Abstract
Purpose
Sagittal malalignment is frequently observed in adult scoliosis. C7 plumb line, lumbar lordosis and pelvic tilt are the main factors to evaluate sagittal balance and the need of a vertebral osteotomy to correct it. We described a ratio: the lumbar lordosis index (ratio lumbar lordosis/pelvic incidence) (LLI) and analyzed its relationships with spinal malalignment and vertebral osteotomies.
Methods
53 consecutive patients with a surgical adult scoliosis had preoperative and postoperative full spine EOS radiographies to measure spino-pelvic parameters and LLI. The lack of lordosis was calculated after prediction of theoretical lumbar lordosis. Correlation analysis between the different parameters was performed.
Results
All parameters were correlated with spinal malalignment but LLI is the most correlated parameter (r = −0.978). It is also the best parameter in this study to predict the need of a spinal osteotomy (r = 1 if LLI <0.5).
Conclusion
LLI is a statistically validated parameter for sagittal malalignment analysis. It can be used as a mathematical tool to detect spinal malalignment in adult scoliosis and guides the surgeon decision of realizing a vertebral osteotomy for adult scoliosis sagittal correction. It can be used as well for the interpretation of clinical series in adult scoliosis.
Keywords: Adult scoliosis, Pelvic incidence, Lumbar lordosis, Fixed sagittal malalignment, Lumbar lordosis index
Introduction
The loss of lumbar lordosis increases disability and pain [1, 2] even when sagittal balance is preserved [3]. Adult scoliosis is associated with hypo-lordosis and is an often source of sagittal malalignment [2, 4, 5]. The loss of lumbar lordosis initiates sagittal imbalance pushing the C7 plumb line forwards [6]. Compensatory mechanisms, involving spinal column, pelvis and lower extremities, can limit the C7 plumb line going forwards. An ideal sagittal balance can be defined as a C7 plumb line less than 5 cm from the posterior corner of the top margin of S1 [7] and a pelvic tilt <25° [8]. Treatment of fixed sagittal malalignment in adult degenerative scoliosis can require a spinal osteotomy to regain global balance [9]. The main osteotomies are Smith Petersen Osteotomy (SPO) and Pedicle Subtraction Osteotomy (PSO) [10]. A preoperative planning is needed to determine the type, size and location of the osteotomy. Several methods exist [11, 12], but there are few simple parameters to help surgeons decide the need of realizing an osteotomy to regain spinal alignment. Sagittal malalignment can be appreciated by the measure of lumbar lordosis (LL), pelvic tilt (PT) and sagittal vertical axis (SVA) (Fig. 1) [12]. In the Adult Scoliosis Classification described by Schwab et al. [13], those parameters are correlated with patient disability. But their impact on treatment has not been tested. In Schwab’s classification, a lumbar lordosis <40° or a SVA distance over 9.5 cm are considered as pejorative factors.
Fig. 1.
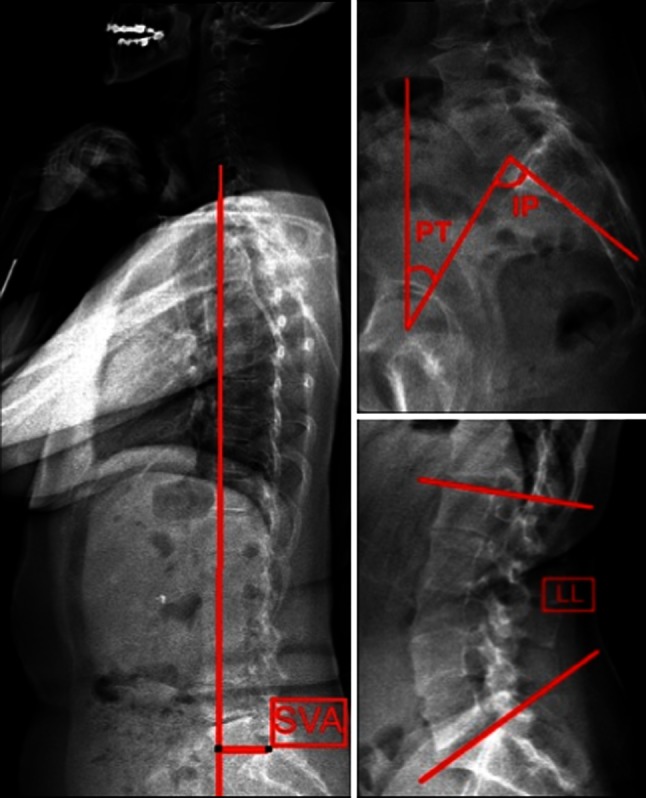
Radiographic parameters to evaluate sagittal malalignment
The relationship between lumbar lordosis and pelvic incidence is nowadays admitted [14]. Lumbar lordosis tends to decrease with aging process, as pelvic incidence remains constant for a given human being [14]. Since the loss of lumbar lordosis initiates spinal malalignment, we decided to evaluate the impact of a new mathematical ratio, called the lumbar lordosis index (LLI). This index is the ratio between two existing parameters: lumbar lordosis and pelvic incidence. Our hypothesis is that LLI is highly correlated with spinal malalignment in adult scoliosis and that it can have a clinical impact in predicting the need of a spinal osteotomy in adult scoliosis to restore sagittal balance. The purpose of this study is not to demonstrate a new method to calculate the correction needed in degrees but to evaluate the relationship between LLI, PT, SVA, LL, and spinal malalignment in adult scoliosis.
