Abstract
Background
Femoroacetabular impingement (FAI) is an incompletely understood clinical concept that implies pathomechanical changes in the hip as a cause for hip-related pain in young adults. While a positive anterior impingement test is suggestive of FAI, its association with clinical and radiographic findings remain unconfirmed in healthy young adults.
Questions/purposes
We determined the prevalence of a positive test in 1170 young adults and examined its possible associations with (1) self-reported hip discomfort for the past 3 months; (2) weekly physical exercise; (3) hip ROM; and (4) radiographic findings associated with femoroacetabular impingement.
Methods
We invited 2344 healthy 19-year-olds to a population-based hip study between 2008 and 2009; 1170 patients (50%) consented. The study included questionnaires on medical and functional status, a clinical hip examination including the impingement test and hip ROM, and two pelvic radiographs (AP and frog-leg views).
Results
Based on at least one affected hip, 35 of 480 (7.3%) men and 32 of 672 (4.8%) women had positive impingement tests. Eighteen of the 1170 patients were excluded owing to suboptimal or missing radiographs. Self-reported hip discomfort in the women and increased physical exercise in the men were strongly associated with the positive impingement tests. Decreased abduction and internal rotation in the men, decreased flexion in both genders, and radiographic cam type findings in the men also were associated with positive tests.
Conclusion
A positive test for anterior impingement is not uncommon in healthy young adults, especially in males. We believe it always should be performed along with pelvic radiographs in young, active patients presenting with hip pain.
Level of Evidence
Level II, diagnostic study. See the Guidelines for Authors for a complete description of level of evidence.
Introduction
Femoroacetabular impingement (FAI) has gained increasing interest as a clinical concept during the last decade and is now recognized as a risk factor for early hip osteoarthritis [1, 11, 12]. The diagnosis of FAI should be suspected when there is a history of hip and/or groin discomfort or pain and reduced hip motion on clinical examination; specifically, decreased hip flexion and internal rotation [12, 20, 53]. The pain in FAI can be reproduced by a positive clinical test for anterior impingement [23, 29] (Fig. 1). However, the test alone is not specific [30, 35] and radiographic findings associated with FAI are needed to confirm the diagnosis [49].
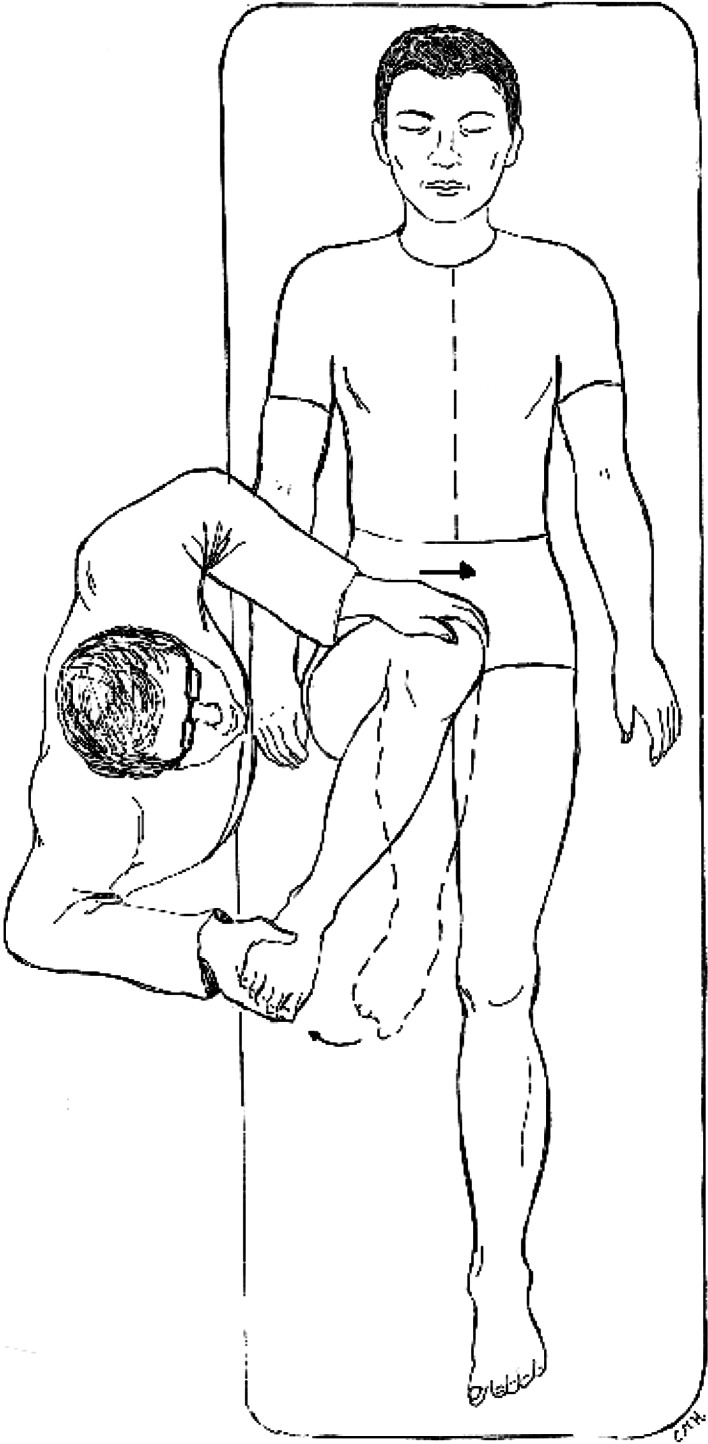
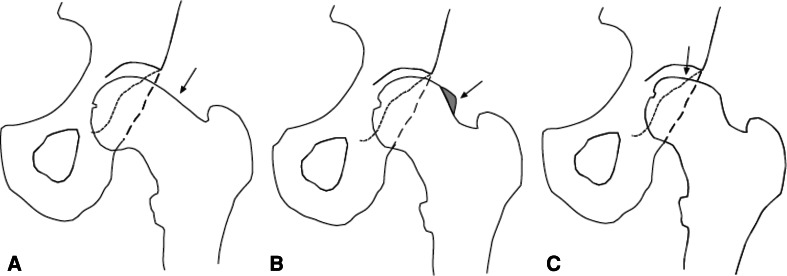
Fig. 1.
A pain-provocation test for anterior impingement was performed with the patient supine and scored as 0 (no pain provoked) or 1 (definite pain provoked when asked). A combined maneuver, consisting of 90° passive flexion of the hip, followed by forced adduction and internal rotation, was used.
