Abstract
Purpose
To identify factors that can affect postoperative shoulder balance in AIS.
Method
89 adolescent idiopathic scoliosis patients with six types of curvatures who underwent surgery were included in this study. Whole spine antero-posterior and lateral radiographs were obtained pre- and postoperatively. In radiograms, shape and changes in curvatures were analyzed. In addition, four shoulder parameters and coronal balance were analyzed in an effort to identify factors significantly related to postoperative shoulder balance.
Result
In general, all the four shoulder parameters (CHD, CA, CRID, RSH) were slightly increased at final follow up (t test, P < 0.05), although there was a decrease in Lenke type II and IV curvatures. However, pre- and postoperative shoulder parameters were not significantly different between each curvature types (ANOVA, P > 0.05). Moreover, no significant differences of pre- and postoperative shoulder level between different level of proximal fusion groups (ANOVA, P > 0.05) existed. In the analysis of coronal curvature changes, no difference was observed in every individual coronal curvatures between improved shoulder balance and aggravated groups (P > 0.05). However, the middle to distal curve change ratio was significantly lower in patients with aggravated shoulder balance (P < 0.05). In addition, patients with smaller preoperative shoulder imbalance showed the higher chance of aggravation after surgery with similar postoperative changes (P < 0.05).
Conclusions
Significant relations were found between correction rate of middle, and distal curvature, and postoperative shoulder balance. In addition, preoperative shoulder level difference can be a determinant of postoperative shoulder balance.
Keywords: Adolescent idiopathic scoliosis, Shoulder balance, Correction surgery
Introduction
In surgical treatment of scoliosis, surgeons have focused on the amount of coronal curvature correction, which can determine the surgical outcome. However, many factors contribute to adolescent idiopathic scoliosis (AIS) patient’s satisfaction after surgery, such as, surgical scars, improved back shape, reduced coronal curvature, and reduced back pain. In addition, cosmesis of the back and shoulders with a coronally balance spine are critically important for AIS patients, and the achievement of shoulder balance is one of the most important measures of successful scoliosis surgery [1–9]. Traditionally, the left shoulder is often elevated in AIS patients with a double thoracic curve. Hence, the achievement of shoulder balance in such AIS patients is an important component of surgical decision making and of evaluations of clinical outcome [5, 10, 11]. In addition, fusion of double structural curvatures in such types with Lenke’s criteria, appears to minimize postoperative shoulder imbalance [12–15]. However, several types of scoliosis without significant proximal thoracic curvature, and we have experienced postoperative shoulder imbalance for other curvature types exist. Moreover, shoulder imbalance can remain in the double thoracic type after instrumentation for either structural curvature. In addition, different levels of postoperative shoulder balance in patients with identical curve classifications and the same fusion level suggest that fusion level and curvature type are not the only factors that determine shoulder balance. It appears that other factors, which affect postoperative shoulder level after corrective surgery exist. Accordingly, the aim of this study was to identify factors that affect final postoperative shoulder level in all types of curvatures.
Materials and methods
Patient and radiological assessment
A total of 89 AIS patients who had been operated between 2005 and 2010 were included in the present study. The study group comprised 23 males and 66 females with an average age of 15.5 years (range 10.7–18.0 years). Exclusion criteria were revision surgery or scoliosis with other disease, such as, congenital, and cerebral palsy. In addition, we excluded the patients with less than 2 years of follow up. There were 19, 26, 11, 14, 7, and 12 Lenke type 1, 2, 3, 4, 5, and 6 patients, respectively. Whole spine standing antero-posterior (AP) and lateral radiographs were taken pre- and postoperatively (at final follow up; mean 27.5 months). The whole spine AP radiographs were taken at a standard tube-film distance of 180 cm, with the central ray targeting at the T6–T7 area. The subjects held onto a vertical pole with their hands at elbow level to keep the upper extremities from projecting over the spine. The typical radiographic exposure factors were 25 mAs and 100 kVp. To identify factors related to postoperative shoulder balance, several parameters were measured in radiograms, pre- and postoperatively.
Surgical procedure
A senior surgeon (SWS) performed the surgery, with only posterior pedicle screw fixation. To correct the curve, derotation maneuver was performed after fixation of the screws. Pre-contoured long rods were applied on pedicle screws, and forceful derotation was performed. In addition, if any residual curvature existed, in situ bending of the rod was performed to obtain maximal corrections. Moreover, posterior fusion was performed with auto- and allogenic cancellous bone after decortication of the lamina. Overall, all the structural curvatures were instrumented with a pedicle screw according to Lenke’s criteria in different types of curvatures [12, 13]. Particularly, in cases of structural proximal thoracic curvature (more than 25° of side bending Cobb angle), the fusion from T1 or T2 including proximal end of the curvature in the fusion segment was performed. In addition, in cases of prominent shoulder imbalance (<10 mm) with non-structural proximal thoracic curvature, the fusion from T2 or T3 was performed to correct the shoulder imbalance. In addition, in other types of scoliosis without significant proximal thoracic curvature, the fusion from below the T4 was performed to minimize the fusion segment.
Coronal curvature measures
All the curvatures were analyzed pre- and postoperatively. After selecting the main structural curvature, consecutive curvatures were identified by each portion, and included compensatory or non-structural curvatures (proximal, middle, distal). For all the curvatures, pre- and postoperative Cobb angles, postoperative changes of each curve and curve change ratios vs initial values were calculated.
Shoulder and truncal balance measures
The four parameters, which were previously studied, and coronal balance were analyzed.
Coracoid height difference (CHD, mm): Height difference between the horizontal lines passing through the upper margin of each coracoid process (Fig. 1a) [6, 16].
Fig. 1.
a Coracoid height difference (CHD, mm): Height difference between the horizontal lines passing through the upper margin of each coracoid process. b Clavicular angle (CA, °): Angle between the line connecting the highest points of the clavicle in the horizontal plane. c Clavicle–rib intersection difference (CRID, mm): Height difference between the horizontal lines passing through the point where the superior border of the clavicle intersects with the outer edge of the second rib on each side d Radiographic shoulder height (RSH, mm): The difference in soft tissue shadow directly superior to the acromioclavicular joint
Clavicular angle (CA, °): angle between the line connecting the highest points of the clavicle in the horizontal plane (Fig. 1b) [6, 17].
Clavicle–rib intersection difference (CRID, mm): height difference between the horizontal lines passing thorough the point where the superior border of the clavicle intersects with the outer edge of the second rib on each side (Fig. 1c) [6, 16].
Radiographic shoulder height (RSH, mm): The difference in soft tissue shadow directly superior to the acromioclavicular joint on standing anteroposterior radiographs (Fig. 1d) [6, 17].
Coronal balance (CB, mm): The horizontal distance between the center of the S1 vertebra and vertical line drawn from the center of C7.
