Abstract
The current study examined the relationships among marijuana dependence, a theoretical model of condom use intentions, and subsequent condom use behavior in justice-involved adolescents. Participants completed baseline measures of prior sexual and substance use behavior. Of the original 720 participants, 649 (90.13 %) completed follow-up measures 6 months later. There were high levels of marijuana use (58.7 % met criteria for dependence) and risky sexual behavior among participants. Baseline model constructs were associated with condom use intentions, and intentions were a significant predictor of condom use at follow-up. Marijuana dependence did not significantly influence the relationships between model constructs, nor did it moderate the relationship of model constructs with subsequent condom use. Findings suggest that the theoretical model of condom use intentions is equally valid regardless of marijuana dependence status, suggesting that interventions to reduce sexual risk behavior among both marijuana dependent and non-dependent justice-involved adolescents can be appropriately based on the model.
Keywords: Justice-involved adolescents, Risky sexual behavior, Marijuana dependence, STIs, Theory of planned behavior
Introduction
Every year 19 million new cases of sexually transmitted infections (STI) are diagnosed, with the majority occurring in young adults aged 15–24 [1] who represent one fourth of the population, but acquire nearly half of all new STIs [2]. Young people involved with the juvenile justice system have higher rates of risky sexual behavior, lifetime and recent sexual partners, and illicit drug use than their non-justice-involved peers, and are thus at even greater risk for acquiring STIs including HIV/AIDS [3–7]. One factor that may contribute to risky sexual behavior is substance use [8]. Alcohol use has received the most attention in the literature regarding this relationship and, thus far, the outcomes of this work are inconclusive [5, 9–15]. Our own work among justice-involved adolescents found a negative relationship such that those who drank prior to a sexual event were less likely to use a condom [16], although a negative relationship between these two factors is not always found [13].
Marijuana is the most commonly used illicit drug among justice-involved adolescents and has been the most widely used illicit drug in the last quarter century [17]. Although marijuana use is far more common than alcohol use in the juvenile-justice population, the degree to which marijuana use may influence justice-involved adolescents’ sexual risk behaviors, and related cognitions, is far less studied. Thus the relationship between these two risk behaviors remains unclear. Early marijuana use is related to earlier sexual initiation, sexual intercourse with casual partners, increased number of sexual partners, and decreased condom use [18–25]. The influence of marijuana use on sexual risk behavior both at a global level (i.e. general tendency to use marijuana or use condoms) and at an event level (i.e. marijuana and condom use at the time of a particular event) is complex [26]. Some research supports positive associations between marijuana use and sexual risk behaviors [20, 26–29], some studies find null relationships between marijuana use and sexual risk behavior [30], and finally, other research shows negative associations such that more marijuana use is actually associated with less sexual risk behaviors [31]. Thus more work is needed to help elucidate when, and if, marijuana use influences sexual risk. The co-occurrence of substance use and risky sexual behavior in high-risk adolescents provides the perfect opportunity to study questions regarding the nature of the possible association of marijuana use and sexual risk. Further, the high co-morbidity between marijuana use and sexual risk among high-risk adolescents suggests the potential utility of including substance use components in interventions targeting sexual risk [32–34]. More broadly, it is well known that theoretically based interventions are more successful than those not based on theory [35], but questions arise regarding whether the same theoretical model is equally appropriate for participants who differ on their substance use status. It is this last point, which forms the basis for our analyses.
The Theory of Planned Behavior (TPB) [36] posits that intentions to engage in a behavior are the most proximal determinant of that behavior, and that intentions are determined by attitudes towards the behavior, norms supportive of the behavior, and self-efficacy for or perceived control over the behavior. In a meta-analysis, Sheeran and Taylor [37] provided support for the TPB as an empirically validated predictor of condom use generally, and several studies have utilized the TPB to examine the cognitive correlates of risky sexual behavior among justice-involved adolescents specifically [12, 38–41]. Bryan et al. [12] tested whether a modified version of the TPB that included adolescent-targeted constructs of future orientation and positive self-concept would be equally predictive of condom use for justice-involved adolescents who did or did not drink alcohol. Neither frequency of use nor alcohol-related problems significantly altered the relationships between model constructs. Further, correlations between self-efficacy and intentions, attitudes and intentions, and, importantly, between intentions and behavior were not significantly different for those who used alcohol and those who did not. These results suggest that interventions targeting TPB constructs should effectively increase condom use intentions and behavior regardless of participants’ alcohol use level. While this study provides evidence in support of the TPB in the context of alcohol use status, there have been no studies to date examining the potential influence of marijuana use on cognitive correlates of condom use intentions and behavior.
In thinking about whether marijuana use may disrupt the relationships between constructs in the TPB, it is helpful to review what is known about the influence of marijuana use on cognition more broadly. In sum, the effects of marijuana use on cognition are currently not well understood. Empirical evidence suggests that cognitive impairment may be associated with heavy marijuana use or marijuana dependence [42, 43]. Further, heavy marijuana use during adolescence has been linked to decreased attention and processing speed related to structural brain abnormalities [44] and to memory and executive function impairments [45], although the full effects of long-term use are yet unknown [46, 47]. Studies investigating the effects of marijuana use on cognitive functioning in adult populations suggest that marijuana use is primarily related to increased willingness to take risks [48, 49]. For example, Wesley et al. [50] found that compared to controls, chronic marijuana users had less activation to losses (via behavioral response) during the strategy development phase of the Iowa Gambling task, suggesting a decreased sensitivity to negative feedback. In other words, chronic marijuana users were more likely to make risky decisions during the task. An increased sensitivity to reward is common among justice-involved adolescents (i.e. sensation seeking/impulsivity) and is related to increased participation in risky behavior [51], but further research is needed to determine the extent to which marijuana may influence this relationship.
