Abstract
Background
Slipped capital femoral epiphysis (SCFE) is a common hip problem in adolescents that results in a cam-type femoroacetabular impingement (FAI) deformity. Although the treatment for mild (slip angle of 0°–30°) and moderate (slip angle of 31°–60°) SCFE has historically been in situ fixation, recent studies have demonstrated impingement-related articular damage, irrespective of slip severity. Our series confirms previous reports that acetabular chondral injury occurs in mild to low-moderate (slip angle of ≤ 40°) SCFE.
Case Description
We retrospectively reviewed five patients who underwent arthroscopy and femoral osteoplasty within 18 months after in situ stabilization. All had labral and/or acetabular damage.
Literature Review
Osteoarthritis rates after SCFE range from 24% to 92% at 11 to 28 years, depending on how osteoarthritis is defined. Long-term followup suggests patients have acceptable outcomes, but these studies are limited by heterogeneity and a ceiling effect from the instruments used to assess function. Although the femoral deformity remodels, it is unclear what secondary changes occur in the acetabulum. Recent investigations suggest patients are functionally limited after SCFE owing to FAI compared with controls. MRI findings and surgical reports document impingement-related joint damage after SCFE, even in the absence of symptoms. Based on this, some advocate timely correction of the cam deformity inherent in SCFE.
Purposes and Clinical Relevance
Further study is warranted to determine whether immediate osteoplasty after in situ fixation of mild SCFE is beneficial to limit articular damage and improve long-term outcomes.
Introduction
Slipped capital femoral epiphysis (SCFE) is the most common adolescent hip problem, occurring at a rate of 10.8 per 100,000 children [20]. The physeal disruption results in anterior displacement of the femoral neck metaphysis relative to the epiphysis, which remains in the acetabulum. The ensuing deformity of a prominent anterosuperior femoral neck metaphysis is the prototypical morphology of cam-type femoroacetabular impingement (FAI). Because reduction of the slip has been associated with an increased risk of osteonecrosis and arthrosis [5, 13] and the head-neck deformity has been observed to remodel over time [3, 4, 6, 8, 15, 16, 29, 39], the recommended treatment for SCFE has traditionally been in situ fixation [4, 5, 13–15, 37].
With improved understanding of the pathologic consequences of FAI as a risk factor for osteoarthritis (OA) [11, 35], there is growing concern that delay or failure to correct the impingement component of a SCFE may lead to articular damage that is otherwise preventable [26]. It is of particular concern that young patients may be incurring joint injury with mild deformity [17, 41] despite the absence of pain [9]. CT and computer-generated motion simulations of mild (slip angle of 0°–30°) and moderate (slip angle of 31°–60°) [1, 33] SCFE demonstrate the metaphyseal prominence enters the joint in normal positions of function, which can lead to chondral damage as it impinges on the anterior acetabulum and labrum [24, 30]. Two studies reporting intraoperative findings in patients undergoing surgical hip dislocation after SCFE support these models [22, 32]. Both document anterosuperior acetabular cartilage damage in the zone of mechanical contact, which did not correlate with slip severity, and substantial damage was noted in hips with low-grade slip angles. A recent case series of patients undergoing arthroscopic femoral osteoplasty concomitant with in situ fixation noted labral fraying and acetabular chondromalacia in three patients with stable SCFE and slip angles of less than 25° [23]. Our case series confirms the findings of previous reports demonstrating acetabular chondral damage in patients with mild to low-moderate (slip angle of ≤ 40°) SCFE.
We present the intraoperative findings from five patients in whom arthroscopy and femoral osteoplasty were carried out within 18 months of in situ fixation. For all patients, the femoral osteoplasty was performed by recontouring the femoral head-neck junction with a motorized burr from the medial retinacular fold to the lateral retinacular vessels, which were preserved. Both arthroscopic and fluoroscopic dynamic examinations were performed pre- and postosteoplasty to confirm adequacy of the bony correction [18, 19]. In each patient, there was gross damage to the labrum and/or articular cartilage, despite a short duration from the time of the SCFE. These findings warrant further study and discussion regarding whether a more aggressive approach is indicated to treat the impingement inherent in SCFE.
