Abstract
Purpose
To determine the mid-term clinical and radiographic impact of pedicle screw fixation in patients with adolescent idiopathic scoliosis (AIS).
Methods
A multicenter AIS database was retrospectively queried to identify 99 consecutive patients who underwent posterior spinal fusion using an all pedicle screw construct with a minimum of 5-year follow-up. Radiographic and clinical parameters were reviewed at regular intervals up to 5 years.
Results
The mean age was 14.4 ± 2.0 years with 79 % being female. The mean preoperative major curve was 51.7 ± 14.2° with a mean correction of 66 and 64 % at 2 and 5 years (p = 0.16). Pre-op thoracic kyphosis averaged 22.3 ± 12.9° and was 18.4 ± 10.6° at 5 years with no significant change from 2 years (p = 0.33). SRS total and domain scores demonstrated significant improvements at 2 years, which were slightly decreased at 5 years (p = 0.06). SRS scores of self-image (p = 0.99) and satisfaction (p = 0.18) were significantly improved after surgery with minimal change by 5 years. The change in SRS total scores from 2 to 5 years was attributed to differences in SRS scores of pain and mental health (p < 0.05).
Conclusions
Intermediate follow-up of patients with AIS treated with an all pedicle screw construct demonstrates maintenance of their coronal, and sagittal plane correction between 2- and 5-year follow-up. At 5 years, improvements in SRS scores were consistent with 2-year values, except for a decline in pain and mental health scores.
Keywords: Pedicle screw, Adolescent idiopathic scoliosis, SRS scores, Outcomes, Complications
Introduction
Instrumented correction of scoliotic deformities has evolved from Harrington rods, to Cotrel–Dubousset (CD) instrumentation, to the more recent advent of thoracic pedicle screw fixation [1–6]. Although Harrington rod distraction improved coronal deformity, sagittal plane imbalance was often associated with a high incidence of flatback syndrome [7–9]. The development of CD instrumentation improved upon Harrington rod constructs, but correction of axial rotation remained suboptimal [3–6]. Most recently, the application of thoracic pedicle screws has improved upon many of the limitations from earlier constructs while providing maintenance of correction in the short-term [10–15].
Surgical management of AIS has changed with the application of pedicle screws to the thoracic spine [5]. In 1995, Suk et al. [5] reported outcomes in 78 patients and noted improved coronal correction and less loss of correction at 2 years using screws when compared to hybrid constructs. Subsequently, other studies have shown pedicle screw constructs to provide greater immediate postoperative correction of coronal curvature, axial translation, and axial rotation [11–13]. Better maintenance of correction at 2 years has been reported in both fused and compensatory curves, as well as a reduction in the number of segments fused and a lower revision rate associated with pedicle screw constructs [12, 15, 16]. However, pedicle screw use has also been associated with worsening of thoracic hypokyphosis [17–20].
Although long-term results have been reported for older instrumentation types and anterior constructs, clinical and radiographic outcomes of pedicle screw only constructs are largely based on short to mid-term follow-up with a paucity of data addressing mid- to longer term results [1, 21–25]. Suk et al. [26] reported a 3 % loss of radiographic correction at 5-year follow-up, but did not have clinical correlation. Kim et al. [27] compared hybrid and screw constructs with 5-year minimum follow-up but focused primarily on proximal junctional kyphosis (PJK). We reviewed a large, multicenter series to determine 5-year radiographic and clinical outcomes of pedicle screw instrumentation in the management of AIS.
Materials and methods
IRB approval for the study was obtained locally from each contributing institution’s review board, and consent was obtained from each patient prior to data collection. We retrospectively reviewed a prospectively collected multicenter database of pediatric patients (age ≤18) from January 2002 to December 2006 and identified 99 patients with adolescent idiopathic scoliosis (AIS) and a minimum 5-year follow-up. All patients were consecutively enrolled from each institution and patients that met inclusion criteria were included in our analysis. All patients were primarily treated with pedicle screw instrumentation (>80 % pedicle screws used for possible points of fixation). This definition was adopted as several surgeons favor placement of hooks at the most rostral point of fixation of the construct. Some patients had concurrent anterior releases or adjuvant thoracoplasties, but none were primarily fused anteriorly. The selection of instrumentation levels and technique of surgical correction including use of anterior releases, thoracoplasties, or direct vertebral body derotation were at the discretion of the surgeon.
