Abstract
Background
The treatment of unstable slipped capital femoral epiphysis (SCFE) is rapidly evolving with the ability to correct epiphyseal alignment using the modified Dunn technique. Adopting a new treatment method depends on confirming that it achieves its goals, produces few, nonserious complications with no lasting sequelae, and improves the natural history of the disorder compared with known treatment methods. As such, the rates of osteonecrosis and complications after current treatments of unstable SCFE must be compared with those of newer surgical techniques.
Questions/purposes
We therefore addressed the following questions: (1) What is the rate of osteonecrosis of the femoral head after treatment of unstable SCFE? (2) What treatment modalities have been used for unstable SCFE and (3) what are the reported complications?
Methods
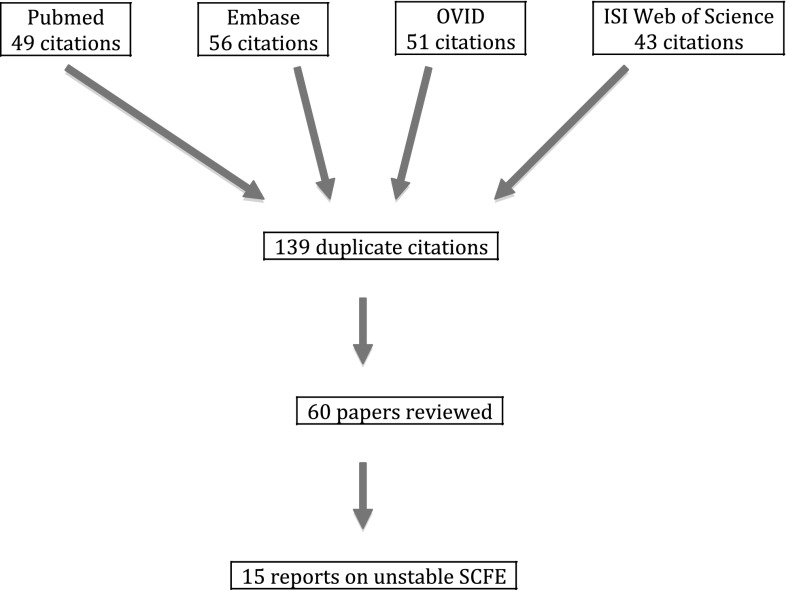
We performed a systematic electronic literature search for the keywords unstable and slipped capital femoral epiphysis and identified 199 articles. Of these, 60 met our inclusion criteria. Fifteen articles were included for analysis.
Results
The literature concerning the treatment and results of unstable SCFE is retrospective Level IV data that suggest an overall rate of osteonecrosis of 23.9%. Multiple treatment modalities were used for unstable SCFE treatment with varying, inconsistently recorded complications over the reporting period.
Conclusions
We found limited data concerning the rate of osteonecrosis and complications after treatment of unstable SCFE. Considering recent widespread interest in the modified Dunn procedure and the possibility of iatrogenic osteonecrosis, there is a need for prospective studies to identify complications and establish outcome based on standardized scores for established and emerging treatments of unstable SCFE.
Introduction
Slipped capital femoral epiphysis (SCFE), a well-recognized disorder affecting adolescents, has potential long-term sequelae that may permanently alter hip function [2, 3]. Traditionally, the near-term prognosis after SCFE treatment was based on the duration of the patient’s symptoms at the time of presentation for treatment. The studies of Boyer et al. and Carney et al. [2, 3] suggest patients presenting acutely, within 3 weeks of symptom onset, were considered at increased risk for developing osteonecrosis of the upper femoral epiphysis. They believed the choice of technique and method used to stabilize or reposition the epiphysis affected the function and survivorship of the treated hip. Attempted closed reduction of a displaced epiphysis, possibly influenced by the timing of reduction, has been associated with the highest prevalence of osteonecrosis, considered the most serious complication after SCFE [2, 3, 11, 13]. In 1993, Loder et al. [14] proposed classifying patients based on epiphyseal stability, an approach that more accurately predicts the development of osteonecrosis. Consequently, Carney et al. [3] concluded that treating SCFE by in situ pinning without reduction was associated with the fewest complications, and this has become the most common surgical treatment worldwide.