Case Reports
Patient 1
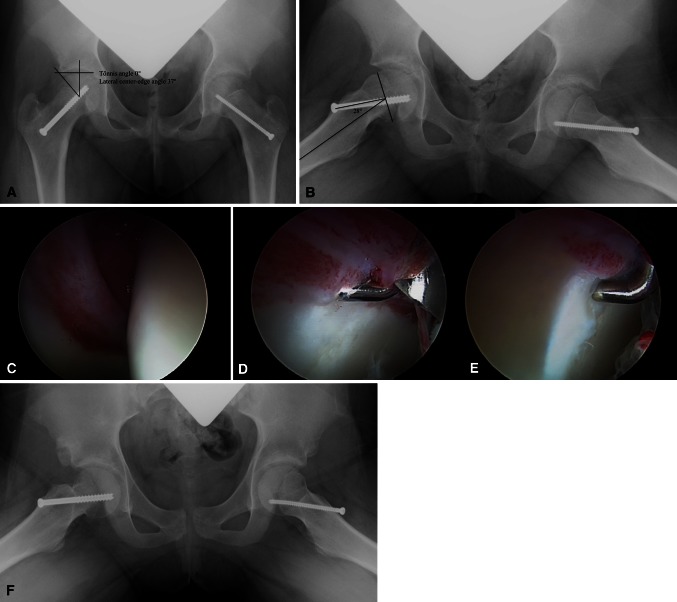
At 5 months after in situ cannulated screw stabilization of a stable, right SCFE (with prophylactic stabilization of the contralateral side), an otherwise healthy 10-year-old girl had ongoing right groin pain and limited motion. Hip flexion was less than 90° with −20° of internal rotation in a flexed position. Radiographs showed bilateral coxa profunda, a right slip angle of 28°, a lateral center-edge angle of 37° [38], an anterior center-edge angle of 45° [21], a Tönnis acetabular roof angle of 0° [36], and an alpha angle of 70° [28] (Fig. 1A–B). Her pain and limited hip motion were attributed to combined impingement from acetabular overcoverage and the prominent proximal femoral metaphysis from her SCFE. The patient and family were presented with treatment options, including continued observation, femoral osteoplasty, or femoral osteoplasty combined with triradiate epiphysiodesis to arrest further deepening of her acetabulum. After reviewing the risks and benefits of these options, the family opted for osteoplasty and triradiate epiphysiodesis. She underwent diagnostic arthroscopy to evaluate labral pathology followed by open femoral osteoplasty and triradiate epiphysiodesis. No acetabular rim trim was performed. Arthroscopy revealed extensive synovitis, labral hyperemia, and an anterior acetabular chondral fissure with a small flap tear that was conservatively débrided (Fig. 1C–E). At 3-year followup, she had no pain, hip flexion to 110°, and 10° internal rotation in 90° flexion. Radiographs showed a lateral center-edge angle of 33°, an anterior center-edge angle of 27°, and an alpha angle of 41° (Fig. 1F).
Fig. 1A–F.
(A) In an AP pelvis radiograph of Patient 1, the right lateral center-edge angle is 37°, the Tönnis acetabular roof angle is 0°, and the anterior center-edge angle on false-profile view (not shown) is 45°. (B) In the frog leg lateral image, the right hip slip angle is 28° and the alpha angle is 70°. Note the slip angle is reported as head-shaft angle on the involved side, rather than as a difference between head-shaft angles between the two sides as described by Southwick [33]. (C) Synovitis and labral hyperemia are evident at arthroscopy 5 months after in situ stabilization of the SCFE. (D) There is disruption at the anterior labrochondral junction and (E) an acetabular chondral fissure with a small, unstable flap. (F) A frog leg lateral image after right anterior arthrotomy shows improvement in the femoral head-neck offset.
Patient 2
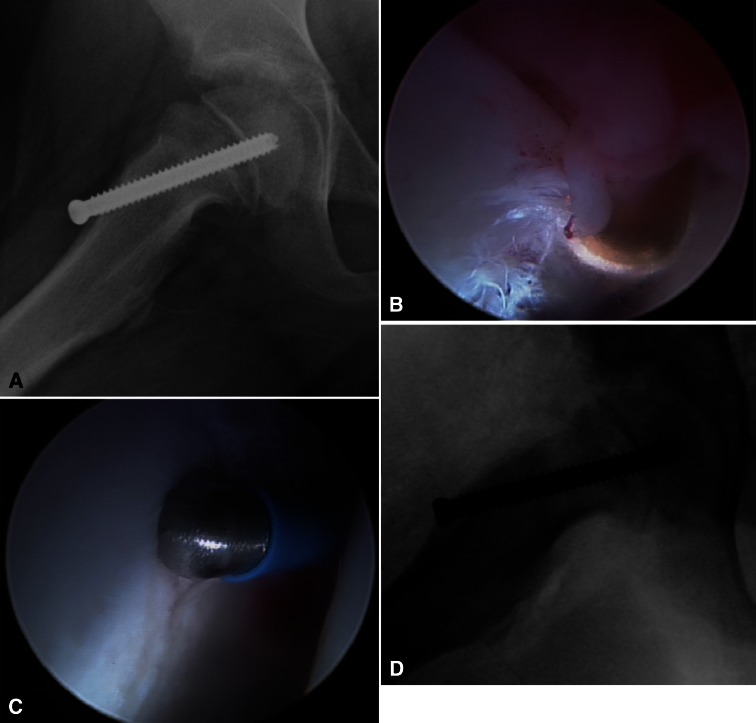
At 5 months after stabilization of a clinically unstable SCFE with a slip angle of 21° and an alpha angle of 87° (Fig. 2A), a 13-year-old boy with McCune-Albright syndrome had ongoing right groin pain and limited hip motion. On physical examination, hip flexion of greater than 60° resulted in external rotation of the hip. At 90° flexion, internal rotation was −20°. The patient and family consented to proceed with arthroscopic femoral osteoplasty in an effort to improve his pain and motion. Intraoperatively, there was substantial synovitis, labral fraying, and an anterosuperior acetabular partial thickness chondral fissure (Fig. 2B–C). At 9 months after arthroscopy, he had no right hip pain, improved flexion to 95° and 10° internal rotation at 90° flexion. The postosteoplasty alpha angle was 47° (Fig. 2D).