Clinical, radiographic, and intraoperative measurements were recorded. Data fields recorded included age, gender, curve pattern and modifiers, upper thoracic, main and lumbar curves and flexibility, T5–T12 and T2–T12 kyphosis, lumbar lordosis, thoracic and lumbar rib prominences, instrumentation used, and surgical details. Inclinometer measurements were obtained by having patients stand upright with both feet together in parallel. Patients were then asked to lean forward with their arms extended reaching for the floor while keeping their legs straight. The inclinometer was then centered over the spinous process and translated rostrally and caudally to obtain the largest measure for both the thoracic and lumbar regions. Post-operatively, inclinometer values were first measured at 1 year of follow-up. Clinical outcomes and complications were categorized into groups (infection, re-operation, pulmonary, pseudarthrosis, neurological deficits, instrumentation-related or medical such as significant blood loss).
All institutions contributing data to this study had previously agreed to measure clinical and radiographic variables using a standard technique. For this multicenter study, all radiographs were measured/assessed by one of two personnel dedicated to radiographic evaluation and measurement utilizing digital software. Our internal studies of inter-/intra-rater reliability have shown good to excellent ICC statistics for all continuous measures (0.67–0.99).
Statistical analysis was performed using SPSS 12.0.2® software using Student t tests, Chi square tests and Fisher’s exact tests or Yates’ correction when appropriate. All results were reported as means and standard deviation (SD). A p value of 0.05 was considered statistically significant.
Results
Entire cohort
The entire cohort had a mean age of 14.4 ± 2.0 years of which 78 were female and 21 male. The majority had Lenke type 1 curves (54), whereas 17 had Lenke type 2 curves, 6 had Lenke 3, 2 had Lenke 4, 8 had Lenke 5, and 12 had Lenke type 6 curves. The pre-operative main thoracic curve was 51.7 ± 14.2°, which corrected to 13.7 ± 6.3° translating into a 74 % correction (p < 0.05) (Figs. 1, 2). The lumbar curve similarly improved from 38.7 ± 14.2° to 12.1 ± 8.0° (69 %, p < 0.05). The sagittal profile changed from a T5–T12 kyphosis of 22.3 ± 12.9° to 18.9 ± 9.0° (p < 0.05) while the lumbar lordosis decreased from 59.9 ± 11.5° to 53.4 ± 11.6° (p < 0.05). Rib prominences were not routinely performed immediately post-op, but were significantly improved at 1 year. The thoracic rib prominence improved from 14.5 ± 5.7° to 6.9 ± 3.9° while the lumbar prominence decreased from 8.1 ± 5.6° to 2.8 ± 2.7°.
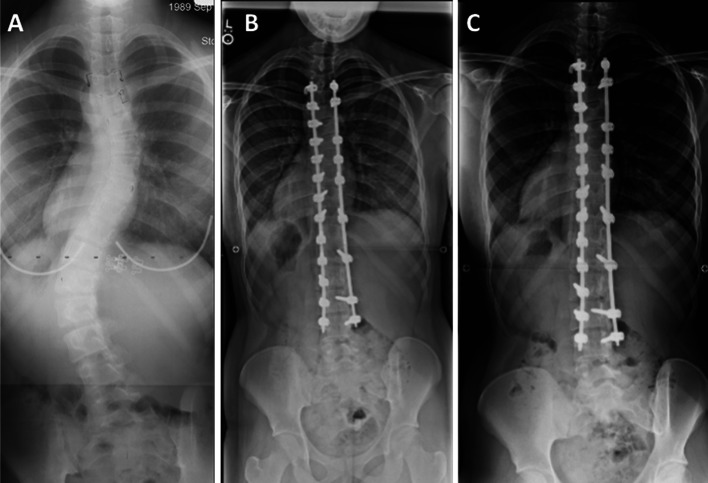
Fig. 1.
