History
Classifications of Legg-Calvé-Perthes disease (LCPD) may be divided into three categories: those defining the stage of the disease, those attempting to prognosticate outcome, and those defining outcome. Although Arthur Legg MD [13], Jacques Calvé [2], and Georg Perthes MD [17] share credit for their descriptions of the disease published between 1909 and 1910, according to Wenger and Pandya, Henning Waldenstrom of Norway published on LCPD in 1909, mistaking it for tuberculosis of the hip [24]. Although Waldenstrom’s name does not appear in the disease eponym, he is credited with development of the first classification of the disease in 1922, which recognized four stages of radiographic progression: initiation, fragmentation, reossification, and healed [10]. Outcome classifications also are based on radiographic characteristics. The classification of Stulberg et al. groups mature hips by shape of the femoral head and congruency in the joint and is the most widely used outcome measure [11, 23].
Several prognostic classification systems for use at disease onset have been proposed. Catterall [3] was the first to publish a widely accepted prognostic classification in 1971. This system described four categories based on the location of involvement of the femoral head as viewed on AP and lateral radiographs. In 1984, Salter and Thompson [22] proposed a two-category system based on a review of 1057 children with 1264 involved hips. They determined that subchondral fracture was predictive of eventual degree of involvement of the femoral head and also believed that a two-category classification could increase reliability. This system has been criticized as difficult for less experienced surgeons to use as the subchondral fracture line can be quite subtle and not always present [14]. Finally, Herring et al. [7] followed a group of 86 patients (93 hips) longitudinally and correlated their presenting radiographs to their Stulberg classification and found that the height of the lateral column on AP radiographs was predictive of the final outcome of the disease. This is considered to be the most reproducible classification system and consequently has grown in popularity [11, 14, 16].
Purpose
A classification system is needed to aid the physician in understanding the natural history of LCPD. Most cases are unilateral, but some may be bilateral. For some children, outcomes may be excellent with no intervention, while others may require surgery to maintain ROM and prevent early-onset arthritis. The prognosis is dependent on age at disease onset, with younger patients generally faring better than older patients [4, 7, 15, 21].
An ideal classification system should predict functional outcomes and prescribe treatment, enabling the surgeon to distinguish operative from nonoperative cases. A practical classification system must be reproducible, relying on landmarks that are only minimally affected by the disease process. It must accurately group similar hips so that treatment outcomes may be compared.
Classification
Herring et al. [7] proposed to classify LCPD based on the height of the lateral aspect of the capital femoral epiphysis during the fragmentation stage of the disease. The researchers found this system correlated well with the Stulberg classification of outcomes (Table 1).
Table 1.
The Stulberg classification of Legg-Calvé-Perthes disease
| Stulberg class | Description | Outcome |
|---|---|---|
| I | Normal, congruent hip | Arthritis does not develop |
| II | Spherical head, concentric in acetabulum on AP and frog leg lateral; shortened femoral neck or abnormally steep acetabulum | |
| III | Ovoid, mushroom, or umbrella-shaped femoral head; not flat | Mild to moderate arthritis in adulthood |
| IV | Flat head and acetabulum (congruent joint) | |
| V | Flat femoral head, normal femoral neck and acetabulum (incongruent joint) | Severe arthritis before 50 years of age |
The Herring classification divides the femoral head into three parts or pillars at 90° to the physis (Fig. 1). The central pillar is defined by central sequestration during the fragmentation stage of the disease and makes up approximately 50% of the epiphysis on a true AP radiograph. The lateral pillar makes up 15% to 30% of the femoral head, while the medial pillar makes up the remaining 20% to 35%. Herring Group A consists of lateral pillars without disease involvement, including no loss of height or density changes. Group B pillars measure between 50% and 100% of original height, and Group C pillars measure less than 50% of original height. Herring et al. [6] modified their classification in 2004 after a large, multicenter trial revealed a clinically important fourth category, the group B/C Border (Table 2). Pillars in the B/C border group fall into three distinct types: (1) tall and narrow, with greater than 50% of height maintained and 2 to 3 cm of width; (2) poorly ossified, with at least 50% height maintained, or (3) relatively depressed as compared with the central pillar, with exactly 50% of pillar height maintained [5]. The modified classification system with expected outcomes and treatment guidance [6] is summarized below.
Fig. 1 A–E.