Fig. 2A–D.
(A) A right frog leg lateral view of Patient 2 shows an alpha angle of 87° before osteoplasty. (B) At arthroscopy, there was anterior synovitis and labral fraying with (C) a partial thickness chondral fissure. (D) An intraoperative fluoroscopic image shows an alpha angle of 47° after osteoplasty.
Patient 3
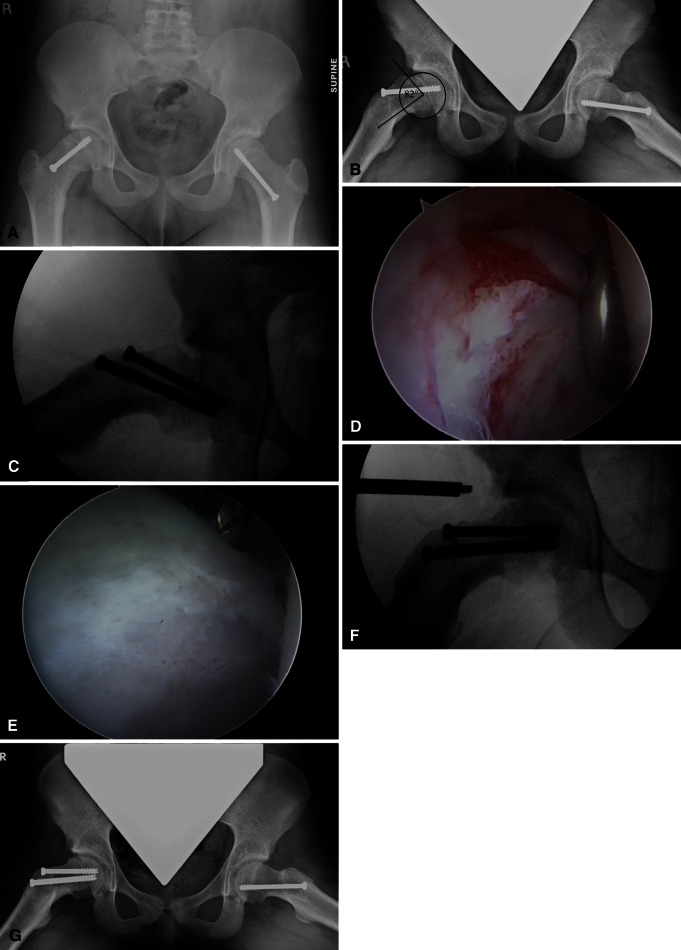
A 14-year-old female softball player was seen for a second opinion after undergoing in situ stabilization of a left SCFE 26 months and right SCFE 16 months previously. She had no pain but an altered gait, particularly during running, owing to external rotation of the right leg. Physical examination demonstrated external rotation of the right hip and leg with hip flexion beyond 60°. At 90° flexion, she had −30° internal rotation. At initial fixation, the right epiphysis was minimally displaced with a slip angle measuring 15°. Serial radiographs showed continued displacement had occurred to a slip angle of 39° and an alpha angle of 82° at the time she was seen at our institution (Fig. 3A–B). Femoral retroversion measured 20° on the right and 0° on the left by CT scan. The slip progression had stabilized from comparison radiographs over 10 months and the physis was near closure. The patient and family were primarily interested in intervention to correct her gait disturbance. They were presented with treatment options of arthroscopic osteoplasty or surgical dislocation with osteoplasty and derotational osteotomy for correction of femoral retroversion. They opted to proceed with arthroscopic osteoplasty because of the shorter duration of recovery and the potential for earlier return to sports. Concomitant with the arthroscopy, an additional cannulated screw was placed to ensure no further displacement of the epiphysis (Fig. 3C). Intraoperatively, the patient had severe labral fraying and diffuse fibrillation of the anterior acetabular cartilage (Fig. 3D–E). At 6 months after surgery, she had returned to full athletic activity and had no pain. Hip flexion was to 100° with 0° internal rotation at 90° flexion. The alpha angle was 42° on 45° Dunn lateral view (Fig. 3F–G).
Fig. 3A–G.
In (A) AP and (B) 45° Dunn lateral images of Patient 3 on presentation to our institution 16 months after right and 26 months after left in situ fixation of SCFE, the right slip angle is 39° and the alpha angle is 82°. The alpha angle is created from a line drawn through the center of the femoral head and a line parallel to the femoral neck, rather than through the femoral neck itself, due to posterior translation of the femoral head [23, 31]. (C) A second screw was placed to augment epiphyseal fixation. (D) At arthroscopy, there was hyperemia with anterior labral and labrochondral fraying. (E) A broader view demonstrates labral fraying, disruption of the labrochondral junction, and diffuse fibrillation of the cartilage in the anterosuperior quadrant of the acetabulum. (F) After femoral osteoplasty, the alpha angle is 42°. (G) A 45° Dunn lateral view shows maintenance of offset correction at 6 months after right femoral osteoplasty. The patient was pain-free and had returned to competitive sports.
