Abstract
Background
The majority (86%) of THAs performed in the United States are uncemented. This may increase the revision burden if uncemented fixation is associated with a higher risk of revision than other approaches.
Question/purposes
We sought to investigate trends for use of uncemented fixation and to analyze age-stratified risk of revision comparing cemented, hybrid, and uncemented fixation as reported by national hip arthroplasty registries.
Methods
Data were extracted from the annual reports of seven national hip arthroplasty registries; we included all national registries for which annual reports were available in English or a Scandinavian language, if the registry had a history of more than 5 years of data collection.
Results
Current use of uncemented fixation in primary THAs varies between 15% in Sweden and 82% in Canada. From 2006 to 2010 the registries of all countries reported overall increases in the use of uncemented fixation; Sweden reported the smallest absolute increase (from 10% to 15%), and Denmark reported the greatest absolute increase (from 47% to 68%). Looking only at the oldest age groups, use of uncemented fixation also was increasing during the period. In the oldest age group of each of the registries we surveyed (age older than 65 years for England-Wales; age older than 75 years in three registries), cemented fixation was associated with a lower risk of revision than was uncemented fixation.
Conclusions
Increasing use of uncemented fixation in THA is a worldwide phenomenon. This trend is paradoxic, given that registry data, which represent nationwide THA outcomes, suggest that cemented fixation in patients older than 75 years results in the lowest risk of revision.
Level of Evidence
Level II, systematic review. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Surgeons perform more than a quarter of a million primary THAs each year in the United States [13]. As a result of a growing population of elderly, the demand for primary THAs is estimated to increase to more than half a million before 2030, and as a consequence, the revision burden is projected to double during the same period [15]. Optimized treatment strategies to secure high rates of long-term implant survivorship, and thereby keep the revision burden as low as possible, are warranted.
One epidemiologic estimate of current practice in the United States has suggested that 86% of primary THAs are uncemented, most of the rest use hybrid fixation, and less than 1% of THAs are fully cemented [13]. A poll among members of the American Academy of Orthopaedic Surgeons (AAOS) at the 2009 annual meeting regarding preferences in THA revealed 47% of respondents used an uncemented femoral component in all cases, and another 47% used uncemented femoral components in 75% or more of cases [2].
However, fixation strategies vary widely in other countries. In contrast to the United States, Sweden generally has favored cemented implants; only approximately 15% of THAs there were uncemented in 2010 [21]. Countries with hip arthroplasty registries have valid and population-based numbers for the use of different fixation types. Countries with longer-standing (minimum > 5 years) hip arthroplasty registries include Australia, Canada, Denmark, England-Wales, Finland, New Zealand, Norway, and Sweden. The registries convey valid estimates for risk of revision THA for different fixation types and specific implant designs [19, 20].
Good long-term survivorship has been reported for cemented and uncemented THA implants in single-center studies from North America [3, 4, 7, 9]. However, these studies are limited as they may not represent the national composite implant survivorship data that could be anticipated for the THAs performed across all orthopaedic facilities in the United States. Assuming that nationwide collection of data in countries with longer-standing hip arthroplasty registries would resemble a data collection in the United States, assessment of these registry data is appropriate if nationwide quality of THA is of concern.
We sought to use established national hip registries to answer the following questions: (1) In the registries, what fraction of THAs are uncemented? (2) Has uncemented fixation become more or less common during the past half decade? (3) After stratifying by age, what fixation strategies (cemented versus uncemented, cemented versus hybrid, and hybrid versus uncemented) lead to the lowest risk of revision?
Methods and Materials
Countries with established hip arthroplasty registries or current studies underway to develop a registry include: Australia, Austria, Canada, Croatia, Czech Republic, Denmark, England-Wales, Finland, France, Holland, Hungary, Italy, Ireland, Lithuania, New Zealand, Norway, Portugal, Romania, Scotland, Slovakia, Slovenia, South Africa, Spain, Sweden, Switzerland, the United States, and Turkey. In the current study, we reviewed registry reports if these were available in English or a Scandinavian language and if the registry had a history of more than 5 years of data collection. Thus, we included data from hip arthroplasty registries from Australia [1], Canada [5], Denmark [8], England-Wales [18], New Zealand [22], Norway [23], and Sweden [21] (reports from Finland could not be readily downloaded and no response was received following written inquiry to the registry).