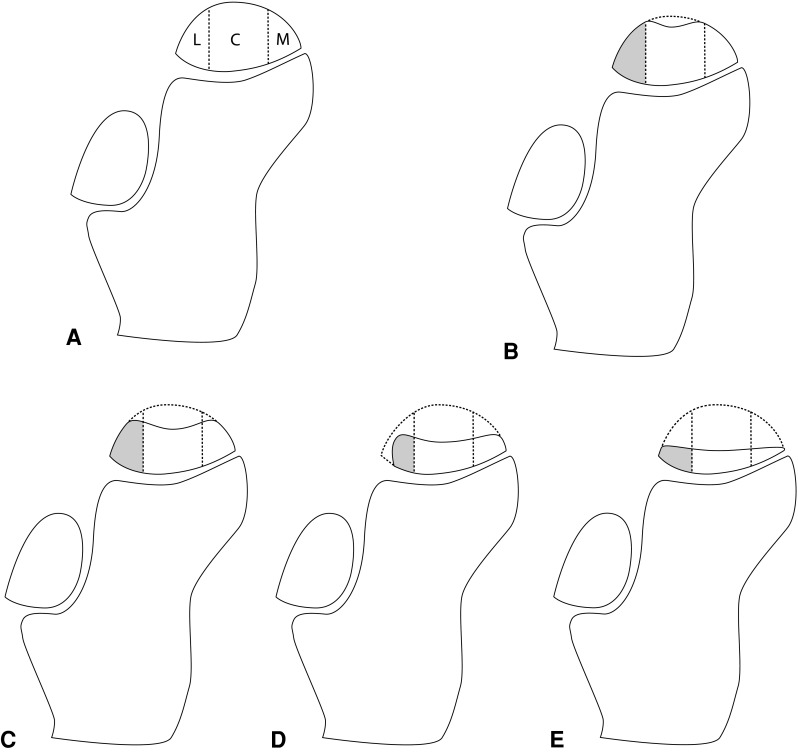
The drawings show a pediatric hip, identifying the three Herring pillars and the height of each Herring class hip. (A) The three pillars in the Herring lateral pillar classification are: L = lateral pillar; C = central pillar; and M = medial pillar. (B) In Herring Group A, 100% of lateral pillar height is maintained. (C) In Herring Group B, greater than 50% of the lateral pillar height is maintained. (D) In this example of Herring Group B/C border, the tall and narrow type is shown with slightly more than 50% of the lateral pillar height maintained on a narrow base. (E) In Herring Group C, less than 50% of the lateral pillar height is maintained.
Table 2.
Modified Herring lateral pillar classification
| Herring group | Description | Expected outcome | Suggested treatment |
|---|---|---|---|
| A | The lateral pillar is uninvolved, with full height maintained | Uniformly good outcome (100% Stulberg Class I or II) | No treatment |
| B | Greater than 50% of lateral pillar height maintained | Good outcome (67% Stulberg Class I or II, 27% Stulberg Class III, 6% Stulberg Class IV or V) | Less than 8 years: nonsurgical treatment Greater than 8 years: innominate osteotomy or varus femoral osteotomy |
| B/C border | Greater than 50% of lateral pillar height, column is narrow (2–3 cm), or approximately 50% of pillar height maintained with poor ossification, or 50% pillar height maintained but depressed relative to central pillar | Intermediate outcome (28% Stulberg Class I or II, 43% Stulberg Class III, 30% Stulberg Class IV or V) | |
| C | Less than 50% of lateral pillar height maintained | Poor prognosis (13% Stulberg Class II, 52% Stulberg Class III, 35% Stulberg Class IV or V) | Nonsurgical treatment |
Validation
Many investigators have validated the original Herring classification system. Farsetti et al. [4] retrospectively studied 49 nonoperatively managed patients with LCPD with an average followup of 24 years. They found that the Herring classification system accurately predicted outcomes with 10 of 11 Group A hips. This shows good remodeling of the femoral head, good outcomes in members of Group B in patients younger than 9 years, and uniformly deformed femoral heads in members of Group C [4]. Ritterbusch et al. [20] found the Herring classification system more predictive of Stulberg outcome than the Catterall classification. The Herring lateral pillar classification has been validated for young children. Generally, young children have a better prognosis than older children at disease onset. In a retrospective study of children with onset of disease when younger than 6 years receiving minimal treatment, Rosenfeld et al. [21] validated the modified lateral pillar classification and found it to be highly correlated with Stulberg outcome. Eighty percent of children did well, and only those classified as Group B/C border and Group C had a poor prognosis.