Patient 4
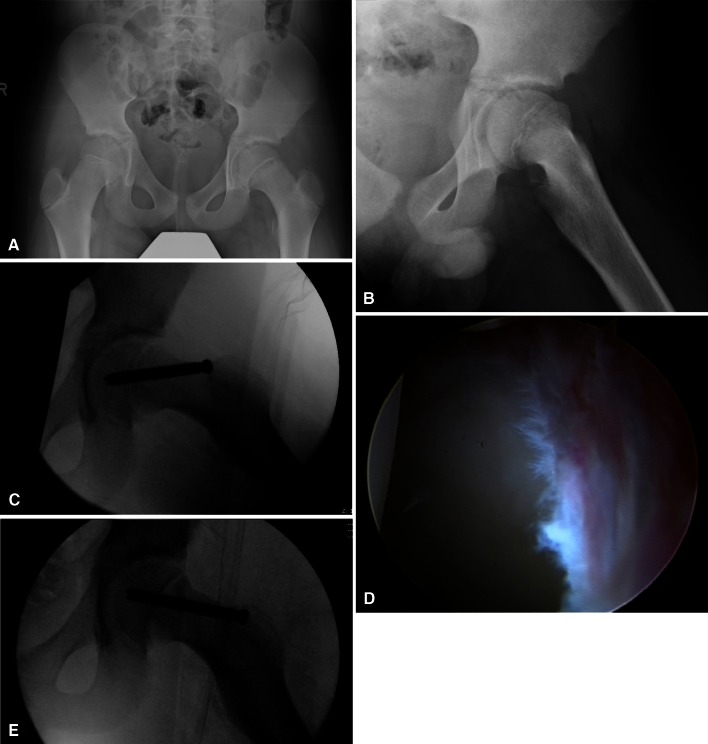
A 13-year-old boy presented to the emergency department with several months of hip and thigh pain that had acutely worsened after playing basketball. AP pelvis and frog leg lateral radiographs demonstrated a left SCFE with a slip angle of 31° and an alpha angle of 85° (Fig. 4A–B). Cautious physical examination demonstrated 5° internal rotation and 50° external rotation in full extension. At 60° flexion, the hip began to externally rotate; further flexion and internal rotation were not tested to avoid further displacement. Based on the experience from the previous three cases of finding intraarticular chondral damage after low-grade slips, we presented the option of in situ fixation alone or fixation combined with arthroscopic femoral osteoplasty to the patient and his parents. We thoroughly explained the risks and benefits of the additional procedure, as well as the limits of our knowledge about the long-term effect of this intervention compared to the natural history of in situ stabilization alone. The family opted to proceed with concomitant arthroscopic femoral osteoplasty. After securing the SCFE with in situ fixation on a radiolucent operating table (Fig. 4C), the patient was transferred to a table fitted with a distraction attachment (Smith & Nephew, Inc, Andover, MA, USA) for hip arthroscopy. He had a hyperemic, frayed anterior labrum with superficial abrasive changes at the adjacent acetabular chondral surface (Fig. 4D). In the peripheral compartment, there was obvious separation between the epiphysis and metaphysis with roughened, bony spicules in the interval. After osteoplasty, dynamic examination confirmed fluoroscopic and arthroscopic impingement-free flexion to 90° with internal rotation to 15° in flexion. The postosteoplasty alpha angle measured 44° on a fluoroscopic 45° Dunn lateral view (Fig. 4E). The patient was pain-free 9 months after surgery.
Fig. 4A–E.
(A) Irregularity of the left femoral physis is evident on the AP pelvis radiograph of Patient 4. (B) The frog leg lateral image demonstrates a slip angle of 31° and an alpha angle of 85°. (C) An intraoperative fluoroscopic 45° Dunn lateral view shows prominence of the anterior metaphysis with an alpha angle of 60° before osteoplasty. (D) Diffuse labral hyperemia and fraying are seen at arthroscopy, which was performed immediately after in situ fixation. (E) After osteoplasty, the alpha angle is 45°.
Patient 5
A 14-year-old boy presented to the emergency department with 4 weeks’ duration of groin pain and was diagnosed with a stable, chronic SCFE. On physical examination, his hip began to externally rotate with hip flexion of greater than 80°. At 90° flexion, he had −15° internal rotation. As in Patient 4, the patient and family were presented with the option of in situ stabilization alone or combined with arthroscopic femoral osteoplasty. Again, after thorough discussion of the risks, benefits, and long-term uncertainty of this approach, they opted for the combined procedure with arthroscopy performed after in situ stabilization of the slipped epiphysis. Intraoperatively, there was anterior labral hyperemia with a partial-thickness labral tear and a roughened area at the metaphyseal-epiphyseal junction of the proximal femur (Fig. 5A). After osteoplasty, he had impingement-free flexion to 95° and 20° internal rotation in flexion. The alpha angle improved from 60° to 43° on the 45° Dunn lateral radiograph (Fig. 5B–C). At 3 months’ followup, he was pain-free and had a normal gait.
Fig. 5A–C.