Recently, advances in understanding the applied anatomy of the medial femoral circumflex artery have enabled safe surgical dislocation of the hip, mobilization of the upper femoral epiphysis, and reduction and fixation [6, 7, 9, 21, 23]. This technique is anecdotally controversial, has not been universally accepted, and has been criticized because of the potential for complications [9, 21, 23]. Since the inception of this technique, it has been possible to preserve the vascular supply [9, 21, 23] and to realign anatomically the unstable SCFE. However, the widespread adoption of this (or any) new surgical treatment must be based on improvements over the natural history of the untreated disease and the outcome of current techniques (in situ pinning, alternative methods of reduction and fixation) and complications related to the procedure itself. To provide a framework for future studies on the treatment of unstable SCFE, there is a need to review and analyze the current literature and clinical evidence regarding the treatment of this disorder.
The purpose of this systematic review of the literature regarding treatment of unstable SCFE was to answer the following two questions: (1) What is the rate of osteonecrosis of the femoral head after treatment of the unstable SCFE? (2) What treatment modalities have been used for unstable SCFE and what are the reported complications?
Search Strategy and Criteria
We searched four medical literature databases (PubMed, EMBASE, OVID, and ISI Web of Science) between January 1, 1994, and November 30, 2010, and repeated the search on June 28, 2012. Identical keywords were used in all database searches. We searched PubMed and EMBASE for “unstable slipped femoral epiphysis”, and OVID and ISI Web of Science were searched for “unstable AND slipped capital femoral epiphysis”. One hundred ninety-nine entries were recorded from the four databases (PubMed 49, EMBASE 56, OVID 51, and ISI Web of Science 43). The 199 abstracts generated by these four searches were reviewed by the first author (IZ) and 139 duplicate results were eliminated leaving 60 unique citations (Fig. 1). The first author reviewed the full text of each of the 60 unique citations and included articles for review if they were (1) published in peer-reviewed English language journals; (2) included greater than or equal to 10 patients treated for an unstable SCFE; and (3) followed for a mean of 2 years. We additionally excluded commentaries, surveys, in vitro studies, animal studies, reviews, and studies that were not related to treatment. We excluded one article because it presented the same cohort of patients in another journal. Fifteen articles met inclusion criteria and were systematically reviewed by the first author.
Fig. 1.
The search strategy is shown.
We reviewed each article for study design and study purpose. The definition of an unstable SCFE used by each author was recorded. The absolute number of patients presenting with an unstable SCFE was evaluated and, when recorded, the proportion of patients with unstable SCFE was reviewed. We recorded demographic data, when available, including age at presentation, body mass index, slip severity, and average followup.
Three recent studies published by Slongo et al. [21], Ziebarth et al. [23], and Huber et al. [9] were used for discussion purposes but not to establish the historical prevalence of osteonecrosis in unstable SCFE.
Treatment methods that were recorded in each study were reviewed. We recorded the duration of symptoms before presentation, time from presentation to definitive fixation, method of fixation, performance of either inadvertent or intentional closed or open reduction, postoperative management protocol, and any associated complications presented in the article.
The absolute number of patients diagnosed with osteonecrosis of the upper femoral epiphysis was recorded. When reported, we recorded the method used to establish the diagnosis of osteonecrosis and the elapsed time after index treatment until osteonecrosis was diagnosed. When reported, specific measures of outcomes were evaluated. Specifically, the management of osteonecrosis complicating unstable SCFE and the clinical outcome of any treatment were not a subject of this review.
