Abstract
Study design
Radiological reproducibility study.
Purpose
To assess intra and interobserver reliability of radiographic measurements for global sagittal balance parameters and sagittal spine curves, including cervical spine.
Summary of background data
Sagittal spine balance in adolescent idiopathic scoliosis (AIS) is a main issue and many studies have been reported, showing that coronal and sagittal deformities often involve sagittal cervical unbalance. Global sagittal balance aims to obtain a horizontal gaze and gravity line at top of hips when subject is in a static position, involving adjustment of each spine curvature in the sagittal plane. To our knowledge, no study did use a methodologically validated imaging analysis tool able to appreciate sagittal spine contours and distances in AIS and especially in the cervical region.
Methods
Lateral full-spine low-dose EOS radiographs were performed in 75 patients divided in three groups (control subjects, AIS, operated AIS). Three observers digitally analyzed twice each radiograph and 11 sagittal measures were collected for each image. Reliability was assessed calculating intraobserver Pearson’s r correlation coefficient, interobserver intra-class correlation coefficient (ICC) completed with a two-by-two Bland–Altman plot analysis.
Results
This measurement method has shown excellent intra and interobserver reliability in all parameters, sagittal curvatures, pelvic parameters and global sagittal balance.
Conclusions
This study validated a simple and efficient tool in AIS sagittal contour analysis. It defined new relevant landmarks allowing to characterize cervical segmental curvatures and cervical involvement in global balance.
Keywords: Adolescent idiopathic scoliosis, Sagittal balance, Cervical spine
Introduction
Adolescent idiopathic scoliosis (AIS) is a tridimensional deformity, altering frontal and sagittal contours. A thoracic kyphosis decrease is often reported, which is very difficult to correct surgically [1]. As shown in several studies, thoracic kyphosis is correlated to lumbar lordosis in adults [2, 3]. Thus, cervical lordosis and thoracic kyphosis should also correlate to assume a globally balanced spine in the sagittal plane.
Cervical spine remains poorly studied in AIS and it is clinically relevant to focus on cervical sagittal alignment before and after surgical correction of AIS, as it can be responsible for cervical degenerative pathologies [4]. Moreover, a recent study trends to demonstrate that hypokyphotic thoracic AIS spines are associated with hypolordotic to kyphotic cervical spines [5]. In order to be able to appreciate these correlations and the postoperative changes of the major components of sagittal balance, it appeared necessary to characterize reliable radiological landmarks. This study aims to define reliable radiological sagittal landmarks when analyzing cervical spine and global balance on AIS spines, native and instrumented.
Materials and methods
Patients
Following institutional review board approval, 50 consecutive patients followed at our institution for Lenke type 1 or 2 AIS were prospectively analyzed. Two groups were individualized: non-operated AIS and operated AIS. 25 non-operated AIS subjects and 25 operated AIS patients who had undergone posterior arthrodesis using hybrid constructs, combining pedicle screws (Instinct, ZimmerSpine, Bordeaux, France) at lumbar levels and Universal Clamps (ZimmerSpine, Bordeaux, France) at thoracic levels [6] were included.
Control patients
Twenty-five control subjects were randomly chosen from institution’s imaging database. Subjects were matched for age and gender. Inclusion criteria were age between 7 and 18, availability of full-spine EOS radiographs in standard standing position. All control subjects underwent full-spine imaging for screening of siblings in AIS families. Control subjects presenting a spinal deformity in frontal/sagittal plane, transitional anomaly, spondylolisthesis or uncommon bone density were excluded.
Radiological analysis
All patients underwent standing EOS (EOS imaging, Paris, France) biplanar stereoradiographs. Standard standing position was defined by straight-ahead look and fists on clavicles to avoid superposition of the arms over the spine [7]. Images acquisitions were made from orbits to the upper third of femurs. Radiographs that did not include spine from orbits to coxofemoral joints were excluded.
A widespread radiological visualization tool was used to analyze each image and perform measurements of angles and distances (Kodak Carestream, Rochester, NY, USA). The 75 EOS radiographs were analyzable. When needed, variation of contrast and luminosity helped to optimally reveal bone landmarks.
