Abstract
Background
Ideal surgical treatment for hallux valgus is still controversial. A traditional distal metatarsal osteotomy with rigid fixation (Scarf procedure) and a more minimally invasive approach to a distal metatarsal osteotomy, termed SERI (Simple, Effective, Rapid, Inexpensive), have proven successful with short-term followup. However, no data are available directly comparing the two procedures.
Questions/Purposes
We performed a prospective randomized trial to determine which technique (SERI or Scarf) was associated with (1) better functional outcomes, (2) better radiographic correction, and (3) fewer complications at 2 and 7 years followup.
Methods
Twenty patients, 53 ± 11 years of age, with bilateral hallux valgus, clinically and radiographically similar, underwent bilateral surgery with Scarf on one side and SERI on the other, at random. Clinical (AOFAS score) and radiographic assessments were considered before surgery, and at 7 years followup.
Results
SERI and Scarf techniques provided correction of the hallux valgus angle, intermetatarsal angle, and distal metatarsal angle in the range of normal. Both led to similar clinically important improvements in the AOFAS. No differences were observed between the groups. All osteotomies healed, and two patients who underwent the Scarf procedure required hardware removal. Reduction of ROM with respect to preoperative was observed in three patients for SERI and three patients for Scarf procedures.
Conclusions
Scarf and SERI techniques resulted in effective correction of hallux valgus with similar outcomes, however the SERI technique required a shorter skin incision, less surgical time, less expensive fixation device, and was without residual pain attributable to hardware.
Level of Evidence
Level II, prospective comparative study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Hallux valgus is a common and disabling condition [6]. The aim of surgical correction of hallux valgus is to rebalance the first ray and correct the various features of the deformity [9–12]. Despite the common occurrence of this condition, treatment remains controversial with more than 150 surgical procedures described [2, 18, 20]. Distal first metatarsal osteotomies traditionally have been indicated for correction of mild-to-moderate deformities with an intermetatarsal angle (IMA) as much as 20° and for correction of the distal metatarsal articular angle (DMAA) [18]. The Scarf osteotomy is a distal first metatarsal osteotomy that is popular in Europe. It allows for the use of strong fixation and often is combined with other osteotomies and soft tissue procedures [5, 22]. There is a trend toward more minimally invasive approaches to distal metatarsal osteotomies that have the theoretical advantages of less soft tissue dissection and the need for only temporary hardware [3, 19].
One such approach is the SERI (Simple, Effective, Rapid, Inexpensive) osteotomy performed through a small incision under direct visual control that allows for fast and safe correction of the deformity [10]. Although one study reported the outcome of a single surgical procedure for hallux valgus [7], there is only one study between Scarf and a less invasive approach for a distal metatarsal osteotomy [16] and none to our knowledge, with long-term followup.
In this prospective randomized study, we sought to determine which technique (SERI or Scarf) was associated with (1) better functional outcomes, (2) better radiographic correction, and (3) fewer complications at 2 and 7 years followup.
Patients and Methods
The local medical ethics committee approved the study; all patients received oral and written study information. All the described devices are approved by FDA.
Twenty consecutive female patients, mean age of 53 ± 11 years, with bilateral hallux valgus clinically and radiographically were recruited for this study (Fig. 1). All patients underwent bilateral surgery in the same surgical setting, receiving SERI osteotomy on one foot and Scarf osteotomy on the other according to a randomly generated list.
Fig. 1.

The photograph shows the feet of a 35-year-old woman with bilateral hallux valgus deformities.
Inclusion criteria were patients between 20 and 70 years old with bilateral hallux valgus similar in severity in both feet. The hallux valgus angle (HVA) ranged from 15° to 40° and the IMA averaged less than 20°. All patients had adequate ROM of the first metatarsophalangeal (MTP) joint. All patients reported having pain and difficulty wearing shoes, with no benefit from conservative treatments. Patients were excluded if they had rheumatoid arthritis or other inflammatory diseases, previous hallux valgus surgery that failed, interphalangeal hallux valgus, symptomatic or radiographic evidence of arthritis of the MTP joint, or associated deformities in other joints of the foot. None of the patients had preexisting transfer lesions or first-ray hypermobility.
