Abstract
Introduction
Controversy exists concerning the importance of operative time on patient outcomes. It is unclear whether faster is better or haste makes waste or similarly whether slower procedures represent a safe, meticulous approach or inexperienced dawdling. The objective of the present study was to determine the effect of operative time on 30-day outcomes in laparoscopic surgery.
Methods
Patients who underwent laparoscopic general surgery procedures (colectomy, cholecystectomy, Nissen fundoplication, inguinal hernia, and gastric bypass) from the ACS-NSQIP 2005–2008 participant use file were identified. Exclusion criteria were defined a priori to identify same-day admission, elective procedures. Operative time was divided into deciles and summary statistics were analyzed. Univariate analyses using a Cochran-Armitage test for trend were completed. The effect of operative time on 30-day morbidity was further analyzed for each procedure type using multivariate regression controlling for case complexity and additional patient factors. Patients within the highest deciles were excluded to reduce outlier effect.
Results
A total of 76,748 elective general surgical patients who underwent laparoscopic procedures were analyzed. Univariate analyses of deciles of operative time demonstrated a statistically significant trend (p \ 0.0001) toward increasing odds of complications with increasing operative time for laparoscopic colectomy (n = 10,135), cholecystectomy (n = 37,407), Nissen fundoplication (n = 4,934), and gastric bypass (n = 17,842). The trend was not found to be significant for laparoscopic inguinal hernia repair (n = 6,430; p = 0.14). Multivariate modeling revealed the effect of operative time to remain significant after controlling for additional patient factors.
Conclusion
Increasing operative time was associated with increased odds of complications and, therefore, it appears that speed may matter in laparoscopic surgery. These analyses are limited in their inability to adjust for all patient factors, potential confounders, and case complexities. Additional hierarchical multivariate analyses at the surgeon level would be important to examine this relationship further.
Keywords: Operative time, Laparoscopic surgery, Outcome
The importance of operative time on patient outcomes in laparoscopic surgery remains controversial. Operative time is the result of a complex interaction of patient and provider factors and, at present, there is a paucity of data to examine how the length of a procedure impacts outcome in laparoscopic surgery.
It is not known whether longer operative times represent meticulous attention to technique and thereby would reduce complications or whether a longer duration of surgery indicates intraoperative difficulties that would predict increased postoperative complications. Similarly, it is not clear whether shorter operative times represent advanced skills and a smooth intraoperative course or potentially less attention to detail that may place a patient at risk for complications.
With increasing importance being placed on operative time to track performance and allocate resources, a better understanding of the relative importance of operative time on the quality of patient care is needed. The objective of the present study was to determine the effect of operative time on 30-day outcomes in elective laparoscopic general surgery procedures.
Methods
Study design
The American College of Surgeons—National Surgery Quality Improvement Program (ACS-NSQIP) is a prospective, multi-institutional, cohort study for collecting rich clinical data on patients undergoing surgical procedures in private sector hospitals. Data are collected on preoperative, intraoperative, and postoperative variables, including 30-day outcomes. ACS-NSQIP methodology has been described in detail previously [1–5].
Patient population
Patients undergoing elective laparoscopic general surgery procedures from the ACS-NSQIP 2005–2008 participant use file were identified using current procedural terminology (CPT) codes. Within this validated data source, patients who underwent laparoscopic segmental colectomy without colostomy (CPTs = 44204, 44205, 44207), laparoscopic Roux-en-Y gastric bypass (LRYGB) (CPTs = 43644, 43645), laparoscopic cholecystectomy (CPTs = 47562, 47563, 47564), laparoscopic inguinal hernia repair (CPT = 49650), and laparoscopic Nissen fundoplication (CPT = 43280) were included for analysis.
Exclusion criteria were defined a priori to identify only same-day admission, elective cases within the dataset. Patients who were identified as having an emergency procedure, ASA class 4 or 5, admission date not equal to procedure date, admission from another healthcare facility, wound classification of IV (dirty or infected), sepsis or SIRS, COPD, chronic steroid use, disseminated cancer, ascites, recorded DNR status, 10% weight loss in previous 6 months (except in bariatric patients), radiation therapy, or known bleeding disorder were excluded. Cases in which any component of operative time was missing were excluded from the analysis (7 patients).