Full-spine radiographs were analyzed twice in a randomized order at 1-week interval by three independent observers: a senior pediatric spine surgeon, a senior pediatric radiologist and an orthopedic resident (total: 4,950 measures).
Five full-spine lateral radiographs were used by the three observers as a common training and then excluded from the study. Each observer collected eleven angles and distances for each patient. The following spinal parameters were measured (Fig. 1).
C1C3 angle: measured between a line joining the upper extremity of the C1 anterior arch and the upper extremity of the C1 posterior arch and the lower endplate of C3
C3C7 angle: measured between the upper endplate of C3 and the lower endplate of C7 (Fig. 2).
C2C6 angle: measured between the lower endplate of C2 and the lower endplate of C6, as described by Hilibrand et al. [8].
T1T12 thoracic kyphosis and L1L5 lumbar lordosis were calculated, as well as pelvic parameters (pelvic version and pelvic incidence) according to Guigui et al. [2] description.
The following parameters reflecting sagittal balance were measured (Fig. 3).
C7 plumb line (C7PL): horizontal distance between the posterosuperior angle of S1 and a vertical line through the middle of C7 inferior endplate
External auditory canal plumb line (CAEPL): horizontal distance between the postero-superior angle of S1 superior endplate and a plumb line drawn from the middle of the segment uniting external auditory canals
External auditory canal-hips (CAEH): horizontal distance between plumb line drawn from the middle of the segment uniting external auditory canals/plumb line drawn from the middle of the segment uniting femoral heads
CAEPL-C7PL distance (CAEC7): horizontal distance between plumb line drawn from the middle of the segment uniting external auditory canals/vertical line through middle of inferior C7 endplate.
Fig. 1.

Cervical spinal sagittal angles. Upper cervical lordosis (C1C3), global cervical lordosis (C2C6), lower cervical lordosis (C3C7) on plain EOS lateral radiographs
Fig. 2.
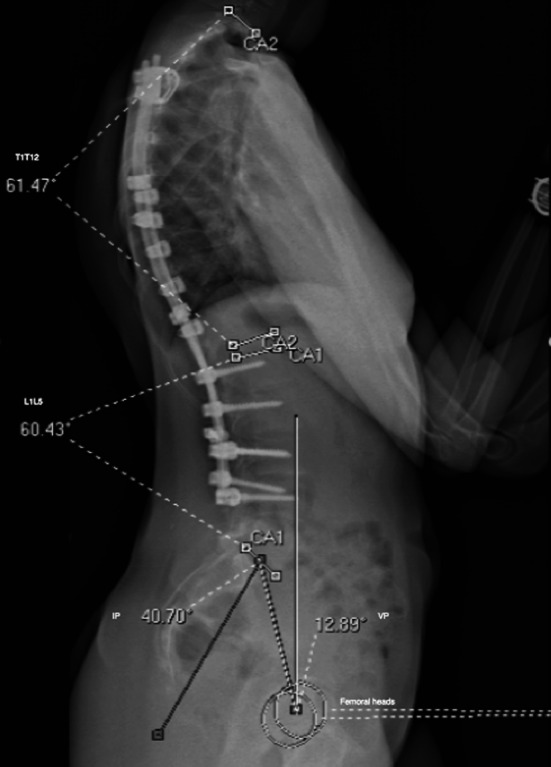
Thoracic kyphosis (T1T12), lumbar lordosis (L1L5), pelvic incidence (IP), pelvic version (VP) on plain EOS lateral radiographs
Fig. 3.