Clinical evaluation data were collected preoperatively, 24 months postoperatively, and at final followup 7 years after surgery using the AOFAS score [14].
Radiographic examination included dorsoplantar and lateral weightbearing views of the forefoot, allowing assessment of arthritis and congruency of the joint (Fig. 2). The measurement of HVA, IMA, and DMAA were evaluated preoperatively and at both followup periods [15]. Radiographic evaluation was performed according to standardized procedures. Measurement on the dorsoplantar weightbearing radiographs of the HVA, IMA, and DMAA were made. The HVA was measured as the angle between the line from the center of the metatarsal base to the center of the first metatarsal head and the line connecting the midpoints of the proximal and distal articular surfaces of the proximal phalanx. The IMA was measured as the angle between the line of the first metatarsal and the line bisecting the diaphyseal portions of the second metatarsal, and the DMAA describes the lateral slope of the articular surface in relation to the long axis of the first metatarsal.
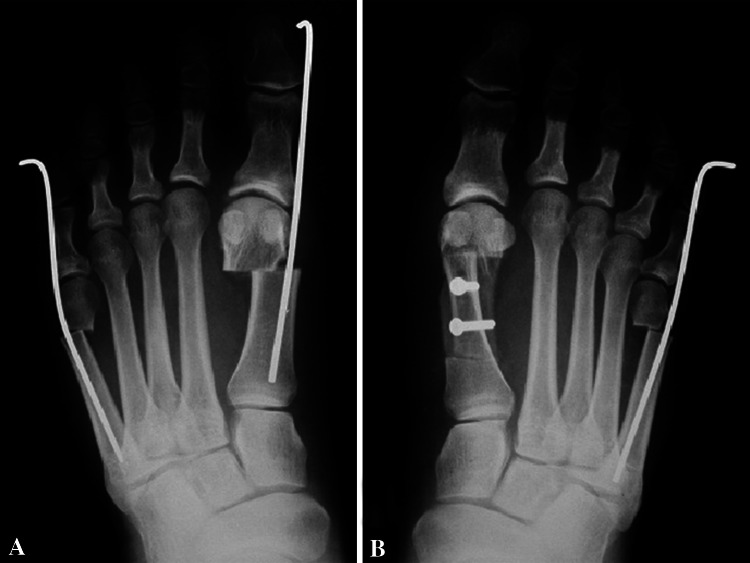
Fig. 2A–B.
Preoperative dorsoplantar weightbearing radiographs of the patient’s (A) left and (B) right feet show the deformities.
The surgical procedures were performed with the patient receiving local or block anesthesia, while in the supine position, and under tourniquet control. The foot is kept externally rotated with its lateral edge on the operating table. Manual stretching of the adductor hallucis is performed forcing the big toe into a varus position.
For SERI, a 1-cm medial incision is made just proximal to the medial eminence through the skin and subcutaneous tissue, down to the bone.
The osteotomy is performed using a standard pneumatic saw with a 9.5 × 25 × 0.4-mm blade. A 2-mm K wire is inserted using a normal drill passing through the incision into the soft tissue adjacent to the bone in a proximodistal direction along the longitudinal axis of the great toe. The K wire exits at the medial area of the tip of the toe approximately 5 mm below the medial border of the nail. The wire is advanced past the osteotomy allowing a small grooved lever to manipulate the osteotomy site and achieve correction of the deformity. Stabilization of the correction then is obtained by inserting the K wire into the diaphyseal channel in a distal-proximal direction until its proximal end reaches the metatarsal base. In two cases in the SERI group, the metatarsal head was slightly dislocated plantarly to reduce metatarsalgia.