Considering the high rate of marijuana use among justice-involved adolescents, and existing evidence regarding the potential influence of marijuana use on risky sexual behavior [19, 20, 52–55], the aim of the current study is to examine the influence of marijuana dependence on the relationships among the constructs in a TPB-based theoretical model. Few studies have used the TPB to investigate the effects of substance use on the cognitive correlates of condom use, but even fewer have examined these factors within the context of substance use disorders. One such study among African American cocaine-smoking adults with high comorbid marijuana use found that personal condom use norms were highly related to intentions to use condoms [53]. In addition to being a specialized population, the investigators did not compare users to non-users in order to explore the potential specificity of the effects of marijuana use on TPB relationships [53].
Given some empirical evidence that heavy marijuana use and marijuana dependence is associated with compromised cognitive function, it follows that relationships among constructs of a theoretical model of health behavior relying heavily on cognitive ability (e.g. the TPB) might be altered for those with compromised cognitive ability due to marijuana use. If true, then employing an intervention based on the TPB for individuals whose cognitive abilities are compromised by heavy marijuana use/dependence could prove to be less effective. Therefore, it is important to determine whether the relationships among TPB constructs are consistent with the application of a TPB-based intervention with individuals who are heavy marijuana users.
Our study builds on prior research by testing the relationships among TPB constructs and condom use behavior among high-risk adolescents who are either marijuana dependent or not in order to provide evidence of the potential influence of marijuana dependence on relationships outlined in the TPB. We hypothesized that marijuana dependence would not influence the relationship of other cognitive correlates to intentions to engage in condom use, consistent with Bryan et al. [12]. However, given the effects of marijuana on decision-making [45], we predicted that marijuana use would moderate the relationship between intentions and behavior, such that adolescents not dependent on marijuana would show a stronger association between intentions and behavior than their marijuana dependent peers. The TPB is a common platform for HIV/STI prevention programs intended for adolescents, but this is the first study to our knowledge exploring whether marijuana dependence influences the relationships among TPB constructs.
Methods
Participants
Data were collected from 720 justice-involved adolescents (66.2 % male) who were 14–18 years of age (M = 15.71, SD = 1.05) at baseline. The majority of young men (89.2 %) and of young women (84.3 %) reported ever having sexual intercourse, with a mean age of first intercourse of 13.3 years (SD = 1.5). Among those who had ever engaged in sexual intercourse (n = 596), the median number of sexual partners was five (M = 8.12, range 1–90). The sample was racially and ethnically diverse (41.5 % Hispanic, 24 % African-American, 15.6 % Caucasian, 11.3 % multi-racial, 3.9 % American Indian, 2.5 % other race/ethnicity, 1.0 % Asian/Pacific Islander, and 0.2 % not reported). Most participants (81 %) indicated that they were still in school, with an average grade level of 9.96 (SD = 1.21, range 7–12). The most frequently reported reasons for arrest were assault (23.7 %) and theft or stealing (16 %), and the mean length of time left on probation at the baseline assessment was 10.56 months (SD = 8.6, range 1–90).
Procedure
Posters detailing the study were hung in the lobbies of adolescent probation offices in the Denver-metropolitan area. Research staff members were regularly available to answer questions and screen for eligibility. Participants were required to be between the ages of 14 and 18, be currently on probation, be able to adequately read and speak English, and be able to understand and comprehend the purpose of the study and the details of the assent form. Each interested adolescent was fully assented in person. For those under 18, parental consent was obtained verbally over the phone and recorded. Participants were then scheduled and paid US$20 after completing the baseline measures. Due to high rates of suboptimal literacy in justice-involved populations, questionnaires were administered via ACASI (Audio Computer-Assisted Self-Interviewing) technology on laptop computers, which assists participants by reading questions aloud over headphones as they are presented. ACASI has been used successfully in previous work with similar populations [3, 32, 41, 56].
Baseline assessments were completed in private conference rooms within the probation office with a trained research assistant present to answer questions. No probation staff were present during the administration of any measures in order to safeguard participant privacy. Participants were reminded that all information was confidential and would not be shared with probation staff or with their parents/guardians, that their participation was completely voluntary, and that they could stop at any time or skip any question they did not feel comfortable answering. All procedures were reviewed and approved by the relevant institutional review boards, and a certificate of confidentiality was obtained from the federal government National Institutes of Health (NIH) and National Institute on Drug Abuse (NIDA) for additional protection.
Baseline Assessment
Model Constructs
Participants answered a range of questions regarding their attitudes, self-efficacy, norms, and intentions about condom use reflecting the core constructs of the TPB. All Cronbach’s alphas (α) refer to the current sample. We assessed self-efficacy as opposed to perceived behavioral control, the traditional construct measured within the TPB framework, as self-efficacy allows for the assessment of perceived confidence across a number of domains. Notably, Ajzen and Madden themselves [57] equate their notion of perceived behavioral control and Bandura’s description of self-efficacy, placing self-efficacy within a more general framework of the relations among beliefs, attitudes, intentions, and behavior. Attitudes toward condoms (k = 7, α = .81; sample item, “I like sex with condoms”), norms for condom use (k = 4, α = .82; sample item, “Most of my friends use condoms when they have sex”), self-efficacy (k = 34, α = .83; sample item, “I am confident that I could get condoms without feeling embarrassed”), and intentions to use condoms (k = 4, α = .82; sample item, “How likely is it that you will buy or get condoms in the next six months?”) were measured with previously validated scales [12, 39]. Two adolescent-specific constructs were control over the future [58], (k = 7, α = .62; sample item, “I just live for today”) and future optimism [12, 39], (k = 4, α = .85; sample item, “How likely do you think it is that you will get a good job someday?”). Self-esteem was assessed with the Rosenberg Self-Esteem Scale [59], (k = 8, α = .74, sample item, “In general, I am satisfied with myself”). Positive future outlook was a single score formed as a combination of the scales of control over the future, future optimism and self-esteem, consistent with the use of this construct in a separate study with a similar population [60]. Each of the three scales was z-scored and averaged (α = .81) to give participants one score for positive future outlook.