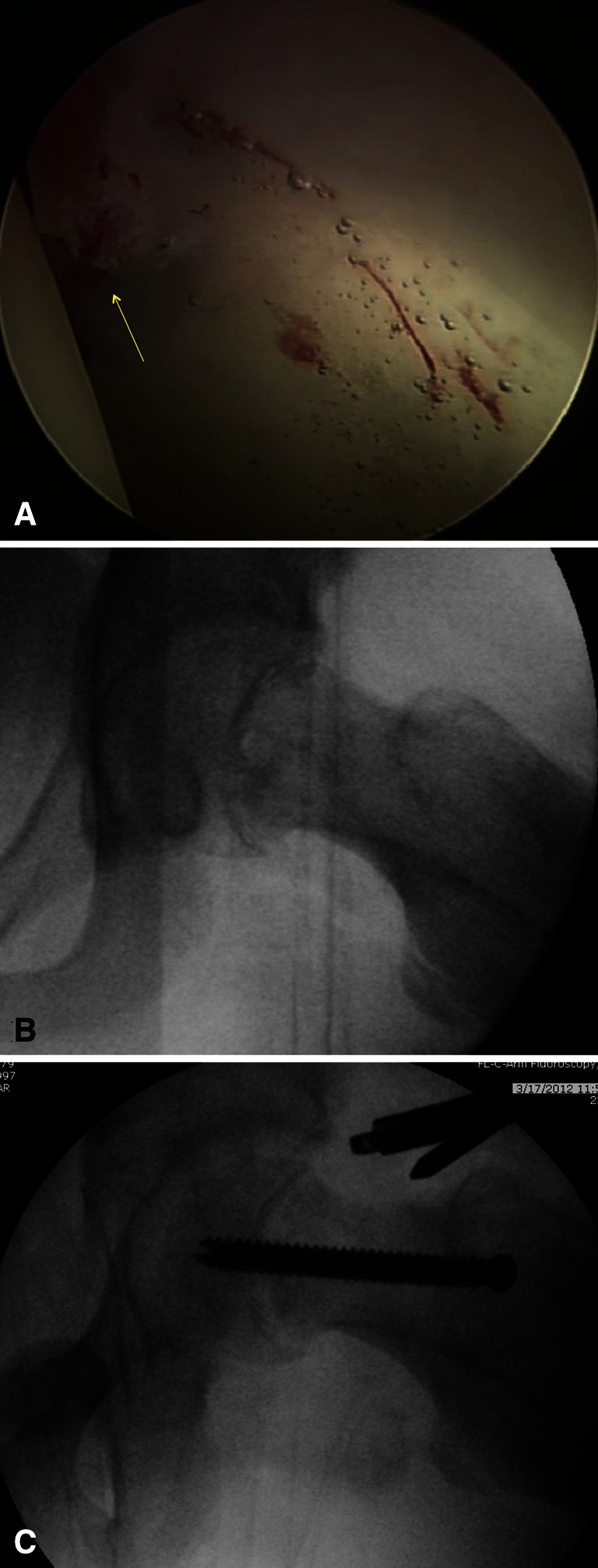
(A) An arthroscopic image shows anterior labral hyperemia and a radial tear (arrow) in Patient 5. The slip angle on the frog leg lateral view (not shown) measures 29°. Intraoperative fluoroscopic 45° Dunn lateral views show (B) an alpha angle of 60° before osteoplasty and (C) an alpha angle of 43° after osteoplasty.
Discussion
In this series, damage was observed early after SCFE, even in patients with mild deformities (slip angle of ≤ 40º). In all cases, there was synovitis, labral injury, and/or anterosuperior acetabular chondrosis.
The primary limitation of this report is the small number of patients. It is possible these individuals are not representative of all patients with SCFE; others may not be incurring damage. Second, because arthroscopy was performed early after the SCFE, the articular injuries may have been caused by the initial slip and not indicative of ongoing damage. Third, the chondral changes could stabilize over time and not lead to long-term disability.
This series confirms the findings of previous reports. Leunig et al. [23] similarly noted labral and acetabular damage in three cases of immediate arthroscopy after fixation of mild SCFE. Futami et al. [10] first reported simultaneous arthroscopy at the time of SCFE stabilization. In four patients, there was anterosuperior acetabular cartilage and posterolateral labral injury, which they attributed to trauma at the time of the slip and friction from the epiphysis. This injury pattern is now understood to result from anterior FAI with a posterior contre-coup lesion [11, 30].
It is notable all patients in our series had substantially limited hip motion. Internal rotation at 90° flexion correlates with bone structure, specifically the space between the acetabular rim and femoral neck, rather than soft tissue tension [40]. Thus, although these patients had low-to-moderate slip angles, their restricted motion reflects more profound bony deformity.