FAI can be divided pathomechanically into a cam-type or a pincer-type impingement, based on the underlying anatomic deformity [10] (Fig. 2). The cam-type is characterized by a flattened or convex femoral head-neck junction, commonly seen at the anterosuperior aspect [13, 20, 36, 46, 48]. For the pincer-type, the underlying mechanism lies on the acetabular side, resulting in global or focal overcoverage [3, 12, 19, 21, 37, 42, 45]. In a recent population-based study on 2081 young adults (58% women), also including the 1170 subjects of this study, we reported prevalences of radiographic findings thought to be associated with cam- and pincer-type FAI on plain radiographs [24]. One or more findings indicating cam-type or pincer-type FAI were seen in 35 and 34% of the men and 10 and 17% of the women, respectively. Many of the radiographic findings coexisted. Clinically, the cam-type FAI is predominant in young, athletic boys and men, whereas the pincer-type FAI is seen more often in middle-aged women [11, 12, 20]. Often, a mixed type is present [3]. FAI can occur as a result of abnormal morphologic change or excessive ROM in the hip [8]. Increased physical exercise has been associated with FAI [11, 35]. Additional knowledge regarding the prevalence of a positive clinical test and its associations with clinical and radiographic findings would help to further understand FAI as a clinical concept and to integrate it in daily clinical practice, but remain to be confirmed in large population-based cohorts.
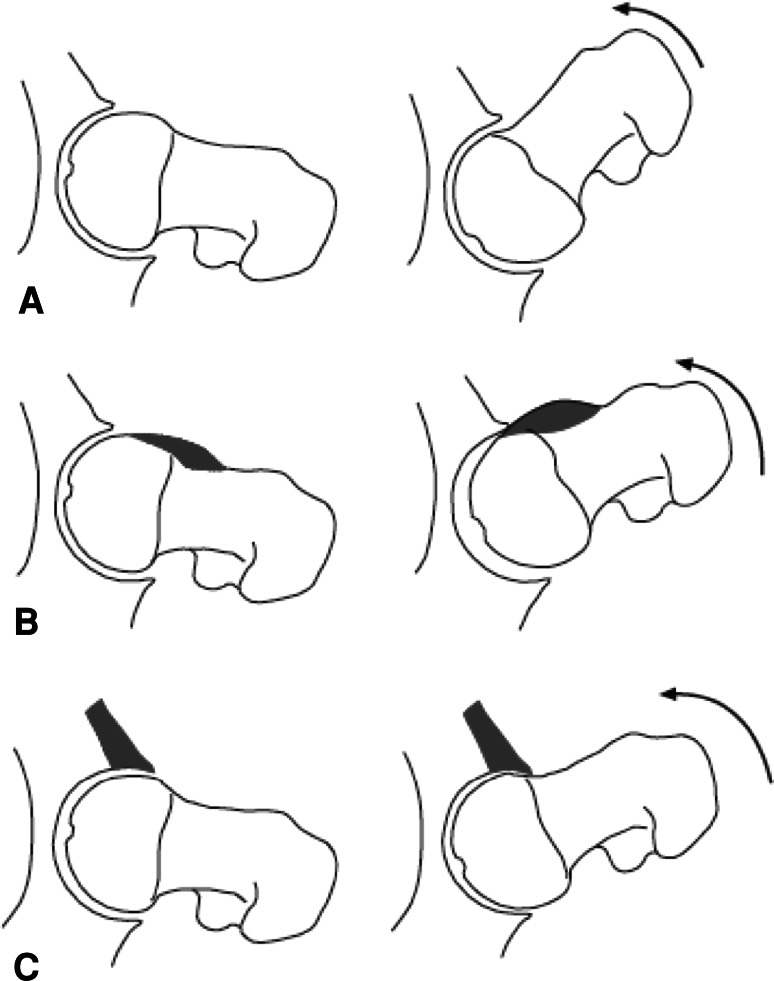
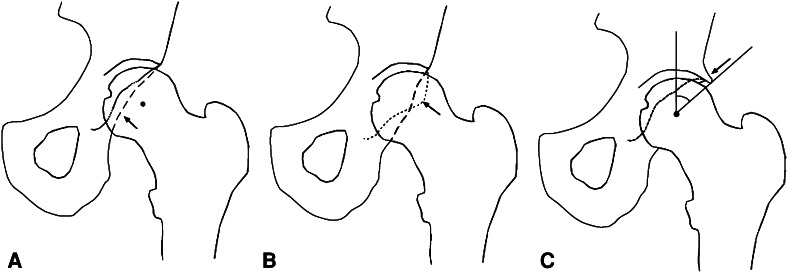
Fig. 2A–C.
(A) Normal anatomy of the hip (left) allows sufficient space for the caput to rotate properly in the acetabulum (right). In cam-type and pincer-type impingements, abnormal contact between the proximal femur and the acetabular rim disturbs adequate movement. (B) In cam-type impingement, during forceful motion, the aspheric portion of the head abuts and subsequently damages the acetabular rim, further damaging the cartilage and labrum. (C) In pincer-type impingement, an increase in either the coverage of the femoral head or the relative depth of the acetabulum causes an injured acetabular rim, followed by hypertrophy and degenerative changes in the labrum.
We, therefore, determined the prevalence of a positive femoroacetabular impingement test in a cohort of healthy young men and women, and examined associations of a positive test with (1) self-reported hip discomfort the past 3 months; (2) physical exercise; (3) clinically assessed hip ROM; and (4) radiographic findings associated with FAI.
Patients and Methods
This study was performed on healthy young adults 18 to 20 years old as part of the followups of the population-based ‘1989 Bergen Birth Cohort’ which comprised all babies born at Haukeland University Hospital during 1989 (n = 4703). They were part of a large randomized trial at birth, designed to assess different screening strategies for developmental dysplasia of the hip in 11,925 newborns born from 1988 to 1990 [43]. Between 2007 and 2009, 3935 of the 4703 subjects from the 1989 cohort were invited for long-term followups when they were 18 to 20 years old (Fig. 3). For this paper, we included only the 2344 who were invited after the impingement test was added to the clinical assessment. Of 2344 invited, 1170 (50%) attended the followups. These 1170 patients also were reported in our earlier report on radiographic FAI findings [24]. Patients with excessive pelvic rotation as assessed by an obturator foramen index outside 0.6 to 1.8 [51] or without radiographs owing to possible early pregnancy were excluded. Thus, 1152 patients, 480 men (42%; mean age, 19 years [SD, 0.4]) and 672 women (58%; mean age, 19 years [SD, 0.4]), were included for further analyses. Fifteen men and 46 women had been treated for developmental dysplasia of the hip as newborns. A sensitivity analysis was performed while considering an inverse probability weighted (IPW) approach to take into account a possible no response bias [44]. The results of the observed data were reported, as they gave similar results. The research protocol was approved by the Medical Research Ethics Committee of the Western Region of Norway and the Norwegian Data Inspectorate (No 3.2006.144). All participants gave written, informed consent, according to the Helsinki declaration.