Marijuana Use
The majority of participants (60 %) indicated that they had smoked marijuana in the last 6 months. Participants were then asked to indicate on an ordinal 8-point scale how often they smoked marijuana in the past 6 months from 1 = “occasionally” to 8 = “every day”. Of those that indicated marijuana use in the last 6 months, 16.4 % of participants indicated that they smoked occasionally, 14.3 % smoked monthly, 21.8 % smoked weekly, and 47.5 % smoked every day. Notably, adolescents on probation are asked to submit to routine urinalysis screenings for drug use, and our informal conversations with probation staff indicated that most adolescents fail these screenings, lending anecdotal support to the accuracy of the high level of self-reported marijuana use in this sample. Consistent with other work on justice-involved adolescents [3], there was also a high level of other substance use in this sample. The majority of participants drank alcohol at least occasionally (66.8 %) and had smoked at least one cigarette (65.7 %) in the previous 6 months.
Marijuana Dependence
To better describe the severity of marijuana use in this population, subjects completed the Marijuana Dependence Scale (MDS) [61], (k = 10, α = .72). This scale asks participants about 10 symptoms related to marijuana use they may have experienced over the past 12 months (e.g. “spending a significant amount of time trying to obtain, use, or recover from marijuana”), and participants respond “yes” or “no” to each item. Scores range from 0 to 10 with a score of 3 or more indicative of dependence [61]. Of the 632 participants who had ever smoked marijuana, 58.7 % endorsed 3 or more items on the scale, suggesting that over half of the marijuana smokers in this sample could be classified as marijuana dependent.
Condom Use
Consistent with prior studies [12, 32], sexually experienced adolescents were asked, “How much of the time have you used condoms when you have had sexual intercourse?” Responses were scored on a 5-point scale ranging from 1 = “never” to 5 = “always”. Roughly half of participants indicated that they always (28.2 %) or sometimes (24.5 %) used a condom, and 3.7 % said they never used a condom when they have sexual intercourse. Participants also reported how frequently they engaged in sexual intercourse while under the influence of marijuana by answering the question, “In the past 6 months how often were you using marijuana when you were having sex?” Answers were scored on a 5-point scale from 1 = “never” to 5 = “always”. Among those who answered this question (n = 453), the majority indicated never or almost never using marijuana during intercourse (56.7 %), while 24.2 % indicated sometimes and almost one-fifth (19.1 %) indicated they almost always or always had sexual intercourse under the influence of marijuana.
Follow-up Assessment
Participants were contacted 6 months after the baseline assessments to complete the same substance use and sexual behavior measures. Participants were contacted first by a postcard 1 month after the baseline to verify contact information and contacted by phone approximately 2 weeks before their scheduled follow-up. Participants chose a location convenient for them to meet research staff within reasonable driving distance of the lab offices, such as their home, a local restaurant, a community center, or their probation office. To ensure privacy and accurate responses, research assistants only administered questionnaires in locations where participants felt comfortable, were able to focus, and could not be overheard by others. To further ensure privacy, the follow-up questionnaires were also administered via ACASI with headphones. Of the 720 original participants, 649 (90.13 %) completed the six-month follow-up and were paid US$50 upon completion.
Recent Sexual Behavior
The majority of young men (78.5 %) and of young women (76 %) reported being sexually active over the past 6 months. Of those who reported having had sexual intercourse in the past 6 months (n = 487), 55.2 % indicated always or almost always using a condom, 19 % indicated sometimes using a condom, and 25.8 % indicated almost never or never using a condom during intercourse. Adolescents also self-reported whether they had been tested for an STI, tested for HIV/AIDS, gotten pregnant (or got someone else pregnant), and whether they contracted an STI over the past 6 months. Chi square tests revealed that marijuana dependent and non-dependent individuals reported a similar likelihood of being tested for STIs (55.9 and 64.1 % respectively, p = .69), being tested for HIV (43.3 and 50.2 % respectively, p = .13), getting pregnant (or getting someone else pregnant) (13.7 and 11.7 % respectively, p = .52), and likelihood of contracting an STD (6.3 and 5.3 % respectively, p = .64).
Recent Substance Use
At follow-up, roughly half (46.8 %) of participants indicated that they had used marijuana in the past 6 months (n = 337). Of those that indicated marijuana use in the last 6 months, 19.1 % of participants indicated that they smoked occasionally, 16.8 % smoked monthly, 27.4 % smoked weekly, and 36.7 % of participants indicated that they smoked every day, suggesting that frequency of marijuana use did not change dramatically from baseline. When asked about probationary status, 64.2 % indicated that they were currently on probation and had an average of 6 months left to serve (SD = 8.19, range 1–48).
Substance Use and Sexual Activity
Of those who indicated that they had engaged in sexual intercourse in the past 6 months, 48.3 % indicated that they had used marijuana during sexual intercourse at least once and 11.2 % indicated that they had always used marijuana when they had sexual intercourse in the prior 6 months.
Results
The main goal of this study was to test whether marijuana dependence distally influences risky sexual behavior by influencing the cognitive determinants of condom use intentions and behavior. We estimated the same theoretical model of condom use intentions previously tested by Bryan et al. [12] (see Fig. 1), with the exception that a much larger sample allowed the inclusion of condom use at 6 months (rather than intentions) as a behavioral outcome measure. We then assessed whether marijuana dependence moderated the relationships between model variables, or the relationship of model variables assessed at baseline to subsequent condom use (see Fig. 2). The correlations, means and standard deviations of all model variables are summarized in Table 1. All of the model constructs were significantly associated with each other (p’s < .01). Marijuana dependence was negatively associated with positive outlook (r = −.236, p < .01), condom use self-efficacy (r = −.136, p < .01), and attitudes (r = −.092, p < .01), but was not associated with intentions or reported condom use at baseline or follow-up.
Fig. 1.
