from most commonly performed CT scans. Further, the study indicates that physicians have significantly better knowledge and awareness of the risk of CT scans than the MLP. It should be noted that a unique feature of our study is that the study population included MLP. To our knowledge none of the previously published studies in the scientific literature evaluating physician knowledge of radiation exposure from diagnostic imaging studies included the MLP in their data sampling. Like physicians, the MLP have clinical privileges to order diagnostic imaging studies to assist with diagnosis and management of their patients on a daily basis. Although the observed difference in knowledge was not found to be statistically significant at p-value of 0.05, the dramatic difference in absolute numbers 11 physicians versus only 1 MLP possessing accurate knowledge of the LAR merits further evaluation with a larger sample size.
In evaluating the provider’s perception of the unnecessary use of CT scans we found the clinical experience of the ED providers to be a significant determinant in appropriate utilization of CT scans. In addition, providers with greater clinical experience were more likely to check the patient’s previous radiation dose history and explain to the patient risks and benefits of a CT scan before ordering a CT scan. The providers with longer clinical experience also gave radiation dose a higher rank under the clinical scenario 1 (p-value 0.04). These findings suggest that providers with greater clinical experience, although lacking in the accuracy of knowledge of the LAR, through cumulative clinical acumen have developed skills that enable them to effectively conduct a risk/benefit analysis, effectively communicate with the patient’s risks and benefits before ordering a CT scan and thus minimize unnecessary use of CT scans. On the other hand, providers with the least amount of clinical experience, although more likely to possess an accurate knowledge of the LAR, perhaps because of the lack of experience, may rely more on technology for accurate diagnostic information, which can often prove to be unnecessary once the results become available.
An intriguing finding was that a majority of the providers, while lacking an accurate knowledge of LAR from commonly performed CT scans, reported investigating their patients’ prior CT scan history and thought it important to consider prior radiation dose history and discuss the risks and benefits of a CT scan with the patient prior to ordering one. Yet in contradiction to the above findings, the majority of providers were of the opinion that after reviewing the results somewhere between less than 25 to less than 50% of the CT scans they ordered were probably unnecessary. We believe that this is reflective of a provider bias introduced by the timing of this investigation. At the time of this investigation there was extensive media coverage focusing on an unprecedented growth in the number of CT scans performed and a projected substantial increase in radiation-induced cancer deaths in the USA. This was compounded by the simultaneous publishing of several newspaper reports throughout the country of a few mishaps where patients were overexposed to radiation due to preventable technical problems. This resulted in a heightened public awareness of the cancer risk from CT scans. We believe that the media explosion of radiation related cancer risks from CT scans also resulted in increased sensitization of practicing clinicians as to the risks of CT scans and they began to consider the patients’ radiation dose history and discuss with the patients the risks and benefits of a CT scan before ordering a CT scan. In addition, this study may have acted as a catalyst in reinforcing the importance of risk/benefit analysis before ordering a CT scan. It is hoped that the providers will not stop here, but will continue to build on the knowledge base and help prevent the unnecessary use of CT scans by conducting an accurate risk/benefit analysis.
Particular strengths and limitations are implicit in this research. A limiting feature of this study is that the findings may not be generalizable as it only included providers in two ED’s in the same system and did not include direct medical care providers from disciplines other than the ED. The knowledge and awareness of other medical specialists who commonly order CT scans may differ greatly from that of ED providers and knowledge among ED providers may differ substantially between geographic regions, academic and non-academic settings, and local and regional medical centers. The data collected was by self-report and may greatly differ from the actual practice of ED providers. Further, the study does not explore in detail the views and opinions of the radiologists that may shed light on how to prevent inappropriate and unnecessary use of the CT scans. The investigation of these views is an important topic for future research. A major strength of this research is the fact that it collected data regarding the reasons why ED providers have particular ordering patterns for CT scans. It also explored the interrelationships of provider behaviors that intersect with CT scan ordering patterns in order to characterize the risk/benefit analysis that providers use when approaching patients who may benefit from modern medical imaging.
CONCLUSION
A majority of the ED providers lack accurate knowledge of the life-time risk of carcinogenesis associated with commonly performed CT scans and order too many unnecessary scans. Awareness and the knowledge of the LAR has an inverse relationship to the provider’s attitude and behavior toward risk/benefit analysis and their discussion of the risks and benefits of a CT scan with the patient. Clinical experience matters and appears to be an important factor influencing provider’s attitude and behavior toward risk/benefit analysis. The providers with greater clinical experience, although likely to lack an accurate knowledge of the LAR, were more likely to consider patient’s radiation dose history, conduct risk/benefit analysis and less likely to order a CT scan unnecessarily.
APPENDIX A
Contributor Information
Savita Puri, Email: Savita_Puri@urmc.rochester.edu, University of Rochester, Strong Memorial Hospital, Department of Imaging Sciences, 601 Elmwood Ave, Box 648, Rochester, NY 14642-8648, (P) 585-273-2436, (F) 585.
Rui Hu, Department of Biostatistics and Computational Biology, 601 Elmwood Ave, Box 648, Rochester, NY 14642-8648
Robin R. Quazi, Mallinckrodt Institute of Radiology, 510 S. Kingshighway Blvd., St Louis, MO 63110
Susan Voci, University of Rochester, Strong Memorial Hospital, Department of Imaging Sciences, 601 Elmwood Ave, Box 648, Rochester, NY 14642-8648.