Pre- and postoperative values were calculated for the above-mentioned five parameters. In addition, we calculated postoperative changes in these parameters, and ratios of postoperative changes vs initial levels. The negative values represent the right shoulder elevation, whereas positive values represent the left elevation. Absolute values were used to examine any deviation from normal value regardless of the direction of shoulder or truncal imbalance.
Statistical analysis
Two orthopedic surgeons carried out measurements twice independently at least 1 week apart to decrease intra-observer (ICCs > 0.93, 95 % CI = 0.87–0.95) and inter-observer errors (ICCs > 0.90, 95 % CI = 0.84–0.91). Statistical analysis was performed to determine the presence of significant differences between groups and the nature of correlations between the above-mentioned parameters. All the analyses were performed using the SPSS version 13 (SPSS, Chicago, IL) and MedCalc version 11.5.1 (MedCalc Software, Belgium).
Results
Changes in coronal curvature
For the 89 study subjects, mean preoperative and postoperative Cobb angles, correction angle and rate of each curvature were proximal 32.4, 15.0, 17.8° (54.9 %), middle 58.4, 18.7, 40.0° (68.5 %), and distal 36.7, 10.5, 26.4° (71.9 %), respectively. Furthermore, there was a significant change in the values after surgery (t test, P < 0.0001).
Changes in general postoperative shoulder balance
Table 1 shows the pre- and postoperative values of parameters covering all the curvature types. Preoperatively, the four shoulder parameters were similar for the different curvature types (ANOVA, P > 0.05), except for type VI in CHD (ANOVA; Tukey post hoc test, P = 0.028). Besides, no significant differences between different curvature types were observed in terms of postoperative values and changes in these parameters (ANOVA, P > 0.05). However, 89 patients showed aggravated shoulder level differences at final follow up (t test, P < 0.05). According to curvature types, there was an increase in four shoulder parameters after surgery in Lenke type I, III, IV and V scoliosis, especially in type I and IV curvature with statistical significance (t test, P < 0.05). However, there was a decrease in the values in type II and VI, especially on type II with statistical significance (t test, P < 0.05). In addition, there was a significant improvement in the coronal balance in all curvature types (t test, P < 0.05), and was similar pre- and postoperatively between all the curvature types (ANOVA, P > 0.05).
Table 1.
Mean pre- and post operative values, and changes in shoulder balance in different curvature types
| Lenke type | ||||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | V | VI | P | Total | |
| Shoulder balance (4 parameters) | ||||||||
| CHD (mm) | ||||||||
| Pre-OP | 5.6 ± 5.2 | 10.3 ± 9.9 | 7.3 ± 6.5 | 8.1 ± 8.8 | 7.8 ± 4.2 | 21.2 ± 24.8 | *0.028 | 9.6 ± 11.6 |
| Post-OP | 13.6 ± 9.7 | 8.5 ± 8.4 | 9.6 ± 5.7 | 16.8 ± 10.6 | 9.6 ± 11.9 | 12.0 ± 5.9 | 0.199 | 12.7 ± 9.0 |
| Change | 16.2 ± 12.0 | 15.0 ± 13.7 | 9.3 ± 6.1 | 14.9 ± 15.6 | 12.0 ± 8.8 | 18.4 ± 16.2 | 0.787 | 14.9 ± 13.0 |
| P | *0.006 | *0.037 | 0.853 | *0.001 | 0.823 | 0.272 | *0.043 | |
| CA (°) | ||||||||
| Pre-OP | 1.8 ± 1.4 | 2.6 ± 2.4 | 1.8 ± 1.7 | 2.9 ± 3.3 | 1.7 ± 1.0 | 4.1 ± 6.3 | 0.131 | 2.6 ± 3.0 |
| Post-OP | 3.3 ± 2.2 | 2.4 ± 2.0 | 4.0 ± 7.0 | 4.2 ± 2.3 | 3.5 ± 3.4 | 3.2 ± 1.2 | 0.946 | 3.5 ± 2.9 |
| Change | 4.1 ± 2.9 | 3.7 ± 3.5 | 4.8 ± 6.2 | 4.4 ± 4.0 | 3.2 ± 3.6 | 4.3 ± 4.1 | 0.970 | 4.1 ± 3.7 |
| P | *0.015 | 0.222 | 0.424 | 0.216 | 0.448 | 0.356 | *0.041 | |
| CRID (mm) | ||||||||
| Pre-OP | 4.4 ± 4.0 | 8.2 ± 8.7 | 6.8 ± 9.1 | 5.1 ± 6.7 | 3.3 ± 3.7 | 15.2 ± 17.8 | 0.063 | 7.1 ± 9.3 |
| Post-OP | 8.8 ± 7.1 | 8.0 ± 6.3 | 9.2 ± 4.8 | 13.2 ± 6.7 | 10.1 ± 8.6 | 9.7 ± 5.3 | 0.476 | 10.5 ± 6.5 |
| Change | 11.9 ± 6.7 | 12.7 ± 11.1 | 11.9 ± 11.4 | 14.3 ± 8.6 | 6.8 ± 6.6 | 11.8 ± 12.9 | 0.861 | 12.3 ± 9.7 |
| P | 0.051 | 0.193 | 0.544 | *0.008 | 0.133 | 0.367 | *0.009 | |
| RSH (mm) | ||||||||
| Pre-OP | 7.7 ± 6.8 | 10.9 ± 10.8 | 8.3 ± 6.9 | 8.6 ± 9.9 | 11.7 ± 9.4 | 16.9 ± 17.5 | 0.175 | 10.6 ± 12.7 |
| Post-OP | 15.6 ± 11.0 | 9.7 ± 8.7 | 11.5 ± 8.4 | 18.6 ± 11.8 | 16.5 ± 13.6 | 15.8 ± 5.5 | 0.613 | 15.1 ± 9.8 |
| Change | 19.9 ± 15.2 | 15.5 ± 16.8 | 15.1 ± 6.5 | 18.4 ± 15.4 | 14.6 ± 9.8 | 18.9 ± 17.9 | 0.922 | 17.4 ± 15.4 |
| P | *0.007 | *0.039 | 0.558 | *0.011 | 0.616 | 0.576 | *0.007 | |
| Coronal balance | ||||||||
| CB (mm) | ||||||||
| Pre-OP | 50.4 ± 16.5 | 63.7 ± 23.5 | 59.0 ± 21.1 | 68.6 ± 20.3 | 53.3 ± 9.7 | 50.1 ± 7.9 | 0.060 | 58.9 ± 20.2 |
| Post-OP | 19.8 ± 8.5 | 21.8 ± 13.3 | 23.8 ± 11.8 | 32.2 ± 20.3 | 24.0 ± 13.4 | 18.4 ± 7.3 | 0.107 | 23.0 ± 13.5 |
| Change | 30.9 ± 17.6 | 43.1 ± 22.2 | 36.9 ± 22.9 | 36.8 ± 22.9 | 29.3 ± 16.9 | 31.7 ± 6.1 | 0.352 | 36.7 ± 20.1 |
| P | *0.0001 | *0.0001 | *0.006 | *0.0001 | *0.041 | *0.0001 | *0.0001 | |
| N | 19 | 26 | 11 | 14 | 7 | 12 | 89 | |
To determine the differences in parameters between curvature types, ANOVA was used
To determine the differences in parameters between pre- and postoperative values, t test was used
CHD coracoid height difference, CA clavicular angle, CRID clavicle–rib interface difference, RSH radiologic shoulder height, CB coronal C7 plumb line, Pre-OP preoperative value, Post-OP postoperative value, Change postoperative changes
* Indicates statistical significance (P < 0.05)
Postoperative shoulder balance according to different proximal fusion level
Table 2 shows the pre- and postoperative values of parameters according to different proximal fusion levels in all the types of curvatures. We determined the fusion level up to T1 or T2, T3 and below T4 according to our experiences and the literature [5, 11, 14, 17]. In general, there was an increase in all the shoulder parameters after surgery in all the groups, although CA was slightly decreased in T1 or T2 fusion group without statistical significance (t test, P > 0.05). In addition, no significant differences in preoperative shoulder level between different proximal fusion groups, and all the three groups showed the similar final shoulder level with similar changes (ANOVA, P > 0.05) existed.