Variable selection
NSQIP collects data on five time intervals surrounding surgical procedures: duration from anesthesia start to surgery start; duration from surgery stop to anesthesia stop; duration that was in the operating room; duration of anaesthesia; and total operative time (“skin to skin” time). Total operative time measured in minutes was used for analysis. Variables for total number of complications were created for each patient. This included the aggregate sum of any surgical complication recorded in the NSQIP database during the 30-day follow-up period.
Statistical analysis
Summary statistics were performed to define the study population. By procedure type, the patients were divided by deciles of total operative time. The 30-day outcomes were measured by presence or absence of a complication and number of complications per procedure. Number of complications per procedure was plotted against deciles of operative time for each procedure type to reveal trends. Univariate analyses using a Cochran-Armitage test for trend were then completed to assess f o r statistical significance.
Multivariate regression was used to assess the effect of operative time on 30-day outcome while controlling for additional available patient factors in the database. Stratified by procedure type, variables that may confound or modify the relationship of operative time on number of postoperative complications were considered. A forward stepwise approach was used to build the regression models. The dependent variable was the number of complications per patient, and the independent variables are the operative time and additional preoperative patient characteristics. Any independent variables that had a univariate relationship with complication rates at the p \ 0.2 level of significance w e r e included in the model as potential confounders. Only variables that remained significant at p \ 0.05 within the models were included.
For the regression modeling, patients within the tenth deciles of operative time were excluded to reduce potential outlier effects. The models were assessed for calibration using the Hosmer-Lemeshow goodness-of-fit test and discrimination using the c-statistic. Models are presented in tables with adjusted odds ratio, 95% confidence interval, and p value. Sensitivity analyses using operative time as both a continuous variable and as deciles were conducted. All analyses were performed using STATA v9.0 (Stata Corp, College Station, TX).
Results
The study population consisted of 76,748 patients who underwent elective laparoscopic general surgical procedures. This included 17,842 LRYGBs, 10,135 laparoscopic colectomies, 37,407 laparoscopic cholecystectomies, 4,934 laparoscopic Nissen fundoplications, and 6,430 laparoscopic inguinal hernia repairs. Demographic and patient characteristics are listed in Table 1. Percentage of patients with cardiovascular, pulmonary, renal comorbidities, and diabetes was highest in the LRYGB group.
