Abstract
This review discusses the basic knowledge and recent innovation of surgical treatment for scoliosis. Surgical treatment for scoliosis is indicated, in general, for a curve exceeding 45 to 50 degrees by the Cobb’s method on the basis that:
Curves larger than 50 degrees progress even after skeletal maturity.
Curves larger than 60 degrees cause loss of pulmonary function, and much larger curves cause respiratory failure.
Greater the curve progression, the more difficult it is to treat with surgery.
Posterior fusion with instrumentation has been the standard form of surgical treatment for scoliosis. In modern instrumentation systems, more anchors are used to connect the rod and the spine, resulting in better correction and less frequent implant failures. Segmental pedicle screw constructs or hybrid constructs using pedicle screws, hooks, and wires are the trend of today. Anterior instrumentation surgery was once the choice of treatment for thoracolumbar and lumbar scoliosis because better correction could be obtained with shorter fusion levels. But in the recent times, superiority of anterior surgery for the thoracolumbar and lumbar scoliosis has been questioned. Initial enthusiasm for anterior instrumentation for the thoracic curve using video assisted thoracoscopy has faded out.
Keywords: scoliosis, surgery, instrumentation, fusion, fusionless
Review
This review discusses the basic knowledge and recent innovation of surgical treatment for scoliosis. Since relatively little data are obtained regarding outcomes in the long-term or clinical outcomes such as patients’ satisfaction, the techniques are discussed mainly based on the radiological outcomes in the middle-term or sometimes based on short-term follow-up.
Indication of Surgery
Surgical treatment for scoliosis is indicated, in general, for a curve exceeding 45 to 50 degrees by the Cobb’s method on the basis that:
Curves larger than 50 degrees progress even after skeletal maturity. Thoracic curves with a magnitude between 50 and 75 degrees at skeletal maturity (Risser IV or V) progressed by an average of 29.4 degrees over the 40.5 years follow-up period.1 Curves greater than 55 degrees at skeletal maturity (partial or total fusion of the iliac apophyses) progressed by more than 0.5 degrees per year.2 Thoracic curves with an average Cobb angle of 60.5 degrees progressed to 84.5 degrees over the 50 year follow-up period.3
Curves larger than 60 degrees cause loss of pulmonary function, and much larger curves cause respiratory failure. In patients with curves between 60 and 100 degrees, total lung capacity was 68% of the predicted normal values.4 Nearly half of the patients with thoracic curve greater than 80 degrees had shortness of breath, by an average age of 42 years.5 Vital capacity below 45% of the normal value and a Cobb angle greater than 110 degrees were risk factors to develop respiratory failure and earlier death.6
Greater the curve progression, the more difficult it is to treat surgically, with more surgical anchors being necessary, duration of surgery prolonged, increased blood loss, and higher surgical complication rate.
Sometimes patient’s motivation to straighten his/her spine by surgery should be respected, especially for the patient with a gray zone curve and a Cobb angle of 40 to 45 degrees.
Surgical treatment for scoliosis can be divided into fusion surgery and fusionless surgery.
Fusion Surgery
Posterior instrumentation
Posterior fusion with instrumentation has been the standard form of surgical treatment for scoliosis. The first instrumentation system of the modern era was introduced by Paul Harrington.7 In his system, correction force was applied with distraction along the concavity of the curve. In the second generation instrumentation system developed by Cotrel and Dubousset,8 on which all the current systems are modeled, correction was attempted by the rod-rotation maneuver. Segmental spinal instrumentation developed by Luque9 has been widely used mainly for neuromuscular scoliosis. In modern instrumentation systems, more anchors are used to connect the rod and the spine, resulting in better correction and less frequent implant failures.10 Use of segmental pedicle screw constructs (Figs. 1, 2) or hybrid constructs using pedicle screws, hooks, and wires (Figs. 3, 4) are the trend currently.