If the proximal stump of the osteotomy is medially prominent, a small wedge of bone is removed. The skin is sutured with only one 3-0 reabsorbable stitch. The distal extremity of the K wire is curved and cut out of the tip of the toe. Duration of surgery was recorded.
For the Scarf ostetomy, a 3-cm medial incision is made from the medial eminence to the base of first ray through the skin and subcutaneous tissue. The Z osteotomy is performed using a standard pneumatic saw. The correction is obtained moving the distal stump of the metatarsal depending on the pathoanatomy of the deformity.
Two 3-mm screws are used for stabilizing the osteotomy site. If the proximal stump of the osteotomy is medially prominent, a small wedge of bone is removed. The skin is sutured with one 3-0 reabsorbable stitch (Fig. 3).
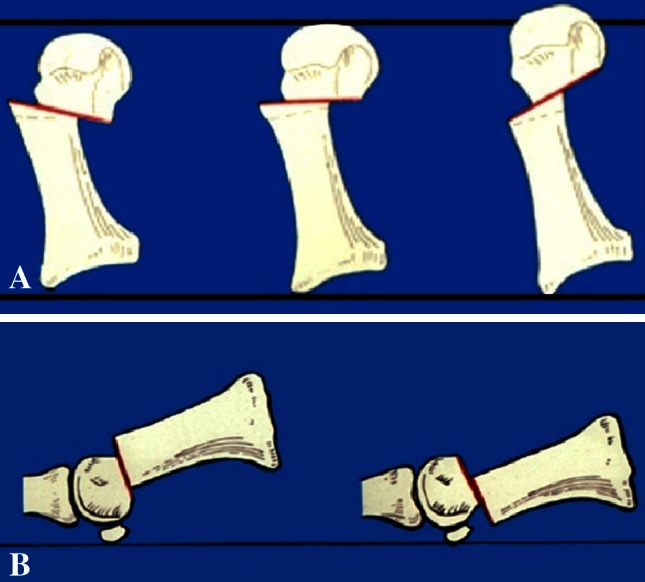
Fig. 3A–B.
Immediate postoperative radiographs of the patient’s feet show the correction obtained with the (A) SERI technique and (B) the Scarf technique.
With both techniques, by changing the inclination of the osteotomies, all the characteristics of the deformity were corrected (Fig. 4). In cases of first-ray insufficiency the distal fragment was displaced plantarward and when the first ray was overloaded the distal fragment was displaced dorsalward (Fig. 5).
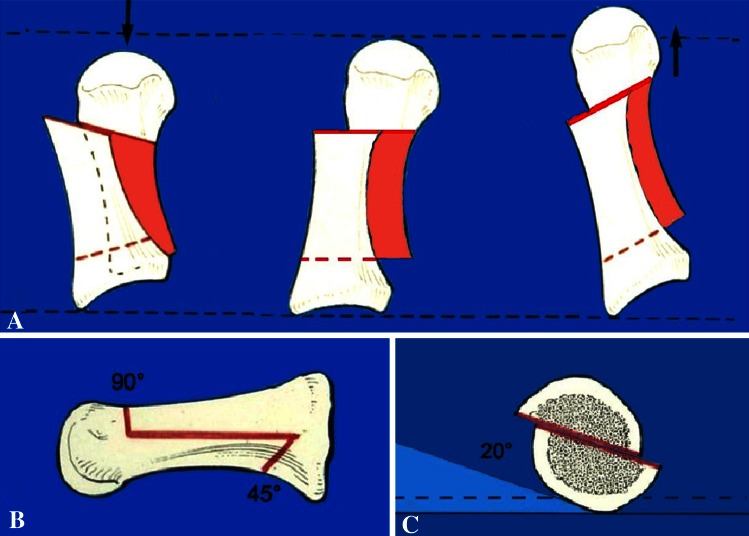
Fig. 4A–B.