Table 1.
Patient characteristics
| Preoperative characteristic |
Laparoscopic Roux-en-Y gastric bypass |
Laparoscopic colectomy |
Laparoscopic cholecystectomy |
Laparoscopic Nissen fundoplication |
Laparoscopic inguinal hernia |
|---|---|---|---|---|---|
| Number | 17,842 | 10,135 | 37,407 | 4,934 | 6,430 |
| Age (year) | 44.14 ± 11.07 | 60.83 ± 13.58 | 47.22 ± 16.18 | 52.34 ± 14.72 | 51.74 ± 15.56 |
| Gender | |||||
| Male | 3,320 (18.63) | 4,899 (48.34) | 8,813(23.56) | 1,894 (38.39) | 5,949 (92.53) |
| Female | 14,504 (81.37) | 5,236 (51.66) | 28,594 (76.44) | 3,040 (61.61) | 480 (7.47) |
| BMI (kg/m2) | 47.20 ± 8.34 | 28.08 ± 6.32 | 30.15 ± 8.15 | 29.37 ± 6.16 | 26.28 ± 4.98 |
| Smoke | 2,211 (12.4) | 1,524 (15.04) | 7,140 (19.09) | 731 (14.82) | 1,165 (18.12) |
| Alcohol [ 2/d | 42 (0.24) | 365 (3.6) | 392 (1.05) | 96 (1.95) | 231 (3.59) |
| ASA class | |||||
| 1 | 96 (0.54) | 577 (5.69) | 6,266 (16.75) | 270 (5.47) | 1,909(29.69) |
| 2 | 5,872 (32.94) | 6,657 (65.68) | 24,315 (65) | 3,392 (68.75) | 3,742 (58.2) |
| 3 | 11,856 (66.52) | 2,901 (28.62) | 6,826 (18.25) | 1,272 (25.78) | 779 (12.12) |
| Diabetes | 4,822 (27.05) | 1,053 (10.39) | 3,159 (8.44) | 245 (4.97) | 252 (3.92) |
| Cardiovascular Comorbidities | 9,404 (52.76) | 4,657 (45.95) | 11,480 (30.69) | 1,789 (36.26) | 1,681 (26.14) |
| Pulmonary Comorbidities | 5,217 (29.27) | 676 (6.67) | 2,028 (5.42) | 524 (10.6) | 141 (2.19) |
| Renal comorbidities | 13 (0.07) | 14 (0.14) | 127 (0.34) | 2 (0.04) | 11 (0.17) |
BMI body mass index, ASA American Society of Anesthesiologists
Cardiovascular comorbidities included a history of myocardial infarction, congestive heart failure, angina, hypertension requiring medications, peripheral vascular disease, or stroke. Respiratory comorbidities included history of dyspnea, previous requirement of ventilator, pneumonia. Patients with a diagnosis of COPD were excluded. Renal comorbidities include renal failure and dialysis
Data are numbers with percentages in parentheses or means ± standard deviations
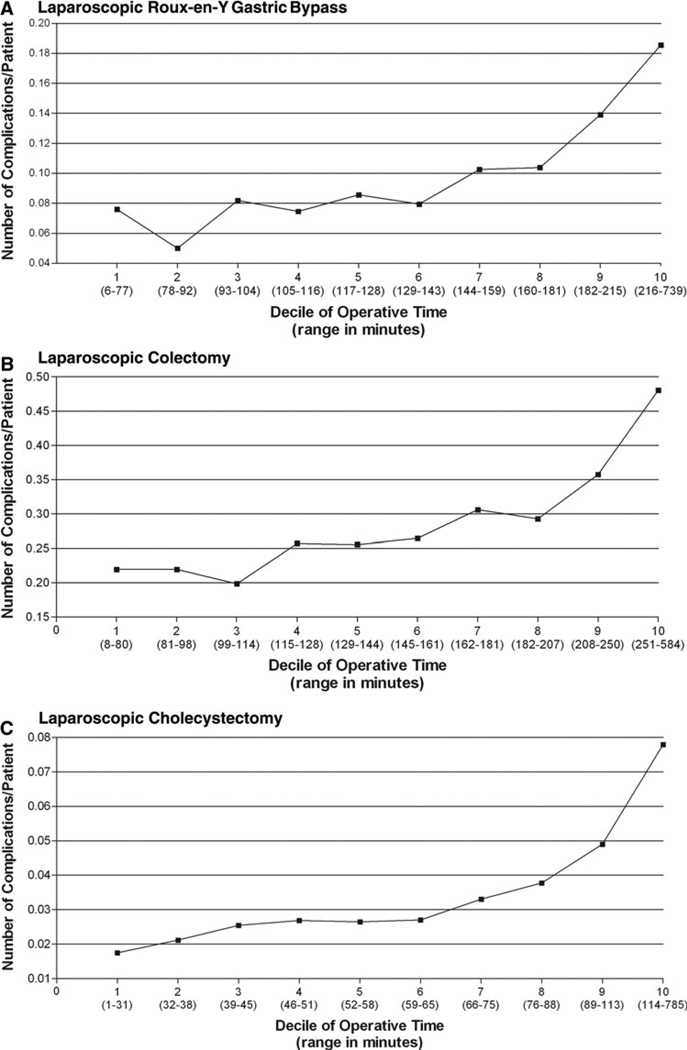
The operative times (mean ± SD) and complication rates for were 140 ± 57.14 min and 6.63% for LRYGB, 159.89 ± 64.10 min and 13.7% for laparoscopic colectomy, 63.14 ± 33.73 min and 2.64% for laparoscopic cholecystectomy, 134.45 ± 59.73 min and 3.97% for laparoscopic Nissen fundoplication, and 67.06 ± 33.71 min and 1.62% for laparoscopic inguinal hernia (Table 2). Univariate analyses of deciles of operative time using the Cochran-Armitage test demonstrated a statistically significant trend (p \ 0.001) toward increasing odds of complications with increasing operative time for LRYGB, laparoscopic colectomy, laparoscopic cholecystectomy, and laparoscopic Nissen fundoplication. The trend was not found to be significant for laparoscopic inguinal hernia repair (p = 0.14). Figure 1 demonstrates number of complications per procedure plotted against deciles of operative time for each procedure type.