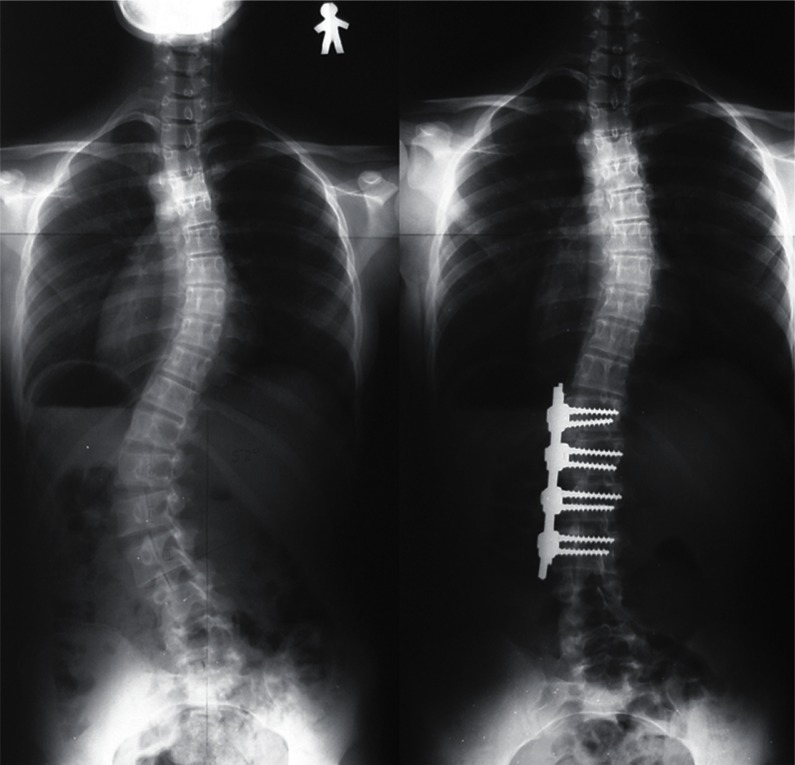
Figure 1.
Segmental pedicle screw constructs. Right thoracic curve between the T5 and T11 was corrected from 68 to 25 degrees.
Figure 2.
Segmental pedicle screw constructs. Lateral radiographs before and after surgery.
Figure 3.
Hybrid constructs using pedicle screws, hooks, and wires. Right thoracic curve between the T5 and T11 was corrected from 70 to 23 degrees.
Figure 4.
Hybrid constructs using pedicle screws, hooks, and wires. Lateral radiographs before and after surgery.
By the segmental pedicle screw concept, the idiopathic thoracic curves of an average of 51 degrees were corrected to 16 degrees (69% correction) with a follow-up for a minimum of five years.11 Although 1.5% of the screws inserted in the thoracic level were malpositioned, they did not cause neurologic complications or adversely affect the long-term results. Using hybrid constructs with hooks, apical sublaminar wires, and pedicle screws, the correction rate was 63% with a follow-up for a minimum of five years.12 No difference was found between the apical sublaminar wires and pedicle screws for initial correction (67.4% vs. 68.1%), loss of correction (4.6% vs. 5.1%), operating time (350 minutes vs. 357 minutes), and satisfaction of the patients, but intraoperative blood loss was more with wires (1791 ml vs. 824 ml) and instrumentation cost was higher with screws (8341 USD vs. 13462 USD).13 Another concern with segmental pedicle screw constructs is that vigorous correction of a major curve is an overcorrection, relative to the flexibility of the upper compensatory curve.14 Generally, the extent of fusion level is determined by the flexibility of the curves demonstrated on the radiographs taken in positions such as supine side bending, fulcrum side bending, traction, or push-prone position.15–17 With segmental pedicle screw technique, to avoid the postoperative shoulder imbalance, fusion has to be extended frequently to the upper thoracic vertebrae, which is not included in the fusion with other techniques.