Table 2.
Postoperative shoulder balance according to different proximal fusion level
| T1 or T2 | T3 | T4 below | P | Total | |
|---|---|---|---|---|---|
| Shoulder balance (4 parameters) | |||||
| CHD (mm) | |||||
| Pre-OP | 11.9 ± 11.3 | 10.2 ± 9.9 | 8.5 ± 15.1 | 0.645 | 9.6 ± 11.6 |
| Post-OP | 15.2 ± 10.4 | 10.7 ± 7.4 | 11.5 ± 7.9 | 0.113 | 12.7 ± 9.0 |
| Change | 16.2 ± 15.0 | 13.9 ± 11.8 | 14.4 ± 11.5 | 0.777 | 14.9 ± 13.0 |
| P | 0.144 | 0.279 | *0.037 | *0.043 | |
| CA (°) | |||||
| Pre-OP | 2.9 ± 2.9 | 2.2 ± 2.5 | 2.9 ± 4.0 | 0.576 | 2.6 ± 3.0 |
| Post-OP | 2.7 ± 3.2 | 3.6 ± 3.8 | 3.1 ± 2.0 | 0.773 | 3.5 ± 2.9 |
| Change | 3.7 ± 3.7 | 4.4 ± 4.1 | 4.2 ± 3.2 | 0.765 | 4.1 ± 3.7 |
| P | 0.160 | *0.045 | 0.814 | *0.041 | |
| CRID (mm) | |||||
| Pre-OP | 7.9 ± 9.3 | 7.2 ± 9.5 | 7.4 ± 9.4 | 0.989 | 7.1 ± 9.3 |
| Post-OP | 11.6 ± 97.0 | 10.4 ± 5.6 | 8.7 ± 6.7 | 0.306 | 10.5 ± 6.5 |
| Change | 12.2 ± 9.8 | 13.5 ± 10.9 | 10.6 ± 7.3 | 0.614 | 12.3 ± 9.7 |
| P | *0.028 | 0.119 | 0.650 | *0.009 | |
| RSH (mm) | |||||
| Pre-OP | 12.7 ± 11.3 | 10.4 ± 10.3 | 8.6 ± 14.1 | 0.394 | 10.6 ± 12.7 |
| Post-OP | 16.5 ± 11.0 | 13.8 ± 8.8 | 14.9 ± 9.0 | 0.558 | 15.1 ± 9.8 |
| Change | 17.7 ± 17.2 | 17.6 ± 14.7 | 16.3 ± 11.5 | 0.942 | 17.4 ± 15.4 |
| P | 0.174 | *0.031 | 0.283 | *0.007 | |
| Coronal balance | |||||
| CB (mm) | |||||
| Pre-OP | 57.9 ± 20.5 | 64.6 ± 21.9 | 51.1 ± 13.9 | 0.072 | 58.9 ± 20.2 |
| Post-OP | 25.8 ± 16.2 | 21.8 ± 12.2 | 19.9 ± 9.4 | 0.269 | 23.0 ± 13.5 |
| Change | 33.2 ± 21.6 | 43.3 ± 19.98 | 31.5 ± 14.8 | 0.061 | 36.7 ± 20.1 |
| P | *0.0001 | *0.0001 | *0.0001 | *0.0001 | |
To determine the differences in parameters between different fusion levels, ANOVA was used
CHD coracoid height difference, CA clavicular angle, CRID clavicle–rib interface difference, RSH radiologic shoulder height, CB coronal C7 plumb line, Pre-OP preoperative value, Post-OP postoperative value, Change postoperative changes
* Indicates statistical significance (P < 0.05)
Analysis of possible factors to determine postoperative shoulder balance
Pre- and postoperative magnitude of coronal curvature (proximal, middle, and distal)
When the parameters in both the final shoulder balance aggravated and improved groups were analyzed, no significant difference between pre- and postoperative values and changes in proximal, and middle curvatures was observed between these two groups (t test, P > 0.05) (Table 3). However, changes in distal curvature was higher in CA and CRID aggravated group with statistical significance (t test; P = 0.043, P = 0.048, respectively). In addition, it was consistently higher in CHD and RSH aggravated group without any statistical significance (t test; P = 0.105, P = 0.266, respectively).
Table 3.