The level of clinical evidence regarding the management of patients presenting with an unstable SCFE is Level IV (Table 1). With one exception, all studies were retrospective, Level IV case series in which the diagnosis of osteonecrosis was established on routine radiographic followup. Only Ramachandran et al. [18] published a Level III study investigating the efficacy of intravenous bisphosphonate treatment. To identify candidates for bisphosphonate therapy, they evaluated all patients treated for an unstable SCFE with a postoperative bone scan. They did not, however, comment on SCFE treatment modality because this was not the focus of their research. The majority of the articles included in the study were designed to investigate factors associated with the development of osteonecrosis after specific treatments for an unstable SCFE; however, timing of treatment, intention of epiphyseal reduction, number and type of implants, and postoperative management varied substantially depending on both the era of treatment and institutional preferences.
Table 1.
General data from analyzed reports
| Author | Slips/patients | Unstable SCFE (%) | Male:female | Average age (years) | Mean followup (months) | Era | Number avascular necrosis (%) | Level of evidence |
|---|---|---|---|---|---|---|---|---|
| Palocaren et al. (2010) [15] | 280/280 | 27 (9.8) | 196:84 | 12.2 | 36 | 1995–2006 | 6 (22.2) | 4 |
| Chen et al. (2009) [4] | 30/28 | 30 (100) | 19:11 | 11.6 | 65 | 1992–2002 | 4 (14.3) | 4 |
| Kalogrianitis et al. (2007) [11] | 117/82 | 16 (19) | 7:9 | 11.5 | 18 | 1998–2002 | 8 (50) | 4 |
| Lim et al. (2007) [13] | 38/30 | 22 (58) | 11:12 | 11 | 34 | 1997–2005 | 3 (12.5) | 4 |
| Ramachandran et al. (2007) [18] | 22/28 | 22 (100) | 3:9 | 12.8 | 40 | 2000–2003 | 12 (54.5) | 3 |
| Seller et al. (2006) [20] | 32/29 | 29 (90) | 10:19 | 12.5 | 42 | 1990–1999 | 2 (6.8) | 4 |
| Fallath and Lett (2004) [5] | 104/87 | 14 (16) | 7:7 | 12.8 | 35 | 1990–2000 | 3 (21) | 4 |
| Tokmakova et al. (2003) [22] | 240/240 | 36 (15) | 92:148 | 12.8 | 54 | 1965–1999 | 21 (58) | 4 |
| Gordon et al. (2002) [8] | 16/16 | 16 (100) | 8:8 | 11.1 | 27 | 1992–1998 | 2 (12) | 4 |
| Kennedy et al. (2001) [12] | 299/212 | 27 (13) | 10:17 | 11.3 | minimum 24 | 1985–1993 | 4 (14.8) | 4 |
| Phillips et al. (2001) [17] | 100/100 | 14 (14) | 5:9 | 13 | minimum 36 | 1972–1998 | 0 (0) | 4 |
| Peterson et al. (1997) [16] | 91/87 | 87 (100) | 27:60 | ? | Minimum 84 | 1950–1990 | 13 (14.2) | 4 |
| Aronson and Tursky (1996) [1] | ?/15 | 12 (80) | ? | ? | Minimum 24 | 1984–1994 | 2 (13.3) | 4 |
| Rao et al. (1996) [19] | 64/43 | 15 (35) | 18:25 | 12.3 | 35 | 1980–1990 | 1 (5.5) | 4 |
| Loder et al. (1993) [14] | 55/55 | 30 (55) | 16:14 | 12 | 36 | 1975–1991 | 14 (46.6) | 4 |
? = information not available from published article.
Results
We identified 397 (range, 12–91) unstable slips presented from 15 unique articles with 95 cases of osteonecrosis diagnosed after treatment. Overall, 23.9% of patients developed osteonecrosis but the reported ranges varied from 0% to 58% (Table 2). Only two articles established diagnostic radiographic criteria for osteonecrosis [18, 22], and only three studies documented the timeframe for establishing the diagnosis of osteonecrosis [13, 16, 18]. For 13 studies, the minimum length of followup was 12 months (average, 36 months; range, 12–72 months).
Table 2.