To assess our hypothesis we will try to answer to two questions: which parameter is most correlated with spinal malalignment between: PT, SVA, lumbar lordosis, and LLI in an adult scoliosis population? Which parameter is the most correlated with the performance of a spinal osteotomy to restore a proper balance in adult scoliosis?
Materials and methods
Since pelvic incidence is specific to a human being and lumbar lordosis related to pelvic incidence, several authors proposed formulas to predict theoretical lumbar lordosis based on the pelvic incidence, which remains constant during adulthood [15, 16]. We used two formulas proposed by Duval-Beaupère and co-workers to determine the ideal lordosis [17, 18]. The lack of lordosis was the difference between the theoretical lordosis and the measured lumbar lordosis. As it has already been done in the literature [19], we thought that the best way to evaluate the correlation between the spino-pelvic parameters described above and spinal malalignment was to compare them with the lack of lordosis as spinal malalignment can be represented by lack of lordosis.
Inclusion criteria were all adults (age over 18 years old) with a lumbar or thoracolumbar scoliosis (degenerative or evolving idiopathic scoliosis in adulthood) requiring an extensive fusion. Exclusion criteria were previous spine surgery with fusion, neurologic disease (Parkinson), and thoracic scoliosis. All eligible patients were included in this study. For each patient, a preoperative computerized planning was done to evaluate postoperative balance; the need of realizing an osteotomy (PSO or SPO) and to calculate in this last case the correction needed [11]. Peri-operative blood recuperation limited the needs of transfusion. Somatosensitive and motor-evoked potentials were performed in all surgeries. All patients had a thermoforming thoracolumbar orthotics for 3 months. The patients had preoperative and postoperative full length standing radiographs with the EOS low-dose system (Biospace, Paris, France) with a minimum 1-year radiographic follow-up [20]. Posture in the EOS device was in an easy standing position with fists overlaying ipsilateral clavicles. The following spino-pelvic parameters were measured:
Lumbar lordosis (LL): angle between the superior endplate of L1 and the endplate of S1.
Pelvic incidence (PI): angle between the perpendicular to the sacral plate at its midpoint and the line connecting this point to the femoral heads axis.
Pelvic tilt (PT): angle between the vertical and the line through the midpoint of the sacral plate to femoral head axis.
Sagittal vertical axis (SVA): distance in centimeters between C7 plumb line and posterior corner on the top margin of S1.
Lumbar lordosis index (LLI): ratio between lumbar lordosis and pelvic incidence LLI = LL/PI.
All sagittal measurements were considered positive if the curve was lordotic and negative if the curve was kyphotic.
The lack of lordosis described above and derived from the pelvic incidence was measured from two different formulas of theoretical ideal lumbar lordosis:
The ideal lumbar lordosis based on the formula described by Legaye et al.: LL = ((PI × 0.5481 + 12.7) × 1.087 + 21.61).
The ideal lumbar lordosis based on the formula described by Schwab et al.: LL = PI + 9.
In a second time our population was divided into two subgroups as those who underwent a spinal osteotomy (PSO or SPO) and those who did not. The first subgroup was composed of 18 patients and the second subgroup composed of 35 patients. In the first group, 6 patients underwent a SPO (4 one level SPO and 2 three level SPO) and 12 patients PSO (10 PSO on L4 and 2 PSO on L3). After evaluating that both groups had a correct postoperative balance, by comparing pre- and postoperative values, we evaluated which spinal or pelvic parameter had the most impact in predicting the need of a spinal osteotomy. Goal correction was an ideal sagittal balance with a SVA <5 cm and a PT <25° as described in the literature [7, 8, 21]. In the last part of our study, we evaluated the differences in the first subgroup between PSO and SPO.