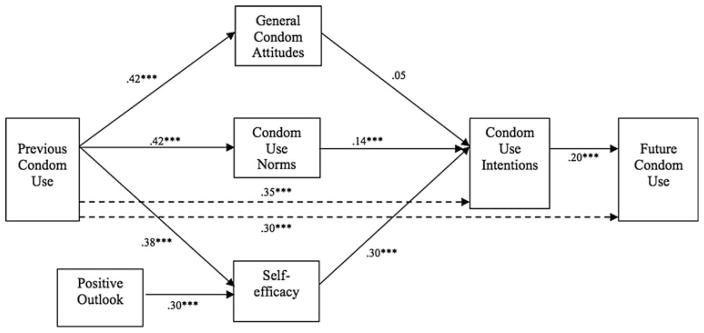
Model of condom use intentions among sexually experienced justice-involved youth. Coefficients are standardized path coefficients. Overall model fit: χ2 (7, N = 720) = 28.47, p < .001; comparative fit index (CFI) = .99; root-mean-square error of approximation (RMSEA) = .04; 90 % confidence intervals of the RMSEA (CI) = .02–.07; SRMR = .009. **p < .05, ***p < .001
Fig. 2.
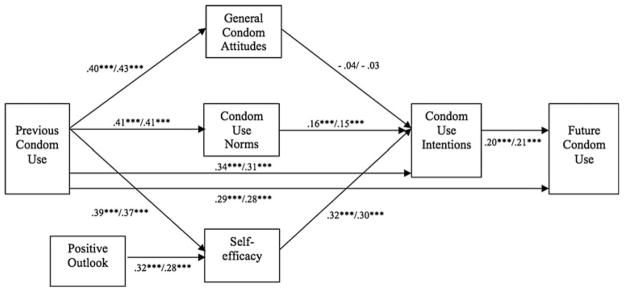
Model of condom use intentions among marijuana dependent and non-dependent participants. Coefficients are standardized path coefficients. Overall model fit: χ2 (28, N = 703) = 44.10; p < .05; comparative fit index = 1.00; root-mean-square error of approximation; RMSEA = .01; 90 % confidence intervals of the RMSEA (CI) = .00–.04; SRMR = .03. The first coefficient shown is for those that are marijuana dependent and the second for those that are non-dependent. ***p < .001
Table 1.
Correlations, raw means, and standard deviations of model constructs for those who ever engaged in intercourse (n = 596)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Positive outlook | – | |||||||||
| 2. Condom use self-efficacy | 0.343* | – | ||||||||
| 3. Condom use attitudes | 0.170* | 0.393* | – | |||||||
| 4. Condom use norms | 0.164* | 0.472* | 0.299* | – | ||||||
| 5. Condom use intentions | 0.216* | 0.517* | 0.344* | 0.471* | – | |||||
| 6. Condom use baseline | 0.122* | 0.409* | 0.435* | 0.414* | 0.511* | – | ||||
| 7. Condom use—six months | 0.075 | 0.236* | 0.307* | 0.286* | 0.342* | 0.388* | – | |||
| 8. Marijuana dependence | −0.236* | −0.136* | −0.092* | −0.068 | −0.030 | −0.059 | −0.064 | – | ||
| 9. Marijuana use—six months | −0.013 | 0.022 | −0.047 | −0.012 | 0.037 | 0.013 | 0.002 | 0.198* | – | |
| 10. Intercourse with marijuana use—six months | −0.070 | 0.013 | −0.008 | 0.023 | −0.005 | 0.025 | 0.008 | 0.187* | 0.498* | – |
| M | 0.044 | 3.549 | 2.944 | 3.010 | 3.301 | 3.767 | 3.483 | 3.277 | 5.325 | 2.309 |
| SD | 0.761 | 0.404 | 0.655 | 0.808 | 0.698 | 1.061 | 1.352 | 2.685 | 2.786 | 1.455 |
Range for all variables is 1–4 except for: positive outlook (z-scored), condom use (1–5), frequency of marijuana use (0–8), marijuana use in conjunction with sexual intercourse, (1–5) and marijuana dependence (0–10)
p < .01
Model of Condom Use Intentions
The model in Fig. 1 was estimated via the EQS structural equation-modeling program [62] with the full sample, utilizing maximum likelihood estimation of missing data (allowing for the inclusion of the whole sample) and consequently robust estimates of standard errors and significance tests [63]. The overall model demonstrated adequate fit to the data, Yuan–Bentler scaled χ2 (9, N = 720) = 108.05, p < .001; comparative fit index (CFI) = .98; root-mean-square error of approximation (RMSEA) = .05; 90 % confidence intervals of the RMSEA (CI) = .03–.07. All hypothesized relationships were supported. Consistent with the marginal fit as indicated by the RMSEA in particular, La Grange multiplier tests for modifications to the model were examined and these suggested that the addition of two paths, one from previous condom use to intentions and one from previous condom use to condom use at 6 months, would significantly improve the fit of the model. The model was estimated again with the addition of these two parameters, providing a two degree of freedom Chi square test of change in fit ( ) [64]. However, since we utilize here the Yuan–Bentler scaled χ2, the test must also be corrected to account for the scaling [65]. In this case, a significant scaled change in χ2 confirmed that the addition of these paths significantly improved model fit, Yuan–Bentler scaled , p < .001. Overall model fit including these paths was excellent, Yuan–Bentler χ2 (7, N = 720) = 28.47, p < .001; CFI = .99; RMSEA = .04; 90 % CI = .02–.07. The final model including all paths, standardized parameter estimates, and significance values for individual paths appears in Fig. 1. The model accounted for 37 % of the variability in condom use intentions and 19 % of the variability in condom use at the six-month follow-up. According to Cohen [66], these represent large and medium effect sizes, respectively, for multivariate models in the social sciences. However, the remaining significant direct paths between previous condom use and current intentions and between previous condom use and condom use 6 months later suggest that influences of prior behavior on intentions and future behavior are not completely accounted for by the constructs included in the model [67].