a Standing PA radiograph of a 15-year-old girl showing a 45° right thoracic curve pre-operatively and a 55° lumbar curve, b 2-year follow-up radiograph showing correction of the curve with a T4–L4 spinal fusion using pedicle screws, c 5-year follow-up films showing a stable correction
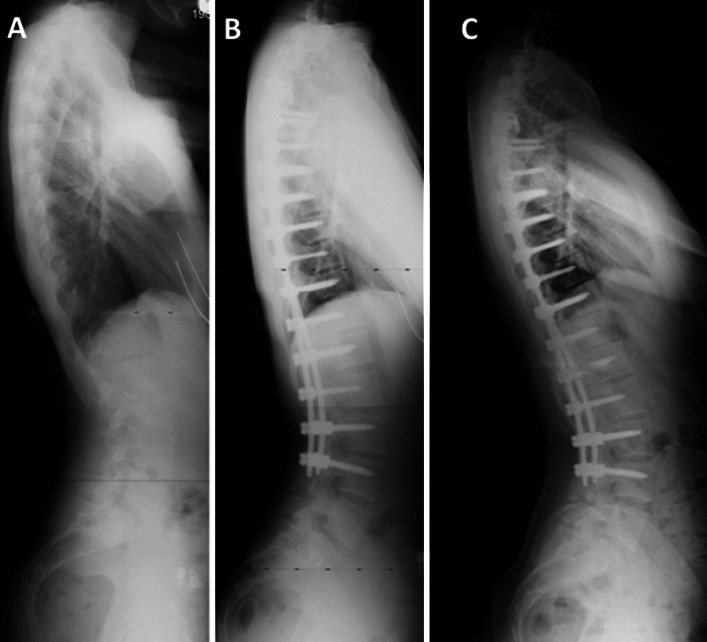
Fig. 2.
a Standing lateral radiograph of a 15-year-old girl with a 45° right thoracic and 55° lumbar curve, b 2-year follow-up lateral radiograph after a T4–L4 spinal fusion, c 5-year follow-up films showing a stable maintenance of the thoracic kyphosis
Radiographic outcomes (Table 1)
Table 1.
Comparison of radiographic outcomes
| Pre-op | First erect | 1-year post-op | 2-year post-op | 5-year post-op | p value (diff between pre-op and first erect year) | p value (diff between first erect and 1 year) | p value (diff between 1 and 2 years) | p value (diff between 2 and 5 years) | |
|---|---|---|---|---|---|---|---|---|---|
| Main thoracic curve (°) | 51.7 ± 14.2 | 13.7 ± 6.3 | 16.5 ± 7.5 | 17.6 ± 7.5 | 18.4 ± 7.5 | <0.05 | <0.05 | 0.05 | 0.16 |
| % correction | NA | 74 | 68 | 66 | 64 | ||||
| Upper thoracic curve (°) | 25.1 ± 10.7 | 13.2 ± 6.4 | 13.2 ± 7.3 | 13.5 ± 7.2 | 13.6 ± 6.4 | <0.05 | 0.86 | 0.46 | 0.93 |
| Thoracic flexibility (%) | 45 ± 20 | NA | NA | NA | NA | NA | NA | NA | NA |
| Lumbar curve (°) | 38.7 ± 14.2 | 12.1 ± 8.0 | 12.8 ± 7.1 | 12.8 ± 7.9 | 13.5 ± 8.0 | <0.05 | 0.05 | 0.33 | 0.31 |
| Lumbar flexibility (%) | 65 ± 24 | NA | NA | NA | NA | NA | NA | NA | NA |
| T5–T12 kyphosis (°) | 22.3 ± 12.9 | 18.9 ± 9.0 | 19.8 ± 9.6 | 19.1 ± 9.3 | 18.4 ± 10.6 | <0.05 | 0.37 | 0.26 | 0.33 |
| Lordosis (°) | 59.9 ± 11.5 | 53.4 ± 11.6 | 58.8 ± 11.8 | 55.7 ± 11.0 | 57.2 ± 11.8 | <0.05 | <0.05 | 0.05 | 0.56 |
| Thoracic scoliometer (°) | 14.5 ± 5.7 | NA | 6.9 ± 3.9 | 7.6 ± 3.9 | 6.7 ± 4.0 | NA | NA | 0.29 | 0.42 |
| Lumbar scoliometer (°) | 8.1 ± 5.6 | NA | 2.8 ± 2.7 | 3.2 ± 3.1 | 2.8 ± 3.1 | NA | NA | 0.09 | 0.62 |
Bold values represent statistical significance
First erect to 1-year post-operative
All measured radiographic parameters had statistically significant change from pre-operative values to the first post-operative recording. However, in the post-operative interval of first erect radiographs to the 1-year follow-up, only a few parameters experienced significant changes. The main thoracic curve worsened slightly from 13.7 ± 6.3° to 16.5 ± 7.5° (p < 0.05) for a change of 6 % with respect to percent correction. The progression in the lumbar curve magnitude was significant (p = 0.05) with a change from 12.1 ± 8.0° to 12.8 ± 7.1° representing a 2 % loss of correction. Although no significant change was noted in the thoracic kyphosis (p = 0.37), the lumbar lordosis increased from 53.4 ± 11.6° to 58.8 ± 11.8° (p < 0.05). The remaining radiographic measures were not significantly changed at 1 year of follow-up (Table 1).