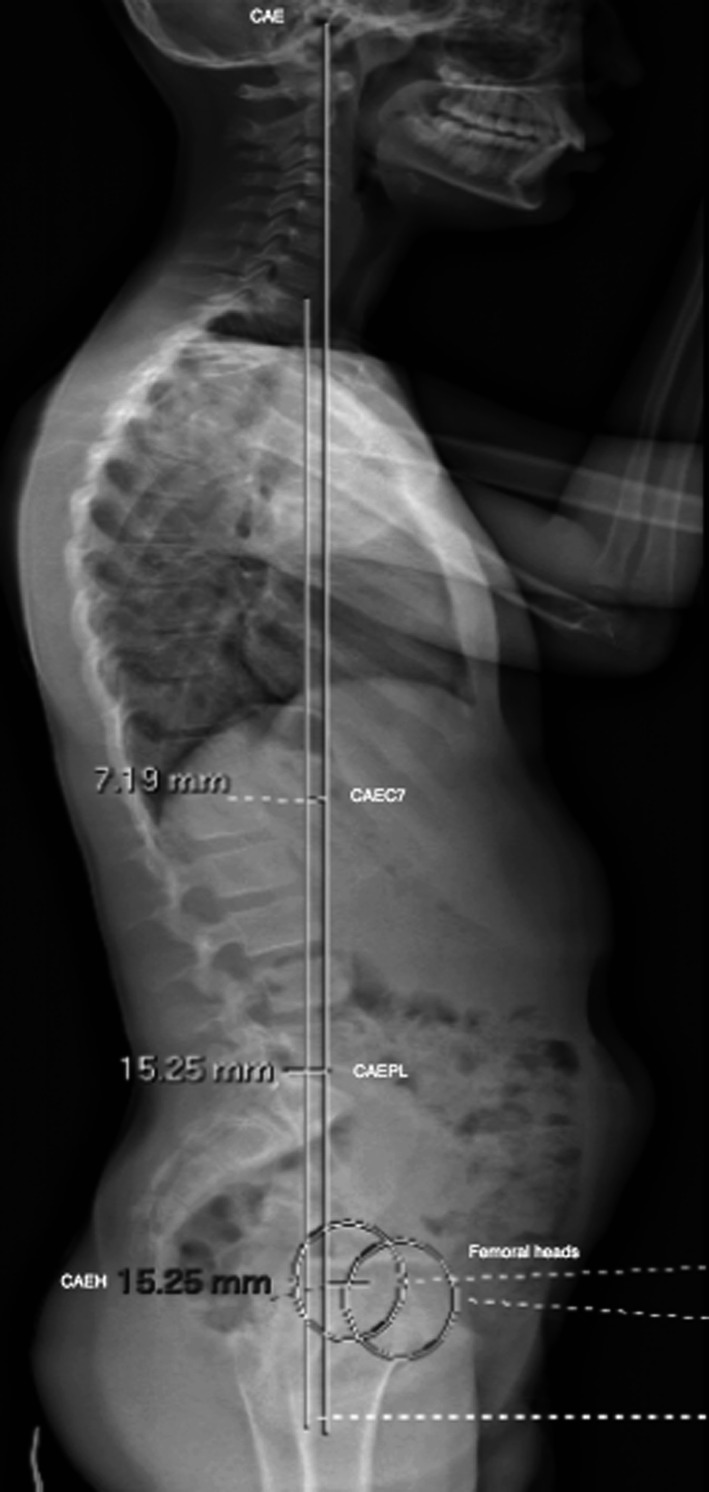
Global sagittal distances. External auditory canal plumb line (CAEPL), external auditory canal-C7 translation (CAEC7), external auditory canal-hips distance (CAEH), C7 plumb line on EOS lateral radiographs.
Statistical analysis
Statistical analysis was performed on Graphpad Prism v5 (GraphPad Software Inc. La Jolla, CA, USA). Intraobserver correlation was assessed with Pearson’s r linear regression coefficient. Interobserver correlation coefficient (ICC) was used to assess interobserver reproducibility, completed with Bland–Altman plot [9, 10] for detection of systemic errors, comparing pairs of examiners. ICC coefficient illustrates the proportion of the global variability that is due to the variability among subjects. According to Rosner et al. [11], an ICC value of less than 0.40 indicates poor reproducibility, values in the range 0.40–0.75 indicate fair good reproducibility and values greater than 0.75 show excellent reproducibility.
Comparisons of Pearson’s r in each group of patients (i.e. control, non-operated AIS and operated AIS) were made using Student’s t test. Statistical significance was set at p < 0.05.