General data from analyzed reports
| Author | Treatment/fixation | Time to treat | Reduction | Capsulotomy | Postoperative management |
|---|---|---|---|---|---|
| Palocaren et al. (2010) [15] | In situ fixation | Average 27 hours (range, 6–240 hours) | Inadvertent | None | NWB or PWB |
| Chen et al. (2009) [4] | 2 6.5-mm cannulated screws | Within 12–24 hours | Simple positioning to preslip alignment | 16 percutaneous, 5 open, 9 none | NWB with crutches or wheelchair for 2 months |
| Kalogrianitis et al. (2007) [11] | Single cannulated screw | < 24 hours in 6, 24–72 hours in 7, > 8 days in 3 | Nondeliberate | None | NWB 6 weeks, PWB 6 weeks |
| Lim et al. (2007) [13] | Single cannulated screw, except 2 | Traction for 6 days | 11 manipulated | None | Hip spica for 6 weeks or NWB for 1–4 months |
| Ramachandran et al. (2007) [18] | In situ fixation, single screw, 5 were repinned with marrow injection | ? | ? | None | ? |
| Seller et al. (2006) [20] | Fixation with 3 Kirschner wires | Mild traction for 2 days | Gentle reduction | None | Protected weightbearing |
| Fallath and Lett (2004) [5] | 10 single screw, 3 Knowles pin, 1 two screws | Average 28 hours | 2 spontaneous, 9 manipulation | None | Crutches, no duration specified |
| Tokmakova et al. (2003) [22] | 144 single pin, 89 multiple pins | ? | 160 none, 67 partial, 13 complete | None | ? |
| Gordon et al. (2002) [8] | 2 cannulated screws | 11/16 < 24 hours, 3 < 72 hours | 12 closed, 4 open | 6 percutaneous, 4 open | NWM |
| Kennedy et al. (2001) [12] | 19 two screws, 7 single screw, 1 bone graft peg | ? | 17 reduction (3 traction, 11 closed, 2 open) | 2 open reduction, 6 cervical osteotomy | NWB |
| Phillips et al. (2001) [17] | 10/14 multiple pins, 1 cannulated screw, 2 femoral neck osteotomy, 1 Smith-Petersen nail | < 24 hours | Gentle manipulation | 2 osteotomy | ? |
| Peterson et al. (1997) [16] | 4 hip spica, 41 internal fixation, 31 bone peg with spica, 15 bone peg and internal fixation | 42 < 24 hours, 12 24–48 hours, 7 48–72 hours, 30 > 72 hours | 76 gentle flexion, traction, internal rotation, 14 traction and rotation | Capsulotomy in all patients with epiphyseodesis | NWB |
| Aronson and Tursky (1996) [1] | 2 screws | < 24 hours | 9 closed reduction with open approach, 6 indirect reduction | 9 capsulotomy for reduction | PWB 6 weeks |
| Rao et al. (1996) [19] | All except 1 open bone peg epiphyseodesis | ? | Preoperative skin traction | ? | Spica cast or traction for 4–6 weeks |
| Loder et al. (1993) [14] | 6 single screw, 1 single pin, 23 multiple screw or pin | 96 hours | 26 reduction (24 closed, 2 open) | 2 | ? |
NWB = nonweightbearing; PWB = partial weightbearing.
Although surgical stabilization was performed for all patients who presented with an unstable SCFE, the surgical approaches, implant devices, and postoperative management varied substantially between studies and within studies depending on the era in which patients were treated and data collected. Thirteen of 15 studies used internal fixation devices for epiphyseal stabilization that are detailed in Table 2. Depending on the time period over which the cases were collected, fixation type varied and included Knowles pins, Kirschner wires, solid screws, and single or multiple cannulated screws. Fixation type often varied within a single publication. Two reports [16, 19] included patients treated primarily by bone-peg epiphysiodesis; however, within these reports, there was variable use of internal fixation or postoperative spica casting.