The registries rely on the reporting of data from primary and revision surgeries to one national database. Five of the surveyed registries have a high completeness for primary THA (≥ 93%) (Table 1). Completeness is the number of procedures reported to the registry of the actual number of procedures performed. The reported data for primary THAs include information regarding a unique patient identification or social security number and the surgically treated side, thus making it possible to pair any secondary revision surgeries to the primary surgery. Data of interest for late-stage revisions reported to the registries include: brand, design, and fixation of the acetabular and femoral components; femoral head size, modularity, and material; and acetabular liner material.
Table 1.
Registry data for THAs
| Country | Year of initiation | Completeness | Number of primary THAs reported | Last year of followup |
|---|---|---|---|---|
| Australia | 1999 | 93%* | 211,114 | December 2010 |
| Canada | 2001 | 42%‡ | 80,062 | March 2010 |
| Denmark | 1995 | 96.3% | 103,424 | December 2010 |
| New Zealand | 1997 | 98% | 71,057 | December 2010 |
| Norway | 1987 | 100%† | 132,179 | December 2010 |
| England-Wales | 2003 | 83.4%‡ | 405,074 | March 2010 |
| Sweden | 1979 | 98.5%§ | 330,990 | December 2010 |
* Completeness for validated records; †completeness since 1989; ‡completeness includes hip and knee arthroplasties; §completeness for 2010.
During April 2012, we reviewed the annual reports from included hip arthroplasty registries to extract information regarding: (1) the current (2010) use of uncemented fixation in primary THAs as a percentage of all primary THAs as reported in the most recently available reports (2011 annual reports); (2) the use of uncemented fixation in primary THAs as a percentage of all primary THAs for each year from 2006 through 2010, thus establishing a trend of uncemented fixation for each country during that past half decade. For Australia, Denmark, England-Wales, and Norway, we were able to extract these data for the oldest age groups separately (> 75 years for Australia, and Denmark; > 65 years for England-Wales; and > 60 years for Norway); and (3) age-stratified risk estimates of revision when comparing THA with different fixation techniques: cemented versus uncemented, cemented versus hybrid (cemented stem), and hybrid (cemented stem) versus uncemented. These age-stratified risk estimates could be extracted from the registries of Australia, Denmark, England-Wales, and New Zealand. For England-Wales, the risk estimates were reported for each sex separately. Australia, Denmark, and England-Wales report risk estimates as hazard ratios, and New Zealand reports revision rate per 100 component years.
Descriptive statistics are applied. Categorical data are presented as percentages, and risk estimates of revisions when comparing fixation techniques are grouped and color-coded according to whether statistical significance was observed (white or black) or not (grey).
Results
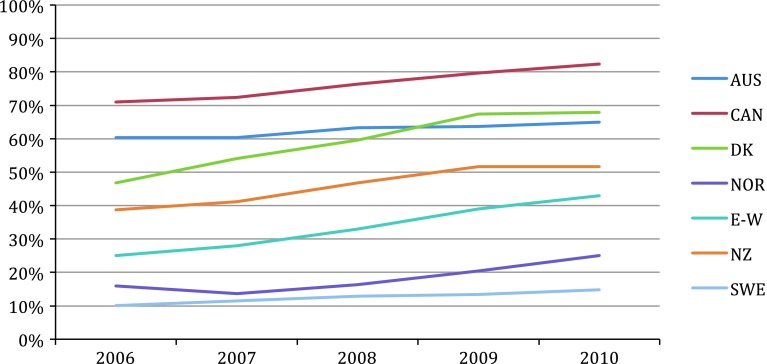
The current use of uncemented fixation varies between 15% and 82% of all primary THAs reported to the registries (Fig. 1). The lowest prevalence of uncemented fixation is in Sweden (15%) and Norway (25%). They are followed by England-Wales (43%), New Zealand (51%), Australia (65%), Denmark (68%), and Canada with a prevalence of uncemented fixation of 82%.