The Herring classification has shown high levels of interobserver and intraobserver reliability. Herring et al. [7] originally published an interobserver agreement rate of 78%. A larger, multicenter prospective study of the modified classification [6] found 85% interobserver agreement and 77% intraobserver agreement. Agus et al. reported that the Herring classification performed poorly in comparison to the Catterall and Salter-Thompson classifications during the diagnostic and treatment phases of the disease [1]. The Herring classification is intended for use during the fragmentation stage only. This may explain the poor performance of the Herring classification during the treatment phase radiographs. Although the Herring classification performed well in the diagnostic phase radiographs, Agus et al. [1] found superior reliability for the Salter-Thompson and Catterall classifications. In contrast, a meta-analysis of Catterall, Salter-Thompson, and Herring classifications found the Herring classification to be the most reproducible and reliable of the measurements owing to its easy use [14]. Podeszwa et al. [18] reported good interrater and intrarater reliability of the lateral pillar classification using kappa statistical analysis. The researchers also found that reliability was independent of experience with pediatric orthopaedics [18]. Wiig et al. [25] verified the superiority of the Herring classification in their prospective trial. Although they found a positive correlation between physician experience and reliability of classification, the Herring classification was the most reliable system for less experienced surgeons [25]. Farsetti et al. [4] found that interobserver agreement using the Herring classification increased from 88% to 100% when observers used a ruler to determine lateral pillar height.
Limitations
The Herring classification should be used only during the fragmentation stage of the disease. In addition, initial radiographs may underestimate the severity of the disease in 33%- to 40% of cases [12, 16]. On average, patients will experience 7 months of symptoms before their radiographs can safely be considered stable. The “wait and classify” approach suggested by Kim and Herring [10] has been criticized [9, 19] because it may delay treatment and impact final outcome, particularly in children older than 8 years who are at higher risk for poor outcomes.
Radiographic measurements and accuracy of classification rely on true AP radiographs and positioning can affect accuracy. It also can be difficult to estimate percentage height loss when significant damage to the lateral pillar is detected. Herring et al. [7] originally suggested that the contralateral hip be used as a control, but this is not always practical in cases of bilateral disease.
Finally, the lateral pillar classification may not be valid in children older than 12 years [8]. At this age, researchers found that the remodeling phase of the disease does not occur, leading to aspherical femoral heads and poor outcomes [8].
Conclusions
The Herring lateral pillar classification may be used to predict outcomes in children younger than 12 years with LCPD. This classification is a helpful tool in identifying surgical candidates. It must be used during the fragmentation stage of disease and physicians also must be wary of disease progression, as approximately  of patients will change categories with time. A “wait and classify” approach as suggested by Kim and Herring [10] will ensure that patients who present before the fragmentation stage and patients who progress will be appropriately classified and treated. Some think the Herring lateral pillar classification is more reproducible than the Salter-Thompson or Catterall classification, and it may be used accurately by orthopaedic surgeons of varying degrees of experience. Careful attention must be paid to positioning on radiographs, and the use of a ruler can increase accuracy of classification. Because no single classification predicts outcomes with perfect accuracy, other factors including age at disease onset and duration of symptoms will further aid the surgeon in predicting outcome and selecting treatment [14].
of patients will change categories with time. A “wait and classify” approach as suggested by Kim and Herring [10] will ensure that patients who present before the fragmentation stage and patients who progress will be appropriately classified and treated. Some think the Herring lateral pillar classification is more reproducible than the Salter-Thompson or Catterall classification, and it may be used accurately by orthopaedic surgeons of varying degrees of experience. Careful attention must be paid to positioning on radiographs, and the use of a ruler can increase accuracy of classification. Because no single classification predicts outcomes with perfect accuracy, other factors including age at disease onset and duration of symptoms will further aid the surgeon in predicting outcome and selecting treatment [14].
Acknowledgments
We thank Jason Black for help with the illustrations.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at the University of Washington Medical Center.