Anterior Instrumentation
Dwyer and Zielke18,19 were the pioneers of the anterior instrumentation surgery (Figs. 5, 6), which was the choice of treatment for thoracolumbar and lumbar scoliosis because better correction could be obtained with shorter fusion levels. Moreover, anterior instrumentation for the thoracic curve using video assisted thoracoscopy was developed.20 Initial enthusiasm for this surgery due to expectations of decreased postoperative pain and patients’ satisfaction with less operative scar has faded out because the thoracic aorta is at risk if the screw penetrates the cortex on the opposite side,21,22 and disruption of the chest cage during the surgical treatment affects pulmonary function after surgery.23 Thoracic curve can be treated successfully with posterior instrumentation surgery without affecting pulmonary function. For the treatment of single thoracic curve, posterior fusion group demonstrated greater curve correction (62% versus 52%) and greater rib hump correction (51% versus 26%) than the anterior fusion group.24 Recently, superiority of anterior instrumentation surgery for the thoracolumbar and lumbar scoliosis has been questioned as well. In adolescent idiopathic thoracolumbar and lumbar scoliosis, the coronal correction with a minimum of a 2-year follow-up was compatible between the posterior segmental pedicle screw instrumentation group and anterior instrumentation group (68% vs. 67%), but the duration of surgery was significantly shorter (189 minutes vs. 272 minutes) as well as the length of hospital stay (6.2 days vs. 8 days), in the posterior segmental pedicle screw group than in the anterior instrumentation group.25
Figure 5.
Anterior instrumentation surgery. Left thoracolumbar curve between the T11 and L4 was corrected from 52 to 19 degrees (By courtesy of Dr. Tomasz Kotwicki).
Figure 6.
Anterior instrumentation surgery. Lateral radiographs before and after surgery (By courtesy of Dr. Tomasz Kotwicki).
Osteotomy in Combination with Instrumentation
Various osteotomies are conducted in combination with instrumentation. These osteotomies are rarely indicated in the primary surgery of idiopathic scoliosis. For the treatment of relatively mild kyphotic deformities such as Scheuermann’s kyphosis, total facet joint resection, which is called as Smith-Peterson osteotomy,26 or Ponte osteotomy27 are performed. To treat more rigid, local or focal kyphotic deformity, pedicle subtraction osteotomy28 is performed. For severe deformity with limited flexibility including revision surgeries for the previous failed fusion surgery, vertebral column resection29 is sometimes conducted. This is one of the most challenging procedures among the treatment of the spinal deformities.
Fusionless Surgery
Various attempts are being made using fusionless surgery to control growth, to avoid fusion, to delay the timing of the definitive fusion surgery, and to increase the volume of the thorax.
To Control Growth
Epiphysiodesis on the convex side of the deformity with or without instrumentation is a technique that provides gradual progressive correction and arrest of the progression of curves. Some authors found that the arrest of anterior and posterior growth alone are not effective in preventing the progression of deformity in infantile scoliosis.30 On the contrary, others showed that stapling the anterior vertebral spinal growth plates could control worsening of the curve in patients with adolescent idiopathic scoliosis.31 By using newly designed biocompatible shape memory metal alloy staples, 6 of 10 patients with average curve magnitude of 35 degrees were stabilized during the follow-up period which was more than 1-year. To avoid overtreatment of a relatively small, non-progressive curve with this technique, definite and solid criteria for hallmarking a curve as non-progressive should be established first.
To Avoid Fusion
By fusion surgery, segmental motion of the vertebral column is eliminated. To avoid fusion in patients with paralysis, for whom maintaining spinal flexibility and mobility is more desirable, fusionless, vertebral wedge ostetomies are developed for the treatment of progressive paralytic scoliosis of skeletally immature children with spinal cord injury or myelodysplasia.32 A specially designed implant system is used to assist with correction and maintenance of alignment. Twelve weeks following the initial surgery, a second surgery is necessary to remove parts of the implants. This technique may be used for idiopathic scoliosis in future.