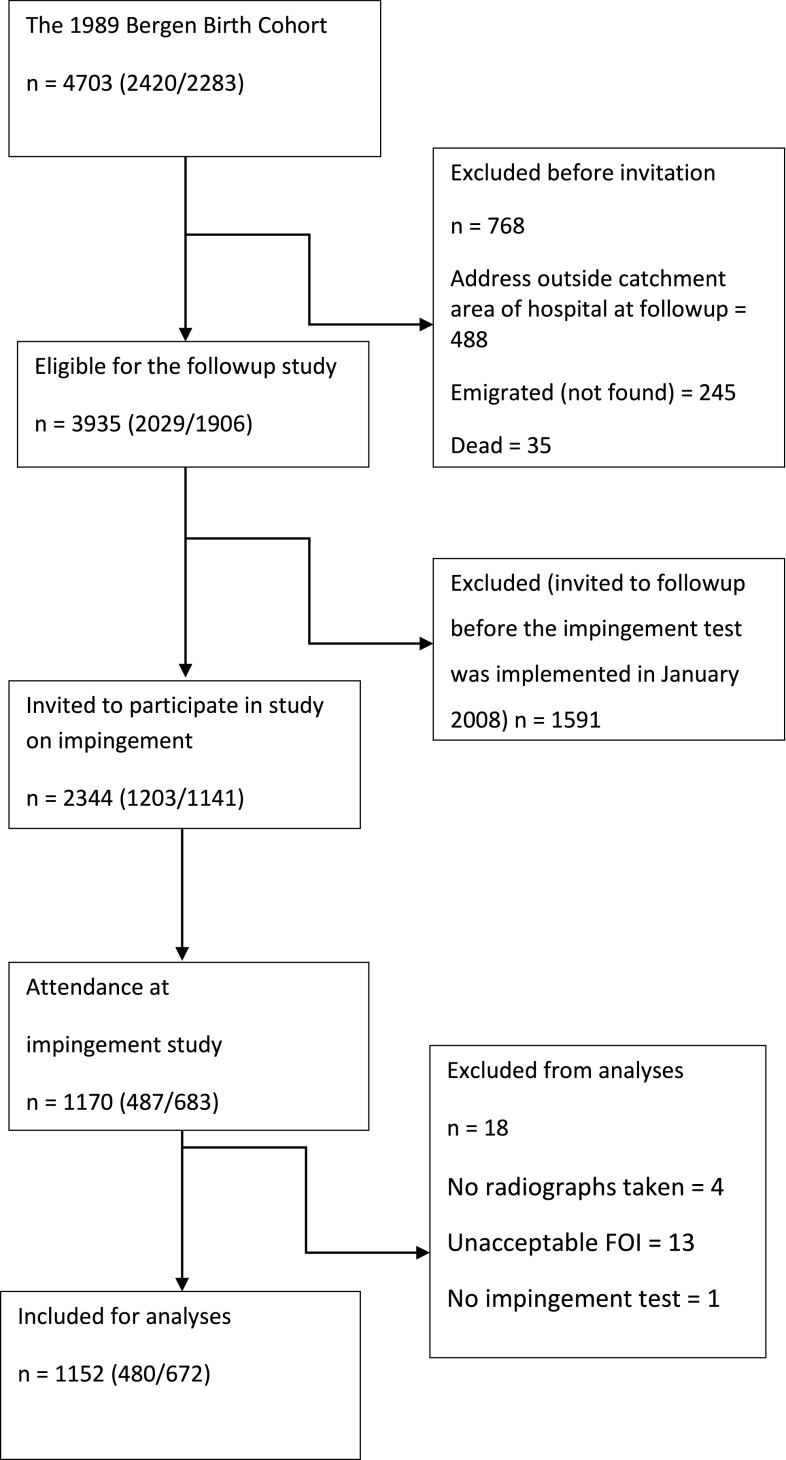
Fig. 3.
The flow chart shows the inclusion and exclusion criteria for our study (n = 1170) at followups. Babies with birth weight less than 1500 g, who died within the first month, or whose mother resided outside the catchment area of the hospital were not included in the 1989 Bergen Birth Cohort. FOI = obturator foramen index.
The followups consisted of questionnaires, clinical examinations, and two pelvic radiographs (one weightbearing AP view and one supine frog-leg view). The first questionnaire comprised questions on medical history, including hip-related problems in childhood, and the second questionnaire included computer-based standardized questionnaires on quality of life (EQ-5D) [50] and on hip problems (WOMAC™ osteoarthritis index) [4], and specific questions related to hip discomfort and to physical activity. The participants were asked the following questions regarding each hip separately: “Have you experienced hip discomfort from the hip the past 3 months?”, and “Outside school hours, how many hours do you usually exercise in your free time—so much that you get out of breath or sweat?” This last question originates from the WHO Health Behaviour in School Children (HBSC) physical activity questionnaire and had six response alternatives: none, about half an hour a week, about one hour a week, about 2 to 3 hours a week, about 4 to 6 hours a week, or 7 hours per week or more [5, 28, 40]. One experienced senior orthopaedic surgeon (LBE) standardized the clinical examination and trained the four less-experienced physicians (LBL, IØE, TGL, AMH). They were blinded to the results of the questions and the radiographs. A standardized protocol was obtained, including hip ROM and impingement test assessments. Flexion, abduction, and adduction were measured with the patient supine, whereas extension and internal and external rotations were measured with the patient prone and the knee flexed 90°. Extension was not measured in one man and six women.
The standardized radiographic examination was performed by a specially trained radiographer (ST) using a low-dose, digital radiography technique (Digital Diagnost X-ray System, release 1.5, Philips Medical Systems DMC GmbH, Hamburg, Germany). The mean total effective dose was 0.15 mSv for both radiographs together. Men were offered gonadal shields. In women, however, shields were not offered as they risk obscuring important anatomy. In addition, the effect of shielding on dose reduction in females has been questioned [2]. Hips were kept in a neutral abduction-adduction position with the toes directed forward for the AP view. The radiographer ensured correct posture to avoid excessive tilt or rotation of the pelvis [47]. We used a film and focus distance of 1.2 m and centered 2 cm proximal to the pubic symphysis for the AP view and at the pubis symphysis for the frog-leg view. All radiographs were blocked for patient confidentiality, and assessed by gross visual inspection on a high-resolution screen by one experienced pediatric musculoskeletal radiologist (KR). Positioning of the pelvis on the AP view and presence or absence of any of the qualitative cam-type and pincer-type radiographic findings on the two views were noted. In addition, all the AP views were assessed in a validated digital measurement program by three of the authors (LBL, IØE, TGL) (Adult DDH, University of Iowa Hospitals and Clinics, Iowa City, Iowa, USA) [9, 38]. The digital program initially included the center edge (CE) angle [52], and later was extended to include the alpha angle and the triangular index [13, 36] (Appendix 1). To assess a cam-type deformity one of the physicians (LBL) measured the alpha angle measurement and the triangular index (Fig. 4), while the radiologist (KR) by gross visual inspection determined the presence of a pistol grip deformity, focal prominence of the femoral neck, and lateral flattening of the femoral head [12, 20, 46] (Fig. 5). The presence of a pincer-type FAI was determined by measuring increased CE angles (LBL, IØE, TGL), indicating lateral overcoverage, and by gross visual inspection (KR) by the posterior wall sign and the crossover sign [12, 21, 37, 42, 52] (Fig. 6). The pistol grip deformity and the focal prominence were scored as positive if present in the AP and/or the frog-leg view. All other measurements were performed on the AP view. The alpha angle, crossover sign, and lateral flattening of the femoral head were not measured on three, 33, and five radiographs respectively.