1-year post-operative to 2-year post-operative
Although both main thoracic curvature and lumbar lordosis were statistically significantly different between 1- and 2-year follow-up, the difference was less notable than previously calculated (p = 0.05) and the lumbar curve magnitude did not experience any statistically significant change (p = 0.33). The main thoracic curve progressed from 16.5 ± 7.5° to 17.6 ± 7.5° (p = 0.05) while lordosis decreased from 58.8 ± 11.8° to 55.7 ± 11.0° (p = 0.05). No significant changes were observed in the remaining radiographic measures (Table 1).
2-year post-operative to 5-year post-operative follow-up
In the post-op interval between 2 and 5 years, no significant changes were noted in any of the radiographic parameters measured. Both radiographic and inclinometer values were stable when compared between 2 and 5 years post-op (Table 1).
SRS scores
The total SRS scores were improved from pre-operative values at 2 (p < 0.05) and 5 years (p < 0.05), but a statistical trend with worsening scores between 2- and 5-year follow-up was present (p = 0.06, Table 2). All values appeared to have improvement at 2-year post-op, but tended to decline by 5-year follow-up. SRS scores for self-image (5 year: 4.37 ± 0.63) and satisfaction (5 year: 4.59 ± 0.64) were improved from pre-op values (3.38 ± 0.63 and 3.51 ± 1.12, respectively, p < 0.05) and did not display any significant change between 2 and 5-year follow-up (p = 0.99 and p = 0.18). SRS scores of pain and mental health were improved from pre-op to 2 years, but were not significantly different between pre-op and 5 year follow-up secondary to a statistically decline between 2 and 5 years (Table 2).
Table 2.
Comparison of clinical SRS outcomes between pre-op, 2-year and 5-year follow-up
| Pre-op | 2-year post-op | 5-year post-op | p value (diff between pre-op and 2 years) | p value (diff between pre-op and 5 years) | p value (diff between 2 years and 5 years) | |
|---|---|---|---|---|---|---|
| SRS scores (total) | 4.00 ± 0.45 | 4.59 ± 0.33 | 4.39 ± 0.56 | <0.05 | <0.05 | 0.06 |
| SRS scores (pain) | 4.26 ± 0.66 | 4.65 ± 0.47 | 4.38 ± 0.71 | <0.05 | 0.14 | <0.05 |
| SRS scores (self-image) | 3.38 ± 0.63 | 4.49 ± 0.43 | 4.37 ± 0.63 | <0.05 | <0.05 | 0.99 |
| SRS scores (function) | 4.63 ± 0.52 | 4.80 ± 0.34 | 4.62 ± 0.60 | <0.05 | 0.89 | 0.18 |
| SRS scores (mental health) | 4.01 ± 0.72 | 4.43 ± 0.48 | 4.15 ± 0.76 | <0.05 | 0.07 | <0.05 |
| SRS scores (satisfaction) | 3.51 ± 1.12 | 4.71 ± 0.46 | 4.59 ± 0.64 | <0.05 | <0.05 | 0.18 |
Bold values represent statistical significance
Complications
Fifty-one complications were reported in the entire cohort. Four patients had gastro-intestinal issues (1 ileus, 1 superior mesenteric artery syndrome, and 2 general discomfort) that all resolved with conservative management. One patient experienced transient vocal cord paresis. Two patients were reported to have excessive blood loss treated with transfusions and one patient was hypotensive from over medication who required supportive therapy. Another patient had a urinary tract infection. Six patients had respiratory system complications (2 atelectasis, 4 pleural effusions/pneumothoraces), which were managed medically. One of the patients who developed a pleural effusion had a thoracoplasty and two with atelectasis had anterior releases. The incidence of pulmonary complications in patients who had anterior releases or thoracoplasties was not statistically different from those that only had posterior fusions (p = 0.09).