Correlations between measurements were evaluated by Spearman correlation rank factor, and the significance was tested with the t test. A p < 0.05 was considered statistically significant.
Results
The study included 53 patients from a single center, included prospectively between January 2009 and December 2010. There were 46 female and 7 male patients with an average age of 61 years (range 27–79). The mean Cobb angle was 37.2° (range 17°–82.6°).
Radiographic measurements (Table 1)
Table 1.
Radiographic measurements
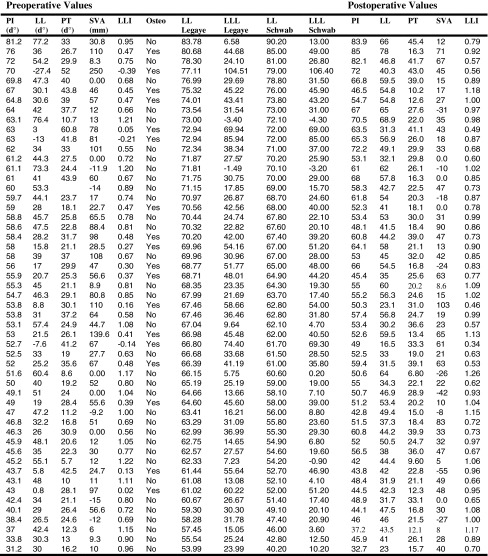
Population description (Table 2)
Table 2.
Patient’s radiographic parameters
| Measurement | Preoperative | Last follow-up | p |
|---|---|---|---|
| P. incidence | 55.28 (±10.83) | 56.29 (±10.87) | 0.3 |
| L. lordosis | 33.99 (±20.97) | 46.67 (±12.84) | <0.05 |
| SVA | 45.86 (±48.74) | 25.07 (±33.91) | <0.05 |
| Pelvic tilt | 27.56 (±11.34) | 25.20 (±9.68) | 0.12 |
| LLI | 0.63 (±0.37) | 0.84 (±0.20) | <0.05 |
Pelvic incidence was 55.28° (mean value) in preoperative and 56.29° in postoperative. There were no differences between these two values. Lumbar lordosis was 33.99° in preoperative and 46.67° in postoperative. SVA was 45.86 cm in preoperative and 25.07 cm in postoperative. Pelvic tilt was 27.56° in preoperative and 25.2° in postoperative. LLI was 0.63 in preoperative and 0.84 in postoperative. Except for PT and PI all other values were statistically different between pre- and postoperative.
Subgroups description (Table 3)
Table 3.
Radiographic parameters evaluating spino-pelvic parameter changes in osteotomy and non-osteotomy subgroups
| Osteotomy | No osteotomy | p* | |
|---|---|---|---|
| n = 18 | n = 35 | ||
| P. incidence | |||
| Preoperative | 57.68 (±8.64) | 53.42 (±10.83) | 0.1 |
| Postoperative | 57.02 (±10.95) | 55.9 (10.97) | 0.74 |
| p** | 0.72 | 0.2 | |
| L. lordosis | |||
| Preoperative | 13.47 (±17.10) | 44.85 (±13.15) | <0.05 |
| Postoperative | 45.39 (±14.90) | 47.35 (±11.79) | 0.69 |
| p** | <0.05 | 0.26 | |
| SVA | |||
| Preoperative | 79.76 (±53.20) | 27.36 (±34.05) | <0.05 |
| Postoperative | 34.24 (±37.70) | 20.08 (±31.12) | 0.2 |
| p** | <0.05 | 0.25 | |
| P. tilt | |||
| Preoperative | 34.57 (±11) | 24.07 (±9.58) | <0.05 |
| Postoperative | 24.60 (±10.87) | 25.63 (±9.12) | 0.75 |
| p** | <0.05 | 0.33 | |
| LLI | |||
| Preoperative | 0.23 (±0.27) | 0.84 (±0.2) | <0.05 |
| Postoperative | 0.8 (±0.24) | 0.85 (±0.18) | 0.5 |
| p** | <0.05 | 0.8 | |
| Lack LL Schwab | 56.3 (±17.35) | 17.18 (±11.69) | <0.05 |
| Lack LL Legaye | 53.21 (±18.33) | 22.18 (10.72) | <0.05 |
* Osteotomy versus no osteotomy
** Preoperative versus postoperative
LL, SVA, PT, LLI and Lack of LL were statistically different in the two subgroups for preoperative values. In the osteotomy subgroup, parameters changed comparing pre- and postoperative values. On the opposite, none of the parameters measured were changed in postoperative for the group without osteotomy. When we compare postoperative values there are no statistical difference between the two subgroups for PI, LL, SVA, PT, LLI. The mean postoperative SVA in the osteotomy subgroup is 34.24 and 20.08 mm in the subgroup without osteotomy. In both groups mean global balance is restored. Eight patients had an SVA over 5 cm. Five of them belonged to the osteotomy subgroups and presented a major malalignment where the mean correction was a gain of 32.3° of lordosis. The three others belonged to the subgroup without osteotomy. In these cases, the postoperative lordosis was inferior to the preoperative one explaining the raise of SVA.