The drawings show the SERI osteotomy technique. (A) In the dorsoplantar view, the inclination of the osteotomy in the mediolateral direction is perpendicular to the foot axis (the long axis of the second metatarsal bone) if the length of first metatarsal bone must be maintained. The osteotomy is inclined in a distal to proximal direction as much as 25° if shortening of the metatarsal bone or decompression of the metatarsophalangeal joint is necessary. If lengthening is necessary, the osteotomy is inclined 15° in a proximal to distal direction. (B) In the lateral view, the adjustment of the plantar or dorsal dislocation of the metatarsal head is possible fixing the osteotomy with the K wire in the upper, or more rarely in the lower, site with regard to the long axis of the metatarsal head.
Fig. 5A–C.
The drawings show the Scarf osteotomy technique. (A) The dorsoplantar view shows how to maintain or modify the length of first metatarsal bone. (B) The lateral view shows how to perform a correct osteotomy, and (C) the AP view shows how to correct a first ray insufficiency. The osteotomy must be performed with a 20°-angle and the distal portion is displaced plantarward.
Postoperative care was similar in both groups and consisted of a gauze bandage, with ambulation being allowed immediately using talus shoes for 30 days. After 1 month, comfortable normal shoes, cycling, and swimming were advised.
Results
All the patients underwent clinical and radiographic evaluations at 2 and 7 years after surgery (Fig. 6). According to the AOFAS score, the SERI group improved from 51 ± 10 preoperatively to 89 ± 10 at 2 years followup. At 7 years the AOFAS score for the SERI group was 81.2 ± 15.1. A significant improvement of 29.6 ± 22.3 points (p = 0.002), with respect to the preoperative score, was still evident even if a decrease of the clinical score was seen with time.
Fig. 6.

A photograph of the patient’s feet was taken at the 7-year followup.
The Scarf group preoperatively scored 48 ± 9 according to the AOFAS score and 87 ± 12 at 2 years followup. At 7 years the AOFAS score for the Scarf group was 77.6 ± 16.6. A significant improvement of 30.7 ± 15.7 points (p < 0.0005) with respect to preoperative score was evident even if a decrease of the clinical score was seen with time.
The HVA in the SERI group changed from 35.8° ± 3.5o to 21.8° ± 4.1o at 7 years followup, the IMA changed from 16.1o ± 3.9o to 6.8o ± 4.3o, and the DMAA changed from 21.7o ± 5.5o to 15.9o ± 5.4o. The HVA in Scarf group changed from 35.5° ± 4.7o to 20.1° ± 3.6o at 7 years followup, the IMA changed from 16.1o ±3.8o to 8.3o ± 3.4o, while the DMAA from 21.7o ± 8.4o to 15.0o ± 7.5o (Fig. 7).
Fig. 7A–B.
Dorsoplantar weightbearing radiographs of the (A) left and (B) right feet obtained at the 7-year followup shows maintenance of correction.
Two patients who underwent the Scarf procedure required hardware removal owing to intolerance, whereas reduction of ROM with respect to preoperative ROM was observed in three patients who had the SERI osteotomy and three who had the Scarf osteotomy. There was only one poor result (AOFAS score, 61), in a patient in the Scarf group, with arthritis and severely reduced ROM of the first MTP joint, with transfer metatarsalgia.
The average surgical time of the procedure was 17 minutes for the Scarf and three minutes for the SERI (p < 0.0005). No intraoperative or postoperative complications were found; in particular, no pin tract infections, nerve injury, or avascular necrosis of the first metatarsal head was recorded. All osteotomies had healed properly by the 6 months radiographic control.
Eight patients expressed their subjective preference for the SERI procedure because of the less-evident scar (Fig. 8).
Fig. 8A–B.

Photographs of the patient’s feet taken 7 years after surgery show the scar from the (A) Scarf osteotomy and the scar from the (B) SERI osteotomy, which had a smaller scar compared with the Scarf procedure.