Three patients had malpositioned instrumentation that required revision surgery and one had prominent instrumentation that was managed conservatively. Seven patients complained of post-op radicular symptoms that did not require re-operation. Five patients had superficial wound infections or drainage that were resolved with oral antibiotics and one patient had drainage from a chest incision 5 years after surgery requiring drainage of a deep infection. Two patients had treatment for cosmetically unpleasant scarring. Seventeen patients had complaints of pain after recovering from the surgery. Eleven patients complained of back pain of which three developed four or more years after surgery. Three patients had chest wall pain and three others had miscellaneous complaints of pain (shoulder and neuropathic). All were treated with a combination of physical therapy and medication.
Almost all complications were reported within 2 years of the index surgery. Only one deep infection and three cases of back pain occurred after 2-year follow-up.
Subgroup analysis
Given the potential ambiguity in interpreting thoracic and lumbar prominences after thoracoplasty, a subgroup analysis was performed comparing patients without thoracoplasty (N = 81) against those that did have one performed (N = 18). Both groups had statistically significant improvement in the thoracic and lumbar prominences from pre-op to the 1-year measure (p < 0.05), which was maintained at 2 and 5 years except for lumbar prominence in the patients that did not receive a thoracoplasty. The subgroup that did not undergo a thoracoplasty had a change from 2.60 ± 2.44° to 3.43 ± 3.20° (p = 0.01). When comparing prominences between the two groups, only the thoracic prominence was statistically different at 1 and 5 years with the thoracoplasty group having less of a rib prominence. At 1 year, the thoracoplasty group had an average measure of 5.07 ± 3.34° versus 7.33 ± 3.94° in the non-thoracoplasty group. Similarly at 5 years, the thoracoplasty group had a measure of 4.72 ± 3.41° versus 7.25 ± 4.00° (p < 0.05).
A separate subgroup analysis was performed comparing radiographic outcomes at the same post-op intervals excluding patients that had a thoracoplasty or anterior release (N = 26). Similarly to our entire cohort, the change in thoracic curvature and lumbar lordosis was statistically significant (p < 0.05) at all intervals except between 2 and 5 years (p = 0.60). Thoracic kyphosis was similarly paralleled in the subgroup analysis except that a statistical difference was noted between the 2- and 5-year interval (p < 0.05). Thoracic kyphosis changed from 18.6 ± 9.2° at 2 years to 16.8 ± 10.2° at 5 years (p < 0.05), but had remained stable from first erect to 2 years. The thoracic rib prominence was also unchanged from 2 to 5 years. Overall, the trends observed in the subgroup were similar to those noted in the entire cohort.
Discussion
Long-term outcomes have been reported using older posterior spinal instrumentation constructs [1, 21–23, 28] as well as anterior spinal fusions [24, 25]. Some series have reported slight increases or progression of radiographic parameters, but most have displayed evidence of correction maintenance with increased follow-up extending up to 20 years [1, 22–25, 28]. Although several studies comparing earlier instrumentation systems have evaluated long-term surgical outcomes in AIS, the relatively recent innovation of thoracic pedicle screws has limited the long-term data available for pedicle screw-only constructs [1, 2, 21, 22, 26, 27, 29].
Using pedicle screw constructs, Suk et al. [26] reported their surgical outcomes on 203 patients having undergone pedicle screw fixation with at least 5-year follow-up and noted a loss of 3 % correction of the main thoracic curve and a 5 % loss of correction of the unfused compensatory lumbar curve over time. However, their sagittal profile and lumbar lordosis remained stable at 5 years with no significant change compared to 1-month postoperative radiographs. Other series have also reported mid-term pedicle screw outcomes, but have been limited by their cohort size. Hwang et al. [30] assessed skipped pedicle screw fixation in 57 patients with 5-year follow-up and noted minimal loss of correction from the immediate post-op (2 %), but did not remark on any changes at the 2-year interval. Di Silvestre et al. [11] compared hybrid and pedicle screw constructs with a mean follow-up of 6.7 years and found better maintenance of correction with screws. They noted a mean loss of 11.3° with hybrid constructs as compared to 1.9° using screws (p = 0.0005).