Correlation between spino-pelvic parameters and lack of lumbar lordosis (Table 4)
Table 4.
Spearman correlation factor between lack of lordosis and preoperative spino-pelvic parameters
| ρ | p | |
|---|---|---|
| Lack of lordosis Schwab | ||
| Lumbar lordosis | −0.883 | 0.01 |
| Pelvic tilt | 0.736 | 0.01 |
| Sagittal vertical axis | 0.696 | 0.01 |
| Lumbar lordosis index | −0.978 | 0.01 |
| Lack of lordosis Legaye | ||
| Lumbar lordosis | −0.928 | 0.01 |
| Pelvic tilt | 0.635 | 0.01 |
| Sagittal vertical axis | 0.587 | 0.01 |
| Lumbar lordosis index | 0.988 | 0.01 |
LL, PT, SVA and LLI correlated with both formulas of lack of lordosis. With the two formulas the best correlation factor was found when lack of lordosis was correlated to LLI (p = 0.01). The most correlated parameter with lack of lordosis is LLI. Since lack of Lordosis represents spinal malalignment as described above we are able to conclude that LLI is more correlated with spinal malalignment than SVA, PT or LL in this study.
Correlation between spino-pelvic parameters and spinal osteotomies (Table 5)
Table 5.
Correlation between spino-pelvic parameters and spinal osteotomies
| Spearman correlation factor | Osteotomy | p |
|---|---|---|
| Lumbar lordosis <40° | 0.604 | <0.01 |
| Sagittal vertical axis >95 mm | 0.365 | <0.01 |
| Lumbar lordosis index <0.5 | 1 | <0.01 |
Lumbar lordosis <40° (r = 0.604) and SVA >95 mm (r = 0.365) correlated moderately with spinal osteotomies. With a correlation factor of one spinal osteotomies and LLI <0.5 factors are highly correlated. This result demonstrates a clinical impact of LLI in this study.
Relationship between the type of spinal osteotomy and lumbar lordosis index (Table 6)
Table 6.
LLI preoperative mean with SPO and OTP in spinal osteotomy subgroup
| Mean LLI | |
|---|---|
| SPO | 0.44 (±0.05) |
| PSO | 0.13 (±0.28) |
| Total | 0.23 (±0.27) |
The mean preoperative value of LLI in the osteotomy subgroup is 0.13 when a PSO is realized and 0.43 when a SPO is realized. A LLI <0.35 were associated with a PSO in all cases. When LLI >0.35; SPO or PSO was used.
Discussion
Adult scoliosis specific classifications appeared recently. After Aebi’s classification [22] based on scoliosis etiology, the SRS committee and F. Schwab proposed radiologic classifications. The Adult Scoliosis Classification [23] is interesting since the parameters, used to categorize patients, have a clinical impact on disability and pain. A lumbar lordosis <40° and a SVA distance >95 mm are the parameters dealing with sagittal malalignment. In this study, we evaluated their impact on treatment and their ability to be correlated with vertebral osteotomies. We also added a new mathematical ratio named LLI. The idea was to match pelvic incidence and lumbar lordosis since those two parameters are highly correlated and proper to a specific human being [1, 2, 24]. Since PI is not affected with aging a decrease of LLI reveals a decrease of LL. It seems difficult to compare LL alone since LL is specific to a given human being. The interest of LLI was to match lumbar lordosis with PI since PI is specific for a human being, correlated with LL, but not affected by aging. LLI offers the possibility to categorize patients and compare lumbar lordosis between patients. In this study, we established the relationship between LLI, PT, SVA, LL, and spinal malalignment represented by lack of lordosis. We also demonstrated a potential therapeutic impact of LLI in adult scoliosis and its association with spinal osteotomies. Sagittal malalignment can be found in adult scoliosis and needs to be detected to treat the deformity correctly. In our study, sagittal malalignment was represented by the lack of lordosis, as it has already been described [19].