Analysis of pre- and postoperative coronal curvature changes (proximal, middle, and distal) in the aggravated and improved shoulder balance groups
| Shoulder balance (4 parameters) | Body balance | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CHD | CA | CRID | RSH | CB | |||||||||||
| Agg (n = 56) | Imp (n = 33) | P | Agg (n = 56) | Imp (n = 33) | P | Agg (n = 60) | Imp (n = 29) | P | Agg (n = 58) | Imp (n = 31) | P | Agg (n = 8) | Imp (n = 81) | P | |
| Magnitude of proximal curve (°) | |||||||||||||||
| Pre-OP | 33.0 ± 12.9 | 31.3 ± 12.5 | 0.564 | 32.7 ± 12.6 | 31.9 ± 13.0 | 0.803 | 32.6 ± 12.2 | 31.9 ± 13.8 | 0.798 | 33.6 ± 12.8 | 30.2 ± 12.5 | 0.251 | 33.1 ± 22.0 | 32.4 ± 12.3 | 0.951 |
| Post-OP | 14.4 ± 9.1 | 16.1 ± 6.5 | 0.365 | 14.5 ± 9.0 | 15.9 ± 6.7 | 0.452 | 14.5 ± 9.0 | 16.0 ± 6.4 | 0.391 | 14.6 ± 8.9 | 15.7 ± 6.9 | 0.596 | 14.1 ± 12.2 | 15.0 ± 8.1 | 0.817 |
| Change | 18.8 ± 12.1 | 16.0 ± 9.5 | 0.273 | 18.4 ± 11.9 | 16.8 ± 10.2 | 0.540 | 18.3 ± 11.3 | 16.7 ± 11.3 | 0.556 | 19.1 ± 12.5 | 15.3 ± 8.2 | 0.147 | 24.6 ± 18.1 | 17.4 ± 10.9 | 0.214 |
| Magnitude of middle curve (°) | |||||||||||||||
| Pre-OP | 59.3 ± 18.9 | 56.9 ± 15.1 | 0.546 | 58.2 ± 18.3 | 58.6 ± 16.4 | 0.925 | 58.3 ± 18.2 | 58.6 ± 16.3 | 0.935 | 58.3 ± 18.7 | 58.5 ± 15.3 | 0.963 | 60.9 ± 24.5 | 58.3 ± 17.3 | 0.770 |
| Post-OP | 19.6 ± 10.3 | 17.1 ± 9.8 | 0.283 | 19.2 ± 9.9 | 17.8 ± 10.6 | 0.562 | 19.4 ± 10.1 | 17.2 ± 10.3 | 0.357 | 19.0 ± 9.8 | 18.0 ± 10.8 | 0.681 | 18.1 ± 12.8 | 18.7 ± 10.1 | 0.915 |
| Change | 39.7 ± 14.4 | 39.8 ± 13.0 | 0.983 | 39.1 ± 13.7 | 40.8 ± 14.1 | 0.586 | 38.9 ± 13.5 | 41.4 ± 14.6 | 0.436 | 39.3 ± 14.5 | 40.5 ± 12.7 | 0.718 | 42.8 ± 18.2 | 39.6 ± 13.7 | 0.653 |
| Magnitude of distal curve (°) | |||||||||||||||
| Pre-OP | 38.9 ± 15.6 | 33.0 ± 18.4 | 0.119 | 38.2 ± 15.6 | 34.2 ± 18.7 | 0.295 | 38.5 ± 16.1 | 32.9 ± 18.0 | 0.156 | 37.8 ± 16.3 | 34.7 ± 17.9 | 0.434 | 40.6 ± 14.0 | 36.5 ± 17.0 | 0.636 |
| Post-OP | 10.9 ± 7.7 | 9.7 ± 10.2 | 0.541 | 10.1 ± 7.3 | 11.1 ± 10.7 | 0.603 | 10.4 ± 7.8 | 10.5 ± 10.5 | 0.956 | 10.4 ± 7.2 | 10.5 ± 11.1 | 0.990 | 22.4 ± 18.4 | 9.9 ± 7.7 | 0.267 |
| Change | 28.1 ± 11.7 | 23.5 ± 13.8 | 0.105 | 28.2 ± 11.9 | 23.3 ± 13.4 | *0.043 | 28.2 ± 12.3 | 22.6 ± 12.8 | *0.048 | 27.5 ± 12.4 | 24.3 ± 13.0 | 0.266 | 18.3 ± 7.5 | 26.8 ± 12.8 | 0.102 |
To determine the differences between the groups, t test was used
CHD coracoid height difference, CA clavicular angle, CRID clavicle–rib interface difference, RSH radiologic shoulder height, Agg postoperative aggravated group, Imp postoperative improved group, CB coronal C7 plumb line, Change postoperative changes, Pre-OP preoperative value, Post-OP postoperative value
* Indicates statistical significance (P < 0.05)
Change ratio between coronal curvature [Change ratio = 1st curve changes (°)/2nd curve changes (°)]
When postoperative change ratio between each coronal curvature (proximal, middle, distal) was analyzed, it was observed that middle to distal curve change ratio (middle curve change/distal curve change) was significantly lower in aggravated group (CHD, CA, CRID; t test, P < 0.05) (Table 4). In addition, it was consistently lower in RSH aggravated group without any statistical significance (t test, P = 0.469). Besides, no significant difference in parameters between other comparisons (proximal vs. middle, proximal vs. distal; t test, P > 0.05) existed.
Table 4.
Analysis of differences in coronal curvature change (proximal, middle, and distal) in the aggravated and improved shoulder balance groups
| Shoulder balance (four parameters) | Body balance | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CHD | CA | CRID | RSH | CB | |||||||||||
| Agg (n = 56) | Imp (n = 33) | P | Agg (n = 56) | Imp (n = 33) | P | Agg (n = 60) | Imp (n = 29) | P | Agg (n = 58) | Imp (n = 31) | P | Agg (n = 8) | Imp (n = 81) | P | |
| Proximal vs middle curve | |||||||||||||||
| Change ratio | 0.55 ± 0.68 | 0.47 ± 0.40 | 0.543 | 0.55 ± 0.68 | 0.47 ± 0.39 | 0.574 | 0.56 ± 0.67 | 0.43 ± 0.38 | 0.341 | 0.57 ± 0.69 | 0.43 ± 0.32 | 0.307 | 0.63 ± 0.45 | 0.52 ± 0.60 | 0.719 |
| Proximal vs distal curve | |||||||||||||||
| Change ratio | 1.19 ± 3.19 | 1.58 ± 2.85 | 0.578 | 1.18 ± 3.19 | 1.59 ± 2.85 | 0.552 | 1.17 ± 3.08 | 1.67 ± 3.04 | 0.486 | 1.47 ± 3.70 | 1.08 ± 1.18 | 0.585 | 1.46 ± 1.12 | 1.33 ± 3.13 | 0.934 |
| Middle vs distal curve | |||||||||||||||
| Change ratio | 1.68 ± 0.96 | 2.33 ± 1.64 | *0.049 | 1.65 ± 0.94 | 2.37 ± 1.64 | *0.031 | 1.64 ± 0.91 | 2.49 ± 1.72 | *0.023 | 1.85 ± 1.40 | 2.06 ± 1.06 | 0.469 | 2.75 ± 1.79 | 1.88 ± 1.26 | 0.186 |
To determine the differences between groups, t test was used
CHD coracoid height difference, CA clavicular angle, CRID clavicle–rib interface difference, RSH radiologic shoulder height, Agg postoperative aggravated group, Imp postoperative improved group, CB coronal C7 plumb line, Change ratio 1st curve changes (°)/2nd curve changes (°)
* Indicates statistical significance (P < 0.05)
Initial shoulder level differences (CHD, CA, CRID, and RSH)
When the preoperative value of each shoulder parameters was analyzed, significant differences existed between aggravated and improved groups. In the aggravated group, all the shoulder parameters (CHD, CA, CRID, and RSH) were lower preoperatively (t test, P < 0.0001), with similar postoperative changes (t test, P > 0.05) (Table 5).