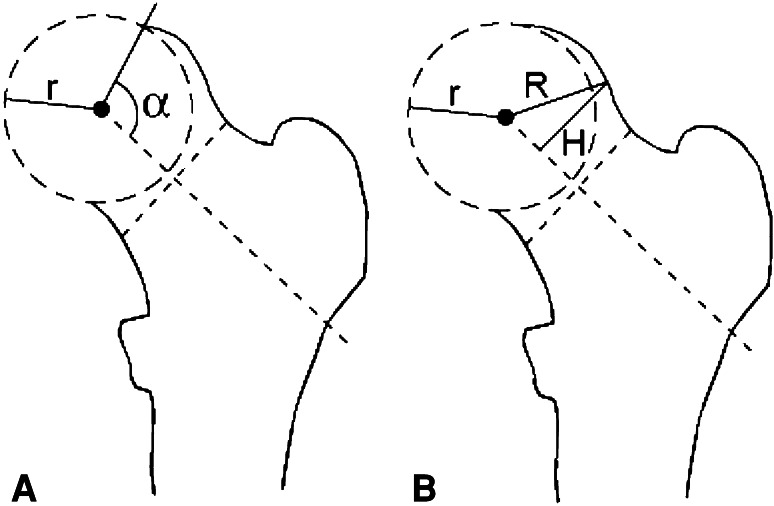
Fig. 4A–B.
(A) The alpha angle is the angle between a line running through the head center and the long axis of the femoral neck, and a line originating from the head center and to the point where the bone of the head neck junction crosses outside the radius curvature of the head. The higher the alpha angle, the greater the cam defect will be. (B) The triangular index is based on the equation R ≥ r + 2, where “r” is the head radius, and “R” is the pathologically increased radius. Half of the head radius distance measured along the neck axis is found, and a perpendicular line H is drawn up to the crossing point of the bony cam curvature. “R” then is found. If R ≥ r + 2, a head-neck asphericity indicating a cam type is confirmed.
Fig. 5A–C.
(A) A pistol-grip deformity is flattening of the normal concavity of the femoral head-neck junction. (B) A focal prominence is a prominence or bump to the femoral neck. (C) Flattening of the lateral aspect of the femoral head is shown in this drawing.
Fig. 6A–C.
(A) The posterior wall sign is scored positive when the posterior wall lies medial to the center of the femoral head. (B) The crossover-sign is scored positive when the upper part of the anterior acetabular wall lies more laterally than the posterior wall and crosses medially. (C) Excessive acetabular coverage leading to a deep acetabular socket is seen as a bony extension of the upper acetabular roof, quantified by an increased center-edge angle.
Interobserver reliabilities for flexion, extension, abduction, adduction, and external and internal rotations presented as intraclass correlation coefficients (ICC), have been reported as 0.87, 0.44, 0.34, 0.54, 0.18, and 0.79, respectively [39]. The κ value for interobserver variability for the anterior impingement test is reportedly 0.58 (95% CI, 0.29–0.87) [31], and the interobserver agreement for the impingement test is reportedly 96% [39]. A small interobserver study (30 right hips, 30 left hips) (LBE, TGL) showed the interrater agreement for the impingement test to be 95%. Two of the authors (blinded to the patients’ identification), measured and remeasured the images (after an interval of at least 8 weeks), and found intraobserver and interobserver agreements of κ = 0.85 and κ = 0.69, respectively for the triangular index, and 95% limits of agreement of intraobserver and interobserver variabilities for the alpha angle; −5.95°; 6.71° and −7.76°; 12.78°, respectively. Interobserver agreements for assessments of findings for the cam-type and pincer-type impingements were reported earlier (κ = 0.74–0.84) [24]. For the CE angle, the 95% limits of agreement of intraobserver and interobserver statistics have been reported at −4.18; 4.20 and −3.61; 3.32 [9].
The prevalences of a positive impingement test are presented as numbers (percentages) with corresponding 95% CIs. Differences in the prevalence of a positive impingement test according to sex and side were examined using Pearson chi-square test. Descriptive statistics for the variables considered as possible predictors of a positive impingement test were summarized by sex and side and were reported as numbers (percentages) or means (SD) as appropriate (Table 1). We used generalized estimating equations (GEE) models to study possible associations between the predictor variables and a positive impingement test. P values and prevalence rate ratios (PRR) with corresponding 95% CIs were estimated with GEE models [18], adjusted by side (left or right), to take into account the correlation between bilateral hips. The p value was used to evaluate the effect of the variables on a positive test. All the reported p values were two-tailed. A PRR value describes how the presence of a given variable alters the prevalence of a positive test; ie, a PRR of 3.1 means an increase of 210%. For continuous variables (hip ROM and CE angle) the PRR represents the increase of the prevalence for a unit (5°) change of the continuous variable.
Table 1.