For right thoracic curve with idiopathic scoliosis, multiple vertebral wedge osteotomies without fusion (Figs. 7, 8) are performed.33 Twenty patients were treated with osteotomies on an average of 3.6 periapical vertebrae and followed-up for 8.9 years on an average. There were no neurologic complications. For four patients with Risser 0 or I, the average curve magnitude was 74.8 degrees before surgery and 67.5 degrees at the latest follow-up (correction rate was 9.8%), whereas, for 16 patients with Risser IV or V, the curve was 61.3 degrees before surgery and 43.3 degrees at the latest follow-up (correction rate 29.4%).
Figure 7.
Multiple vertebral wedge osteotomy. Right thoracic curve between the T5 and T12 corrected from 56 to 26 degrees.
Figure 8.
Multiple vertebral wedge osteotomy. Lateral radiographs before and after surgery.
Delay of the Timing of Fusion
Fusion surgery at a very young age results in short trunk relative to the extremities. It also affects the development of the lung. To provide correction and maintain it during the growing years, while allowing spinal growth, in patients with early onset scoliosis, technique of instrumentation without fusion or with limited fusion using Harrington rod, Cotrel-Dubousset rod, or Luque rod were developed.34,35 Recently, the technique using Isola dual rod instrumentation has been developed.36 Upper and lower foundations are made bilaterally using hooks or pedicle screws as anchoring devices. Each foundation is connected to a rod, and the rods are connected by a tandem connector, which is placed at the thoracolumbar junction on each side. Lengthening is performed usually every 6 months by distraction inside the tandem connector or between the rod and the tandem connector. Once maximum spinal growth is accomplished, definitive final arthrodesis with instrumentation is performed. Between 1993 and 2001, 23 patients with various etiologies underwent this treatment procedure at an average age of 5.4 years. The average curve magnitude was 82 degrees before surgery, 38 degrees after the initial surgery, and 36 degrees after an average of 6.6 times of lengthening procedures. The length of thoracic and lumbar spine increased by 5 cm at the initial surgery and 4.7 cm in addition, during the lengthening period.
To Increase the Volume of the Thorax
To treat thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis, vertical expandable prosthetic titanium ribs (VEPTR) have been developed.37 After an opening-wedge thoracostomy, the acute correction is stabilized by VEPTR. The device is extended from the cephalad rib to the caudal rib, to the lumbar spine, or to the posterior iliac crest. Following the initial implantation, the devices are expanded at scheduled intervals of four to six months. Twenty-seven patients underwent this procedure at an average age of 3.2 years and were followed-up for 5.7 years. Vital capacity increased significantly; moreover, the deformity due to scoliosis was indirectly corrected from 74 to 49 degrees at the last follow-up.
Conclusions
The indications for surgical treatment of scoliosis, results of the innovative surgical techniques, in terms of, posterior fusion with instrumentation, anterior fusion with instrumentation, and various kinds of fusionless surgery are discussed.
Acknowledgments
We would like to thank Dr. Tomasz Kotwicki for approval to use radiographs of his patient.
Footnotes
Authors’ Contributions
Toru Maruyama conceived of the study, participated in its design and drafted the manuscript. Katsushi Takeshita participated in the design of the study and helped draft the manuscript. All authors read and approved the final manuscript.
Disclosure
The authors report no conflicts of interest.
