Abstract
Background
Modularity of the femoral head-neck junction provides increased intraoperative flexibility to the surgeon. Complications of this modularity include damage to the trunnion, with subsequent bone and/or soft tissue loss from adverse reactions to metal debris.
Case Description
We describe two cases of severe metal-induced osteolysis and soft tissue damage requiring revision 10 and 13 years following implantation of a unipolar endoprosthesis. Damage to the trunnion resulted in severe acetabular and trochanteric osteolysis and soft tissue loss requiring complex revision surgery.
Literature Review
Several reports have shown the trunnion, the head-neck interface, and the neck-stem couple as the causes of this early failure secondary to metal ion release from mechanical fretting corrosion or from crevice corrosion at these modular interfaces. These reports have been in association with a total hip prosthesis rather than a unipolar endoprosthesis. Revision of a unipolar endoprosthesis is most commonly attributable to stem loosening or acetabular erosion from the large femoral head articulating on the host acetabular cartilage and not owing to failure of the trunnion.
Purposes and Clinical Relevance
Trunnion damage resulting in a severe reaction to metal debris with acetabular osteolysis, erosion of the greater trochanter, and loss of the abductor mechanism can occur years after implantation of a cementless unipolar endoprosthesis. This raises questions regarding long-term safety of the modular interface of a contemporary cementless stem and a large-diameter unipolar head. We recommend long-term followup of patients with a unipolar endoprosthesis as early recognition and treatment are required to avoid a potentially complex revision.
Introduction
Modularity of the femoral head-neck junction allows the surgeon the flexibility to alter head size, leg length, and femoral offset during hip arthroplasty. Complications of this modular junction include fretting [6–8, 12, 16, 23], crevice corrosion [6–8, 12, 13, 16, 23], and fracture of the trunnion [2, 4, 13, 15, 19, 28]. The most common reason for revision of a unipolar endoprosthesis is stem loosening [1, 10, 27] or acetabular erosion from the large femoral head articulating on the host acetabular cartilage and not from complications of the trunnion [10, 17, 24, 26, 27]. Recent reports of large diameter heads in metal-on-metal THA have shown increased rates of trunnion corrosion [3, 11, 20], increased serum metal ion levels [3, 11, 20, 21], and soft tissue damage from adverse reactions to metal debris (ARMD) [3, 20, 21]. In these implants a trunnion would not be the only potential source of debris. We present two cases of severe metal-induced osteolysis and soft tissue damage requiring revision, 10 and 13 years after implantation of a unipolar endoprosthesis to treat a subcapital hip fracture in which the only source of debris could have been the trunnion.
Case Reports
A 67-year-old man with a BMI of 24.7 kg/m2 presented with acute onset of pain, inability to bear weight, and shortening of his left leg after getting up from a seated position. Before presentation he had no symptoms. Ten years previously the patient had undergone an uncomplicated implantation of a cementless endoprosthesis for a subcapital hip fracture nonunion. The endoprosthesis was a VerSys Fiber Metal Midcoat collared stem (Zimmer, Warsaw, IN, USA) made of titanium alloy (Ti-6Al-4V) with a 12/14 taper modular head-neck junction having no intervening taper adapter and a 52 mm + 10.5 mm Co-Cr-Mo unipolar femoral head (Fig. 1A).
Fig. 1A–E.
(A) An AP radiograph of the pelvis obtained 1 year after unipolar endoprosthesis implantation shows the normal position of the large femoral head in the acetabulum and the normal anatomy of the greater trochanter. (B) An AP radiograph shows the femoral head in the superiorly located acetabulum with the femoral stem dissociated from the head. The trunnion is intact but grossly deformed with notching of its inferior aspect and bulging of its superior aspect. (C) An intraoperative photograph before removal of the stem shows abundant black stained tissues throughout the hip. The proximal femur has erosions filled with blackened tissue and the abductors are absent from the greater trochanter. In the background, there is extensive black stained tissue involving the capsule and acetabulum. (D) A photograph of the explanted femoral stem shows the trunnion is grossly distorted with notching of the proximal inferior neck (arrow) and deformation of the superior aspect of the taper. (E) A representative histologic section of the hip capsule shows abundant large and small metal debris particles (black particles) (Stain, Hematoxylin and eosin; original magnification, ×20).
The radiographs showed the prosthetic femoral head was located in the acetabulum, but the stem had dissociated from the head and was dislocated superiorly and posteriorly (Fig. 1B). There was marked erosion of the acetabulum with superior migration of the femoral head and severe osteolysis of the greater trochanter. The trunnion was grossly deformed with notching of its inferior aspect and bulging of its superior aspect. No preoperative metal ion serum levels were obtained.