Descriptive statistics for variables considered possible predictors of a positive impingement test
| Variable | Men, number (%) or mean (SD) | Women, number (%) or mean (SD) | ||
|---|---|---|---|---|
| Physical activity (hours/week), n (%) | ||||
| None | 41 (9) | 74 (11) | ||
| 0.5 | 37 (8) | 57 (9) | ||
| 1 | 55 (12) | 109 (17) | ||
| 2–3 | 113 (24) | 196 (30) | ||
| 4–6 | 122 (26) | 142 (22) | ||
| ≥ 7 | 104 (22) | 82 (12) | ||
| Right | Left | Right | Left | |
| Hip discomfort, n (%) | 7 (1.5) | 15 (3.1) | 47 (7) | 55 (8) |
| Hip ROM (°), mean (SD) | ||||
| Flexion | 118 (10) | 118 (10) | 122 (11) | 122 (11) |
| Abduction | 59 (6.0) | 59 (5.9) | 62 (6.5) | 62 (6.5) |
| Adduction | 38 (4.7) | 38 (4.6) | 39 (4.3) | 39 (4.4) |
| Extension | 26 (6.1) | 26 (6.1) | 28 (6.0) | 28 (6.0) |
| Internal rotation | 38 (12) | 38 (12) | 51 (12) | 52 (12) |
| External rotation | 58 (13) | 57 (13) | 47 (11) | 46 (11) |
| Radiographic cam-type findings | ||||
| Alpha borderline*, n (%) | 114 (24) | 99 (21) | 101 (15) | 111 (16) |
| Alpha pathologic**, n (%) | 39 (8.2) | 18 (3.8) | 124 (19) | 103 (15) |
| Triangular index, n (%) | 166 (35) | 163 (34) | 64 (10) | 45 (6.7) |
| Pistol grip, n (%) | 78 (16) | 93 (19) | 13 (1.9) | 19 (2.8) |
| Focal prominence, n (%) | 46 (10) | 50 (10) | 15 (2.2) | 17 (2.5) |
| Flattened lateral head, n (%) | 63 (13) | 71 (15) | 28 (4.2) | 34 (5.1) |
| 1 cam marker, n (%) | 70 (15) | 78 (17) | 180 (27) | 185 (28) |
| 2 cam markers, n (%) | 80 (17) | 77 (16) | 61 (9) | 46 (7) |
| ≥ 3 cam markers, n (%) | 78 (16) | 71 (15) | 12 (1.8) | 14 (2.1) |
| Radiographic pincer-type findings | ||||
| Acetabular overcoverage: | ||||
| CE angle (°), mean, (SD) | 32 (6) | 33 (6) | 31 (6) | 31 (6) |
| CE angle > 45°, n, (%) | 9 (1.9) | 10 (2.1) | 9 (1.3) | 8 (1.2) |
| Posterior wall sign, n, (%) | 100 (21) | 86 (18) | 70 (10) | 55 (8) |
| Crossover sign, n, (%) | 213 (46) | 228 (49) | 271 (41) | 273 (41) |
| 1 pincer marker, n, (%) | 158 (34) | 202 (43) | 217 (33) | 235 (35) |
| ≥ 2 pincer markers, n, (%) | 79 (17) | 59 (13) | 64 (10) | 49 (7) |
* Men, 69°–82°, women, 51°–56°, ** men ≥ 83°, women ≥ 57°.
Weekly physical activity was treated as a continuous variable with 1-hour increments; ie, a linear effect was assumed. The hip ROM values were continuous variables with 5° decrements. All the cam-type and pincer-type variables assessed by gross visual inspection were categorical variables. The alpha angle was categorized into normal (men (M) ≤ 68, women (W) ≤ 50), borderline (M = 69–82; W = 51–56), or pathologic (M ≥ 83; W ≥ 57) groups [13]. A CE angle greater than 45° was considered to indicate acetabular overcoverage [15]. The CE angle also was considered as a continuous variable with 5° increments. We created a radiographic composite score of 1, 2, or cam-type three or greater and of 1 or 2 or greater pincer-type findings, respectively. All 1152 patients included in the analyses had the clinical examinations, impingement tests, and radiographs taken. For the analyses only patients without missing data were analyzed for each variable. Statistics were performed in Stata® Statistical Software: Release 11 (StataCorp LP®, College Station, TX, USA) and in IBM® SPSS® Statistics, version 20.0 (Armonk, New York, USA).
Results
Based on the worst affected (ie, at least one) hip, 35 of 480 men (7.3%) and 32 of 672 women (4.8%) had positive tests for anterior impingement (Table 2). Fourteen of 480 (2.9%) men and eight of 672 (1.2%) women tested positive bilaterally. The differences in the prevalences of a positive test for males compared with females were 21 of 480 versus 24 of 672 unilaterally (p = 0.451), 14 of 480 versus eight of 672 bilaterally (p = 0.039), and 35 of 480 versus 32 of 672 when based on at least one hip (p = 0.073).
Table 2.
Positive tests for anterior impingement in 480 men and 672 women
| Positive test for anterior impingement | Men, number (%) | 95% CI | Women, number (%) | 95% CI |
|---|---|---|---|---|
| Right hip | 25 (5.2) | 3.2–7.2 | 18 (2.7) | 1.5–3.9 |
| Left hip | 24 (5.0) | 3.0–7.0 | 22 (3.3) | 1.9–4.6 |
| Unilateral | 21 (4.4) | 2.5–6.2 | 24 (3.6) | 2.2–5.0 |
| Bilateral | 14 (2.9) | 1.4–4.4 | 8 (1.2) | 0.4–2.0 |
| At least one hip (worst) | 35 (7.3) | 5.0–9.6 | 32 (4.8) | 3.1–6.4 |
The 95% CIs were calculated using binomial CIs.
Self-reported hip discomfort during the past 3 months was associated with positive impingement tests by women (p < 0.001), but not by men (p = 0.437) (Table 3).
Table 3.
Analysis of associations of positive impingement tests
| Variable | Men | Women | ||||
|---|---|---|---|---|---|---|
| p value | PRR* | 95% CI** | p value | PRR* | 95% CI** | |
| Physical exercise (hours/week) | 0.001 | 1.23 | 1.08–1.40 | 0.967 | 1.00 | 0.86–1.15 |
| Hip discomfort past 3 months | 0.437 | 1.67 | 0.46–6.15 | < 0.001 | 3.88 | 1.90; 7.92 |
| Hip ROM (5° decrement) | ||||||
| Flexion | 0.062 | 1.16 | 0.99–1.35 | 0.003 | 1.24 | 1.08–1.44 |
| Abduction | 0.018 | 1.32 | 1.05–1.67 | 0.271 | 1.15 | 0.90–1.46 |
| Adduction | 0.675 | 1.08 | 0.76–1.53 | 0.271 | 0.78 | 0.51–1.21 |
| Extension | 0.119 | 1.22 | 0.95–1.57 | 0.133 | 1.26 | 0.93–1.71 |
| Internal rotation | 0.001 | 1.31 | 1.12–1.54 | 0.366 | 0.93 | 0.80–1.08 |
| External rotation | 0.212 | 0.92 | 0.81–1.05 | 0.243 | 1.10 | 0.94–1.28 |
| Radiographic cam findings | ||||||
| Alpha angle borderline† | 0.518 | 1.23 | 0.66–2.28 | 0.724 | 0.85 | 0.35–2.06 |
| Alpha pathological‡ | 0.249 | 1.68 | 0.69–4.08 | 0.647 | 1.20 | 0.55–2.60 |
| Triangular index | 0.288 | 1.33 | 0.78–2.27 | 0.372 | 0.51 | 0.11–2.25 |
| Pistol grip deformity | 0.548 | 1.26 | 0.59–2.67 | 0.945 | 1.08 | 0.13–8.63 |
| Focal prominence | 0.181 | 1.70 | 0.78–3.68 | 0.930 | 1.10 | 0.14–8.77 |
| Flattened lateral head | 0.165 | 1.71 | 0.80–3.65 | – | – | – |
| Composite cam score | ||||||
| 1 | 0.043 | 2.04 | 1.02–4.09 | 0.980 | 1.01 | 0.52–1.97 |
| 2 | 0.050 | 2.04 | 1.00–4.18 | 0.224 | 0.31 | 0.05–2.06 |
| ≥ 3 | 0.309 | 1.58 | 0.65–3.83 | 0.878 | 1.18 | 0.14–9.66 |
| Radiographic pincer findings | ||||||
| Acetabular overcoverage§ | 0.367 | 0.89 | 0.70–1.14 | 0.508 | 0.91 | 0.69–1.20 |
| Posterior wall sign | 0.921 | 0.96 | 0.47–1.97 | 0.199 | 0.25 | 0.03–2.10 |
| Crossover sign | 0.804 | 0.93 | 0.51–1.68 | 0.189 | 0.62 | 0.30–1.27 |
| Composite pincer score | ||||||
| 1 | 0.780 | 1.09 | 0.60–1.99 | 0.281 | 0.67 | 0.32–1.39 |
| ≥ 2 | 0.598 | 0.78 | 0.30–1.99 | 0.175 | 0.21 | 0.02–2.00 |
* PRR = prevalence rate ratio describes how the presence of a given variable alters the prevalence of a positive test; ** 95% CI, PRR values are presented with corresponding 95% CI; †men, 69°–82°, women, 51°–56°; ‡men ≥ 83°, women ≥ 57°; §based on a continuous center-edge angle with 5° increment; ¶none of the women with a flattened lateral head had a positive impingement test and therefore the statistical model is not valid in this case.