Table 2.
Operative times and outcomes
| Laparoscopic Roux-en-Y gastric bypass |
Laparoscopic colectomy |
Laparoscopic cholecystectomy |
Laparoscopic Nissen fundoplication |
Laparoscopic inguinal hernia |
|
|---|---|---|---|---|---|
| Operative time (min), mean ± SD | 140 ± 57.14 | 159.89 ± 64.1 | 63.14 ± 33.73 | 134.45 ± 59.73 | 67.06 ± 33.71 |
| Operative time by decile (min), range (mean) | |||||
| 1 | 6–77 (64.17) | 8–80 (66.08) | 1–31 (25.16) | 5–72 (55.74) | 6–32 (25.86) |
| 2 | 78–92 (85.47) | 81–98 (90.52) | 32–38 (35.16) | 73–87 (80.55) | 33–40 (36.73) |
| 3 | 93–104 (98.62) | 99–114 (106.76) | 39–45 (42.07) | 88–100 (94.36) | 41–47 (44.03) |
| 4 | 105–116 (110.57) | 115–128 (121.51 | 46–51 (48.57) | 101–112 (106.5) | 48–54 (50.93) |
| 5 | 117–128 (122.27) | 129–144 (136.47) | 52–58 (54.89) | 113–125 (118.59) | 55–60 (57.37) |
| 6 | 129–143 (135.9) | 145–161 (152.8) | 59–65 (61.92) | 126–138 (132.2) | 61–69 (65.03) |
| 7 | 144–159 (151.12) | 162–181 (171.23) | 66–75 (70.04) | 139–154 (146) | 70–78 (73.74) |
| 8 | 160–181 (169.50) | 182–207 (193.87) | 76–88 (81.58) | 155–175 (164.57) | 79–90 (84.34) |
| 9 | 182–215 (196.79) | 208–250 (227.21) | 89–113 (99.19) | 176–210 (191.32) | 91–110 (99.62) |
| 10 | 216–739 (262.73) | 251–584 (298.84) | 114–785 (147.27) | 211–790 (261.23) | 111–519 (139.54) |
| Complication rate | 6.63% | 13.7% | 2.64% | 3.97% | 1.62% |
| No. of complications per patient, mean ± SD | 0.098 ± 0.45 | 0.228 ± 0.75 | 0.026 ± 0.16 | 0.06 ± 0.37 | 0.019 ± 0.16 |
SD standard deviation
Fig. 1.
Average number of complications per patient within each decile vs. deciles of operative time
Multivariate regression
Multivariate regression modeling revealed that increasing operative time remained significantly associated with 30-day morbidity when additional patient factors were controlled for patients who underwent laparoscopic RYGB, colectomy, cholecystectomy, and Nissen fundoplication but not in patients who underwent laparoscopic inguinal hernia repair. The regression models are presented in Table 3a–e.
Table 3.