Influence of Marijuana Use on Model Relationships
A score of three or more on the MDS is a clinically meaningful definition of heavy marijuana use [61]. Thus, to test marijuana use as a moderator we created two groups based on participant scores on the MDS: those who met criteria for marijuana dependence (i.e. score of three or greater; n = 376) and those who did not (i.e. score of two or fewer; n = 327). A cross-groups model was tested [67] by simultaneously estimating the model in marijuana dependent and non-dependent participants. All paths were constrained to be equal between the two groups. Note that 17 participants did not answer the questions about marijuana dependence and thus could not be included in the model. The fit of the model (see Fig. 2) was adequate, χ2 (28, N = 703) = 44.10; p < .05; CFI = 1.00; RMSEA = .01; 90 % CI = .00–.04. Importantly, the size and significance of the structural relationships in the model was invariant across the groups, suggesting that the model performs equally well in marijuana dependent versus non-dependent adolescents.
Discussion
The goal of this study was to examine the influence of heavy marijuana use (i.e. marijuana dependence) on the relationships among cognitive correlates of condom use as defined by the TPB and behavior in justice-involved adolescents. We found extremely high levels of marijuana use among these adolescents, with almost half of this sample reporting that they smoked every day in the prior 6 months at the baseline assessment, and over half meeting criteria for marijuana dependence. Further, almost half of our participants were under the influence of marijuana during sexual intercourse at least once in the prior 6 months. Consistent with our predictions, marijuana dependence did not moderate the relationship of cognitive correlates to intentions to use condoms at baseline, which suggests that participants engage in similar cognitive processes for developing condom use intentions regardless of marijuana dependence status. This finding is consistent with previous research examining the distal influence of alcohol use on condom use cognitions and behavior [12]. In contrast to our expectations, our results demonstrated that the significant relationship between intentions at baseline and condom use behavior 6 months later was not moderated by marijuana dependence status. Our findings indicate that either heavy marijuana use simply does not influence the relationships of cognitive correlates of condom use to intentions and behavior, or that there are perhaps more complex mediating mechanisms or moderating factors that may influence the intention-behavior relationship as it relates to marijuana use. Finally, in general our results did not indicate a significant direct relationship between marijuana use and dependence and a number of domains of risky sexual behavior.
Although inconclusive, a small area of research has addressed the issue of marijuana’s effects on risky decision-making, but less work has focused on the cognitive correlates of risk behavior in conjunction with marijuana use. Thus, the utilization of the TPB to examine the influence of marijuana use on the relationships among the cognitive correlates of condom use and behaviors is a unique contribution and strength of the current study. This study also extends the findings of Bryan et al. [12] by including a prospective measure of behavior—instead of a cross-sectional measure of intentions—in the structural model. Our data suggest that although marijuana dependence is negatively associated with condom use self-efficacy, attitudes, and norms, neither the relationships among these constructs nor the intention-behavior relationship are influenced by level of marijuana use. These findings suggest that interventions focused on cognitive determinants of condom use may be especially important for marijuana dependent young adults, but that the content may not need to be tailored according to whether one is marijuana dependent or not.
These findings add to the larger and complex literature that has demonstrated positive, negative, and null relationships between marijuana use and risk behavior. The negative consequences of chronic marijuana use range from decreased decision-making abilities [68] and decreased sensitivity to negative feedback during MRI tasks [50] to greater risk for developing psychosis during adolescence [69]. Other investigators have documented potential protective consequences of marijuana use including protection of the integrity of the white matter in the brains of adolescent binge drinkers [70] as well as decreased anxiety among frequent smokers [71]. Despite the cognitive impairments that might occur due to marijuana use, our work suggests there may be little influence of marijuana use on the development of condom use intentions or the relationship between intentions and condom use behavior. Additional research is needed to characterize the cognitive and behavioral domains in which marijuana may have negative consequences, no consequences, and even potentially positive consequences.
The current research is limited by our reliance on self-report data and the sensitive nature of the assessments, which may cause biased responding. We are also limited in that self-reported marijuana use was not verified through urine analysis. However, work with high-risk adolescents suggests acceptable correspondence between self-reported marijuana use and biological confirmation [72]. Another concern may be the inclusion of self-efficacy in the TPB instead of perceived behavioral control. Some work has found that it may be possible to empirically differentiate between self-efficacy and perceived behavioral control (e.g. [73]); however, the authors of the TPB suggest that these constructs are conceptually the same [57]. Next, while our sample is ideal for examining behavior among high-risk justice-involved adolescents, our results are not representative of all adolescents and may not generalize to other adolescent populations, especially considering the high frequency of substance use and sexual activity that exists within this sample. Finally, despite the prospective design, the data are ultimately still correlational and any assumptions of causation are tenuous at best.
The current study validated the use of a TPB-based model of the cognitive correlates of condom use among justice-involved adolescents, and demonstrated that marijuana dependence may not influence model relationships, nor moderate the association between intentions to use condoms and condom use behavior. Our results provide insight into the relationship between condom use and marijuana use in justice-involved adolescents, a population with high levels of both marijuana use and unprotected sexual intercourse. Effective, theory-based interventions are needed to reduce behavior that may lead to negative sequellae including HIV/AIDS, other STIs, and unplanned pregnancy. Our results indicate that such interventions based on the TPB framework need not be tailored to marijuana dependence status. These findings contribute to the broader literature on the potential associations of substance use with risky sexual behavior, and reinforce the need to further assess the specific role of marijuana use and the development of interventions meant to decrease risky sexual behavior among populations with co-morbid and heavy marijuana use.
Acknowledgments
The research described in this article was conducted with support from the National Institute on Drug Abuse (1 RO1 DA019139; PI: Angela Bryan). We gratefully thank Dr. Joshua Tybur and Tom Chavez for their assistance with the manuscript, and two anonymous reviewers for their feedback.