Increased physical exercise was found to be associated by men (p = 0.001) but not by women (p = 0.967) (Table 3).
As for the ROM, decreased hip flexion in women and men (p = 0.003 and p = 0.062), and abduction (p = 0.018) and internal rotation (p = 0.001) for men were associated with positive impingement tests (Table 3).
A cam-type finding was associated with positive impingement tests in men for a composite score value of one or two (p = 0.043 and p = 0.050, respectively) positive findings, respectively. In men with three or more positive findings, no association was seen with a positive test (p = 0.309) (Table 3). Radiographic pincer-type findings were not associated with positive tests in either gender.
Discussion
The prevalence of a positive anterior impingement test and its association with clinical and radiographic findings thought to be related to FAI remain unconfirmed in healthy young adults. We, therefore, determined the prevalence of a positive impingement test in a population-based cohort of 1170 young adults and examined possible associations of a positive test with (1) self-reported hip discomfort; (2) physical exercise; (3) clinically assessed hip ROM; and (4) radiographic findings associated with FAI.
We acknowledge some limitations that require consideration. First we had a moderate attendance rate of 50%. A selection bias could exist, as the cohort was drawn from a previous population-based hip trial designed to evaluate the effect of ultrasound screening in the diagnosis of hip dysplasia in newborns. Those who received a hip ultrasound as newborns or experienced hip-related problems in infancy possibly could be more prone to participate, along with participants with hip-related problems at the time of followups. A sensitivity analysis with an inverse probability weighted approach, however, did not reveal any no-response bias. Furthermore, no noteworthy differences in growth data characteristics for attendees and nonattendees were seen at birth or at 7 years of age, except for sex distribution, as reported previously [24]. Second, our cohort was homogenous and young, and there are likely to be at-risk patients who have not had the anterior acetabular labral disorder fully developed that will make the impingement test positive, even though they have typical radiographic cam-type findings. The prevalences presented here therefore are likely to be age-dependent. Further followup of the cohort may provide more answers. Third, there is the possibility of a false positive or false negative impingement test. According to the literature, the sensitivity and specificity of the test for anterior impingement are 70% and 44%, when the test represents the most painful provocative movement [35]. In addition, patients with acetabular dysplasia could test positive [25, 27]. A high positive predictive value of the anterior impingement test was recently reported [17]. Fourth, the question regarding hip discomfort during the past 3 months for each of the hips was not validated. However, it appeared to be appropriate and without risk for confusion. Fifth, our digital software program allowed measurements of the alpha angle on the AP view only, which is believed adequate by some authors [13, 22, 34]. Others advocate the modified Dunn or the frog-leg view shows the cam deformity better [7, 32]. We therefore included scoring of the cam-type findings from the frog-leg view into the composite cam score. The strengths of our study included the population-based cohort design with a homogenous age group, the standardized protocols for radiographic and clinical examination, and GEE models to account for the correlation between bilateral hips when evaluating the associations with the different variables.
The prevalence of clinically assessed FAI has been estimated at 10% to 15% in a general adult population [26], as compared with our figures of 7.3% in men and 4.8% in women at age 19 years. The difference may in part be age-related, as the impingement test turns positive after labral damage has occurred; ie, with time. A study presenting the prevalence of cam type FAI morphology in 200 asymptomatic volunteers (89 men, 111 women; mean age 29.4 years) reported three of 200 patients (1.5%) had tested positive for anterior impingement [16]. Patients with ongoing hip or groin problems and/or earlier childhood hip problems were not included, which may explain the lower prevalence of positive tests compared with our results. Numerous studies reported the prevalence of radiographic cam type FAI (Table 4). Overall, the radiographic prevalence in young men was higher than the prevalence of the positive impingement test. Followup studies are needed to understand if these radiographic cam-type findings actually represent a potentially large amount of at-risk patients in a presumed presymptomatic FAI stage.
Table 4.
Prevalence of femoroacetabular impingement reported in the literature
| Study | Year | Country | Study population | Prevalence of FAI, based on: | Radiographic modality and FAI findings | |
|---|---|---|---|---|---|---|
| Positive impingement test | Radiographic cam findings | |||||
| Gosvig et al. [14] | 2008 | Denmark | 3202 (M = 1184, F = 2018) | M = 17%, F = 4%, age range, 22–93 years | Standardized AP pelvic radiographs, alpha angle, and triangular index | |
| Hack et al. [16] | 2010 | Canada | 200 (M = 89, F = 111); mean age, 29 years (range, 21–51 years) | At least one hip, 1.5% (M + F) | 14% (M + F) (10.5% unilateral, 3.5% bilateral) M = 25%, F = 5% | MRI, alpha angle |
| Reichenbach et al. [41] | 2010 | Switzerland | M = 244; mean age, 20 years | M = 24% | MRI, scoring system for grading the maximum offset of the head-neck junction | |
| Jung et al. [22] | 2011 | USA | 380 (M = 108, F = 272); M = mean age, 63 years (range, 27–93 years), F = 60 years (range, 26–91 years) |
M: pathological (≥ 83°): 14%, borderline (6–82°): 15%; F: pathological (≥ 57°): 6%; borderline (51–56°): 6% |
AP pelvic CT scout, alpha angle | |
| Laborie et al. [24] | 2011 | Norway | 2060 (M = 868, F = 1192); mean age, 19 years (range, 17–20 years) | At least one hip, M = 35%, F = 10%; M = 25%, F = 6% |
Standardized AP and frog-leg pelvic radiograph, subjective evaluation of cam type | |
| Current study | 2012 | Norway | 1152* (M = 480, F = 672); mean age, 19 years (SD 0.4). | At least one hip: M = 7.3%, F = 4.8% Bilaterally: M = 2.9%, F = 1.2% |
||
FAI = femoroacetabular impingement; * these 1152 were included in the study by Laborie et al. [24].