Multivariate regression models (10th decile of patients excluded)
| Variable | OR | Confidence limits* |
p value |
|---|---|---|---|
| (a) Laparoscopic Roux-en-Y gastric bypassa | |||
| Operative time | 1.005 | (1.003, 1.006) | \0.001 |
| Age (yr) | 1.013 | (1.006, 1.019) | \0.001 |
| Dialysis | 10.047 | (2.807, 35.958) | \0.001 |
| BMI | 1.012 | (1.005, 1.02) | 0.002 |
| CHF | 12.8 | (1.778, 92.164) | 0.011 |
| Hypertension | 1.181 | (1.024,1.362) | 0.023 |
| (b) Laparoscopic colectomyb | |||
| Operative time | 1.004 | (1.003, 1.005) | \0.001 |
| ASA | 1.421 | (1.237, 1.632) | \0.001 |
| Smoking | 1.357 | (1.156, 1.594) | \0.001 |
| Dyspnea | 1.323 | (1.058, 1.655) | 0.014 |
| BMI | 1.011 | (1.001, 1.021) | 0.025 |
| Hypertension | 1.157 | (1.014, 1.32) | 0.030 |
| (c) Laparoscopic cholecystectomyc | |||
| Operative time | 1.011 | (1.008, 1.014) | \0.001 |
| Age (yr) | 1.013 | (1.009, 1.018) | \0.001 |
| ASA | 1.342 | (1.130, 1.594) | 0.001 |
| BMI | 1.015 | (1.007, 1.024) | 0.001 |
| CHF | 3.849 | (1.137, 13.036) | 0.03 |
| (d) Laparoscopic Nissen fundoplicationd | |||
| Operative time | 1.007 | (1.003, 1.011) | 0.001 |
| Age (yr) | 1.028 | (1.016, 1.04) | \0.001 |
| (e) Laparoscopic inguinal herniae | |||
| Operative time | 1.009 | (0.997, 1.019) | 0.059 |
| Age (yr) | 1.021 | (1.007, 1.036) | 0.004 |
| Sex | 0.45 | (0.246, 0.822) | 0.009 |
| PVD | 4.581 | (1.03, 20.384) | 0.046 |
c-index = 0.604, n = 16,129. Hosmer-Lemeshow p = 0.486
c-index = 0.594, n = 9,168. Hosmer-Lemeshow p = 0.409
c-index = 0.614, n = 34,531. Hosmer-Lemeshow p = 0.41
c-index = 0.638, n = 4,934. Hosmer-Lemeshow p = 0.159
c-index = 0.641, n = 5,780. Hosmer-Lemeshow p = 0.0017
95% Wald confidence limits.
BMI body mass index; ASA American Society of Anesthesiologists Classification (3 vs. 1 or 2); CHF congestive heart failure; PVD peripheral vascular disease
For patients undergoing LRYGB (Table 3a), operative time and five preoperative variables (age, dialysis, BMI, CHF, and hypertension) were found to be significantly associated with increased 30-day postoperative complications. For the laparoscopic colectomy patients (Table 3b), the model included operative time, ASA class, smoking, dyspnea, body mass index (BMI), and hypertension. Within the laparoscopic cholecystectomy model (Table 3c), operative time and age, ASA, BMI, and CHF were included. Only operative time and age were found to be significantly associated with increased odds of 30-day postoperative complications in the laparoscopic Nissen fundoplication model (Table 3d). Operative time was not found to be significant in the laparoscopic inguinal hernia model (Table 3e). Hosmer-Lemeshow goodness-of-fit testing was not significant for the LRYGB, laparoscopic colectomy, laparoscopic cholecystectomy, and laparoscopic inguinal hernia models but was significant for the laparoscopic Nissen fundoplication model.
In addition, the effect of operative time on postoperative wound infection rates was examined within a multivariate model. Increasing operative time was independently associated with increased wound infection rates for LRYGB, laparoscopic colectomy, and laparoscopic cholecystectomy. The impact of level of training of surgical assistant also was explored. The odds of having a trainee as an assistant increased with each decile of operative time, although this trend was significant only within the laparoscopic colectomy group.
When operative time was modeled as both a continuous variable and as deciles during sensitivity analysis, the effect of operative time remained significant. Furthermore, the findings did not change when the dependent variable was substituted with any versus no complications as the outcome of interest. When comparable, open RYGB, colectomy, and cholecystectomy patients were analyzed, similar results were found (data not shown).
Discussion
In this analysis of 76,748 patients, increasing operative time was independently associated with increased odds of complications in several laparoscopic elective general surgical procedures, including RYGB, colectomy, cholecystectomy, and Nissen fundoplication. This relationship was found to remain statistically significant after risk adjustment to control for additional patient factors.