Although described by various terms—pistol grip [34], post slip [12], and tilt deformity [27]—the bony morphology resembling SCFE has been associated with OA for decades. SCFE is the prototypical example of cam-type FAI, which is an increasingly recognized cause of OA [2, 11, 35]. Computer and CT modeling studies simulate the pathologic motion and contact that occur with SCFE deformity [24, 30]. Rab [30] described two patterns of impingement, depending on the severity of the slip. In the inclusion phenomenon, the metaphyseal prominence from mild and low-moderate slips enters the joint in flexion, causing damage to the acetabular cartilage and labrum. In severe slips, the larger prominence abuts the acetabular rim but cannot enter the joint. This results in peripheral labral injury but less acetabular cartilage damage. Thus, mild or moderate slips have the potential to cause more intraarticular damage than severe slips; this model is supported by reports showing the degree of joint damage [41] and need for subsequent surgery [17] are not linearly correlated with the severity of deformity. Further, the pattern of injury predicted by these models has been documented with T2- and T2*-mapped MRI [25] and in patients undergoing surgical hip dislocation after SCFE [22, 32].
The main argument against immediate osteoplasty is that the metaphyseal deformity remodels over time [6, 7, 16, 29]. However, there are conflicting findings regarding the factors that predict remodeling. There is evidence of increased remodeling with a more severe slip [3, 39] and evidence to the contrary [15]. It has been reported remodeling requires an open triradiate cartilage [15], which is a proxy for remaining growth potential; however, others have found no correlation with the status of the triradiate [39]. None of these studies evaluated secondary changes in the acetabulum. In view of documented acetabular chondral damage, we question whether the stimulus for remodeling is repeated contact of the metaphyseal prominence against the normal acetabulum rather than spontaneous resorption at the femoral neck. In other words, does remodeling occur at the expense of the labrum and acetabular cartilage? In followup of patients with SCFE at our institution, we have observed flattening and sclerosis of the lateral acetabular margin (Fig. 6).
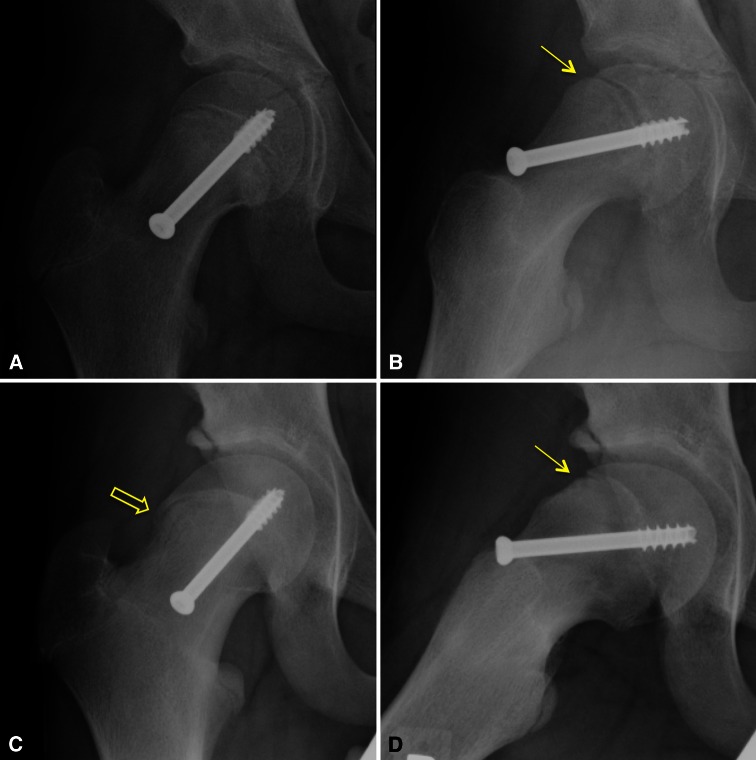
Fig. 6A–D.
(A) AP and (B) lateral views show the hip of a 14-year-old boy 3 weeks after in situ fixation of a mild SCFE. (C) AP and (D) lateral views show the hip 17 months later at age 16 years. There is flattening of the lateral acetabular margin at the acetabular epiphysis and sclerosis of the sourcil. Remodeling of the metaphyseal step-off adjacent to the epiphysis (solid arrows) is evident, but a prominence persists distally on the anterior femoral neck. There is lateral extension of the femoral epiphysis (open arrow) [31].
Long-term outcome studies after SCFE are compromised by heterogeneity in the modes of treatment, variation in functional scoring, and inconsistency in the radiographic methods used to grade epiphyseal displacement and OA [4, 5, 13, 14, 37]. Rates of radiographic OA range from 24% at 28 years’ followup [13] to as high as 92% at 11 years’ followup [41], depending on how OA is defined. Rates of conversion to arthrodesis or arthroplasty vary from 4.5% at 16 years’ followup [17] to 22% at 38 years’ followup [37]. Long-term reports cite good functional outcomes by the Iowa hip score [5] or Harris hip score [14, 17, 37, 41]. However, there is a ceiling effect when applying instruments that were validated in patients with arthritis and arthroplasty to a younger population [17]. In one report, despite having high Harris hip scores (average, 91.9), a group of 38 patients at a mean of 11.1 years after in situ fixation of SCFE had lower Tegner-Lysholm activity scores compared with healthy controls [41]. In addition, this group, with an average age of 23.4 years, had lower values on the physical functioning and role physical components of the SF-36 compared with normative data. Thus, despite having minimal pain and apparently good functional scores, these patients perceived themselves as physically limited compared with the general population.