Fig. 1.
The percentages of uncemented fixation of all primary THAs each year from 2006 to 2010 are shown. AUS = Australia; CAN = Canada; DK = Denmark; E-W = England-Wales; NOR = Norway; NZ = New Zealand; SWE = Sweden.
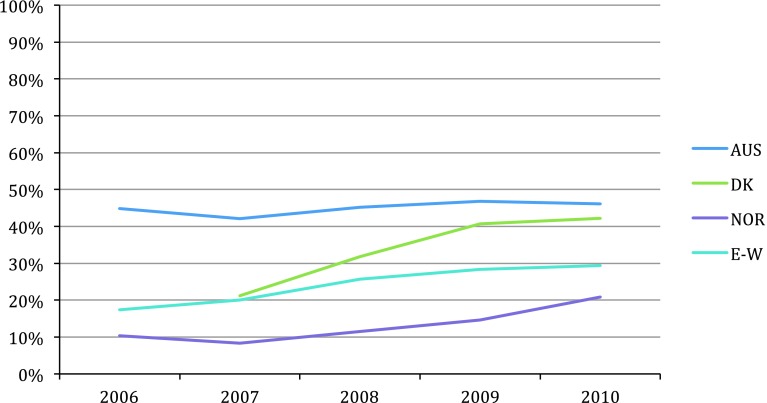
From 2006 to 2010, the registries of all countries reported overall increases in uncemented fixation use (Fig. 1). The smallest absolute increases in uncemented fixation use during the period in question were reported by the Swedish (from 10% to 15%) and Australian (from 60% to 65%) registries. The largest absolute increases in uncemented fixation use were reported by the Danish (from 47% to 68%) and England-Wales (from 25% to 43%) registries. In Canada, New Zealand, and Norway, the absolute prevalence of uncemented fixation use increased by 10% to 12% during the period. Uncemented fixation use for the oldest age group reported by Australia, Denmark, England-Wales (> 75 years for all), and Norway (> 60 years) also shows overall increases during the period (Fig. 2). The increases approximate those observed for uncemented fixation use in all age groups (Fig. 1). The current prevalence of uncemented fixation use in the oldest age group is 47% in Australia, 42% in Denmark, 29% in England-Wales, and 21% in Norway.
Fig. 2.
The percentages of uncemented fixation of all THAs performed in patients older than 75 years (Norway, > 60 years) each year from 2006 to 2010 are shown. Data could not be extracted for Denmark in 2006. AUS = Australia; DK = Denmark; E-W = England-Wales; NOR = Norway.
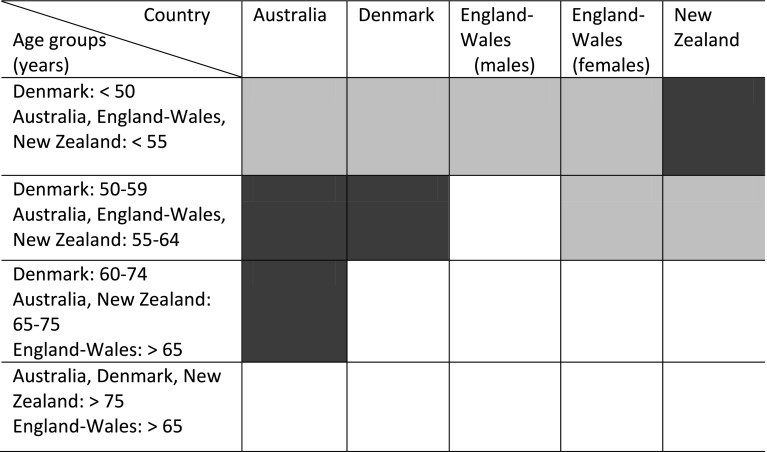
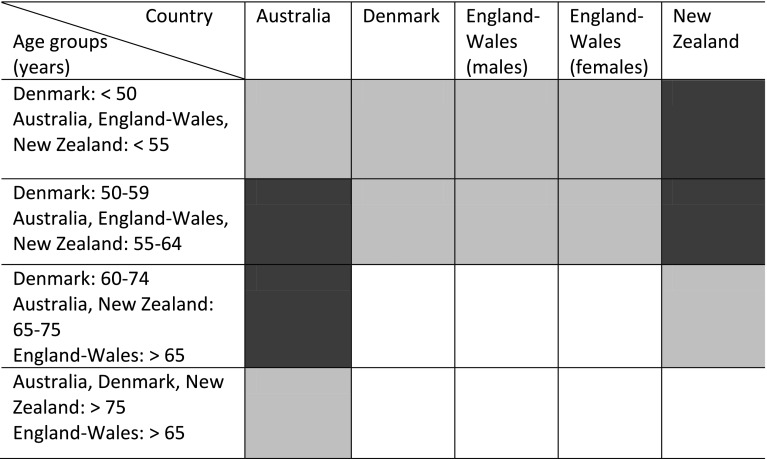
Cemented fixation resulted in statistically significantly lower revision rates (Appendix 1) than uncemented fixation in the oldest age groups of all registries surveyed (> 75 years; except England-Wales, > 65 years) (Fig. 3). Cemented fixation resulted in lower revision rates than hybrid (cemented femur) fixation in the oldest age group, except for Australia where no statistical difference was observed for patients older than 75 years, comparing hybrid and cemented fixation (hazard ratio, 1.07; 95% CI, 0.90–1.26) (Fig. 4). Considering risk profiles of hybrid (cemented femur) versus uncemented fixation, the pattern is less clear and only the Australian and New Zealand registries reported statistically significantly reduced revision risks (Appendix 1) when fixation was hybrid (cemented femur) compared with uncemented fixation for the oldest age group (Fig. 5).