We are not surprised to observe a high correlation between LL, SVA and vertebral osteotomies since vertebral osteotomies modifies LL to restore a correct SVA. But it appears clearly in our study, that the LLI is the most correlated parameter with lack of lordosis in adult scoliosis. In this series of patients, an adult scoliosis with a LLI <0.5 is always associated with a vertebral osteotomy and an adult scoliosis with a LLI above 0.5 was treated without a vertebral osteotomy. These results should not be applied for all adult scoliosis as a rule since LLI has only been tested on 58 patients with adult scoliosis, but these findings underline the potential therapeutic impact of LLI and its ability to categorize spinal malalignment.
In Table 2, regarding PT no statistical difference was found between preoperative and postoperative values. Table 2 represents the mean values for the entire population. In this group, many patients are well balance and will not change their PT after surgery explaining the lack of difference. On the contrary, mean LL and mean SVA are modified. The standard deviations of those parameters are much higher making it easier to establish statistical significant differences. In Table 3, mean value of PT is modified around 10 degree for the osteotomy subgroup. No statistical differences are observed for postoperative values of PT in the two subgroups.
LLI appears in our study to be a better parameter for sagittal malalignment assessment than the SVA. This can be explained by the fact that the C7 plumb line goes forward lately in the sagittal malalignment cascade [25]. Sagittal malalignment is a consequence in LL decrease and LLI changes will appear before the raise of SVA. But LLI cannot be used to predict the amount of correction in degree when a vertebral osteotomy is decided. LLI is useful to detect spinal malalignment but other parameters need to be taken into account like the spine stiffness, knee flexion, thoracic kyphosis and pelvic tilt. Mathematical or computerized methods already exist and the aim of LLI is not to replace them [11, 12]. Before realizing an adult scoliosis surgery, a preoperative planning must be done to decide the extension of the fusion, the amount of correction needed for sagittal balance treatment [11], the frontal plane correction and the decompression needed. LLI remains a very simple ratio, like the Cobb angle for coronal deformity, to detect spinal malalignment in adult scoliosis. It could integrate an adult scoliosis classification instead of LL where normal variations between individuals are too large to categorize patients.
To highlight the impact of LLI on treatment and reinforce its reliability, we analyzed it with another series of patients published by Rose et al. [7]. In this study, 17 patients with adult scoliosis were operated with an extensive fusion associated with a PSO. 15 patients had a LLI <0.5 and the two others had a LLI <0.55. These two patients had high pelvic incidence (over 74°). These results underline the impact of LLI on treatment in adult scoliosis. The choice of a spinal osteotomy in adult scoliosis cannot be realized solely with the LLI but it remains the most reliable radiologic parameter tested in both series.
Despite adult scoliosis is a frequent source of sagittal malalignment, it is not the only one. The choice of an adult scoliosis population was its opportunity to highlight two groups (osteotomy, no osteotomy) since all patients with adult scoliosis are not concerned by spinal malalignment. The impact of LLI makes it a reliable tool to integrate an adult scoliosis instead of LL. We thought it would have been a source of confusion to study all kinds of spinal malalignment and LLI could not then be used in an adult scoliosis classification. The natural evolution of adult scoliosis with no prior surgery made it an interesting process to study. Other studies could be useful to appreciate the impact of LLI in other sources of sagittal imbalance (disc aging, flat back syndrome…) and its ability to detect spinal malalignment. Relationships between LLI and low back pain could also be established in the future.
Conclusion
In adult scoliosis the lumbar lordosis index appears to be a statistically validated radiographic parameter to evaluate spinal malalignment in adult scoliosis with a true impact on treatment. The aim of LLI is not to substitute a preoperative planning to calculate the correction needed for osteotomies. It can be used as a mathematical tool to detect spinal malalignment in adult scoliosis and guides the surgeons in his choice of realizing a spinal osteotomy for sagittal balance correction. It can be used as well for the interpretation of clinical series in adult scoliosis instead of LL and could be added to a new adult scoliosis classification. Further studies using LLI could be done to evaluate its relationship with spinal malalignment with other series of patients.
Conflict of interest
None.