We observed a more significant loss of correction in the main thoracic curves over time. We noted a 6 % loss of improvement at 1 year of follow-up which represented a statistically significant change that progressed another 2 % by 2 years. Although some minor changes still developed, no statistical difference was noted in progression between 2- and 5-year follow-up. The more notable differences in progression from our series may be partially attributed to variations in instrumentation; however, details of rod thickness and screw types were not reported in prior series to compare. Some of the variations may also be secondary to the magnitude of initial correction. Our series reported a slightly higher percent correction of 74 % when compared to Hwang et al. (67 %) and Suk et al. (72 %) [26, 30]. Statistical differences were not reported in prior series and therefore limit our ability to infer the significance of the loss of correction, however in our series, with most radiographic parameters, the magnitude of progression diminished over time and was not substantial between 2- and 5-year follow-up.
Similarly, SRS scores were stable between 2- and 5-year follow-up. There was a statistical trend toward significance of the overall SRS total (p = 0.06), largely attributed to diminished scores in mental health and pain. SRS domain scores for self-image and satisfaction were improved from pre-op at all post-op intervals without any significant change between 2 and 5 years. Within our cohort, 17 patients had complaints of pain after having recovered from the immediate post-op period. The most common type of pain was back pain, of which three cases were late presentations at 4 and 5 years post-op and may have contributed to the overall decrease in SRS domain scores for pain. Furthermore, repeated episodes of pain may impact overall scores of mental health and could also have contributed to such a decrease in related domain scores.
Prior series have reported a high incidence of back pain at 10-years follow-up in post-operative scoliosis patients [1, 22, 31]. However, poor sagittal balance and flatback syndrome associated with Harrington rod instrumentation may account to some degree for the high incidence of long-term back pain. Bartie et al. [31] reported that 75 % of patients having Harrington rod instrumentation implanted at 10-year follow-up had back pain, which was significantly higher than their control group. Similarly Cochran et al. [1] reported 41 % of patients with at least 5-year follow-up having intermittent back pain. Bjerkreim et al. [22] reported 45 % of their patients with CD instrumentation having some degree of back pain with 10-year follow-up. Our reported rates of back pain are significantly less than prior series; however, many of these reports have longer patient follow-up. Given the incidence of back pain in the general population, a higher incidence among post-op scoliosis patients with increasing time would be expected.
Prior series have reported complication rates using pedicle screw constructs, but most have revolved around placement of screws and not the clinical complications [32–34]. Our series only had three malpositioned screws, but these were not evaluated by post-operative CT imaging. The majority of complications encountered occurred within 2 years of the index surgery with little change by 5 years.
Although there is a paucity of data at 5-year follow-up, there is currently no data on 10-year outcomes with pedicle screw constructs. Greater follow-up is required to better evaluate the incidence of long-term clinical outcomes after pedicle screw only constructs and to determine radiographic results.
Conclusion
Intermediate follow-up of patients with AIS treated with an all pedicle screw construct demonstrates maintenance of their coronal, and sagittal plane correction. At 5 years, improvements in SRS scores were consistent with 2-year values, except for changes in pain and mental health after surgery which statistically worsened.
Conflict of interest
This study was supported by a research grant from Depuy Spine to the Setting Scoliosis Straight Foundation of the Harms Study Group.