Appendix 1.
Specific age-stratified revision risks for comparison of cemented, uncemented, and hybrid (cemented femur) fixation
| Australia: Hazard ratio (95 % CI) | |||
|---|---|---|---|
| Patient age (years) | Uncemented versus cemented | Cemented versus hybrid | Uncemented versus hybrid |
| < 55 | 1.01 (0.69, 1.47) | 1.12 (0.74, 1.70) | 1.13 (0.90, 1.41) |
| Cemented versus uncemented | Cemented versus hybrid | Uncemented versus hybrid | |
|---|---|---|---|
| 55–64 | 1.48 (1.18, 1.85) | 1.45 (1.15, 1.81) | 0.81 (0.63, 1.03) |
| Uncemented versus cemented | Cemented versus hybrid | Uncemented versus hybrid | |
|---|---|---|---|
| 65–74 | 0.80 (0.68, 0.94) | 1.29 (1.10, 1.51) | 1.03 (0.91, 1.16) |
| Uncemented versus cemented | Hybrid versus cemented | Uncemented versus hybrid | |
|---|---|---|---|
| > 75 | 1.40 (1.14, 1.72) | 1.07 (0.90, 1.26) | 1.43 (1.24, 1.64) |
| Denmark: Hazard ratio (95 % CI) | |||
|---|---|---|---|
| Uncemented versus cemented | Hybrid versus cemented | Hybrid versus uncemented | |
| < 50 | 0.82 (0.62–1.08) | 1.23 (0.91–1.65) | 1.50 (1.23–1.84) |
| 50–59 | 0.69 (0.59–0.81) | 0.97 (0.82–1.16) | 1.41 (1.21–1.64) |
| 60–74 | 1.14 (1.04–1.25) | 1.29 (1.18–1.41) | 1.13 (1.03–1.25) |
| > 75 | 1.69 (1.43–2.01) | 1.43 (1.25–1.63) | 0.84 (0.70–1.01) |
| England-Wales, Males: Hazard ratio (95 % CI) | |||
|---|---|---|---|
| Uncemented versus cemented | Hybrid versus cemented | ||
| < 55 | 1.10 (0.77 to 1.57) | 0.68 (0.42 to 1.09) | |
| 56–64 | 1.56 (1.22 to 2.01) | 1.09 (0.78 to 1.52) | |
| > 65 | 1.73 (1.48 to 2.02) | 1.48 (1.22 to 1.80) | |
| England-Wales, Females: Hazard ratio (95 % CI) | |||
|---|---|---|---|
| Uncemented versus cemented | Hybrid versus cemented | ||
| < 55 | 1.22 (0.89 to 1.71) | 0.97 (0.64 to 1.48) | |
| 56–64 | 1.54 (1.24 to 1.91) | 1.06 (0.79 to 1.43) | |
| > 65 | 2.21 (1.94 to 2.53) | 1.43 (1.20 to 2.53) | |
| New Zealand: Revision rate per 100 component years (95 % CI) | |||
|---|---|---|---|
| Cemented | Uncemented | Hybrid | |
| < 55 | 1.59 (1.23, 2.02) | 0.77 (0.68, 0.87) | 0.95 (0.81, 1.12) |
| 55–64 | 0.95 (0.80, 1.13) | 0.81 (0.72, 0.90) | 0.62 (0.54, 0.71) |
| 65–74 | 0.56 (0.50, 0.63) | 0.86 (0.73, 1.00) | 0.62 (0.55, 0.69) |
| > 75 | 0.39 (0.33, 0.44) | 0.95 (0.7, 1.25) | 0.59 (0.50, 0.69) |