Several authors have examined the relationship of operative time on outcome in general surgery patients with conflicting findings. In a recent study by Scheer et al. [6], the relationship of operative time on outcome for patients who underwent laparoscopic colon surgery was examined. The authors found no significant association, although identified that patients with procedures longer than 270 minutes did have increased number of complications. This time length corresponds to the highest decile of procedure length in our study, which also was noted to have increased complications. Furthermore, we identified the trend toward increased odds of complications in laparoscopic colectomy patients to be persistent even after excluding the highest decile from our analysis to reduce outlier effect.
Using ACS-NSQIP data, Campbell et al. [7], demonstrated that hospitals that were high outliers for surgical site infections had longer surgery times compared with those hospitals that had shorter operative times; this finding is consistent with our results. In our analysis, we also were able to identify a statistically significant positive association between procedure length and wound infection rates for LRYGB, laparoscopic colectomy, and laparoscopic cholecystectomy.
Sandblom et al. examined patient outcomes in open hernia repair and identified shorter procedure time (\20 min) as being associated with increased risk of reoperation, recurrence, and persistent pain [8]. Although we could not examine these specific endpoints, our findings do contradict their conclusion because we show that shorter operations are associated with lower complication rates. In fact for any procedure type, we could not identify a negative effect of shorter procedure duration on 30-day patient outcome.
Other studies have found no relationship between operative time and patient outcome. Liverani et al. [9] performed a review of 250 open “clean” and “clean-contaminated” abdominal surgeries and found no association between length of procedure and number of septic complications, anastomotic dehiscence, or length of stay. Dexter et al. [10], reviewed complication rates in laparoscopic cholecystectomy lasting [180 min (32 patients) to those lasting\180 min (379 patients). The complication rates were found to be 9% and 3.8%, respectively, although this difference failed to achieve statistical significance. Both studies were retrospective, single-institution case series and lacked large sample sizes required to detect differences in procedures with relatively low complication rates.
Our study is unique in that we have identified a significant association between increased procedure time and number of complications across many different elective laparoscopic procedures, using data from 211 hospitals and including 76,748 cases. The low complication rate within the laparoscopic hernia group likely contributed to failure of operative time to achieve statistical significance in this group of patients. While we have identified an association, a more complete appreciation of how procedure duration influences patient outcome is needed. This will require an understanding of all factors that may contribute to operative time, including surgical expertise, case complexity, presence of learners, extent of teaching, interaction of surgical teams, and more.
This study has several important limitations. An ideal study perhaps would compare the outcomes of faster and slower surgeons rather than compare the outcomes from fast or slow cases. However, surgeon level data were not available. Recognizing that there are likely other factors beyond the individual surgeon that contribute to operative time, additional hierarchical data are needed to further delineate the relationship between procedure time and outcome. Similarly, because hospital effects can have an impact on operative time, multilevel modeling, including hospital level data, also could be important but was not available. Our analysis was limited by the variables available within the ACS-NSQIP database, and so we could not adjust for all potentially important patient factors and confounders. In addition, cases were determined by CPT codes, and variability of coding techniques and types of procedures within specific codes could not be taken into account. We also were not able to account for cases that were converted to open, which may be another potential source of information bias. Furthermore, our follow-up was limited to complications occurring within 30 days of the procedure.
Our results indicated that the number of complications that a patient experiences increases with increasing operative time for several laparoscopic general surgery procedures. For this reason, operative time does seem to matter in laparoscopic surgery and may be considered a potentially important determinant of patient outcome. To further characterize and quantify the relative importance of operative time in laparoscopic procedures, additional hierarchical multivariate modeling with surgeon level data is required.
Footnotes
Presented at the 12th WCES, April 14–17, 2010, National Harbor, MD.
Disclosures Drs. Timothy Jackson, Jeffrey Wannares, R. Todd Lancaster, David Rattner, and Matthew Hutter have no conflicts of interest or financial ties to disclose.
Contributor Information
Timothy D. Jackson, Department of Surgery, Division of General and Gastrointestinal Surgery, Massachusetts General Hospital, 15 Parkman St., WACC 460, Boston, MA 02114, USA The Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, MA, USA; Department of Surgery, University of Toronto, Toronto, ON, Canada.