At the time of revision, the external rotators, capsule, and greater trochanter were stained black, the greater trochanter was eroded with all but the most anterior fibers of the abductors detached from their insertion, and the joint was filled with a large quantity of black-stained fluid. The acetabulum was eroded superiorly and was black, whereas the proximal femur had black-stained soft tissue that had eroded the proximal 2 cm of the femur (Fig. 1C). The stem’s trunnion was severely damaged with extensive asymmetric metal loss and deformity (Fig. 1C–D). There was no gross burnishing or damage to the articulating surface of the prosthetic femoral head or explanted femoral stem. The pathologic analysis of the black stained soft tissues was consistent with ARMD (Fig. 1E). The ingrown stem was removed with an extended trochanteric osteotomy and a cementless revision was done. A constrained liner (Trilogy® Longevity; Zimmer) was needed owing to severe destruction of the abductors and their detachment from the eroded greater trochanter.
A 66-year-old man with a BMI of 21.5 kg/m2 presented for routine followup 13 years after implantation of a right endoprosthesis to treat avascular necrosis that developed after hip pinning for a subcapital hip fracture. He had no pain but reported weakness in his leg and an increasing limp during the last year. On examination he had a positive Trendelenburg sign. The endoprosthesis was a Multilock Ti-6Al-4 V femoral stem (Zimmer) with an 11/13 taper modular head-neck junction, no intervening taper, and a 50 mm + 0 Co-Cr-Mo unipolar femoral head (Fig. 2A).
Fig. 2A–C.
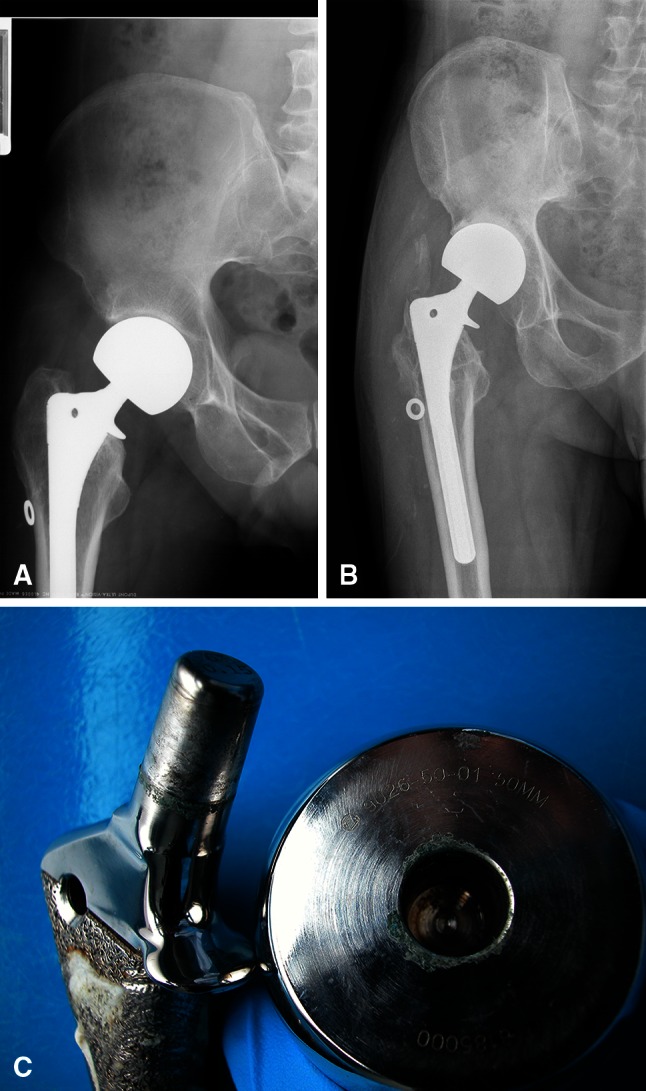
(A) An AP radiograph of the right hip obtained 1 year after unipolar endoprosthesis implantation shows the endoprosthetic head in the anatomic location of the acetabulum and the normal anatomy of the greater trochanter. (B) A preoperative AP radiograph of the right hip shows erosion of the acetabulum with superior migration of the prosthesis. There is marked osteolysis of the greater trochanter. (C) The explanted femoral stem and large-diameter head had extensive black markings and deposits at the trunnion and modular head interface and along the stem trunnion and the corresponding taper in the femoral head.
Radiographs revealed osteolysis of the greater trochanter and superior migration of the femoral head with no evidence of metal debris, similar to that seen in the previous case (Fig. 2B). No preoperative metal ion serum levels were obtained.
At the revision surgery, the abductors were thinned and attenuated, detached from the underlying greater trochanter, but in continuity with the vastus lateralis thereby creating a muscular sleeve adjacent to the trochanter. The acetabulum had black staining throughout with substantial osteolysis and erosion, similar to that seen in the first case. Extensive black markings and deposits were visible at the trunnion and modular head interface and along the trunnion and the corresponding taper in the femoral head (Fig. 2C). There was no gross burnishing or damage to the articulating side of the prosthetic femoral head or the explanted femoral stem. The ingrown femoral stem was removed with an extended trochanteric osteotomy and a cementless revision was performed. The muscular sleeve of the abductors and vastus lateralis were reattached through drill holes to the underlying eroded greater trochanter using FiberWire (Arthrex, Naples, FL, USA) and the hip was constrained using a Trilogy® Longevity constrained liner (Zimmer). Intraoperative cultures were negative for infection and the pathologic analysis of the granulomatous tissues was consistent with ARMD.