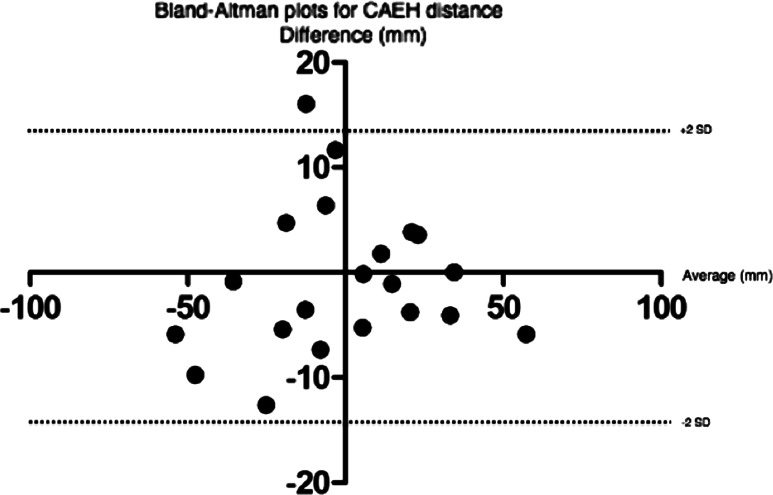
Bland and Altman plot gave a graphical approach of the bias existing between the data of two examiners and allowed to detect specific differences (agreement between observers depending on the measured distance or angle value) that were not shown by ICC.
Results
Demographic results (Table 1)
Table 1.
Demographic data
| Control | Non-operated AIS | Operated AIS | p | |
|---|---|---|---|---|
| Age (years) | ||||
| Mean | 12.24 | 11.69 | 12.04 | n.s. |
| SD | 3.21 | 1.13 | 2.56 | n.s. |
| Sex ratio | 17F/8 M | 19/6 M | 18F/7 M | n.s. |
No difference was found between the three groups
AIS adolescent idiopathic scoliosis
Mean age in the control group was 12.24 ± 3.21 years. Sex ratio was 17 girls for 8 boys. Age in the non-operated AIS group averaged 11.7 ± 1.1 years. Sex ratio was 19 girls for 6 boys. Mean age in the operated group was 12 ± 2.5 years. Sex ratio was 18 girls for 7 boys. No significant difference on demographic data was noted between the three groups.
Radiographic results
Intra and interobserver reproducibility in each group of patients is summarized in Table 2. There was no significant difference of ICC between the three groups of patients, meaning that inter and intraobserver reliability were not affected by the deformity and/or spinal instrumentation.
Table 2.
Comparison of correlation coefficient mean (Pearson’s r) in test patients, non-operated AIS (n/o AIS) and operated AIS for each examiner and among the three examiners
| Test | n/o AIS | Operated AIS | ||
|---|---|---|---|---|
| Examiner 1 | ||||
| r mean | 0.934 | 0.901 | 0.947 | n.s. |
| r SD | 0.031 | 0.078 | 0.033 | |
| Examiner 2 | ||||
| r mean | 0.875 | 0.853 | 0.903 | n.s. |
| r SD | 0.044 | 0.108 | 0.097 | |
| Examiner 3 | ||||
| r mean | 0.912 | 0.893 | 0.955 | n.s. |
| r SD | 0.046 | 0.079 | 0.039 | |
| Interexaminer | ||||
| r mean | 0.918 | 0.938 | 0.959 | n.s. |
| r SD | 0.012 | 0.044 | 0.039 | |
No intraobserver or interobserver correlation difference was found among the three groups
Overall values (Table 3): for examiner 1, r values ranged from 0.889 (±2 standard deviation (SD): 0.8616–0.9768) to 0.999 (0.9992–0.9999), best r value was obtained for CAEPL and worst was obtained for C2C6.
Table 3.