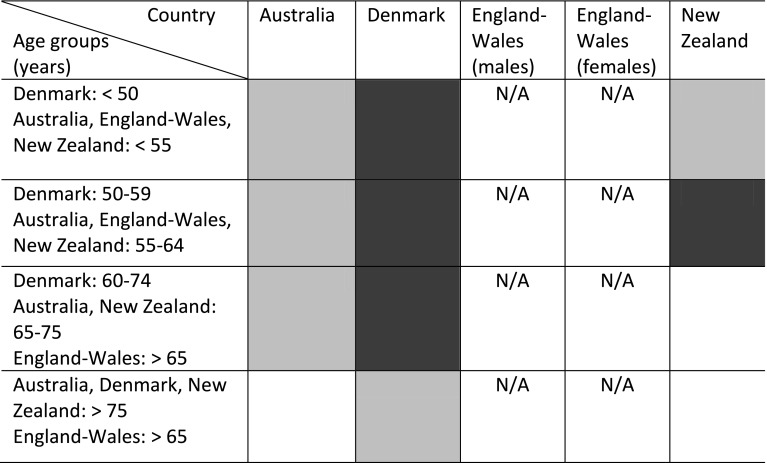
Fig. 3.
The risk profiles for cemented versus uncemented fixation according to age groups were extracted and are color coded as follows: white = statistically significant (p < 0.05) lower risk of revision after cemented versus uncemented fixation; gray = no statistically significant (p > 0.05) difference in risk of revision after cemented versus uncemented fixation; black = statistically significant (p < 0.05) greater risk of revision after cemented versus uncemented fixation. See Appendix 1 for exact risk estimates.
Fig. 4.
The risk profiles for cemented versus hybrid fixation (cemented femur) according to age groups are color coded as follows: white = statistically significant (p < 0.05) lower risk of revision after cemented versus hybrid fixation; gray = no statistically significant (p > 0.05) difference in risk of revision after cemented versus hybrid fixation; black = statistically significant (p < 0.05) higher risk of revision after cemented versus hybrid fixation. See Appendix 1 for exact risk estimates.
Fig. 5.
Risk profiles for hybrid (cemented femur) versus uncemented fixation according to age groups are color coded as follows: white = statistically significant (p < 0.05) lower risk of revision after hybrid (cemented femur) versus uncemented fixation; gray = no statistically significant (p > 0.05) difference in risk of revision after hybrid versus uncemented fixation; black = statistically significant (p < 0.05) higher risk of revision after hybrid versus uncemented fixation. N/A = not available. See Appendix 1 for exact risk estimates.
Discussion
The majority of THAs in the United States (86%) are performed without cement [13], and in every registry we surveyed, we found that the rates of uncemented fixation are increasing. This may increase the revision burden if uncemented fixation is associated with a higher risk of revision than other approaches. Countries with hip arthroplasty registries have valid and population-based numbers for the use of different fixation types and the associated risk of revision [19, 20]. By analyzing the annual reports of hip arthroplasty registries, we assessed the current frequencies of uncemented fixation, the trends in use of uncemented fixation during the past half decade, and age-stratified risks of revision using cemented, uncemented, and hybrid fixation.