Contributor Information
Tiffany J. Callahan, Email: tiffany.callahan@colorado.edu, Department of Psychology and Neuroscience, University of Colorado Boulder, Campus Box 345, Muenzinger Psychology Building, RM. D244, Boulder, CO 80309, USA
Ann E. Caldwell Hooper, Department of Psychology, University of New Mexico, Albuquerque, NM, USA
Rachel E. Thayer, Department of Psychology and Neuroscience, University of Colorado Boulder, Campus Box 345, Muenzinger Psychology Building, RM. D244, Boulder, CO 80309, USA
Renee E. Magnan, Department of Psychology, Washington State University Vancouver, Vancouver, WA, USA
Angela D. Bryan, Department of Psychology and Neuroscience, University of Colorado Boulder, Campus Box 345, Muenzinger Psychology Building, RM. D244, Boulder, CO 80309, USA. Department of Psychology, University of New Mexico, Albuquerque, NM, USA. Center on Alcoholism, Substance Abuse, and Addictions (CASAA), University of New Mexico, Albuquerque, NM, USA
References
- 1.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among American youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health. 2004;36(1):6–10. doi: 10.1363/psrh.36.6.04. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance. Atlanta, GA: Department of Health and Human Services; 2008. [Internet]. 2009 Nov [cited 2010]. http://www.cdc.gov/std/stats08/exordium.htm#a3. [Google Scholar]
- 3.Ewing SWF, Venner KL, Mead HK, Bryan AD. Exploring racial/ethnic differences in substance use: a preliminary theory-based investigation with juvenile justice-involved youth. BMC Pediatr. 2011;11:71. doi: 10.1186/1471-2431-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Robertson AA, Stein JA, Baird-Thomas C. Gender differences in the prediction of condom use among incarcerated juvenile offenders: testing the information-motivation-behavior skills (IMB) model. J Adolesc Health. 2006;38(1):18–25. doi: 10.1016/j.jadohealth.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Rosengard C, Stein LA, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R. Co-occurring sexual risk and substance use behaviors among incarcerated adolescents. J Correct Health Care. 2006;12(4):279–87. doi: 10.1177/1078345806296169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Substance Abuse and Mental Health Services Administration. Results from the 2009 national survey on drug use and health: mental health findings. Rockville MD: Department of Health and Human Services; 2011. Series H-38, HHS Publication No.: SMA 10-4586. [Google Scholar]
- 7.Teplin LA, Mericle AA, McClelland GM, Abram KM. HIV and AIDS risk behaviors in juvenile detainees: implications for public health policy. Am J Public Health. 2003;93(6):906–12. doi: 10.2105/ajph.93.6.906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Parkes A, Wight D, Henderson M, Hart G. Explaining associations between adolescent substance use and condom use. J Adolesc Health. 2007;40(2):180.e1–18. doi: 10.1016/j.jadohealth.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Castrucci BC, Kamb ML, Hunt K. Assessing the center for disease control and prevention’s 1994 HIV counseling, testing, and referral: standards and guidelines—how closely does practice conform to existing recommendations? Sex Transm Dis. 2002;29(7):417–21. doi: 10.1097/00007435-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Devieux J, McMahon R, Rosenberg R, Malow RM. HIV prevention intervention outcome among minority adolescents in court mandated drug treatment. Am J Infect Dis. 2007;3(4):248–54. [Google Scholar]
- 11.Rosengard C, Stein LA, Barnett NP, et al. Randomized clinical trial of motivational enhancement of substance use treatment among incarcerated adolescents: post-release condom non-use. J HIV AIDS Prev Child Youth. 2008;8(2):45–64. doi: 10.1300/J499v08n02_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bryan AD, Rocheleau CA, Robbins RN, Hutchison KE. Condom use among high-risk adolescents: testing the influence of alcohol use on the relationship of cognitive correlates of behavior. Health Psychol. 2005;24(2):133–42. doi: 10.1037/0278-6133.24.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cooper ML. Does drinking promote risky sexual behavior? A complex answer to a simple question. Curr Dir Psychol Sci. 2006;15(1):19–23. [Google Scholar]
- 14.LaBrie J, Earleywine M, Schiffman J, Pederson E, Marriot C. Effects of alcohol, expectancies, and partner type on condom use in college males: event-level analyses. J Sex Res. 2005;42(3):259–66. doi: 10.1080/00224490509552280. [DOI] [PubMed] [Google Scholar]
- 15.Tubman JG, Langer LM. “About last night”: the social ecology of sexual behavior relative to alcohol use among adolescents and young adults in substance abuse treatment. J Subst Abuse. 1995;7(4):449–61. doi: 10.1016/0899-3289(95)90015-2. [DOI] [PubMed] [Google Scholar]
- 16.Bryan AD, Ray LA, Cooper ML. Alcohol use and protective sexual behaviors among high-risk adolescents. J Stud Alcohol Drugs. 2007;68(3):327–35. doi: 10.15288/jsad.2007.68.327. [DOI] [PubMed] [Google Scholar]
- 17.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the future national survey results on drug use, 1975–2008. Volume I: secondary school students. Bethesda (MD): National Institute on Drug Abuse (US); 2009. p. 721. NIH Publication No. 09-7402. [Google Scholar]
- 18.Kingree JB, Betz H. Risky sexual behavior in relation to marijuana and alcohol use among African-American, male adolescent detainees and their female partners. Drug Alcohol Depen. 2003;72(2):197–203. doi: 10.1016/s0376-8716(03)00196-0. [DOI] [PubMed] [Google Scholar]
- 19.Kingree JB, Braithwaite R, Woodring T. Unprotected sex as a function of alcohol and marijuana use among adolescent detainees. J Adolesc Health. 2000;27(3):179–85. doi: 10.1016/s1054-139x(00)00101-4. [DOI] [PubMed] [Google Scholar]