References
- 1.Gelb DE, Lenke LG, Bridwell KH, Blanke K, McEnery KW. An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. [PubMed] [Google Scholar]
- 2.Schwab FJ, Smith VA, Biserni M, Gamez L, Farcy JP, Pagala M. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine. 2002;27:387–392. doi: 10.1097/00007632-200202150-00012. [DOI] [PubMed] [Google Scholar]
- 3.Ploumis A, Liu H, Mehbod AA, Transfeldt EE, Winter RB. A correlation of radiographic and functional measurements in adult degenerative scoliosis. Spine. 2009;34:1581–1584. doi: 10.1097/BRS.0b013e31819c94cc. [DOI] [PubMed] [Google Scholar]
- 4.Joseph SA, Jr, Moreno AP, Brandoff J, Casden AC, Kuflik P, Neuwirth MG. Sagittal plane deformity in the adult patient. J Am Acad Orthop Surg. 2009;17:378–388. doi: 10.5435/00124635-200906000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5:9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]
- 6.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine. 2008;33:1572–1578. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 7.Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, et al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine. 2009;34:785–791. doi: 10.1097/BRS.0b013e31819d0c86. [DOI] [PubMed] [Google Scholar]
- 8.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine. 2009;34:1828–1833. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 9.Bridwell KH. Causes of sagittal spinal imbalance and assessment of the extent of needed correction. Instr Course Lect. 2006;55:567–575. [PubMed] [Google Scholar]
- 10.Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine. 2005;30:2030–2037. doi: 10.1097/01.brs.0000179085.92998.ee. [DOI] [PubMed] [Google Scholar]
- 11.Aurouer N, Obeid I, Gille O, Pointillart V, Vital JM. Computerized preoperative planning for correction of sagittal deformity of the spine. Surg Radiol Anat. 2009;31(10):781–792. doi: 10.1007/s00276-009-0524-9. [DOI] [PubMed] [Google Scholar]
- 12.Le Huec JC, Leijssen P, Duarte M, Aunoble S. Thoracolumbar imbalance analysis for osteotomy planification using a new method: FBI technique. Eur Spine J. 2011;20(S5):669–680. doi: 10.1007/s00586-011-1935-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwab F, Lafage V, Farcy JP, Bridwell K, Glassman S, Ondra S, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine. 2007;32:2723–2730. doi: 10.1097/BRS.0b013e31815a58f2. [DOI] [PubMed] [Google Scholar]
- 14.Duval-Beaupere G. Composante sagittale de la statque rachidienne. Revue de Rhumatologie. 2004;71:115–119. [Google Scholar]
- 15.Mangione P, Gomez D, Senegas J. Study of the course of the incidence angle during growth. Eur Spine J. 1997;6:163–167. doi: 10.1007/BF01301430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marty C, Boisaubert B, Descamps H, Montigny JP, Hecquet J, Legaye J, et al. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J. 2002;11:119–125. doi: 10.1007/s00586-001-0349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, Marty C, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–422. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Legaye J, Duval-Beaupere G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg. 2005;71:213–220. [PubMed] [Google Scholar]
- 19.Obeid I, Hauger O, Aunoble S, Bourghli A, Pellet N, Vital JM. Global analysis of sagittal spinal alignment in major deformities: correlation between lack of lumbar lordosis and flexion of the knee. Eur Spine J. 2011;20(S5):681–685. doi: 10.1007/s00586-011-1936-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dubousset J, Charpak G, Skalli W, Kalifa G, Lazennec JY. EOS stereo-radiography system: whole-body simultaneous anteroposterior and lateral radiographs with very low radiation dose. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:141–143. doi: 10.1016/S0035-1040(07)92729-4. [DOI] [PubMed] [Google Scholar]
- 21.Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance) Spine. 1999;24:1712–1720. doi: 10.1097/00007632-199908150-00013. [DOI] [PubMed] [Google Scholar]
- 22.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 23.Schwab F, Farcy JP, Bridwell K, Berven S, Glassman S, Harrast J, et al. A clinical impact classification of scoliosis in the adult. Spine. 2006;31:2109–2114. doi: 10.1097/01.brs.0000231725.38943.ab. [DOI] [PubMed] [Google Scholar]
- 24.Jackson RP, Simmons EH, Stripinis D. Incidence and severity of back pain in adult idiopathic scoliosis. Spine. 1983;8:749–756. doi: 10.1097/00007632-198310000-00011. [DOI] [PubMed] [Google Scholar]
- 25.Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J. 2011;20(S5):626–633. doi: 10.1007/s00586-011-1930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