Jeffrey J. Wannares, The Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, MA, USA
R. Todd Lancaster, Department of Surgery, Division of General and Gastrointestinal Surgery, Massachusetts General Hospital, 15 Parkman St., WACC 460, Boston, MA 02114, USA; The Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, MA, USA.
David W. Rattner, Department of Surgery, Division of General and Gastrointestinal Surgery, Massachusetts General Hospital, 15 Parkman St., WACC 460, Boston, MA 02114, USA
Matthew M. Hutter, Email: mhutter@partners.org, Department of Surgery, Division of General and Gastrointestinal Surgery, Massachusetts General Hospital, 15 Parkman St., WACC 460, Boston, MA 02114, USA; The Codman Center for Clinical Effectiveness in Surgery, Massachusetts General Hospital, Boston, MA, USA.
References
- 1.Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Jr, Fink AS, Mentzer RM, Jr, Steeger JE. The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg. 2007;204(6):1089–1102. doi: 10.1016/j.jamcollsurg.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 2.Khuri SF, Daley J, Henderson W, Hur K, Gibbs JO, Barbour G, Demakis J, Irvin G, 3rd, Stremple JF, Grover F, McDonald G, Passaro E, Jr, Fabri PJ, Spencer J, Hammermeister K, Aust JB. Risk adjustment of the postoperative mortality rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997;185(4):315–327. [PubMed] [Google Scholar]
- 3.Daley J, Khuri SF, Henderson W, Hur K, Gibbs JO, Barbour G, Demakis J, Irvin G, III, Stremple JF, Grover F, McDonald G, Passaro E, Jr, Fabri PJ, Spencer J, Hammermeister K, Aust JB, Oprian C. Risk adjustment of the postoperative morbidity rate for the comparative assessment of the quality of surgical care: results of the National Veterans Affairs Surgical Risk Study. J Am Coll Surg. 1997;185(4):328–340. [PubMed] [Google Scholar]
- 4.Daley J, Forbes MG, Young GJ, Charns MP, Gibbs JO, Hur K, Henderson W, Khuri SF. Validating risk-adjusted surgical outcomes: site visit assessment of process and structure National VA Surgical Risk Study. J Am Coll Surg. 1997;185(4):341–351. [PubMed] [Google Scholar]
- 5.Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA, Jr, Fink AS, Mentzer RM, Jr, Neumayer L, Hammermeister K, Mosca C, Healey N. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008;248(2):329–336. doi: 10.1097/SLA.0b013e3181823485. [DOI] [PubMed] [Google Scholar]
- 6.Scheer A, Martel G, Moloo H, Sabri E, Poulin EC, Mamazza J, Boushey RP. Laparoscopic colon surgery: does operative time matter? Dis Colon Rectum. 2009;52(10):1746–1752. doi: 10.1007/DCR.0b013e3181b55616. [DOI] [PubMed] [Google Scholar]
- 7.Campbell DA, Jr, Henderson WG, Englesbe MJ, Hall BL, O’Reilly M, Bratzler D, Dellinger EP, Neumayer L, Bass BL, Hutter MM, Schwartz J, Ko C, Itani K, Steinberg SM, Siperstein A, Sawyer RG, Turner DJ, Khuri SF. Surgical site infection prevention: the importance of operative duration and blood transfusion—results of the first American College of Surgeons-National Surgical Quality Improvement Program best practices initiative. J Am Coll Surg. 2008;207(6):810–820. doi: 10.1016/j.jamcollsurg.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 8.Sandblom G, Sevonius D, Stael von Holstein C. Impact of operative time and surgeon satisfaction on the long-term outcome of hernia repair. Hernia. 2009;13(6):581–583. doi: 10.1007/s10029-009-0527-9. [DOI] [PubMed] [Google Scholar]
- 9.Liverani A, Chiarot M, Bezzi M, Angelini L. Is surgery duration really a complication factor? Minerva Chir. 1994;49(9):747–750. [PubMed] [Google Scholar]
- 10.Dexter SP, Martin IG, Marton J, McMahon MJ. Long operation and the risk of complications from laparoscopic cholecystectomy. Br J Surg. 1997;84(4):464–466. [PubMed] [Google Scholar]