- 20.Bellis MA, Hughes K, Calafat A, et al. Sexual uses of alcohol and drugs and the associated health risks: a cross sectional study of young people in nine European cities. BMC Public Health. 2008;8:155. doi: 10.1186/1471-2458-8-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brodbeck J, Matter M, Moggi F. Association between cannabis use and sexual risk behavior among young heterosexual adults. AIDS Behav. 2006;10(5):599–605. doi: 10.1007/s10461-006-9103-9. [DOI] [PubMed] [Google Scholar]
- 22.Brook JS, Balka EB, Whiteman M. The risks for late adolescence of early adolescent marijuana use. Am J Public Health. 1999;89(10):1549–54. doi: 10.2105/ajph.89.10.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Coffey C, Carlin JB, Lynskey M, Li N, Patton GC. Adolescent precursors of cannabis dependence: findings from the Victorian adolescent health cohort study. Br J Psychiatry. 2003;182:330–6. doi: 10.1192/bjp.182.4.330. [DOI] [PubMed] [Google Scholar]
- 24.Guo JT, Stanton B, Clemens RL, et al. Substance use among rural adolescent virgins as a predictor of sexual initiation. J Adolesc Health. 2005;37(3):252–5. doi: 10.1016/j.jadohealth.2004.11.124. [DOI] [PubMed] [Google Scholar]
- 25.Lane SD, Cherek DR, Tcheremissine OV, Lieving LM, Pietras CJ. Acute marijuana effects on human risk taking. Neuropsychopharmacology. 2005;30(4):800–9. doi: 10.1038/sj.npp.1300620. [DOI] [PubMed] [Google Scholar]
- 26.Bryan AD, Schmiege SJ, Magnan RE. Marijuana use and risky sexual behavior among high-risk adolescents: trajectories, risk factors, and event-level relationships. Dev Psychol. 2012 Mar 5; doi: 10.1037/a0027547. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anderson BJ, Stein MD. A behavioral decision model testing the association of marijuana and sexual risk in young adult women. AIDS Behav. 2011;15(4):875. doi: 10.1007/s10461-010-9694-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hendershot CS, Magnan RE, Bryan AD. Associations of marijuana use and sex-related marijuana expectancies with HIV/STD risk behavior in high-risk adolescents. Psychol Addict Behav. 2010;24(3):404–14. doi: 10.1037/a0019844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Valera P, Epperson M, Daniels J, Ramaswamy M, Freudenberg N. Substance use and HIV-risk behaviors among young men involved in the criminal justice system. Am J Drug Alcohol Abuse. 2009;35(1):43–7. doi: 10.1080/00952990802342923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hensel DJ, Stupiansky NW, Orr DP, Fortenberry JD. Event-level marijuana use, alcohol use, and condom use among adolescent women. Sex Transm Dis. 2011;38(3):239–43. doi: 10.1097/OLQ.0b013e3181f422ce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.MacKellar DA, Valleroy LA, Hoffmann JP, et al. Gender differences in sexual behaviors and factors associated with nonuse of condoms among homeless and runaway youths. AIDS Educ Prev. 2000;12(6):477–91. [PubMed] [Google Scholar]
- 32.Bryan AD, Schmiege SJ, Broaddus MR. HIV risk reduction among detained adolescents: a randomized, controlled trial. J Pediatr. 2009;124(6):E1180–8. doi: 10.1542/peds.2009-0679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.O’Leary A, Hatzenbuehler M. Alcohol and AIDS. 3. New York: Macmillan Reference USA; 2009. [Google Scholar]
- 34.Raj A, Reed E, Santana MC, et al. The associations of binge alcohol use with HIV/STI risk and diagnosis among heterosexual African American men. Drug Alcohol Depen. 2009;101(1–2):101–6. doi: 10.1016/j.drugalcdep.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Glanz K, Rimer B. Theory at a glance: a guide for health promotion practice. 2. National Cancer Institute. Public Health Service Editor; Washington, DC: U.S. Government Printing Office; 2005. [Google Scholar]
- 36.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 37.Sheeran P, Taylor S. Predicting intentions to use condoms: a meta-analysis and comparison of the theories of reasoned action and planned behavior. J Appl Soc Psychol. 1999;29(8):1624–75. [Google Scholar]
- 38.Broaddus MR, Bryan AD. Consistent condom use among juvenile detainees: the role of individual differences, social bonding, and health beliefs. AIDS Behav. 2008;12(1):59–67. doi: 10.1007/s10461-007-9260-5. [DOI] [PubMed] [Google Scholar]
- 39.Bryan AD, Aiken LS, West SG. HIV/STD risk among incarcerated adolescents: optimism about the future and self-esteem as predictors of condom use self-efficacy. J Appl Soc Psychol. 2004;34(5):912–36. [Google Scholar]
- 40.Bryan AD, Kagee A, Broaddus MR. Condom use among South African adolescents: developing and testing theoretical models of intentions and behavior. AIDS Behav. 2006;10(4):387–97. doi: 10.1007/s10461-006-9087-5. [DOI] [PubMed] [Google Scholar]
- 41.Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. J Consult Clin Psychol. 2009;77(1):38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;190(40):E2657–64. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Solowij N, Stephens RS, Roffman RA, et al. Cognitive functioning of long-term heavy cannabis users seeking treatment. JAMA. 2002;287(9):1123–31. doi: 10.1001/jama.287.9.1123. [DOI] [PubMed] [Google Scholar]
- 44.Jacobus J, Bava S, Cohen-Zion M, Mahmood O, Tapert SF. Functional consequences of marijuana use in adolescents. Pharmacol Biochem Behav. 2009;92(4):559–65. doi: 10.1016/j.pbb.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lundqvist T. Cognitive consequences of cannabis use: comparison with abuse of stimulants and heroin with regard to attention, memory and executive functions. Pharmacol Biochem Behav. 2005;81(2):319–30. doi: 10.1016/j.pbb.2005.02.017. [DOI] [PubMed] [Google Scholar]