References
- 1.Weinstein SL, Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:447–55. [PubMed] [Google Scholar]
- 2.Edgar M. The natural history of unfused scoliosis. Orthopaedic. 1987;10:931–9. doi: 10.3928/0147-7447-19870601-12. [DOI] [PubMed] [Google Scholar]
- 3.Weinstein SL, Dolan LA, Spratt KF, et al. Health and function of patients with untreated idiopathic scoliosis. JAMA. 2003;289:559–67. doi: 10.1001/jama.289.5.559. [DOI] [PubMed] [Google Scholar]
- 4.Bjure J, Grimby G, Kasalicky J, et al. Respiratory impairment and airway closure in patients with untreated idiopathic scoliosis. Thorax. 1970;25:451–56. doi: 10.1136/thx.25.4.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Collis DK, Ponseti IV. Long-term follow-up of patients with idiopathic scoliosis not treated surgically. J Bone Joint Surg Am. 1969;51:425–45. [PubMed] [Google Scholar]
- 6.Pehrsson K, Bake B, Larsson S, et al. Lung function in adult idiopathic scoliosis: a 20 year follow up. Thorax. 1991;46:474–8. doi: 10.1136/thx.46.7.474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 1962;44:591–610. [PubMed] [Google Scholar]
- 8.Cotrel Y, Dubousset J, Guillaumat M. New universal instrumentation in spinal surgery. Clin Orthop. 1988;227:10–23. [PubMed] [Google Scholar]
- 9.Luque ER. Segmental spinal instrumentation for correction of scoliosis. Clin Orthop Relat Re. 1982;163:192–8. [PubMed] [Google Scholar]
- 10.Shah SA. Derotation of the spine. Neurosurg Clin N Am. 2007;18:339–45. doi: 10.1016/j.nec.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: More than 5-year follow-up. Spine. 2005;30:1602–9. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 12.Asher MA, Lai SM, Burton D, et al. Safety and efficacy of Isola instrumentation and arthrodesis for adolescent idiopathic scoliosis: two-to 12-year follow-up. Spine. 2004;29:2013–23. doi: 10.1097/01.brs.0000138275.49220.81. [DOI] [PubMed] [Google Scholar]
- 13.Cheng I, Kim YJ, Gupta MC, et al. Apical sublaminar wires versus pedicle screws-which provides better results for surgical correction of adolescent idiopathic scoliosis? Spine. 2005;30:2104–12. doi: 10.1097/01.brs.0000179261.70845.b7. [DOI] [PubMed] [Google Scholar]
- 14.Winter RB, Lonstein JE, Denis F. How much correction is enough? Spine. 2007;32:2641–3. doi: 10.1097/BRS.0b013e31815a5207. [DOI] [PubMed] [Google Scholar]
- 15.Vaughan JJ, Winter RB, Lonstein LE. Comparison of the use of spine bending and traction radiographs in the selection of the fusion area in adolescent idiopathic scoliosis. Spine. 1996;21:2469–73. doi: 10.1097/00007632-199611010-00012. [DOI] [PubMed] [Google Scholar]
- 16.Cheung KMC, Luk KDK. Prediction of correction of scoliosis with use of the fulcrum bending radiograph. J Bone Joint Surg Am. 1997;79:1144–50. doi: 10.2106/00004623-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Vedantam R, Lenke LG, Bridwell KH, et al. Comparison of push-prone and lateral-bending radiographs for predicting postoperative coronal alignment in thoracolumbar scoliotic curves. Spine. 2000;25:76–81. doi: 10.1097/00007632-200001010-00014. [DOI] [PubMed] [Google Scholar]
- 18.Dwyer AF, Newton NC, Sherwood AA. An anterior approach to scoliosis. A preliminary report. Clin Orthop Relat Re. 1969;62:192–202. [PubMed] [Google Scholar]
- 19.Zielke K, Stunkat R, Beaujean F. Ventrale derotations-spondylodesis. Arch Orthop Unfallchir. 1976;85(3):257–77. doi: 10.1007/BF00415189. [DOI] [PubMed] [Google Scholar]
- 20.Picetti GD, III, Pang D, Bueff HU. Thoracoscopic techniques for the treatment of scoliosis: early results in procedure development. Neurosurgery. 2002;51:978–84. doi: 10.1097/00006123-200210000-00023. [DOI] [PubMed] [Google Scholar]