Some surgeons advocate a more proactive approach to treat SCFE-related impingement. Millis and Novais [26] argue SCFE should be viewed as a two-fold problem of physeal instability and FAI. It is critical to secure the unstable physis, but the FAI inherent in SCFE must also be addressed. Because of concern that chondral degeneration is irreversible, Leunig et al. [22, 23] have changed their treatment algorithm. Since 2008, mild slips are managed with in situ fixation and immediate arthroscopic head-neck osteoplasty; moderate and severe slips are treated with subcapital realignment.
Our findings confirm mild and low-moderate slips can lead to joint damage that may be apparent within weeks after a SCFE and in the absence of symptoms. More work is needed to define the predictive factors for clinically important OA, elucidate the mechanisms of remodeling, and critically examine functional outcomes after SCFE. This task is complicated by the lengthy followup required to derive meaningful conclusions. Further study and thoughtful discussion are warranted to determine whether immediate osteoplasty after in situ fixation of mild to low-moderate slips is justified in an effort to limit articular damage.
Footnotes
One or more of the authors (YMY) certifies that he or she, or a member of his or her immediate family, has received or may receive payment or benefits, during the study period, an amount of less than $10,000 from Smith & Nephew Inc (Memphis, TN, USA); an amount of less than $10,000 from OrthoPediatrics (Warsaw, IN, USA); and an amount of less than $10,000 from Arthrex Inc (Naples, FL, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
Each author certifies that his or her institution approved the reporting of these case reports, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Boston Children’s Hospital, Boston, MA, USA.
References
- 1.Ballmer PM, Gilg M, Aebi B, Ganz R. [Results following sub-capital and Imhauser-Weber osteotomy in femur head epiphyseolysis] [in German] Z Orthop Ihre Grenzgeb. 1990;128:63–66. doi: 10.1055/s-2008-1039863. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 3.Bellemans J, Fabry G, Molenaers G, Lammens J, Moens P. Slipped capital femoral epiphysis: a long-term follow-up, with special emphasis on the capacities for remodeling. J Pediatr Orthop B. 1996;5:151–157. doi: 10.1097/01202412-199605030-00003. [DOI] [PubMed] [Google Scholar]
- 4.Boyer DW, Mickelson MR, Ponseti IV. Slipped capital femoral epiphysis: long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am. 1981;63:85–95. [PubMed] [Google Scholar]
- 5.Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am. 1991;73:667–674. [PubMed] [Google Scholar]
- 6.Clarke NM, Harrison MH. Slipped upper femoral epiphysis: a potential for spontaneous recovery. J Bone Joint Surg Br. 1986;68:541–544. doi: 10.1302/0301-620X.68B4.3733827. [DOI] [PubMed] [Google Scholar]
- 7.Dawes B, Jaremko JL, Balakumar J. Radiographic assessment of bone remodelling in slipped upper femoral epiphyses using Klein’s line and the alpha angle of femoral-acetabular impingement: a retrospective review. J Pediatr Orthop. 2011;31:153–158. doi: 10.1097/BPO.0b013e3182093dc7. [DOI] [PubMed] [Google Scholar]
- 8.DeLullo JA, Thomas E, Cooney TE, McConnell SJ, Sanders JO. Femoral remodeling may influence patient outcomes in slipped capital femoral epiphysis. Clin Orthop Relat Res. 2007;457:163–170. doi: 10.1097/BLO.0b013e31802d8aaa. [DOI] [PubMed] [Google Scholar]
- 9.Fraitzl CR, Kafer W, Nelitz M, Reichel H. Radiological evidence of femoroacetabular impingement in mild slipped capital femoral epiphysis: a mean follow-up of 14.4 years after pinning in situ. J Bone Joint Surg Br. 2007;89:1592–1596. doi: 10.1302/0301-620X.89B12.19637. [DOI] [PubMed] [Google Scholar]
- 10.Futami T, Kasahara Y, Suzuki S, Seto Y, Ushikubo S. Arthroscopy for slipped capital femoral epiphysis. J Pediatr Orthop. 1992;12:592–597. [PubMed] [Google Scholar]
- 11.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 12.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis: relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489–1497. doi: 10.2106/00004623-199710000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Hagglund G, Hannson LI, Sandstrom S. Slipped capital femoral epiphysis in southern Sweden: long-term results after nailing/pinning. Clin Orthop Relat Res. 1987;217:190–200. [PubMed] [Google Scholar]
- 14.Hansson G, Billing L, Hogstedt B, Jerre R, Wallin J. Long-term results after nailing in situ of slipped upper femoral epiphysis: a 30-year follow-up of 59 hips. J Bone Joint Surg Br. 1998;80:70–77. doi: 10.1302/0301-620X.80B1.7268. [DOI] [PubMed] [Google Scholar]
- 15.Jones JR, Paterson DC, Hillier TM, Foster BK. Remodelling after pinning for slipped capital femoral epiphysis. J Bone Joint Surg Br. 1990;72:568–573. doi: 10.1302/0301-620X.72B4.2380205. [DOI] [PubMed] [Google Scholar]