Overall intra (r) and interobserver reliability (ICC Intraclass Correlation Coefficient) with confidence interval (CI)
| Examiner 1 | Examiner 2 | Examiner 3 | Interobserver | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| r | 95 % CI | p | r | IC 95 % | p | r | IC 95 % | p | ICC | p | |
| C1C3 | 0.949 | 0.9356–0.9896 | <10−4 | 0.932 | 0.9150–0.9861 | <10−4 | 0.955 | 0.9437–0.974 | <10−4 | 0.954 | <10−4 |
| C3C7 | 0.917 | 0.8962–0.9829 | <10−4 | 0.879 | 0.8500–0.9748 | <10−3 | 0.892 | 0.8794–0.9436 | <10−3 | 0.846 | <10−3 |
| C2C6 | 0.889 | 0.8616–0.9768 | <10−3 | 0.847 | 0.8106–0.9676 | <10−4 | 0.871 | 0.8534–0.9222 | <10−3 | 0.947 | <10−4 |
| T1T12 | 0.910 | 0.8872–0.9813 | <10−3 | 0.840 | 0.8027–0.9661 | <10−4 | 0.934 | 0.9121–0.9674 | <10−4 | 0.803 | <10−4 |
| L1L5 | 0.947 | 0.9341–0.9893 | <10−4 | 0.911 | 0.8890–0.9817 | <10−3 | 0.953 | 0.9437–0.9721 | <10−4 | 0.843 | <10−3 |
| VP | 0.962 | 0.9517–0.9922 | <10−4 | 0.809 | 0.7650–0.9589 | <10−4 | 0.933 | 0.8568–0.9836 | <10−4 | 0.937 | <10−3 |
| IP | 0.944 | 0.8862–0.9813 | <10−4 | 0.894 | 0.8067–0.9561 | <10−3 | 0.922 | 0.8568–0.9846 | <10−4 | 0.948 | <10−4 |
| C7PL | 0.998 | 0.9972–0.9996 | <10−4 | 0.936 | 0.9200–0.9870 | <10−4 | 0.965 | 0.9457–0.9721 | <10−4 | 0.991 | <10−4 |
| CAEPL | 0.999 | 0.9992–0.9999 | <10−4 | 0.947 | 0.933–0.9892 | <10−4 | 0.964 | 0.9093–0.984 | <10−4 | 0.967 | <10−4 |
| CAEH | 0.997 | 0.9959–0.9994 | <10−4 | 0.924 | 0.8879–0.97137 | <10−4 | 0.965 | 0.9192–0.9866 | <10−4 | 0.971 | <10−4 |
| CAEC7 | 0.997 | 0.9959–0.9994 | <10−4 | 0.953 | 0.9407–0.9904 | <10−4 | 0.927 | 0.8739–0.9546 | <10−4 | 0.905 | <10−3 |
| Mean | 0.955 | 0.897 | 0.935 | 0.919 | |||||||
| SD | 0.038 | 0.046 | 0.029 | 0.059 | |||||||
All parameters show excellent intra and interobserver reproducibility
For examiner 2, r ranged from 0.840 (0.8027–0.9661) to 0.953 (0.9407–0.9904), best value was CAEC7 and worst was T1T12. For examiner 3, r values ranged from 0.871 (0.8534–0.9222) to 0.965 (0.9192–0.9866). Highest value was obtained for CAEH distance and worst for C2C6 angle. Interobserver ICC ranged from 0.803 (T1T12 angle) to 0.991 (C7PL distance), showing excellent interobserver reliability.
Bland–Altman plot analysis depicted the difference between two observers against the average angle (or distance) from two observers on the same radiograph. Dots included between the +2 SD and −2SD lines are considered as excellent interobserver agreement marks. This analysis showed no systemic error between examiners when reviewed by pairs. An example is shown on Fig. 4.
Fig. 4.
Bland–Altman plots graph for CAEH distance between observer 1 and observer 3. No major difference, good interobserver reproducibility
Discussion
To our knowledge, no reproducibility study has been conducted prior using radiological anatomical cervical spine landmarks, even the latest [4], and it appeared necessary to assess reliability of the chosen landmarks as well as the software used in the present study before manipulating them for further analysis.
Choice of landmarks
Lumbar and thoracic sagittal Cobb angles
The present reproducibility study used widely described lumbar and thoracic sagittal Cobb angles to evaluate lordosis and kyphosis. Intra and interobserver reproducibility found on these parameters in this work was comparable with those obtained using conventional radiographs [12].
Cervical sagittal Cobb angles
Cervical lordosis was assessed by the classical C2C6 angle [8], but is has been also chosen to distinguish the upper cervical lordosis (C1C3 angle) and the lower cervical lordosis (C3C7 angle). Dividing cervical lordosis with C3 threshold has the interest of separating the upper and more mobile cervical spine and the lower cervical spine. C1C3 angle reflects head position and particularly orbits position while subject is gazing toward the horizontal. The upper cervical spine, because of its very mobile character, needed a properly conducted reproducibility test. Lower cervical lordosis angle (C3C7) is less variable than C1C3 angle and more directly linked to thoracic cervical curvature. C3C7 angle is though a reflect of sagittal adaptive changes due to underlying spine. Excellent reliability was found in the current study on these cervical sagittal parameters (intraobserver r ranged from 0.847 to 0.955, ICC ranged from 0.846 to 0.954).