We found that radiographic cam-type findings were associated with a positive impingement test in men for a composite score value of one or two findings. No such association was seen in women. Interestingly, we found no association between the alpha angle measurement and a positive impingement test, in accordance with earlier findings [16]. The radiographic cam-type findings might be associated with lower-limb dominance in sporting activities, particularly those involving hip flexion, for instance, soccer. We found a higher level of weekly physical activity was associated with positive tests in men. Others have found that 70% of patients with FAI participated in sporting activities, 30% of them on a high-level basis [35]. Our results support these findings. We have confirmed a positive test also is associated with decreased hip ROM in both genders for flexion, and for internal rotation and abduction in men. In a prospective study [6] of 51 patients with FAI (29 men, 22 women; mean age, 35 years), 88% had positive tests for anterior impingement, and internal rotation and hip flexion were confirmed to be reduced in symptomatic patients with FAI.
Overall, a positive test for anterior impingement in a cohort of healthy young adults is not uncommon, with a higher prevalence in men (7.3%) than in women (4.8%). A positive impingement test is associated with radiographic cam-type FAI and increasing physical activity in men, confirming the cam-type impingement is more common in young, active men. Self-reported hip discomfort was associated with positive tests in women. Our results also confirm the decrease in ROM in patients with positive impingement tests, particularly for flexion and internal rotation, and also in abduction. It is important that the anterior impingement test along with hip ROM tests are used in a standardized fashion. FAI can be difficult, clinically and radiographically, to diagnose, and a consensus regarding the radiographic criteria is needed.
Acknowledgments
We thank Deborah M. Eastwood MB FRCS, Department of Orthopaedics, Great Ormond Street Hospital for Children, London, UK, for excellent help and support throughout preparation of the manuscript; Francesco Sera (supported by the Arthritis Research UK grant, Ref 18196), MRC Centre of Epidemiology for Child Health, UCL Institute of Child Health, UK, for excellent help in performing the statistical analyses of this study; radiographer, Sigrun Tufta (ST), Department of Radiology, Haukeland University Hospital, for performing all the radiographic examinations during the followups; Monica Olsen, nurse, Department of Orthopedics, for logistic work during the followup consultations; Anne Marte Haukom MD, Haukeland University Hospital, for performing some of the clinical examinations during the followups; and graphic illustrator, Ellinor Moldeklev Hoff, Department of Photography and Drawing, University of Bergen, Norway, for drawing the figures.
Appendix 1: The Digital Measurement Program Adult DDH
The digital measurement program (Adult DDH, University of Iowa Hospitals and Clinics, Iowa City, Iowa, USA) [9, 38], was expanded to include the measurements of the alpha angle and triangular index on the AP view.
First, four points outline the femoral head circle, identical to the circle otherwise applied in the manner described by Mose [33], using a hard transparent plastic sheet containing concentric circles. The four points are placed in the medial and superior part of the head circumference, the most lateral corresponding approximately to the point facing the lateral acetabular edge. None of the four points are placed directly in the cam region. The program automatically generates the best-fit circle based on these four points. Afterward, two more points depict the narrowest collum width, and the program automatically adds the mid-axis of the collum, connecting the middistance of the narrowest collum width to the head center. Then the alpha angle is determined by adding a point where the bony head femoral junction crosses outside the femoral head circle. Last, the program automatically draws a line perpendicular to the midaxis of the collum, at the distance of half the radius from the circle center. The last point, determining the triangular index, is set where this line intersects with the bony curvature of the head-neck junction (H). The program then calculates the distance from this point until the head center (R).
Footnotes
The institution of one or more of the authors has received, during the study period, funding from Helse-Vest (LBL, IØE), the Frank Mohn Foundation (TGL), the University of Bergen (KR, LBE), and the Arthritis Research Campaign (grant number 18196).
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg. consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Haukeland University Hospital, Bergen, Norway.
References
- 1.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91:162–169. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 2.Bardo DM, Black M, Schenk K, Zaritzky MF. Location of the ovaries in girls from newborn to 18 years of age: reconsidering ovarian shielding. Pediatr Radiol. 2009;39:253–259. doi: 10.1007/s00247-008-1094-4. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Booth ML, Okely AD, Chey T, Bauman A. The reliability and validity of the physical activity questions in the WHO health behaviour in schoolchildren (HBSC) survey: a population study. Br J Sports Med. 2001;35:263–267. doi: 10.1136/bjsm.35.4.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clohisy JC, Knaus ER, Hunt DM, Lesher JM, Harris-Hayes M, Prather H. Clinical presentation of patients with symptomatic anterior hip impingement. Clin Orthop Relat Res. 2009;467:638–644. doi: 10.1007/s11999-008-0680-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. doi: 10.1097/BLO.0b013e3180f60b53. [DOI] [PubMed] [Google Scholar]
- 8.Crawford JR, Villar RN. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87:1459–1462. doi: 10.1302/0301-620X.87B11.16821. [DOI] [PubMed] [Google Scholar]
- 9.Engesaeter IO, Laborie LB, Lehmann TG, Sera F, Fevang J, Pedersen D, Morcuende J, Lie SA, Engesaeter LB, Rosendahl K. Radiological findings for hip dysplasia at skeletal maturity: validation of digital and manual measurement techniques. Skeletal Radiol. 2012;41:775–785. doi: 10.1007/s00256-011-1283-3. [DOI] [PubMed] [Google Scholar]
- 10.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 11.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 13.Gosvig KK, Jacobsen S, Palm H, Sonne-Holm S, Magnusson E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J Bone Joint Surg Br. 2007;89:1309–1316. doi: 10.1302/0301-620X.89B10.19405. [DOI] [PubMed] [Google Scholar]
- 14.Gosvig KK, Jacobsen S, Sonne-Holm S, Gebuhr P. The prevalence of cam-type deformity of the hip joint: a survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008;49:436–441. doi: 10.1080/02841850801935567. [DOI] [PubMed] [Google Scholar]