Discussion
Numerous studies have been reported regarding different hallux valgus correction techniques, and a review of the literature reveals satisfaction with all the operations to be in the upper 80% level and higher [1, 2, 5, 13, 17, 18]. However, there is scant information in the literature directly comparing different techniques. In our prospective comparative study, a bilateral surgical procedure is performed and each patient, selected for having bilateral hallux valgus of the same grade, received the SERI technique in one foot and Scarf technique in the other. This study design produced a homogenous case series and overcame subjective variability in the evaluation of parameters such as pain, for example.
Nevertheless a small number of patients is the major limiting aspect of our study.
The clinical and radiographic results were similar in both groups. A decrease of the clinical score was observed with time in both groups that was related partially to slight reduction of the ROM of the first MTP joint, and also arthritic changes of the ipsilateral joints occurred with time and were not necessarily related to the procedures.
The Scarf procedure requires two screws for fixation, and the procedure is not free of complications, as rates of 5% to 10% including superficial wound infection, traumatic dislocation of the distal fragment, and hallux limitus, have been reported [4, 21].
The minimally invasive hallux valgus correction SERI is not a new technique because it uses an osteotomy and a stabilization method already described. Nevertheless, it has high versatility and efficacy as it provides a combination of the strengths of the previously described procedures resulting in a technique with unique characteristics of minimal invasiveness, simplicity, versatility, and good stability of the construct. Different types of percutaneous techniques stabilized with a temporary K wire have been described in the literature, but concerns regarding these techniques may exist as the correction is performed blindly and use of a fluoroscope is required [17]. The SERI technique is performed through a 1-cm medial incision that permits direct control of the osteotomy and of the displacement and stabilization and is capable of overcoming the expressed concerns [3, 9–12, 20].
Two patients in the Scarf group required hardware removal for intolerance, and the only poor result was in the Scarf group and was caused by arthritis and severely reduced ROM of the first MTP joint, with transfer metatarsalgia. The patient has thus far refused revision surgery. The surgical time was significantly less with the SERI technique, with no greater level of intraoperative and postoperative complications.
Our study confirmed that the Scarf and SERI osteotomies are effective for correction of hallux valgus and provided similar results with time, in line with other prospective and retrospective case series in the literature [1, 13].
However the SERI, performed with a minimal skin incision and less surgical time, fixed with a less expensive device (one K wire), resulted in greater patient satisfaction and may be preferable.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that the Independent Ethical Committee of his or her institution has approved the study protocol, including the study rationale, design, material, methods.
References
- 1.Barouk LS. Scarf osteotomy for hallux valgus correction: local anatomy, surgical technique, and combination with other forefoot procedures. Foot Ankle Clin. 2000;5:525–558. [PubMed] [Google Scholar]
- 2.Bauer T, de Lavigne C, Biau D, De Prado M, Isham S, Laffenétre O. Percutaneous hallux valgus surgery: a prospective multicenter study of 189 cases. Orthop Clin North Am. 2009;40:505–514. doi: 10.1016/j.ocl.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 3.Bösch P, Wanke S, Legenstein R. Hallux valgus correction by the method of Bösch: a new technique with a seven-to-ten-year follow-up. Foot Ankle Clin. 2000;5:485–498. [PubMed] [Google Scholar]