References
- 1.Cochran T, Irstam L, Nachemson A. Long-term anatomic and functional changes in patients with adolescent idiopathic scoliosis treated by Harrington rod fusion. Spine. 1983;8:576–584. doi: 10.1097/00007632-198309000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Danielsson AJ, Nachemson AL. Back pain and function 23 years after fusion for adolescent idiopathic scoliosis: a case–control study-part II. Spine. 2003;28:E373–E383. doi: 10.1097/01.BRS.0000084267.41183.75. [DOI] [PubMed] [Google Scholar]
- 3.Ecker ML, Betz RR, Trent PS, Mahboubi S, Mesqarzadeh M, Bonakdapour A, et al. Computer tomography evaluation in Cotrel–Dubousset instrumentation in idiopathic scoliosis. Spine. 1988;13:1141–1144. doi: 10.1097/00007632-198810000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Shufflebarger HL, Smiley K, Roth HJ. Internal thoracoplasty. A new procedure. Spine. 1994;19:840–842. doi: 10.1097/00007632-199404000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Suk S, Choon KL, Won-Joong K, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. [PubMed] [Google Scholar]
- 6.Wood KB, Transfeldt EE, Ogilvie JW, et al. Rotational changes of the vertebral-pelvic axis following Cotrel–Dubousset instrumentation. Spine. 1991;16:S404–S408. doi: 10.1097/00007632-199108001-00019. [DOI] [PubMed] [Google Scholar]
- 7.Booth KC, Bridwell KH, Lenke LG, et al. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance) Spine. 1999;24:1712–1790. doi: 10.1097/00007632-199908150-00013. [DOI] [PubMed] [Google Scholar]
- 8.Bradford DS, Tribus CB. Current concepts and management of patients with fixed decompensated spinal deformity. Clin Orthop Relat Res. 1994;306:64–72. [PubMed] [Google Scholar]
- 9.Weatherley CR, Draycott V, O’Brien JF, et al. The rib deformity in adolescent idiopathic scoliosis. J Bone Jt Surg Br. 1987;69:179–182. doi: 10.1302/0301-620X.69B2.3818745. [DOI] [PubMed] [Google Scholar]
- 10.Asghar J, Samdani AF, Pahys JM, et al. Computed tomography evaluation of rotation correction in adolescent idiopathic scoliosis: a comparison of an all pedicle screw construct versus a hook-rod system. Spine. 2009;34(8):804–807. doi: 10.1097/BRS.0b013e3181996c1b. [DOI] [PubMed] [Google Scholar]
- 11.Di Silvestre M, Bakaloudis G, Lolli F, et al. Posterior fusion only for thoracic adolescent idiopathic scoliosis of more than 80 degrees: pedicle screws versus hybrid instrumentation. Eur Spine J. 2008;17:1336–1349. doi: 10.1007/s00586-008-0731-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dobbs MB, Lenke LG, Kim YJ, et al. Selective posterior thoracic fusions for adolescent idiopathic scoliosis: comparison of hooks versus pedicle screws. Spine. 2006;31:2400–2404. doi: 10.1097/01.brs.0000240212.31241.8e. [DOI] [PubMed] [Google Scholar]
- 13.Karatoprak O, Unay K, Tezer M, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery. Int Orthop. 2008;32:523–528. doi: 10.1007/s00264-007-0359-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adolescent idiopathic scoliosis following segmental posterior spinal instrumentation and fusion. Minimum 5-year follow-up. Spine. 2005;30:2045–2050. doi: 10.1097/01.brs.0000179084.45839.ad. [DOI] [PubMed] [Google Scholar]
- 15.Liljenqvist U. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuklo TR, Potter BK, Lenke LG, et al. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine. 2007;32:2258–2264. doi: 10.1097/BRS.0b013e31814b1ba6. [DOI] [PubMed] [Google Scholar]
- 17.Clements DH, Betz RR, Newton PO, et al. Correlation of scoliosis curve correction with the number and type of fixation anchors. Spine. 2009;34:2147–2150. doi: 10.1097/BRS.0b013e3181adb35d. [DOI] [PubMed] [Google Scholar]
- 18.Helgeson MD, Shah SA, Newton PO, et al. Evaluation of proximal junctional kyphosis in adolescent idiopathic scoliosis following pedicle screw, hook, or hybrid instrumentation. Spine. 2010;35:177–181. doi: 10.1097/BRS.0b013e3181c77f8c. [DOI] [PubMed] [Google Scholar]