- 16.Lacroix P, Verbrugge J. Slipping of the upper femoral epiphysis; a pathological study. J Bone Joint Surg Am. 1951;33:371–381. [PubMed] [Google Scholar]
- 17.Larson AN, Sierra RJ, Yu EM, Trousdale RT, Stans AA. Outcomes of slipped capital femoral epiphysis treated with in situ pinning. J Pediatr Orthop. 2012;32:125–130. doi: 10.1097/BPO.0b013e318246efcb. [DOI] [PubMed] [Google Scholar]
- 18.Larson CM, Wulf CA. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular impingement in the supine position. Arthroscopy. 2009;25:1183–1192. doi: 10.1016/j.arthro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 19.Lee CB, Clark J. Fluoroscopic demonstration of femoroacetabular impingement during hip arthroscopy. Arthroscopy. 2011;27:994–1004. doi: 10.1016/j.arthro.2011.01.020. [DOI] [PubMed] [Google Scholar]
- 20.Lehmann CL, Arons RR, Loder RT, Vitale MG. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop. 2006;26:286–290. doi: 10.1097/01.bpo.0000217718.10728.70. [DOI] [PubMed] [Google Scholar]
- 21.Lequesne MG, Laredo JD. The faux profil (oblique view) of the hip in the standing position: contribution to the evaluation of osteoarthritis of the adult hip. Ann Rheum Dis. 1998;57:676–681. doi: 10.1136/ard.57.11.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leunig M, Casillas MM, Hamlet M, Hersche O, Notzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. doi: 10.1080/000164700317393367. [DOI] [PubMed] [Google Scholar]
- 23.Leunig M, Horowitz K, Manner H, Ganz R. In situ pinning with arthroscopic osteoplasty for mild SCFE: a preliminary technical report. Clin Orthop Relat Res. 2010;468:3160–3167. doi: 10.1007/s11999-010-1408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mamisch TC, Kim YJ, Richolt JA, Millis MB, Kordelle J. Femoral morphology due to impingement influences the range of motion in slipped capital femoral epiphysis. Clin Orthop Relat Res. 2009;467:692–698. doi: 10.1007/s11999-008-0477-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miese FR, Zilkens C, Holstein A, Bittersohl B, Kropil P, Mamisch TC, Lanzman RS, Bilk P, Blondin D, Jager M, Krauspe R, Furst G. Assessment of early cartilage degeneration after slipped capital femoral epiphysis using T2 and T2* mapping. Acta Radiol. 2011;52:106–110. doi: 10.3109/02841851.2010.516015. [DOI] [PubMed] [Google Scholar]
- 26.Millis MB, Novais EN. In situ fixation for slipped capital femoral epiphysis: perspectives in 2011. J Bone Joint Surg Am. 2011;93(suppl 2):46–51. doi: 10.2106/JBJS.K.00040. [DOI] [PubMed] [Google Scholar]
- 27.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–824. doi: 10.1259/0007-1285-38-455-810. [DOI] [PubMed] [Google Scholar]
- 28.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 29.O’Brien ET, Fahey JJ. Remodeling of the femoral neck after in situ pinning for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1977;59:62–68. [PubMed] [Google Scholar]
- 30.Rab GT. The geometry of slipped capital femoral epiphysis: implications for movement, impingement, and corrective osteotomy. J Pediatr Orthop. 1999;19:419–424. doi: 10.1097/00004694-199907000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54–60. doi: 10.1097/00003086-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 32.Sink EL, Zaltz I, Heare T, Dayton M. Acetabular cartilage and labral damage observed during surgical hip dislocation for stable slipped capital femoral epiphysis. J Pediatr Orthop. 2010;30:26–30. doi: 10.1097/BPO.0b013e3181c6b37a. [DOI] [PubMed] [Google Scholar]
- 33.Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49:807–835. [PubMed] [Google Scholar]
- 34.Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthtis of the hip. In: Amstutz HC, editor. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby; 1975. pp. 212–228. [Google Scholar]
- 35.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis. Clin Orthop Relat Res. 2004;429:170–177. doi: 10.1097/01.blo.0000150119.49983.ef. [DOI] [PubMed] [Google Scholar]
- 36.Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 37.Wensaas A, Svenningsen S, Terjesen T. Long-term outcome of slipped capital femoral epiphysis: a 38-year follow-up of 66 patients. J Child Orthop. 2011;5:75–82. doi: 10.1007/s11832-010-0308-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939;83(suppl 58):5–135. [Google Scholar]
- 39.Wong-Chung J, Strong ML. Physeal remodeling after internal fixation of slipped capital femoral epiphyses. J Pediatr Orthop. 1991;11:2–5. doi: 10.1097/01241398-199101000-00002. [DOI] [PubMed] [Google Scholar]
- 40.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. doi: 10.1097/BLO.0b013e3180399430. [DOI] [PubMed] [Google Scholar]
- 41.Zilkens C, Bittersohl B, Jager M, Miese F, Schultz J, Kircher J, Westhoff B, Krauspe R. Significance of clinical and radiographic findings in young adults after slipped capital femoral epiphysis. Int Orthop. 2011;35:1295–1301. doi: 10.1007/s00264-010-1106-5. [DOI] [PMC free article] [PubMed] [Google Scholar]