References
- 1.Agus H, Kalenderer O, Eryanlmaz G, Ozcalabi IT. Intraobserver and interobserver reliability of Catterall, Herring, Salter-Thompson and Stulberg classification systems in Perthes disease. J Pediatr Orthop B. 2004;13:166–169. doi: 10.1097/00009957-200405000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Calve J. On a particular form of pseudo-coxalgia associated with a characteristic deformity of the upper end of the femur. 1910. Clin Orthop Relat Res. 2006;451:14–16. doi: 10.1097/01.blo.0000238799.05338.5a. [DOI] [PubMed] [Google Scholar]
- 3.Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971;53:37–53. [PubMed] [Google Scholar]
- 4.Farsetti P, Tudisco C, Caterini R, Potenza V, Ippolito E. The Herring lateral pillar classification for prognosis in Perthes disease: late results in 49 patients treated conservatively. J Bone Joint Surg Br. 1995;77:739–742. [PubMed] [Google Scholar]
- 5.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: Classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004;86:2103–2120. [PubMed] [Google Scholar]
- 6.Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004;86:2121–2134. [PubMed] [Google Scholar]
- 7.Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calve-Perthes disease. J Pediatr Orthop. 1992;12:143–150. doi: 10.1097/01241398-199203000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Joseph B, Mulpuri K, Varghese G. Perthes’ disease in the adolescent. J Bone Joint Surg Br. 2001;83:715–720. doi: 10.1302/0301-620X.83B5.10663. [DOI] [PubMed] [Google Scholar]
- 9.Kim HK. Legg-Calve-Perthes disease. J Am Acad Orthop Surg. 2010;18:676–686. doi: 10.5435/00124635-201011000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Kim HK, Herring JA. Pathophysiology, classifications, and natural history of Perthes disease. Orthop Clin North Am. 2011;42:285–295, v. [DOI] [PubMed]
- 11.Kuo KN, Wu KW, Smith PA, Shih SF, Altiok H. Classification of Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31(2 suppl):S168–S173. doi: 10.1097/BPO.0b013e318223b50e. [DOI] [PubMed] [Google Scholar]
- 12.Lappin K, Kealey D, Cosgrove A. Herring classification: how useful is the initial radiograph? J Pediatr Orthop. 2002;22:479–482. [PubMed] [Google Scholar]
- 13.Legg AT. An obscure affection of the hip joint. 1910. Clin Orthop Relat Res. 2006;451:11–13. doi: 10.1097/01.BLO.0000238798.05338.13. [DOI] [PubMed] [Google Scholar]
- 14.Mahadeva D, Chong M, Langton DJ, Turner AM. Reliability and reproducibility of classification systems for Legg-Calve-Perthes disease: a systematic review of the literature. Acta Orthop Belg. 2010;76:48–57. [PubMed] [Google Scholar]
- 15.Mukherjee A, Fabry G. Evaluation of the prognostic indices in Legg-Calve-Perthes disease: statistical analysis of 116 hips. J Pediatr Orthop. 1990;10:153–158. [PubMed] [Google Scholar]
- 16.Park MS, Chung CY, Lee KM, Kim TW, Sung KH. Reliability and stability of three common classifications for Legg-Calve-Perthes disease. Clin Orthop Relat Res. 2012;470:2376–2382. doi: 10.1007/s11999-012-2314-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perthes G. The classic: On juvenile arthritis deformans. 1910. Clin Orthop Relat Res. 2012;470:2349–2368. doi: 10.1007/s11999-012-2433-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Podeszwa DA, Stanitski CL, Stanitski DF, Woo R, Mendelow MJ. The effect of pediatric orthopaedic experience on interobserver and intraobserver reliability of the herring lateral pillar classification of Perthes disease. J Pediatr Orthop. 2000;20:562–565. doi: 10.1097/01241398-200009000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Price CT. The lateral pillar classification for Legg-Calve-Perthes disease. J Pediatr Orthop. 2007;27:592–593. doi: 10.1097/01.bpb.0000279028.74397.02. [DOI] [PubMed] [Google Scholar]
- 20.Ritterbusch JF, Shantharam SS, Gelinas C. Comparison of lateral pillar classification and Catterall classification of Legg-Calve-Perthes’ disease. J Pediatr Orthop. 1993;13:200–202. [PubMed] [Google Scholar]
- 21.Rosenfeld SB, Herring JA, Chao JC. Legg-calve-perthes disease: a review of cases with onset before six years of age. J Bone Joint Surg Am. 2007;89:2712–2722. doi: 10.2106/JBJS.G.00191. [DOI] [PubMed] [Google Scholar]
- 22.Salter RB, Thompson GH. Legg-Calve-Perthes disease: the prognostic significance of the subchondral fracture and a two-group classification of the femoral head involvement. J Bone Joint Surg Am. 1984;66:479–489. [PubMed] [Google Scholar]
- 23.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am. 1981;63:1095–1108. [PubMed] [Google Scholar]
- 24.Wenger DR, Pandya NK. A brief history of Legg-Calve-Perthes disease. J Pediatr Orthop. 2011;31(2 suppl):S130–S136. doi: 10.1097/BPO.0b013e318226028c. [DOI] [PubMed] [Google Scholar]
- 25.Wiig O, Terjesen T, Svenningsen S. Inter-observer reliability of radiographic classifications and measurements in the assessment of Perthes’ disease. Acta Orthop Scand. 2002;73:523–530. doi: 10.1080/000164702321022794. [DOI] [PubMed] [Google Scholar]