Other than the development of osteonecrosis, seven studies reported complications related to the treatment of unstable SCFE [5, 8, 11–13, 17, 22]. Among the reported complications there were 16 cases of slip progression, three cases of chondrolysis, 41 pin penetrations, one femoral neck fracture, and two hardware removals. Eight studies did not report complications. Two studies reported clinical outcomes data using unvalidated measures [8, 13] and one study reported radiographic outcomes for patients who developed osteonecrosis using Stulberg’s classification for healed Legg-Calve-Perthes [18].
Discussion
The treatment of SCFE continues to challenge orthopaedic surgeons. Historically, patients presenting with acute or acute-on-chronic type slips were considered most at risk for complications related to the slip deformity or to the treatment of the slip. This classification was refined by Loder et al. [14] who presented the concept of epiphyseal stability and showed that osteonecrosis rarely, if ever, occurs in the stable slip. Although it is difficult to accurately assess the prevalence of unstable SCFE, it is estimated to be approximately 10% to 35% of patients presenting for treatment. The purpose of this literature review was to answer the following questions: (1) what is the rate of osteonecrosis of the femoral head after treatment of unstable SCFE; and (2) what treatment modalities have been used for unstable SCFE, and (3) what are the related complications?
The existing literature regarding the treatment of unstable SCFE is limited for a number of reasons. First, the published data are variable, often span decades, and are retrospective in nature. Although variations in surgical practices and implants are expected, especially given the study lengths, these inconsistencies make direct comparison of studies difficult. Second, the absence of consistently reported treatment complications and use of standardized, validated outcome instruments provide little and variable information on patient function. These findings emphasize the importance of future studies with standardized complication-reporting and validated clinical outcome instruments. Third, the definition of stability, although clearly described by Loder et al. [14], has been subject to interpretation [10] and probably varied among the studies, especially in the three recent articles, not included in the historical analysis, by Slongo et al. [21], Ziebarth et al. [23], and Huber et al. [9]. Fourth, because the concept of epiphyseal instability did not exist before 1993, most studies retrospectively classified patients included for study. This could change the actually denominator compared with a prospective analysis. Fifth, treatment rendered was often performed by multiple surgeons working within the same institution over long periods of time implying variations in clinical skill, implant use, radiologic technique, and patient assessment. Sixth, the limitations of this study reflect the deficiencies in the literature. The rate of osteonecrosis has been derived from multiple patient cohorts that have been published over decades that have witnessed changes in the assessment and classification of SCFE presentation, changes in radiologic technology, and changes in treatment modality, implant design, and application; and the outcome variable and definitions reported in the literature have not been consistent.
Our literature review found a cumulative rate of osteonecrosis of 23.9% among patients with SCFE classified as unstable. This value is derived from reports that span decades and mostly classified slip stability retrospectively based on chart reviews and with a wide range of incidence from 0% to 58%.
Treatment methods varied substantially between reports. The most frequently reported technique was internal fixation using either pins or screws and more recently using cannulated screws. Peterson et al. [16] and Rao et al. [19] reported on the use of bone-peg epiphysiodesis supplemented with either spica casting or internal fixation. There was no identifiable correlation between method of fixation and rate of avascular necrosis. Furthermore, 14 of 15 reviewed studies reported that some form of reduction, either purposeful or inadvertent, was performed in conjunction with treatment; however, there was no correlation between reduction and rate of osteonecrosis. The only study to report no purposeful reductions [8] had the highest reported rate of osteonecrosis. The reported complications were unsystematic and inconsistent. Therefore, it is not possible to establish a prevailing rate of complication based on the reviewed data.
The etiology of osteonecrosis has been incompletely explained. Potential mechanisms for the development of osteonecrosis may be partially dependent on the type of treatment but include kinking of periosteal blood vessels resulting from torsional deformity, synovitis associated with the trauma, vascular tamponade resulting from intracapsular hematoma, timing of treatment, and location of fixation devices within the epiphysis. Multiple treatment algorithms that were developed to address these theoretical causes include intentional delay in treatment [11], preoperative traction [13, 19, 20], both open and closed urgent reduction and fixation [8, 17], and open or percutaneous capsulotomy [8, 12, 19] and are all associated with developing osteonecrosis. Patients with unstable SCFE often presented with substantially more deformity, often correctable, and were more likely to undergo attempted reduction, either intentional or inadvertent. Although current thought reflected by the reviewed literature suggest that reducing a displaced, unstable SCFE may increase the prevalence of osteonecrosis, the only publication in this study reporting no osteonecrosis practiced emergent reduction and stabilization of the epiphysis [17]. As such, the pathomechanism of osteonecrosis seems elusive and, likely, multifactorial.