This study had several limitations. First, this study is based solely on assessment of publicly available annual reports from included hip arthroplasty registries. This is limiting as raw data from the registries cannot be assessed and thus supplemental clarifying analysis, such as adjustment for confounders, was not performed. However, the publicly available reports used to answer our research questions are the sources of evidence that are readily available to the orthopaedic community just like journal papers identified on a search engine. Second, registries have different strategies when presenting data which is an obstacle to uniform interpretation of data on revision risk in this study: hazard ratios and revision rate per 100 component years are given and for hazard ratios the index mode of fixation for comparisons differs between and within registries. In addition, age groups are defined differently among registries, and the same analyses are not presented by all registries resulting in apparent lack of data in our study. This is confusing, but even so, the analysis and numbers are reliable, and for convenience of interpretation we attempted uniform presentation of data in the figures with colored box formats. A joint analysis of all raw data from the included registries, aggregating data from more than one million procedures, is a major task not yet performed. However, in an attempt to join efforts, the Nordic Arthroplasty Register Association (NARA) was established in 2007, and we hope this kind of cooperation will lead to more data uniformity and stronger statements using register data [12]. Third, some limitations of register data in general should be acknowledged: the large number of patients aggregated and included in analysis of register data results in high statistical power, but even after common statistical adjustments residual confounding is inherent to register data since there are limits for what adjustments can be made. Registries are constructed to use revision THA as the end point of the analysis. Although some registries collect and report data on patient-reported outcome measures, the registries generally are less informative regarding how patients are doing and merely reflect technical aspects of surgery and their importance to the revision end point. By inquiry to registries, one gets estimates of revision risk for the entire population of THAs performed in the country. Most registries have high completeness and provide reliable data. Some may argue that overall registry risk estimates are not a valid measure of how good surgical outcome can really be referring to excellent long-term results in expert single-center studies [3, 4, 7, 9]. However, if nationwide quality of THA is of concern, assessment using registry-based data will provide the best estimates of what to expect from revision risk profiles [1, 5, 8, 18, 22, 23].
Why is the variation in current use of uncemented fixation observed by the registries so great? In some countries the registries have been advisors to surgeons in the appropriate choice of fixation, using feedback from the registries concerning risk of revision. In Sweden this has led to a conservative approach with the lowest current use of uncemented fixation and the lowest increase in its use during the reviewed 5-year period [21]. This strategy has led to consistent reports of overall good THA survivorship by the Swedish registry. However, even the presence of a long-standing registry providing data to surgeons at least annually does not necessarily lead to reluctance to use uncemented fixation. This is evidenced by the current use of uncemented fixation observed by the registries in Denmark and England-Wales. Probably multiple factors determine the current large variation in uncemented use in THAs, and even neighboring countries do not necessarily have comparable percentage use of uncemented fixation. This would seem to identify individual surgical cultures in the countries.
What can explain the increasing use of uncemented fixation that is observed by all registries? Historically, the use of cement has been discredited by speculations about cement disease, describing loosening of cemented implants as a unique mode of failure attributable to the material properties of the cement [14]. Furthermore, marketing and rapid developments of good uncemented solutions have been great contributors to push toward an increase in the use of uncemented fixation. This may be particularly true for the United States and Canada with more than eight of 10 primary THAs being uncemented; however, although total use of uncemented fixation is less than in North America, Denmark and England-Wales have experienced dramatic increases in the use of uncemented fixation during the past half decade [8, 18]. Expert single-center experiences reporting good long-term outcomes could lead to increased use of a particular mode of fixation, but such studies do not support favoring just one technique and excellent implant survivorship has been reported for cemented and uncemented THAs [3, 4, 7, 9]. It seems that the increasing use of uncemented fixation worldwide is not backed by evidence that can be generalized to predict the outcome of an entire nation of surgeons performing THAs. Contrary to this thought, studies of large cohorts of patients have suggested inferiority of uncemented fixation [6, 10, 16], and thus it seems that a continuing increase in the use of uncemented fixation is unwarranted. A drawback of the decreasing use of cemented fixation is that the skills to perform an optimal cemented THA potentially are deteriorating among hip surgeons. Denmark observed the largest absolute increase in uncemented use during the study period, and results from the recently published annual registry report of 2012 showed an increased risk of revision of cemented THAs comparing 2007 to 2011 with 1995 to 1998 (hazard ratio,1.24; 95 % CI, 1.08–1.43) [8]. This could in part reflect deterioration of skills, and as a result the profession has to be reeducated with the potential of initial higher risk of revision for cemented THAs attributable to learning curve issues.