Table 5.
Comparisons of pre- and postoperative values of shoulder parameters in the aggravated and improved groups
| Shoulder balance (four parameters) | Body balance | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CHD (mm) | CA (°) | CRID (mm) | RSH (mm) | CB (mm) | |||||||||||
| Agg (n = 56) | Imp (n = 33) | P | Agg (n = 56) | Imp (n = 33) | P | Agg (n = 60) | Imp (n = 29) | P | Agg (n = 58) | Imp (n = 31) | P | Agg (n = 8) | Imp (n = 81) | P | |
| Pre-OP | 4.6 ± 4.5 | 18.0 ± 14.8 | *0.0001 | 1.4 ± 1.1 | 4.7 ± 3.9 | *0.0001 | 3.6 ± 3.4 | 14.5 ± 12.8 | *0.0001 | 5.4 ± 4.8 | 20.3 ± 16.6 | *0.0001 | 31.5 ± 13.6 | 60.3 ± 19.6 | *0.005 |
| Post-OP | 16.0 ± 8.5 | 7.3 ± 7.2 | *0.0001 | 4.4 ± 3.1 | 2.1 ± 1.6 | *0.0001 | 13.0 ± 5.7 | 5.4 ± 4.7 | *0.0001 | 18.1 ± 9.4 | 9.6 ± 7.9 | *0.0001 | 38.7 ± 18.1 | 22.2 ± 12.9 | *0.016 |
| Change | 14.2 ± 10.2 | 16.2 ± 16.9 | 0.541 | 3.9 ± 3.2 | 4.3 ± 4.5 | 0.661 | 11.7 ± 6.8 | 13.6 ± 14.0 | 0.406 | 16.6 ± 11.9 | 18.8 ± 19.8 | 0.530 | 7.2 ± 6.2 | 38.1 ± 19.4 | *0.002 |
To determine the differences between the groups, t test was used
CHD coracoid height difference, CA clavicular angle, CRID clavicle–rib interface difference, RSH radiologic shoulder height, Agg postoperative aggravated group, Imp postoperative improved group, CB coronal C7 plumb line, Pre-OP preoperative value, Post-OP postoperative value, Change postoperative changes
* Indicates statistical significance (P < 0.05)
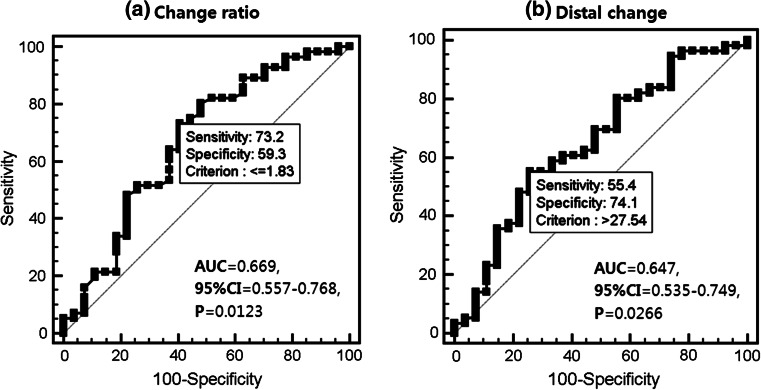
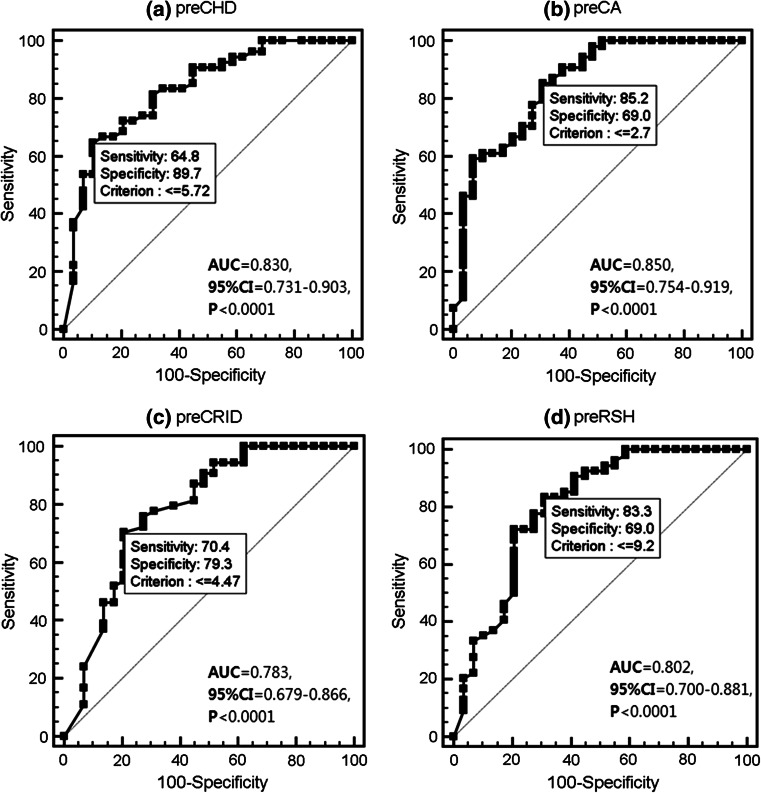
ROC (receiver operating characteristic) curve analysis of related factors
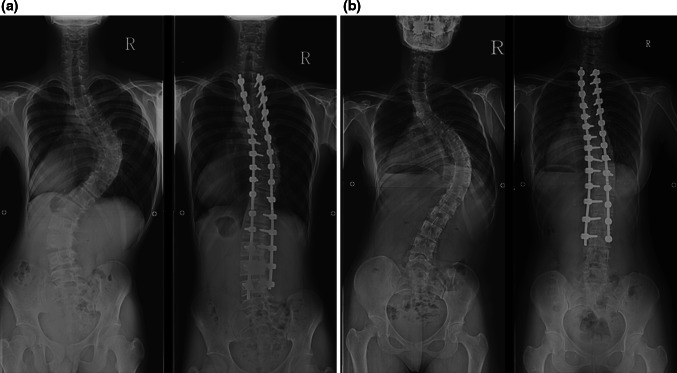
To determine the most effective factor to postoperative aggravation of shoulder balance, we performed the ROC curve analysis. ROC curves were developed by calculating the sensitivity and 1-specificity values for the prediction of the rate of final shoulder level aggravation for the any possible factors. We analyzed ROC curve of the two coronal curvature factors (middle to distal curve change ratio, and magnitude of distal curve change) and four shoulder balance factors (preoperative CHD, CA, CRID, and RSH value), which exhibited significant differences in shoulder balance aggravated group. In terms of coronal curvature factors, middle to distal curvature change ratio showed the cut-off point at <1.83 with statistical significance (P < 0.05) (Fig. 2a). Besides, distal curvature change showed the cut-off point at 27.54> with statistical significance (P < 0.05) (Fig. 2b). In terms of four shoulder balance factors, pre CHD, CA, CRID, and RSH exhibited the cut-off point at <5.72 mm, <2.7°, <4.47 mm, and <9.2 mm with statistical significance (P < 0.0001), respectively (Fig. 3a–d). Figure 4 shows the representative cases.