- 21.Sucato DJ, Kassab F, Dempsey M. Analysis of screw placement relative to the aorta and spinal canal following anterior instrumentation for thoracic idiopathic scoliosis. Spine. 2004;29:554–9. doi: 10.1097/01.brs.0000106495.91477.92. [DOI] [PubMed] [Google Scholar]
- 22.Maruyama T, Takeshita K, Nakamura K, et al. Spatial relations between the vertebral body and the thoracic aorta in adolescent idiopathic scoliosis. Spine. 2004;29:2067–9. doi: 10.1097/01.brs.0000138409.14577.f0. [DOI] [PubMed] [Google Scholar]
- 23.Kim YJ, Lenke LG, Bridwell KH, et al. Pulmonary function in adolescent idiopathic scoliosis relative to the surgical procedure. J Bone Joint Surg Am. 2005;87:1534–41. doi: 10.2106/JBJS.C.00978. [DOI] [PubMed] [Google Scholar]
- 24.Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke type I adolescent idiopathic scoliosis curves. Spine. 2005;30:1859–66. doi: 10.1097/01.brs.0000174118.72916.96. [DOI] [PubMed] [Google Scholar]
- 25.Hee HT, Yu ZR, Wong HK. Comparison of segmental pedicle screw instrumentation versus anterior instrumentation in adolescent idiopathic thoracolumbar and lumbar spine. Spine. 2007;32:1533–42. doi: 10.1097/BRS.0b013e318067dc3d. [DOI] [PubMed] [Google Scholar]
- 26.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. J Bone Joint Surg. 1945;27:1–11. [PubMed] [Google Scholar]
- 27.Geck MJ, Macagno A, Ponte A, et al. The Ponte procedure. Posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech. 2007;20:586–93. doi: 10.1097/BSD.0b013e31803d3b16. [DOI] [PubMed] [Google Scholar]
- 28.Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop. 1985;194:142–52. [PubMed] [Google Scholar]
- 29.Suk SI, Kim JH, Kim WJ, et al. Posterior vertebral column resection for severe spinal deformities. Spine. 2002;27:2374–82. doi: 10.1097/00007632-200211010-00012. [DOI] [PubMed] [Google Scholar]
- 30.Marks DS, Iqbal MJ, Thompson AG, et al. Convex spinal epiphysiodesis in the management of progressive infantile idiopathic scoliosis. Spine. 1996;21:1884–8. doi: 10.1097/00007632-199608150-00010. [DOI] [PubMed] [Google Scholar]
- 31.Betz RR, Kim J, D’Andrea LP, et al. An innovative technique of vertebral body stapling for the treatment of patients with adolescent idiopathic scoliosis: A feasibility, safety, and utility study. Spine. 2003;28:S255–65. doi: 10.1097/01.BRS.0000092484.31316.32. [DOI] [PubMed] [Google Scholar]
- 32.Guille JT, Betz RR, Balsara RK, et al. The feasibility, safety, and utility of vertebral wedge osteotomies for the fusionless treatment of paralytic scoliosis. Spin. 2003;28:S266–74. doi: 10.1097/01.BRS.0000092485.40061.ED. [DOI] [PubMed] [Google Scholar]
- 33.Maruyama T, Kitagawa T, Takeshita K, et al. Fusionless surgery for scoliosis: 2–17 year radiographic and clinical follow-up. Spine. 2006;31:2310–5. doi: 10.1097/01.brs.0000238971.05671.d5. [DOI] [PubMed] [Google Scholar]
- 34.Moe JH, Kharrat K, Winter RB, et al. Harrington instrumentation without fusion plus external orthotic support for the treatment of difficult curvature problems in young children. Clin Orthop. 1984;185:35–45. [PubMed] [Google Scholar]
- 35.Grivas TB, Webb JK, Burwell RG. The effects of epiphysiodesis and rodding for early onset scoliosis. J Bone Joint Surg B. 1991;(Suppl 1):32–3. [Google Scholar]
- 36.Akbarnia BA, Marks DS, Boachie-Adjei O, et al. Dual growing rod technique for the treatment of progressive early-onset scoliosis. Spine. 2005;30:546–57. doi: 10.1097/01.brs.0000175190.08134.73. [DOI] [PubMed] [Google Scholar]
- 37.Campbell RM, Smith MD, Mayes TC, et al. The effect of opening wedge thoracostomy on thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg Am. 2004;86:1659–74. doi: 10.2106/00004623-200408000-00009. [DOI] [PubMed] [Google Scholar]