- 46.Boggio PS, Zaghi S, Villani AB, Fecteau S, Pascual-Leone A, Fregni F. Modulation of risk-taking in marijuana users by transcranial direct current stimulation (tDCS) of the dorsolateral prefrontal cortex (DLPFC) Drug Alcohol Depend. 2010;112(3):220–5. doi: 10.1016/j.drugalcdep.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 47.Fried P, Watkinson B, James D, Gray R. Current and former marijuana use: preliminary findings of a longitudinal study of effects on IQ in young adults. Can Med Assoc J. 2002;166(7):887–91. [PMC free article] [PubMed] [Google Scholar]
- 48.Knutson B, Greer SM. Anticipatory affect: neural correlates and consequences for choice. Philos Trans R Soc Lond B Biol Sci. 2008;363(1511):3771–86. doi: 10.1098/rstb.2008.0155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Knutson B, Wimmer GE, Kuhnen CM, Winkielman P. Nucleus accumbens activation mediates the influence of reward cues on financial risk taking. Neuroreport. 2008;19(5):509–13. doi: 10.1097/WNR.0b013e3282f85c01. [DOI] [PubMed] [Google Scholar]
- 50.Wesley MJ, Hanlon CA, Porrino LJ. Poor decision-making by chronic marijuana users is associated with decreased functional responsiveness to negative consequences. Psychiatry Res. 2011;191(1):51–9. doi: 10.1016/j.pscychresns.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maslowsky J, Buvinger E, Keating DP, Steinberg L, Cauffman E. Cost-benefit analysis mediation of the relationship between sensation seeking and risk behavior among adolescents. Pers Individ Dif. 2011;51(7):802–6. doi: 10.1016/j.paid.2011.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Prev Med. 2001;33(3):179–89. doi: 10.1006/pmed.2001.0869. [DOI] [PubMed] [Google Scholar]
- 53.Scivoletto S, Tsuji RK, Najjar Abdo CH, Queiroz S, Andrade AG, Gattaz WF. Use of psychoactive substances and sexual risk behavior in adolescents. Subst Use Misuse. 2002;37(3):381–98. doi: 10.1081/ja-120002484. [DOI] [PubMed] [Google Scholar]
- 54.Guo J, Chung IJ, Hill KG, Hawkins JD, Catalano RF, Abbott RD. Developmental relationships between adolescent substance use and risky sexual behavior in young adulthood. J Adolesc Health. 2002;31(4):354–62. doi: 10.1016/s1054-139x(02)00402-0. [DOI] [PubMed] [Google Scholar]
- 55.Crosby R, DiClemente R, Wingood G, Rose E, Lang D. Correlates of continued risky sex among pregnant African American teens: implications for STD prevention. J Am Sex Transm Dis. 2003;30(1):57–63. doi: 10.1097/00007435-200301000-00012. [DOI] [PubMed] [Google Scholar]
- 56.Williams ML, Freeman RC, Bowen AM, et al. A comparison of the reliability of self-reported drug use and sexual behaviors using computer-assisted versus face-to-face interviewing. AIDS Educ Prev. 2000;12(3):199–213. [PubMed] [Google Scholar]
- 57.Ajzen I, Madden TJ. Prediction of goal-directed behavior: attitudes, intentions, and perceived behavioral control. J Exp Soc Psychol. 1986;22(5):453–74. [Google Scholar]
- 58.Whitaker CS, Miller KS, Clark LF. Reconceptualizing adolescent sexual behavior: beyond did they or didn’t they? Fam Plann Perspect. 2000;32(3):111–7. [PubMed] [Google Scholar]
- 59.Rosenberg M. Society and the adolescent self-image. Princeton: Princeton University Press; 1965. [Google Scholar]
- 60.Schmiege SJ, Feldstein Ewing SW, Hendershot CS, Bryan AD. Positive outlook as a moderator of the effectiveness of an HIV/STI intervention with adolescents in detention. Health Educ Res. 2011;26(3):432–42. doi: 10.1093/her/cyq060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stephens RS, Roffman RA, Curtin L. Comparison of extended versus brief treatments for marijuana use. J Consult Clin Psychol. 2000;68(5):898–908. [PubMed] [Google Scholar]
- 62.Bentler PM. EQS Program Manual. Encino: Multivariate Software Inc; 1995. [Google Scholar]
- 63.Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociol Methodol. 2000;30:165–200. [Google Scholar]
- 64.Hayduk LA. Structural Equation Modeling with LISREL. Baltimore: Johns Hopkins University Press; 1987. [Google Scholar]
- 65.Satorra A, Bentler P. A scaled difference Chi square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–14. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Kawrence Erlbaum Associates, Inc; 1988. [Google Scholar]
- 67.Hennessy M, Bleakley A, Fishbein M, et al. Differentiating between precursor and control variables when analyzing reasoned action theories. AIDS Behav. 2010;14(1):225–36. doi: 10.1007/s10461-009-9560-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bolla KI, Eldreth DA, Matochik JA, Cadet JL. Neural substrates of faulty decision-making in abstinent marijuana users. Neuroimage. 2005;26(2):480–92. doi: 10.1016/j.neuroimage.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 69.Shapiro GK, Buckley-Hunter L. What every adolescent needs to know: cannabis can cause psychosis. J Psychosom Res. 2010;69(6):533–9. doi: 10.1016/j.jpsychores.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 70.Jacobus J, McQueeny T, Bava S, et al. White matter integrity in adolescents with histories of marijuana use and binge drinking. Neurotoxicol Teratol. 2009;31(6):349–55. doi: 10.1016/j.ntt.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Metrik J, Kahler CW, McGeary JE, Monti PM, Rohsenow DJ. Acute effects of marijuana smoking on negative and positive affect. J Cogn Psychother. 2011;25(1):31–46. doi: 10.1891/0889-8391.25.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Liau A, DiClemente RJ, Wingood GM, et al. Associations between biologically confirmed marijuana use and laboratory-confirmed sexually transmitted diseases among African American adolescent females. Sex Transm Dis. 2002;29(7):387–90. doi: 10.1097/00007435-200207000-00004. [DOI] [PubMed] [Google Scholar]
- 73.Armitage CJ, Conner M. Distinguishing perceptions of control from self-efficacy: predicting consumption of a low fat diet using the theory of planned behavior. J Appl Soc Psychol. 1999;29(1):72–90. [Google Scholar]