Fig. 2.
Receiver operating characteristic (ROC) curve analysis graph that predicts an aggravated shoulder balance after surgery with a middle to distal change ratio, and with b distal curvature changes [area under the ROC curve (AUC), 95 % CI (confidence interval), P value]
Fig. 3.
Receiver operating characteristic (ROC) curve analysis graph that predicts an aggravated shoulder balance after surgery with preoperative shoulder level in CHD, CA, CRID and RSH (a–d) [area under the ROC curve (AUC), 95 % CI (confidence interval), P value]
Fig. 4.
a A 16.2-year-old male patient who showed the 31, 74 and 59° of proximal, middle and distal curvature with Lenke type 3/B/N curvature, respectively. Preoperatively, the patient showed shoulder level differences with −2.5 mm, −1.3°, −0.8 mm and −1.0 mm of CHD, CA, CRID and RSH, respectively. Patient also showed improved coronal curvature with 19, 35 and 18°, postoperatively. However, shoulder balance was aggravated postoperatively with 10.8 mm, 3.0°, 14.0 mm and 16.0 mm of 4 parameters. In our analysis of factors, the patient exhibited (1) smaller preoperative shoulder level difference and (2) smaller middle to distal change ratio (0.94), combination of (1) and (2) signifies an aggravation in shoulder level difference. b A 16.4-year-old female patient who showed the 52, 78 and 29° of proximal, middle and distal curvature with Lenke type 2/A/N curvature. Preoperatively, the patient showed shoulder level differences with −23.6 mm, −6.0°, −20.5 mm and −30.9 mm of CHD, CA, CRID and RSH, respectively. Patient showed improved coronal curvature with 27, 23 and 3°, postoperatively. In addition, shoulder balance was improved postoperatively with 4.8 mm, 1.4°, 0.4 mm and 8.4 mm of 4 parameters. In our analysis of factors, the patient exhibited (1) larger preoperative shoulder level difference and (2) larger middle to distal change ratio (2.08), combination of (1) and (2) signifies an improvement in shoulder level difference
Discussion
The treatment of idiopathic scoliosis has improved considerably over the past several years due to advancements in spinal instrumentation and surgical procedures. In addition, standard treatment recommendations have been proposed for the different curve patterns [14, 18–21]. Moreover, the classification system devised by Lenke et al. [13] decades ago has been rendered as reliable and reproducible. This new classification provides a practical and treatment-based system that could pave the way for the introduction of standard surgical recommendations for idiopathic scoliosis. Recently, surgeons started to fuse the whole structural curve, and this appears to produce better results after AIS surgery [12–14]. For proximal thoracic curvatures, fusion of main and proximal thoracic curves that fulfill Lenke’s criteria for double fusion provides good shoulder balance results [5, 13–15]. Besides, Li et al. [5] reported that in 25 patients, 21 (84 %) achieved normal shoulder balance, and 4 (16 %) only minimal imbalance after double fusion of proximal curvature. However, various types of scoliosis with or without proximal thoracic structural curvature exist. Moreover, even if the surgeon achieves the successful correction of the proximal thoracic curvature, shoulder imbalance can remain regardless of the amount of coronal curvature correction, which can significantly worsen the outcome of the surgery [1–4, 6, 16, 17, 22]. Previously, Trobish et al. reported the iatrogenic trunk imbalance after correction surgery, and they emphasized the importance of distal lumbar curvature correction. Undercorrection of the lumbar curve was identified as potential risk factor, whereas thoracic correction, coronal balance, angulation and translation of the lowest instrumented vertebra did not seem to influence postoperative trunk shift [23]. Therefore, prediction and analysis of the final shoulder level in all types of scoliosis can be an important factor, which can determine the surgical outcome. However, no systemic analysis of factors has been shown to predict postoperative shoulder balance, and analyses have focused on extent of fusion level in specific types of scoliosis, such as, in Lenke II and King V. Scoliosis is a whole spine deformity, with many different types of curvatures, and gross truncal balance and shoulder balance might be closely related to changes in whole curvature (e.g., middle, distal) as well as in the proximal thorax. Therefore, in this study, we hypothesized that other factors that determine final shoulder level in AIS regardless of the curvature type or fusion level exist.
Analysis of shoulder balance in different curvature types
In the present study, final shoulder level was slightly aggravated in 89 patients. However, no significant differences were found between different curvature types in terms of the changes in shoulder level or their preoperative values including, double thoracic curvature type. Although we observed significant improvements in shoulder level in Lenke II and VI curvatures, the results were contradictory to the previous reports, which have stated improvements in shoulder balance, with fusion of all the structural curvatures [5, 12, 14, 15]. Recently, many surgeons have focused on the proximal thoracic curvature corrections in specific types of scoliosis (e.g. Lenke II) with proven good results; although, many other types of scoliosis that should be treated exist. In this study, we found that significant shoulder imbalance could be found in another types of scoliosis, which have previously been neglected. Moreover, in the treatment of various types of scoliosis, final postoperative shoulder level can be aggravated regardless of the significant proximal curvature corrections, although these amounted to only millimeters range in our study. Thus, it appears that middle or distal curvature correction can affect the final shoulder balance in various types of scoliosis. Furthermore, we should reconsider the availability of proximal curvature correction in another type of scoliosis, which had been previously accepted as a gold standard for the postoperative improvement of shoulder level in scoliosis with structural proximal thoracic curvature [5, 12, 14, 15]. We should also consider other factors, which are capable of affecting balance, so that it would be feasible to produce more balanced shoulders in any type of curvatures. The findings regarding postoperative shoulder balance are different from the literature, and might contribute to a change in the current concept of predicting postoperative shoulder level in AIS patients.