Interest of CAE landmark
Studies focusing on spinal sagittal balance mainly use the C7 plumb line to estimate the global sagittal balance. External auditory canals (CAE) are anatomically located at the top of cervical spine. Its sagittal position can easily define a relevant global sagittal balance landmark. Moreover, identification of CAE on lateral full-spine radiographs is easy, but not always shown on conventional radiographs because of the need to limit patients’ irradiation.
Measures of sagittal distances using CAE showed excellent reliability (intraobserver Pearson’s r ranged from 0.924 to 0.999 and ICC ranged from 0.905 to 0.971), indicating that CAE are usable as reliable radiological landmarks when examining global sagittal balance of the spine.
Low-dose biplanar imaging system (EOS)
Global sagittal spine contour can be easily analyzed with an excellent reliability using EOS as demonstrated in the present study. Two-dimensional spine imaging EOS is interesting for numerous reasons. It allows excellent numerical radiographic acquisitions in a short time and is six to nine times less radiating than conventional radiographs [13]. It is easier though to have more extended radiographs showing full cervical spine and head with CAE. Since the acquisition is directly bidimensional (X-rays source and detector have a synchronised parallel translation movement), distances and angles measurements can be performed without projectional bias [14].
EOS acquisition lasts 10–15 s for full-spine radiographs, depending on subject’s height. Subjects are supposed not to breathe during this acquisition time, and no image quality problem was found in the 75 patients.
Imaging analysis software
All images were analyzed with a simple and widespread numerical imaging software, installed on every computer of our institution. This software is currently used to analyze conventional radiographs and to measure distances and angles. The reproducibility results found in this study indicate that it is possible—and reliable—to use a very simple imaging numerical tool to assess sagittal contour analysis.
Statistical analysis
ICC was used instead of kappa correlation coefficient to be able to analyze data from three different observers with a robust enough and adapted statistical tool.
Bland–Altman plot was used as a graphical approach allowing to directly visualize agreement between two observers according to the value of the measure. This method can accurately identify interobserver bias when an examiner systematically overevaluates the measure, which could not be detected by other simple statistical tests. Eleven parameters on 75 subjects read by three observers analyzed with two-by-two Bland–Altman plot made 99 graphs, and it has been chosen not to represent them all in this paper as their result is roughly identical from one to another.
Influence of posterior instrumentation on reproducibility
One may ask if the presence of posterior instrumentation could influence reproducibility, leading to misplacement of bony landmarks on the vertebrae in a lateral view. It has been recently proven that the presence of posterior construct does not induce repeatability differences on sagittal measures at thoracic and lumbar levels on 3D reconstructions using EOS system [15]. Excellent intra and interobserver reproducibility was found on all sagittal parameters postoperatively. Furthermore, no reproducibility difference was found between the three groups (Table 2). These findings indicate that neither the presence of a posterior instrumentation nor sagittal or rotational deformity of the spine influence the reliability of the radiological sagittal parameters that were evaluated in the present study.
Limitations of the study
The present study validates a simple tool to analyze sagittal contour and particularly cervical alignment and global balance of AIS patients. The fifty AIS subjects chosen in this study were classified as Lenke 1 or 2. Other scoliotic deformity types were not assessed, and reproducibility of cervical parameters might be lower on Lenke type 4, as the proximal curve induces more rotated vertebral bodies and more difficult identification of radiological landmarks. The aim of this study was to validate a tool in order to be fully able to use it in further works about sagittal alignment of cervical spine. It has been chosen to analyse twenty-five patients for each category as this effective gave enough power for inter and intraobserver agreement assessment [11].
Conclusion
In conclusion, this study demonstrated that cervical lordosis and global sagittal spine balance in AIS can be reliably measured with a simple and widespread tool with a very satisfying agreement rate.
Cervical spine sagittal alignment can be appreciated with C1C3 angle for the upper and mobile cervical spine, C3C7 angle for the lower cervical spine and C2C6 for the global sagittal curve. Dividing cervical spine in three regions allows to individualize sagittal curvature due to head position.