Peter Veazie, Department Community and Preventive Medicine, 601 Elmwood Ave, Box 648, Rochester, NY 14642-8648.
Robert Block, Department Community and Preventive Medicine, 601 Elmwood Ave, Box 648, Rochester, NY 14642-8648.
References
- 1.UNSCEAR 2000. Sources and Effects of Ionizing Radiation, 2000 Report to the General Assembly with Annexes. New York, NY: United Nations; 2000. [Google Scholar]
- 2.Brenner DJ, Doll R, Goodhead DT, et al. Cancer risks attributable to low doses of ionizing radiation: assessing what we really know. Proc Natl Acad Sci USA. 2003;100:13761–13766. doi: 10.1073/pnas.2235592100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res. 2007;168:1–64. doi: 10.1667/RR0763.1. [DOI] [PubMed] [Google Scholar]
- 4.Cardis E, Vrijheid M, Blettner M, et al. Risk of cancer after low doses of ionizing radiation: retrospective cohort study in 15 countries. BMJ. 2005;331:77. doi: 10.1136/bmj.38499.599861.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, Nuclear and Radiation Studies Board, Division on Earth and Life Studies, National Research Council of the National Academies. Health risks from exposure to low levels of ionizing radiation: BEIRVII Phase 2. Washington, DC: National Academy Press; 2006. [Google Scholar]
- 6.Amis ES, Jr, Butler PF, Applegate KE, et al. American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol. 2007;4:272–284. doi: 10.1016/j.jacr.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Brenner DJ, Hall EJ. Computed tomography: an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 8.Mettler FA, Jr, Thomadsen BR, Bhargavan M, et al. Medical radiation exposure in the U.S. in 2006: preliminary results. Health Phys. 2008;95:502–507. doi: 10.1097/01.HP.0000326333.42287.a2. [DOI] [PubMed] [Google Scholar]
- 9.Wiest PW, Locken JA, Heintz PH, Mettler FA., Jr CT scanning: a major source of radiation exposure. Semin Ultrasound CT MR. 2002;23:402–410. doi: 10.1016/s0887-2171(02)90011-9. [DOI] [PubMed] [Google Scholar]
- 10.Broder J, Bowen J, Lohr J, Babcock A, Yoon J. Cumulative CT exposures in emergency department patients evaluated for suspected renal colic. J Emerg Med. 2007;33:161–168. doi: 10.1016/j.jemermed.2006.12.035. [DOI] [PubMed] [Google Scholar]
- 11.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298(3):317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 12.Sodickson A, Baeyens PF, Andriole KP, Recurrent CT. Cumulative Radiation Exposure and Associated Radiation-induced Cancer Risks from CT of Adults. Radiology. 2009;251:175–184. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 13.Royal HD. Effects of low level Radiation-What is New? Semin Nucl Med. 2008;38(5):392–402. doi: 10.1053/j.semnuclmed.2008.05.006. [DOI] [PubMed] [Google Scholar]
- 14.Inappropriate utilization of diagnostic imaging modalities. 2009 Oct 16; http://www.acr.org.
- 15.Berrington de Gonzalez A, Phil D, Mahadevappa M, Kim K-P. Arch Intern Med. 2009;169(22):2071–207. doi: 10.1001/archinternmed.2009.440. Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations. Neurology. 1994;44:1191–1197. doi: 10.1212/wnl.44.7.1191. [DOI] [PubMed] [Google Scholar]
- 17.Evans RW. Diagnostic testing for the evaluation of headaches. Neurologic Clinics. 1996;14(1):1–26. doi: 10.1016/s0733-8619(05)70240-1. [DOI] [PubMed] [Google Scholar]
- 18.Lee CI, Maims AK, Monico EP. Diagnostic CT scans: Assessment of patients, physicians and radiologist awareness of radiation dose and possible risks. Radiology. 2004;231:393–398. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]
- 19.Guidelines on Diagnosis and Management of Acute Pulmonary Embolism. Eur Heart J. 2000;21:1301–36. doi: 10.1053/euhj.2000.2250. [DOI] [PubMed] [Google Scholar]
- 20.Fadullo PF, Tapson VF. The evaluation of suspected pulmonary embolism. NEJM. 2005;349:1247–56. doi: 10.1056/NEJMcp035442. [DOI] [PubMed] [Google Scholar]
- 21.Morton AS, Iliescu ER, Wilson JWL. Nephrology 1: Investigation and treatment of recurrent kidney stones. CMAJ. 2002:213–18. [PMC free article] [PubMed] [Google Scholar]
- 22.UCLA Medical Group. Practice Guidelines: Ambulatory Radiology. at http://mcoperations.mednet.ucla.edu.
- 23.Berrington de Gonzalez A. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. The Lancet. 2004;363:345–351. doi: 10.1016/S0140-6736(04)15433-0. [DOI] [PubMed] [Google Scholar]
- 24.Shirakar S, Rennie A, Snow M. Doctor’s knowledge of radiation exposure. BMJ. 2003;327:371–2. doi: 10.1136/bmj.327.7411.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ratnapalan S, Bona N, Chandra K. Physician’s perceptions of teratogenic risk associated with radiography and CT during early pregnancy. AJR. 2004;182:1107–1109. doi: 10.2214/ajr.182.5.1821107. [DOI] [PubMed] [Google Scholar]