As surgical techniques evolve, recent advances enable safe surgical dislocation, comprehensive hip exposure with protection of vascular retinacular tissue, and accurate reduction of the unstable, displaced upper femoral epiphysis. The adoption of this newer technique must be based on documented improvement in the natural history of treated unstable SCFE and a reduction in the complications associated with elected treatment. Current data suggest the prevalence of osteonecrosis is 23.9%. In the absence of specific outcomes data, new surgical approaches, at the very least, must demonstrate a lower rate of osteonecrosis. Recent publications by Ziebarth et al. [23], Slongo et al. [21], and Huber et al. [9] reported two cases of osteonecrosis after 92 surgical dislocations for stable and unstable SCFE. Their classification for unstable slipped epiphysis differed from the strict definition of Loder et al. [14] to include both patients who were unable to ambulate and those with surgically unstable epiphysis identified at the time of the modified Dunn procedure. If both groups of unstable patients are included in the analysis, the overall rate of osteonecrosis is 7.6% (two of 26), whereas if one includes only patients unable to ambulate, the rate of osteonecrosis is 8.7% (two of 23), which is similar to the rates of osteonecrosis published by other authors using traditional treatment. These procedures, however, were performed by surgeons with substantial clinical experience who were, theoretically, passed a learning curve. Consequently, these data may not predict rates of osteonecrosis if the technique were adopted in a widespread fashion.
These data suggest that there is an urgent need for either a high-quality, multicenter retrospective study or a prospective study to determine the rate of treatment-related complications, including osteonecrosis, related to the management of unstable SCFE. The aforementioned recent publications suggest there may be a reduction in the rate of osteonecrosis when a modified Dunn approach is used for epiphyseal reduction by an experienced surgeon.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Aronson J, Tursky EA. The torsional basis for slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;322:37–42. doi: 10.1097/00003086-199601000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Boyer DW, Mickelson MR, Ponseti IV. Slipped capital femoral epiphysis. Long-term follow-up study of one hundred and twenty-one patients. J Bone Joint Surg Am. 1981;63:85–95. [PubMed] [Google Scholar]
- 3.Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am. 1991;73:667–674. [PubMed] [Google Scholar]
- 4.Chen RC, Schoenecker PL, Dobbs MB, Luhmann SJ, Szymanski DA, Gordon JE. Urgent reduction, fixation, and arthrotomy for unstable slipped capital femoral epiphysis. J Pediatr Orthop. 2009;29:687–694. doi: 10.1097/BPO.0b013e3181b7687a. [DOI] [PubMed] [Google Scholar]
- 5.Fallath S, Lett M. Slipped capital femoral epiphysis: an analysis of treatment outcome according to physeal stability. Can J Surg. 2004;47:284–289. [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 7.Gautier E, Ganz K, Krugel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679–683. doi: 10.1302/0301-620X.82B5.10426. [DOI] [PubMed] [Google Scholar]
- 8.Gordon JE, Abrahams MS, Dobbs MB, Luhmann SJ, Schoenecker PL. Early reduction, arthrotomy, and cannulated screw fixation in unstable slipped capital femoral epiphysis treatment. J Pediatr Orthop. 2002;22:352–358. [PubMed] [Google Scholar]