CAE were shown to be reliable landmarks for global sagittal spinal alignment. Plumb lines and sagittal distances using CAE as described here are of major interest when measuring sagittal global spine balance as they take into account cervical participation on sagittal balance, which had not been described earlier.
Low-dose biplanar radiographic systems allow obtainment of large full-spine radiographs with much less irradiation, which is of major interest in AIS population who usually undergo long-term radiographic follow-up. Validating this tool permits to use it in further studies, and particularly in assessing cervical spine sagittal changes after corrective surgery in AIS.
Conflict of interest
None.
References
- 1.Sucato DJ, Agrawal S, O’Brien MF, et al. Restoration of thoracic kyphosis after operative treatment of adolescent idiopathic scoliosis: a multicenter comparison of three surgical approaches. Spine. 2008;33(24):2630–2636. doi: 10.1097/BRS.0b013e3181880498. [DOI] [PubMed] [Google Scholar]
- 2.Guigui P, Levassor N, Rillardon L, et al. Physiological value of pelvic and spinal parameters of sagittal balance: analysis of 250 healthy volunteers. Rev Chir Orthop Reparatrice Appar Mot. 2003;89(6):496–506. [PubMed] [Google Scholar]
- 3.Vialle R, Levassor N, Rillardon L, et al. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Jt Surg Am. 2005;87(2):260–267. doi: 10.2106/JBJS.D.02043. [DOI] [PubMed] [Google Scholar]
- 4.Canavese F, Turcot K, De Rosa V, et al. Cervical spine sagittal alignment variations following posterior spinal fusion and instrumentation for adolescent idiopathic scoliosis. Eur Spine J. 2011;20(7):1141–1148. doi: 10.1007/s00586-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hwang SW, Samdani AF, Tantorski M, et al. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine. 2011;15(5):491–496. doi: 10.3171/2011.6.SPINE1012. [DOI] [PubMed] [Google Scholar]
- 6.Ilharreborde B, Even J, Lefevre Y, et al. Hybrid constructs for tridimensional correction of the thoracic spine in adolescent idiopathic scoliosis: a comparative analysis of universal clamps versus hooks. Spine. 2010;35(3):306–314. doi: 10.1097/BRS.0b013e3181b7c7c4. [DOI] [PubMed] [Google Scholar]
- 7.Faro FD, Marks MC, Pawelek J, et al. Evaluation of a functional position for lateral radiograph acquisition in adolescent idiopathic scoliosis. Spine. 2004;29(20):2284–2289. doi: 10.1097/01.brs.0000142224.46796.a7. [DOI] [PubMed] [Google Scholar]
- 8.Hilibrand AS, Tannenbaum DA, Graziano GP, et al. The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop. 1995;15:627–632. doi: 10.1097/01241398-199509000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Altman DG, Bland JM. Measurement in medicine: the analysis of method comparison studies. Statistician. 1983;32:307–317. doi: 10.2307/2987937. [DOI] [Google Scholar]
- 10.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–160. doi: 10.1191/096228099673819272. [DOI] [PubMed] [Google Scholar]
- 11.Rosner B. Fundamentals of biostatistics. Belmont: Duxbury Press; 2005. [Google Scholar]
- 12.Gelb DE, Lenje LG, Bridwell KH, et al. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20(12):1351–1358. [PubMed] [Google Scholar]
- 13.Dubousset J, Charpak G, Dorion I, et al. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med. 2005;189(2):287–297. [PubMed] [Google Scholar]
- 14.Deschênes S, Charron G, Beaudoin G, et al. Diagnostic imaging of spinal deformities: reducing patients radiation dose with a new slot-scanning X-ray imager. Spine. 2010;35(9):989–994. doi: 10.1097/BRS.0b013e3181bdcaa4. [DOI] [PubMed] [Google Scholar]
- 15.Ilharreborde B, Steffen JS, Nectoux E, et al. Angle measurement reproducibility using EOS three-dimensional reconstructions in adolescent idiopathic scoliosis treated by posterior instrumentation. Spine. 2011;36(20):E1306–E1313. doi: 10.1097/BRS.0b013e3182293548. [DOI] [PubMed] [Google Scholar]