The current study suggests superior outcomes in terms of lower revision risk when cemented fixation is compared with uncemented and hybrid fixation in the older age groups of the THA population. Long-term single-center studies have reported good outcomes for cemented and uncemented THAs [3, 4, 7, 9]. In a meta-analysis, Morshed et al. found superiority of cemented fixation over uncemented fixation not just in older age groups [17]. They also found the performance of uncemented implants improved with time. This latter finding also should be acknowledged in relation to registry findings in which improvements in designs and materials, potentially offering improved long-term survivorship, will take some time to break through in reported data of fixation technique. However, the registries do follow specific implant designs and materials to observe their performance individually. Hailer et al., in a register-based study specifically addressing the issue of cemented versus uncemented performance, found lower revision-free 10-year survival for uncemented THAs than for cemented THAs [10]. They identified poorer performance of uncemented cups and increased risk of revision resulting from periprosthetic fractures in uncemented stems to be the main reasons for this. However, they acknowledged that problems related to uncemented cups seemed to be solved by introduction of new developments. Similarly, not all cemented designs have done well, and in another registry-based study, Hallan et al. recommended abandoning a double-tapered cemented titanium stem because survivorship was clearly deteriorating [11]. A meta-analysis on register-based studies of revision risk after primary THA identified that uncemented implants may have a higher 10-year revision rate regardless of age [6]. In a recent register-based cohort study reporting the outcome of 275,000 THAs comparing adjusted mortality and revision rates of cemented compared with uncemented THAs, a statistically significant lower risk of revision was found for cemented THAs [16]. However, a statistically significant lower mortality rate was observed in uncemented THAs compared with cemented THAs. McMinn et al. [16] directed attention toward the possibility of residual confounding, even in adjusted analysis of large cohorts and that mortality risks should be included in the discussion of what mode of fixation in THA is superior. Overall, there seems to be evidence that cemented implants are associated with lower revision risk than uncemented implants, at least in the older age groups.
Increasing use of uncemented fixation in THAs is a worldwide phenomenon. This trend is in conflict with data from registries representing nationwide THA outcomes, which suggest that use of cemented fixation in patients older than 75 years provides the lowest risk of revision. In countries with high use of uncemented fixation, and in countries with dramatic increases in uncemented use, this should warrant close monitoring of population-based outcomes to act on deteriorating long-term outcome.
Appendix
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
This work was performed at the Harris Orthopedic Laboratory, Department of Orthopedics, Massachusetts General Hospital, Boston, MA, USA.
References
- 1.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide, AOA 2011. Available at: https://aoanjrr.dmac.adelaide.edu.au/en/annual-reports-2011. Accessed March 12, 2013.
- 2.Berry DJ, Bozic KJ. Current practice patterns in primary hip and knee arthroplasty among members of the American Association of Hip and Knee Surgeons. J Arthroplasty. 2010;25(suppl):2–4. doi: 10.1016/j.arth.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Harmsen WS, Cabanela ME, Morrey BF. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am. 2002;84:171–177. doi: 10.2106/00004623-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Callaghan JJ, Bracha P, Liu SS, Piyaworakhun S, Goetz DD, Johnston RC. Survivorship of a Charnley total hip arthroplasty: a concise follow-up, at a minimum of thirty-five years, of previous reports. J Bone Joint Surg Am. 2009;91:2617–2621. doi: 10.2106/JBJS.H.01201. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information. CIHI Annual Report. Available at: https://securecihica/estore/productSerieshtm?pc=PCC241. Accessed March 13, 2013.