Analysis of shoulder balance in different proximal fusion level
Kuklo et al. [17] carried out a comparative analysis on 112 patients (proximal curvature >20°) in terms of the shoulder balance. They divided the group into four groups according to proximal fusion level (T2, T3, T4 or T5, T4 below). Subsequently, they reported improvement in the postoperative shoulder level in all the groups. In addition, no significant differences in postoperative shoulder level between the groups exist. Li et al. [5] analyzed postoperative shoulder balance in 25 Lenke type II curvatures. In their study, fusion was performed from T1 or T2 to the distal neutral vertebra of the thoracic curve. A significant improvement in shoulder balance was also demonstrated in their clinical series. However, the aforementioned studies have focused on scoliosis with structural proximal thoracic curvature as Lenke type II. Moreover, the result can be different in other types of scoliosis. In the present study, we analyzed the six types of scoliosis curvature with different proximal fusion level on final follow up radiogram. We performed fusion from T1 or T2 including proximal end of the curvature in the fusion segment with structural proximal thoracic curvature (more than 25° of side bending Cobb angle). In addition, we performed fusion from T2 or T3 to correct the shoulder imbalance in cases of prominent shoulder imbalance (<10 mm) with non-structural proximal thoracic curvature. However, final postoperative shoulder balance was slightly aggravated in 89 patients with various types of scoliosis. In addition, no differences in final shoulder level between different proximal curvature fusion groups exist. Although appropriate proximal fusion may be a determinant of postoperative shoulder balance, and several literatures exist, which show good results, we experienced an unbalanced shoulder level after surgery despite the sufficient proximal fusion in several types of scoliosis. Therefore, another important factor that determines the final shoulder level in any type of scoliosis regardless of whether final proximal fusion level is needed.
Analysis of possible factors that might be related to final shoulder level
Middle and distal curvature correction
In this study, patients with larger middle curvature correction than distal or small distal curvature correction showed improvement in shoulder balance. It appears that correction rate differences between middle and distal curvatures can affect final shoulder level in several types of scoliosis, and can cause either improvement or aggravation in shoulder balance. We suppose that, in majority of scoliosis types, major or large structural curvature is located in middle thoracic region rather than in proximal region. Although proximal curvature correction may have a role in determining the shoulder balance, larger structural middle curvature correction may strongly affect the shoulder balance with the correction of rib cage and vertebral column construct in the thoracic area. However, distal curve is usually located in the lumbar area with flexible form, and might have important role in maintaining a balanced body and shoulder level with compensation. Therefore, excessive correction of distal curve with fusion can lead to collapse of the body balance with different shoulder level. Furthermore, it is supported by our results that show smaller distal curvature correction in shoulder level improved group. Therefore, if the distal curvature is not structural, we suggest shorter distal curvature fixation to preserve the compensatory role of the distal curvature.
Preoperative shoulder level
In this study, the aggravated group showed minimal initial shoulder imbalance than improved group with similar changes. Scoliotic curvature is composed of two or three structured or compensatory curvatures, which all influence the general body shape. It appears that, close relationship exists between curvatures, and this relation may produce the more balanced body shape as well as shoulder level. Apparently, in AIS patients with minimal shoulder imbalance, these coronal curvatures are in a balanced state with compensation, and correction surgery can collapse this state. Thus, seemingly excessive corrections increase the risk of aggravated shoulder balance in less severely affected patients. It is also apparent that to produce more balanced shoulders, appropriate correction with respect to initial shoulder level is important.
Possible shoulder balance determinants
When we analyzed the ROC curve of related factors in final shoulder level aggravated group, the curve change ratio between middle and distal (middle curve change/distal curve change) showed the cut-off point at <1.83 in all the aggravated group. Moreover, although distal curve change showed the cut-off point at 27.54°>, it was only available in CRID aggravated group. In terms of four shoulder balance factors, pre CHD, pre CA, pre CRID, and pre RSH showed the cut-off point at <5.7 mm, <2.7°, <4.5 mm, and <9.2 mm in all the aggravated group. We can assume that approximately less than twice the amount of middle curvature correction than distal leads to more aggravated shoulder balance (with significant distal curve change). In addition, patients with smaller shoulder level differences which are less than the cut-off values are more susceptible to aggravation of shoulder balance after surgery. However, AUC (area under the ROC curve) of the pre CHD, CA, CRID and RSH (0.783>) were higher than that of middle to distal curve change ratio (0.669>) with higher statistical significance (P < 0.0001 vs. P = 0.012). It appears that preoperative shoulder level more strongly influences the final outcome than coronal curvature change ratio.
Recommendations for the surgery
In this study, we found that final shoulder level could be aggravated regardless of the curvature types or fusion level. In addition, it was observed that middle or distal curvature correction could be a factor that affects the postoperative shoulder balance in several types of scoliosis. However, surgeons should be reminded that it should be considered after sufficient fusion of structural proximal thoracic curvature, which have been accepted as gold standard. In addition, if residual shoulder imbalance after fixation of the proximal thoracic curvature exists, surgeons should focus on the correction of middle curvature as well as on minimizing the distal curvature fusion level. We think that correction of gross body balance with significant correction of middle curvature can improve the shoulder level in majority of the scoliosis types. In addition, initial shoulder level should be considered before surgery, which can affect the postoperative shoulder balance. Surgeons should be careful while performing correction surgery of scoliosis with minimal initial shoulder imbalance, which can lead to unfavorable results regardless of the fusion level or type of scoliosis.
Limitations of the present study
The present study is associated with several limitations. The number of subjects was small in some types of scoliosis (e.g., Lenke type V), and subjects were retrospectively gathered that might have a selective bias. In addition, our analysis results might not be available always to predict or prevent the postoperative shoulder level difference in clinical field, and it is hard to control the correction rate of each coronal curvature with current operative techniques. Particularly, although we performed the sufficient proximal fusion in significant upper thoracic curvatures, we could not confirm the standard level of fusion, which can minimize the postoperative shoulder imbalance. In addition, in some cases, we may miss the appropriate fusion level to the good postoperative shoulder balance. In addition, we did not use the direct vertebral rotation method (DVR) in the surgery, which may improve shoulder balance. However, we analyzed the shoulder balance with six types of scoliosis with a unique method in final follow up radiograms. Moreover, the present study identifies the factors related to postoperative shoulder balance, which have previously not been investigated. Finding the other factors besides the proximal fusion level, whether it is evident, may improve the clinical outcomes. Therefore, it is anticipated that the present findings provide useful information to surgeons, and will encourage further studies on the subject of analyzing postoperative shoulder level.
In conclusion, we found that several parameters affect final shoulder level after AIS surgery, regardless of the scoliosis type or proximal curvature changes. In particular, we found a significant relationship between correction rate difference of coronal curvatures (middle, distal) and final shoulder level. Moreover, preoperative shoulder level was the determinant of final shoulder level. Our findings caution that controlled correction of structural and compensating the curvatures considering initial shoulder level probably influence shoulder balance after scoliosis surgery, and we urge that further studies should be conducted on this topic.
Conflict of interest
None.