- 4.Coetzee JC. Scarf osteotomy for hallux valgus repair: the dark side. Foot Ankle Int. 2003;24:29–33. doi: 10.1177/107110070302400104. [DOI] [PubMed] [Google Scholar]
- 5.Coetzee JC, Rippstein P. Surgical strategies: scarf osteotomy for hallux valgus. Foot Ankle Int. 2007;28:529–535. doi: 10.3113/FAI.2007.0529. [DOI] [PubMed] [Google Scholar]
- 6.Coughlin MJ, Jones CP. Hallux valgus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2007;28:759–777. doi: 10.3113/FAI.2007.0759. [DOI] [PubMed] [Google Scholar]
- 7.Deenik AR, Pilot P, Brandt SE, van Mameren H, Geesink RG, Draijer WF. Scarf versus chevron osteotomy in hallux valgus: a randomized controlled trial in 96 patients. Foot Ankle Int. 2007;28:537–541. doi: 10.3113/FAI.2007.0537. [DOI] [PubMed] [Google Scholar]
- 8.Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int. 2007;28:748–758. doi: 10.3113/FAI.2007.0748. [DOI] [PubMed] [Google Scholar]
- 9.Giannini S, Bevoni R, Vannini F, Cadossi M. Hallux valgus surgery: the minimally invasive bunion correction. In: Scuderi GR, Tria AJ, editors. Minimally Invasive Surgery in Orthopedics. New York, NY: Springer; 2010. pp. 463–471. [Google Scholar]
- 10.Giannini S, Ceccarelli F, Bevoni R, Vannini F. Hallux valgus surgery: the minimally invasive bunion correction (SERI) Tech Foot Ankle Surg. 2003;2:11–20. doi: 10.1097/00132587-200303000-00003. [DOI] [Google Scholar]
- 11.Giannini S, Faldini C, Vannini F, Digennaro V, Bevoni R, Luciani D. The minimally invasive osteotomy “S.E.R.I.” (simple, effective, rapid, inexpensive) for correction of bunionette deformity. Foot Ankle Int. 2008;29:282–286. doi: 10.3113/FAI.2008.0282. [DOI] [PubMed] [Google Scholar]
- 12.Giannini S, Vannini F, Faldini C, Bevoni R, Nanni M, Leonetti D. The minimally invasive hallux valgus correction (S.E.R.I.) Interactive Surgery. 2007;1:17–23. doi: 10.1007/s11610-007-0024-8. [DOI] [Google Scholar]
- 13.Jones S, Al Hussainy HA, Ali F, Betts RP, Flowers MJ. Scarf osteotomy for hallux valgus: a prospective clinical and pedobarographic study. J Bone Joint Surg Br. 2004;86:830–836. doi: 10.1302/0301-620X.86B6.15000. [DOI] [PubMed] [Google Scholar]
- 14.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 15.Laporta G, Melillo T, Olinsky D. X-ray evaluation of hallux abducto valgus deformity. J Am Podiatry Assoc. 1974;64:544–566. doi: 10.7547/87507315-64-8-544. [DOI] [PubMed] [Google Scholar]
- 16.Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin North Am. 2009;40:515–524. doi: 10.1016/j.ocl.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Magnan B, Pezzè L, Rossi N, Bartolozzi P. Percutaneous distal metatarsal osteotomy for correction of hallux valgus. J Bone Joint Surg Am. 2005;87:1191–1199. doi: 10.2106/JBJS.D.02280. [DOI] [PubMed] [Google Scholar]
- 18.Oh IS, Kim MK, Lim KY, Bae JH. Modified technique of distal metatarsal osteotomy for hallux valgus. Foot Ankle Int. 2007;28:527–528. doi: 10.3113/FAI.2007.0527. [DOI] [PubMed] [Google Scholar]
- 19.Portaluri M. Hallux valgus correction by the method of Bösch: a clinical evaluation. Foot Ankle Clin. 2000;5:499–511. [PubMed] [Google Scholar]
- 20.Saro C, Andrén B, Wildemyr Z, Felländer-Tsai L. Outcome after distal metatarsal osteotomy for hallux valgus: a prospective randomized controlled trial of two methods. Foot Ankle Int. 2007;28:778–787. doi: 10.3113/FAI.2007.0778. [DOI] [PubMed] [Google Scholar]
- 21.Smith AM, Alwan T, Davies MS. Perioperative complications of the Scarf osteotomy. Foot Ankle Int. 2003;24:222–227. doi: 10.1177/107110070302400304. [DOI] [PubMed] [Google Scholar]
- 22.Zygmunt KH, Gudas CJ, Laros GS. Z-bunionectomy with internal screw fixation. J Am Podiatr Med Assoc. 1989;79:322–329. doi: 10.7547/87507315-79-7-322. [DOI] [PubMed] [Google Scholar]