- 6.Corbett KL, Losina E, Nti AA, Prokopetz JJ, Katz JN. Population-based rates of revision of primary total hip arthroplasty: a systematic review. PloS One. 2010;5:e13520. doi: 10.1371/journal.pone.0013520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. Comparison of total hip arthroplasty performed with and without cement: a randomized trial. A concise follow-up, at twenty years, of previous reports. J Bone Joint Surg Am. 2011;93:1335–1338. doi: 10.2106/JBJS.J.00448. [DOI] [PubMed] [Google Scholar]
- 8.Danish Hip Arthroplasty Register. Available at: http://wwwdhr.dk/annual_report.htm. Accessed March 12, 2013.
- 9.Della Valle CJ, Mesko NW, Quigley L, Rosenberg AG, Jacobs JJ, Galante JO. Primary total hip arthroplasty with a porous-coated acetabular component: a concise follow-up, at a minimum of twenty years, of previous reports. J Bone Joint Surg Am. 2009;91:1130–1135. doi: 10.2106/JBJS.H.00168. [DOI] [PubMed] [Google Scholar]
- 10.Hailer NP, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop. 2010;81:34–41. doi: 10.3109/17453671003685400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hallan G, Espehaug B, Furnes O, Wangen H, Hol PJ, Ellison P, Havelin LI. Is there still a place for the cemented titanium femoral stem? 10,108 cases from the Norwegian Arthroplasty Register. Acta Orthop. 2012;83:1–6. doi: 10.3109/17453674.2011.645194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Havelin LI, Robertsson O, Fenstad AM, Overgaard S, Garellick G, Furnes O. A Scandinavian experience of register collaboration: the Nordic Arthroplasty Register Association (NARA) J Bone Joint Surg Am. 2011;93(suppl 3):13–19. doi: 10.2106/JBJS.K.00951. [DOI] [PubMed] [Google Scholar]
- 13.Huo MH, Dumont GD, Knight JR, Mont MA. What’s new in total hip arthroplasty. J Bone Joint Surg Am. 2011;93:1944–1950. doi: 10.2106/JBJS.K.00656. [DOI] [PubMed] [Google Scholar]
- 14.Jones LC, Hungerford DS. Cement disease. Clin Orthop Relat Res. 1987;225:192–206. [PubMed] [Google Scholar]
- 15.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 16.McMinn DJ, Snell KI, Daniel J, Treacy RB, Pynsent PB, Riley RD. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ. 2012;344:e3319. doi: 10.1136/bmj.e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morshed S, Bozic KJ, Ries MD, Malchau H, Colford JM., Jr Comparison of cemented and uncemented fixation in total hip replacement: a meta-analysis. Acta Orthop. 2007;78:315–326. doi: 10.1080/17453670710013861. [DOI] [PubMed] [Google Scholar]
- 18.NJR National Joint Registry. Archived annual reports. Available at: http://www.njrcentre.org.uk/njrcentre/Reports,PublicationsandMinutes/Annualreports/Archivedannualreports/tabid/87/Default.aspx. Accessed March 13, 2013.
- 19.Pedersen A, Johnsen S, Overgaard S, Soballe K, Sorensen HT, Lucht U. Registration in the Danish Hip Arthroplasty Registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand. 2004;75:434–441. doi: 10.1080/00016470410001213-1. [DOI] [PubMed] [Google Scholar]
- 20.Soderman P. On the validity of the results from the Swedish National Total Hip Arthroplasty register. Acta Orthop Scand Suppl. 2000;71:1–33. doi: 10.1080/000164700753740781. [DOI] [PubMed] [Google Scholar]
- 21.Swedish Hip Arthroplasty Register. Publications. Available at: http://www.shpr.se/en/Publications.aspx. Accessed March 13, 2013.
- 22.The New Zealand Joint Registry. Thirteen Year Report: January 1999 to December 2011. Available at: http://www.cdhb.govt.nz/njr/reports/A2D65CA3.pdf. Accessed March 13, 2013.
- 23.The Norwegian Arthroplasty Register. Publications. Available at: http://nrlweb.ihelse.net/eng/default.htm#Publications. Accessed March 13, 2013.