- 15.Gosvig KK, Jacobsen S, Sonne-Holm S, Palm H, Troelsen A. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 2010;92:1162–1169. doi: 10.2106/JBJS.H.01674. [DOI] [PubMed] [Google Scholar]
- 16.Hack K, DiPrimio G, Rakhra K, Beaule PE. Prevalence of cam-type femoroacetabular impingement morphology in asymptomatic volunteers. J Bone Joint Surg Am. 2010;92:2436–2444. doi: 10.2106/JBJS.J.01280. [DOI] [PubMed] [Google Scholar]
- 17.Hananouchi T, Yasui Y, Yamamoto K, Toritsuka Y, Ohzono K. Anterior impingement test for labral lesions has high positive predictive value. Clin Orthop Relat Res. 2012;470:3524–3529. doi: 10.1007/s11999-012-2450-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- 19.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271. doi: 10.1097/01.blo.0000144861.11193.17. [DOI] [PubMed] [Google Scholar]
- 20.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620X.83B2.11092. [DOI] [PubMed] [Google Scholar]
- 21.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res. 2007;25:758–765. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 22.Jung KA, Restrepo C, Hellman M, AbdelSalam H, Morrison W, Parvizi J. The prevalence of cam-type femoroacetabular deformity in asymptomatic adults. J Bone Joint Surg Br. 2011;93:1303–1307. doi: 10.1302/0301-620X.93B10.26433. [DOI] [PubMed] [Google Scholar]
- 23.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome: a clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]
- 24.Laborie LB, Lehmann TG, Engesaeter IO, Eastwood DM, Engesaeter LB, Rosendahl K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology. 2011;260:494–502. doi: 10.1148/radiol.11102354. [DOI] [PubMed] [Google Scholar]
- 25.Lequesne M, Bellaiche L. Anterior femoroacetabular impingement: an update. Joint Bone Spine. 2012;79:249–255. doi: 10.1016/j.jbspin.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 26.Leunig M, Ganz R. [Femoroacetabular impingement: a common cause of hip complaints leading to arthrosis][in German] Unfallchirurg. 2005;108:9–17. doi: 10.1007/s00113-004-0902-z. [DOI] [PubMed] [Google Scholar]
- 27.Leunig M, Podeszwa D, Beck M, Werlen S, Ganz R. Magnetic resonance arthrography of labral disorders in hips with dysplasia and impingement. Clin Orthop Relat Res. 2004;418:74–80. doi: 10.1097/00003086-200401000-00013. [DOI] [PubMed] [Google Scholar]
- 28.Liu Y, Wang M, Tynjala J, Lv Y, Villberg J, Zhang Z, Kannas L. Test-retest reliability of selected items of Health Behaviour in School-aged Children (HBSC) survey questionnaire in Beijing. China. BMC Med Res Methodol. 2010;10:73. doi: 10.1186/1471-2288-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacDonald SJ, Garbuz D, Ganz R. Clinical Evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9. [Google Scholar]
- 30.Martin RL, Kelly BT, Leunig M, Martin HD, Mohtadi NG, Philippon MJ, Sekiya JK, Safran MR. Reliability of clinical diagnosis in intraarticular hip diseases. Knee Surg Sports Traumatol Arthrosc. 2010;18:685–690. doi: 10.1007/s00167-009-1024-5. [DOI] [PubMed] [Google Scholar]
- 31.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77. doi: 10.2519/jospt.2008.2677. [DOI] [PubMed] [Google Scholar]
- 32.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. doi: 10.1097/01.blo.0000201168.72388.24. [DOI] [PubMed] [Google Scholar]
- 33.Mose K. Methods of measuring in Legg-Calve-Perthes disease with special regard to the prognosis. Clin Orthop Relat Res. 1980;150:103–109. [PubMed] [Google Scholar]
- 34.Nicholls AS, Kiran A, Pollard TC, Hart DJ, Arden CP, Spector T, Gill HS, Murray DW, Carr AJ, Arden NK. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: a nested case-control study. Arthritis Rheum. 2011;63:3392–3400. doi: 10.1002/art.30523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nogier A, Bonin N, May O, Gedouin JE, Bellaiche L, Boyer T, Lequesne M; French Arthroscopy Society. Descriptive epidemiology of mechanical hip pathology in adults under 50 years of age: prospective series of 292 cases: clinical and radiological aspects and physiopathological review. Orthop Traumatol Surg Res. 2010;96(8 suppl):S53–S58. [DOI] [PubMed]
- 36.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 37.Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. doi: 10.5435/00124635-200709000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Pedersen DR, Lamb CA, Dolan LA, Ralston HM, Weinstein SL, Morcuende JA. Radiographic measurements in developmental dysplasia of the hip: reliability and validity of a digitizing program. J Pediatr Orthop. 2004;24:156–160. doi: 10.1097/01241398-200403000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010;2:888–895. doi: 10.1016/j.pmrj.2010.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rangul V, Holmen TL, Kurtze N, Cuypers K, Midthjell K. Reliability and validity of two frequently used self-administered physical activity questionnaires in adolescents. BMC Med Res Methodol. 2008;8:47. doi: 10.1186/1471-2288-8-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reichenbach S, Juni P, Werlen S, Nuesch E, Pfirrmann CW, Trelle S, Odermatt A, Hofstetter W, Ganz R, Leunig M. Prevalence of cam-type deformity on hip magnetic resonance imaging in young males: a cross-sectional study. Arthritis Care Res (Hoboken). 2010;62:1319–1327. doi: 10.1002/acr.20198. [DOI] [PubMed] [Google Scholar]
- 42.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. doi: 10.1302/0301-620X.81B2.8291. [DOI] [PubMed] [Google Scholar]
- 43.Rosendahl K, Markestad T, Lie RT. Ultrasound screening for developmental dysplasia of the hip in the neonate: the effect on treatment rate and prevalence of late cases. Pediatrics. 1994;94:47–52. [PubMed] [Google Scholar]
- 44.Seaman SR, White IR. Review of inverse probability weighting for dealing with missing data. Stat Methods Med Res. 2011 Jan 10. [Epub ahead of print] [DOI] [PubMed]
- 45.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 46.Siebenrock KA, Wahab KH, Werlen S, Kalhor M, Leunig M, Ganz R. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;418:54–60. doi: 10.1097/00003086-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 47.Sierra RJ, Trousdale RT, Ganz R, Leunig M. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689–703. doi: 10.5435/00124635-200812000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Stulberg SD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthitis of the hip. In: Cordell LD, Harris WH, Ramsey PL, MacEwen GD, editors. Proceedings of the Third Open Scientific Meeting of The Hip Society. St Louis, MO: CV Mosby; 1975. pp. 212–228. [Google Scholar]
- 49.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis: what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. doi: 10.2214/AJR.06.0921. [DOI] [PubMed] [Google Scholar]
- 50.The EuroQol Group EuroQol: a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 51.Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 52.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand. 1939;83(suppl 58):5–135. [Google Scholar]
- 53.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. doi: 10.1097/BLO.0b013e3180399430. [DOI] [PubMed] [Google Scholar]