- 19.Hwang SW, Samdani AF, Gressot LV, et al. Effect of direct vertebral body derotation on the sagittal profile in adolescent idiopathic scoliosis. Eur Spine J. 2012;21(1):31–39. doi: 10.1007/s00586-011-1991-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Quan GM, Gibson MJ. Correction of main thoracic adolescent idiopathic scoliosis using pedicle screw instrumentation. Does higher implant density improve correction? Spine. 2010;35:562–567. doi: 10.1097/BRS.0b013e3181b4af34. [DOI] [PubMed] [Google Scholar]
- 21.Andersen MO, Christensen SB, Thomsen K. Outcome at 10 years after treatment for adolescent idiopathic scoliosis. Spine. 2006;31:350–354. doi: 10.1097/01.brs.0000197649.29712.de. [DOI] [PubMed] [Google Scholar]
- 22.Bjerkreim I, Steen H, Brox JI. Idiopathic scoliosis treated with Cotrel–Dubousset instrumentation: evaluation 10 years after surgery. Spine. 2007;32:2103–2110. doi: 10.1097/BRS.0b013e318145a54a. [DOI] [PubMed] [Google Scholar]
- 23.Helenius I, Remes V, Yrjonen T, et al. Harrington and Cotrel–Dubousset instrumentation in adolescent idiopathic scoliosis. Long-term functional and radiographic outcomes. J Bone Jt Surg. 2003;85-A:2303–2309. doi: 10.2106/00004623-200312000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Kelly DM, McCarthy RE, McCullough FL, Kelly HR. Long-term outcomes of anterior spinal fusion with instrumentation for thoracolumbar and lumbar curves in adolescent idiopathic scoliosis. Spine. 2010;35(2):194–198. doi: 10.1097/BRS.0b013e3181bc948e. [DOI] [PubMed] [Google Scholar]
- 25.Tis JE, O’Brien MF, Newton PO, et al. Adolescent idiopathic scoliosis treated with open instrumented anterior spinal fusion: five-year follow-up. Spine. 2010;35(1):64–70. doi: 10.1097/BRS.0b013e3181c4af52. [DOI] [PubMed] [Google Scholar]
- 26.Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine. 2005;30:1602–1609. doi: 10.1097/01.brs.0000169452.50705.61. [DOI] [PubMed] [Google Scholar]
- 27.Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2006;31:291–298. doi: 10.1097/01.brs.0000197865.20803.d4. [DOI] [PubMed] [Google Scholar]
- 28.Boos N, Dolan LA, Weinstein SL. Long-term clinical and radiographic results of Cotrel–Dubousset instrumentation of right thoracic adolescent idiopathic scoliosis. Iowa Orthop J. 2007;27:40–46. [PMC free article] [PubMed] [Google Scholar]
- 29.Jeng CL, Sponseller PD, Tolo VT. Outcome of Wisconsin instrumentation in idiopathic scoliosis. Minimum 5-year follow-up. Spine. 1993;18:1584–1590. doi: 10.1097/00007632-199309000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Hwang CJ, Lee CK, Chang BS, et al. Minimum 5-year follow-up results of skipped pedicle screw fixation for flexible idiopathic scoliosis. J Neurosurg Spine. 2011;15(2):146–150. doi: 10.3171/2011.4.SPINE10321. [DOI] [PubMed] [Google Scholar]
- 31.Bartie BJ, Lonstein JE, Winter RB. Long-term follow-up of adolescent idiopathic scoliosis patients who had Harrington instrumentation and fusion to the lower lumbar vertebrae: is low back pain a problem? Spine. 2009;34(24):E873–E878. doi: 10.1097/BRS.0b013e3181aa7d53. [DOI] [PubMed] [Google Scholar]
- 32.Abul-Kasim K, Ohlin A, Strombeck A, Maly P, Sundgren PC. Radiological and clinical outcome of screw placement in adolescent idiopathic scoliosis: evaluation with low-dose computed tomography. Eur Spine J. 2010;19(1):96–104. doi: 10.1007/s00586-009-1203-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sarlak AY, Tosun B, Atmaca H, Sarisoy HT, Buluc L. Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur Spine J. 2009;18(12):1892–1897. doi: 10.1007/s00586-009-1065-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li G, Lv G, Passias P, Kozanek M, Metkar US, Liu Z, Wood KB, Rehak L, Deng Y. Complications associated with thoracic pedicle screws in spinal deformity. Eur Spine J. 2010;19(9):1576–1584. doi: 10.1007/s00586-010-1316-y. [DOI] [PMC free article] [PubMed] [Google Scholar]