References
- 1.Asher M, Min Lai S, Burton D, Manna B. The reliability and concurrent validity of the scoliosis research society-22 patient questionnaire for idiopathic scoliosis. Spine (Phila Pa 1976) 2003;28:63–69. doi: 10.1097/00007632-200301010-00015. [DOI] [PubMed] [Google Scholar]
- 2.Asher MA, Lai SM, Glattes RC, Burton DC, Alanay A, Bago J. Refinement of the SRS-22 health-related quality of life questionnaire function domain. Spine (Phila Pa 1976) 2006;31:593–597. doi: 10.1097/01.brs.0000201331.50597.ea. [DOI] [PubMed] [Google Scholar]
- 3.Haher TR, Gorup JM, Shin TM, Homel P, Merola AA, Grogan DP, Pugh L, Lowe TG, Murray M. Results of the scoliosis research society instrument for evaluation of surgical outcome in adolescent idiopathic scoliosis. A multicenter study of 244 patients. Spine (Phila Pa 1976) 1999;24:1435–1440. doi: 10.1097/00007632-199907150-00008. [DOI] [PubMed] [Google Scholar]
- 4.Haher TR, Merola A, Zipnick RI, Gorup J, Mannor D, Orchowski J. Meta-analysis of surgical outcome in adolescent idiopathic scoliosis. A 35-year English literature review of 11,000 patients. Spine (Phila Pa 1976) 1995;20:1575–1584. doi: 10.1097/00007632-199507150-00005. [DOI] [PubMed] [Google Scholar]
- 5.Li M, Gu S, Ni J, Fang X, Zhu X, Zhang Z. Shoulder balance after surgery in patients with Lenke Type 2 scoliosis corrected with the segmental pedicle screw technique. J Neurosurg Spine. 2009;10:214–219. doi: 10.3171/2008.11.SPINE08524. [DOI] [PubMed] [Google Scholar]
- 6.Qiu XS, Ma WW, Li WG, Wang B, Yu Y, Zhu ZZ, Qian BP, Zhu F, Sun X, Ng BK, Cheng JC, Qiu Y. Discrepancy between radiographic shoulder balance and cosmetic shoulder balance in adolescent idiopathic scoliosis patients with double thoracic curve. Eur Spine J. 2009;18:45–51. doi: 10.1007/s00586-008-0833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raso VJ, Lou E, Hill DL, Mahood JK, Moreau MJ, Durdle NG. Trunk distortion in adolescent idiopathic scoliosis. J Pediatr Orthop. 1998;18:222–226. [PubMed] [Google Scholar]
- 8.Sanders JO, Polly DW, Jr, Cats-Baril W, Jones J, Lenke LG, O’Brien MF, Stephens Richards B, Sucato DJ. Analysis of patient and parent assessment of deformity in idiopathic scoliosis using the walter reed visual assessment scale. Spine (Phila Pa 1976) 2003;28:2158–2163. doi: 10.1097/01.BRS.0000084629.97042.0B. [DOI] [PubMed] [Google Scholar]
- 9.Smith PL, Donaldson S, Hedden D, Alman B, Howard A, Stephens D, Wright JG. Parents’ and patients’ perceptions of postoperative appearance in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2006;31:2367–2374. doi: 10.1097/01.brs.0000240204.98960.dd. [DOI] [PubMed] [Google Scholar]
- 10.Ilharreborde B, Even J, Lefevre Y, Fitoussi F, Presedo A, Souchet P, Pennecot GF, Mazda K. How to determine the upper level of instrumentation in Lenke types 1 and 2 adolescent idiopathic scoliosis: a prospective study of 132 patients. J Pediatr Orthop. 2008;28:733–739. doi: 10.1097/BPO.0b013e318185a36b. [DOI] [PubMed] [Google Scholar]
- 11.Smyrnis PN, Sekouris N, Papadopoulos G. Surgical assessment of the proximal thoracic curve in adolescent idiopathic scoliosis. Eur Spine J. 2009;18:522–530. doi: 10.1007/s00586-009-0902-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lenke LG, Betz RR, Haher TR, Lapp MA, Merola AA, Harms J, Shufflebarger HL. Multisurgeon assessment of surgical decision-making in adolescent idiopathic scoliosis: curve classification, operative approach, and fusion levels. Spine (Phila Pa 1976) 2001;26:2347–2353. doi: 10.1097/00007632-200111010-00011. [DOI] [PubMed] [Google Scholar]
- 13.Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, Blanke K. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 14.Puno RM, An KC, Puno RL, Jacob A, Chung SS. Treatment recommendations for idiopathic scoliosis: an assessment of the Lenke classification. Spine (Phila Pa 1976) 2003;28:2102–2114. doi: 10.1097/01.BRS.0000088480.08179.35. [DOI] [PubMed] [Google Scholar]
- 15.Suk SI, Kim WJ, Lee CS, Lee SM, Kim JH, Chung ER, Lee JH. Indications of proximal thoracic curve fusion in thoracic adolescent idiopathic scoliosis: recognition and treatment of double thoracic curve pattern in adolescent idiopathic scoliosis treated with segmental instrumentation. Spine (Phila Pa 1976) 2000;25:2342–2349. doi: 10.1097/00007632-200009150-00012. [DOI] [PubMed] [Google Scholar]
- 16.Bago J, Carrera L, March B, Villanueva C. Four radiological measures to estimate shoulder balance in scoliosis. J Pediatr Orthop B. 1996;5:31–34. doi: 10.1097/01202412-199605010-00006. [DOI] [PubMed] [Google Scholar]
- 17.Kuklo TR, Lenke LG, Graham EJ, Won DS, Sweet FA, Blanke KM, Bridwell KH. Correlation of radiographic, clinical, and patient assessment of shoulder balance following fusion versus nonfusion of the proximal thoracic curve in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2002;27:2013–2020. doi: 10.1097/00007632-200209150-00009. [DOI] [PubMed] [Google Scholar]
- 18.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 19.Lenke LG, Bridwell KH, O’Brien MF, Baldus C, Blanke K. Recognition and treatment of the proximal thoracic curve in adolescent idiopathic scoliosis treated with Cotrel–Dubousset instrumentation. Spine (Phila Pa 1976) 1994;19:1589–1597. doi: 10.1097/00007632-199407001-00007. [DOI] [PubMed] [Google Scholar]
- 20.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:1399–1405. [PubMed] [Google Scholar]
- 21.Suk SI, Lee CK, Min HJ, Cho KH, Oh JH. Comparison of Cotrel–Dubousset pedicle screws and hooks in the treatment of idiopathic scoliosis. Int Orthop. 1994;18:341–346. doi: 10.1007/BF00187077. [DOI] [PubMed] [Google Scholar]
- 22.Akel I, Pekmezci M, Hayran M, Genc Y, Kocak O, Derman O, Erdogan I, Yazici M. Evaluation of shoulder balance in the normal adolescent population and its correlation with radiological parameters. Eur Spine J. 2008;17:348–354. doi: 10.1007/s00586-007-0546-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trobisch PD, Samdani AF, Pahys JM, Cahill PJ. Postoperative trunk shift in Lenke 1 and 2 curves: how common is it? and analysis of risk factors. Eur Spine J. 2011;20:1137–1140. doi: 10.1007/s00586-011-1820-8. [DOI] [PMC free article] [PubMed] [Google Scholar]