- 9.Huber H, Dora C, Ramseier LE, Buck F, Dierauer S. Adolescent slipped capital femoral epiphysis treated by a modified Dunn osteotomy with surgical hip dislocation. J Bone Joint Surg Br. 2011;93:833–838. doi: 10.1302/0301-620X.93B6.25849. [DOI] [PubMed] [Google Scholar]
- 10.Kallio PE, Mah ET, Foster BK, Paterson DC, LeQuesne GW. Slipped capital femoral epiphysis. Incidence and clinical assessment of physeal instability. J Bone Joint Surg Br. 1995;77:752–755. [PubMed] [Google Scholar]
- 11.Kalogrianitis S, Tan CK, Kemp GJ, Bass A, Bruce C. Does unstable slipped capital femoral epiphysis require urgent stabilization? J Pediatr Orthop B. 2007;16:6–9. doi: 10.1097/01.bpb.0000236224.14325.f1. [DOI] [PubMed] [Google Scholar]
- 12.Kennedy JG, Hresko MT, Kasser JR, Shrock KB, Zurakowski D, Waters PM, Millis MB. Osteonecrosis of the femoral head associated with slipped capital femoral epiphysis. J Pediatr Orthop. 2001;21:189–193. [PubMed] [Google Scholar]
- 13.Lim YJ, Lam KS, Lim KB, Mahadev A, Lee EH. Management outcome and the role of manipulation in slipped capital femoral epiphysis. J Orthop Surg. 2007;15:334–338. doi: 10.1177/230949900701500319. [DOI] [PubMed] [Google Scholar]
- 14.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75:1134–1140. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Palocaren T, Holmes L, Rogers K, Kumar SJ. Outcome of in-situ pinning in patients with unstable slipped capital femoral epiphysis: assessment of risk factors associated with avascular necrosis. J Pediatr Orthop. 2010;30:31–36. doi: 10.1097/BPO.0b013e3181c537b0. [DOI] [PubMed] [Google Scholar]
- 16.Peterson MD, Weiner DS, Green NE, Terry CL. Acute slipped capital femoral epiphysis: the value and safety of urgent manipulative reduction. J Pediatr Orthop. 1997;17:648–654. doi: 10.1097/00004694-199709000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Phillips SA, Griffiths WE, Clarke NM. The timing of reduction and stabilisation of the acute, unstable, slipped upper femoral epiphysis. J Bone Joint Surg Br. 2001;83:1046–1049. doi: 10.1302/0301-620X.83B7.11640. [DOI] [PubMed] [Google Scholar]
- 18.Ramachandran M, Ward K, Brown RR, Munns CF, Cowell CT, Little DG. Intravenous bisphosphonate therapy for traumatic osteonecrosis of the femoral head in adolescents. J Bone Joint Surg Am. 2007;89:1727–1734. doi: 10.2106/JBJS.F.00964. [DOI] [PubMed] [Google Scholar]
- 19.Rao SB, Crawford AH, Burger RR, Roy DR. Open bone peg epiphysiodesis for slipped capital femoral epiphysis. J Pediatr Orthop. 1996;16:37–48. doi: 10.1097/01241398-199601000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Seller K, Wild A, Westhoff B, Raab P, Krause R. Radiological evaluation of unstable slipped capital femoral epiphysis treated by pinning with Kirschner wires. J Pediatr Orthop B. 2006;15:328–334. doi: 10.1097/01202412-200609000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Slongo T, Kakaty D, Krause F, Ziebarth K. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010;92:2898–2908. doi: 10.2106/JBJS.I.01385. [DOI] [PubMed] [Google Scholar]
- 22.Tokmakova KP, Stanton RP, Mason DE. Factors influencing the development of osteonecrosis in patients treated for slipped capital femoral epiphysis. J Bone Joint Surg Am. 2003;85:798–801. doi: 10.2106/00004623-200305000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Ziebarth K, Zilkens C, Spencer S, Leunig M, Ganz R, Kim YJ. Capital realignment for moderate and severe SCFE using a modified Dunn procedure. Clin Orthop Relat Res. 2009;467:704–716. doi: 10.1007/s11999-008-0687-4. [DOI] [PMC free article] [PubMed] [Google Scholar]