Discussion
Failure of a unipolar endoprosthesis is most commonly the result of stem loosening or acetabular erosion from the large femoral head articulating on the host acetabular cartilage [1, 9, 17, 24, 26, 27]. Our two cases illustrate a new and potentially destructive long-term complication of the articulation between a large-diameter unipolar femoral head and a contemporary femoral stem. In both cases, the Morse taper was severely damaged with extensive black markings and deposits, indicative of corrosion. In the first case, the wear of the trunnion was so severe that the loss of the metal substrate was clearly visible. This loss of substance allowed the head to disengage from the stem. Severe metal debris and granulomas were present throughout both hips, resulting in acetabular bone loss and erosion of the greater trochanter.
This study had several limitations, the most notable being that metal ion levels and microscopic trunnion analysis were not available for these two cases. Regardless, the severe black staining of the bone and soft tissues clearly implicates the blackened and/or eroded neck trunnion as the etiology of the tissue destruction. Second, because this is a case report and not a review of all the unipolar endoprosthesis implantations performed at our institution, we do not know the incidence of this problem. We do not know if any other implants have failed in this manner and if patients have been treated elsewhere or have pending implant failures.
Based on the literature, we can only speculate regarding why there was such extensive wear of the trunnion and subsequent tissue destruction in these unipolar endoprostheses. In vitro and finite element studies have shown that fretting would occur from micromotion at the interface [14, 15, 22, 25]. Retrieval studies have documented corrosion of the head-neck interface secondary to fretting [5, 16, 18, 23]. Such corrosion can be potentiated by crevice corrosion, or that which occurs in spaces to which access of the working fluid from the environment is limited [5–8, 12, 14, 16, 18, 23]. The combination of these processes potentially can cause a substantial release of metal ions and metal debris from these modular interfaces. The release of these ions and debris can result in severe biologic reactions such as the osteolysis and abductor erosion [9]. Increased offset reportedly causes higher degrees of corrosion. In a retrieval study, Brown et al. [5] reported that +5 and +10 mm neck extensions have higher degrees of corrosion than necks without an extension. They noted the highest corrosion occurred in the distal inferior (closer to stem neck interface) and proximal superior aspects of the femoral neck. In addition, Gilbert et al. [14] conducted an in vitro study changing head offset and concluded that when there was no offset, the micromotion behaved like a piston, whereas when the offset was 6 mm, there likely was pivoting, rotating, or rocking-like movement around the neck. These studies could explain some of the deformation seen on the trunnion of our first case that had a high-offset head. The back and forth rocking over multiple cycles and loads would likely result in flattening of the superior tip of the trunnion and notching wear on the inferodistal aspect. Increasing the lever arm, or head size and offset, theoretically would increase the torque generated. This increased torque could increase the rate of corrosion and deformation and lead to catastrophic failure faster than in smaller head sizes by increasing the rate and distance of the micromotion.
Our patients had a severe biologic reaction to metal debris with acetabular osteolysis, erosion of the greater trochanter, and loss of the abductor mechanism in active patients 10 and 13 years after implantation of a cementless unipolar endoprosthesis. Neither of these patients had an associated adapter nor skirted neck, which have been proposed as causes of increased corrosion and elevated metal ion levels [4, 11, 19]. This raises questions regarding long-term safety of the modular interface of a contemporary cementless stem and a large-diameter unipolar head. With damage of the trunnion and soft tissue damage from adverse reactions to metal debris in mind, we recommend long-term followup of patients with an endoprosthesis. Although some surgeons provide long-term followup for patients with THAs, they often are not as arduous in following patients with endoprostheses and our two patients emphasize the importance of doing so. Although postoperative erosion of the acetabulum is most commonly the result of wear of the cartilage and bone by the large metal unipolar head [10, 17, 24, 26, 27], special attention should be directed to detect superior migration of the implant and erosion of the greater trochanter. These findings may herald the need for a complex revision with removal of a well-fixed stem and a constrained liner or dual-mobility cup to deal with the abductor erosion, rather than just placement of an acetabular cup and a femoral head exchange. Early recognition and treatment are required to avoid a potentially complex revision because of bone and soft tissue destruction.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Andersson G, Nielsen JM. Results after arthroplasty of the hip with Moore’s prosthesis. Acta Orthop Scand. 1972;43:397–410. doi: 10.3109/17453677208998960. [DOI] [PubMed] [Google Scholar]
- 2.Atwood SA, Patten EW, Bozic KJ, Pruitt LA, Ries MD. Corrosion-induced fracture of a double-modular hip prosthesis: a case report. J Bone Joint Surg Am. 2010;92:1522–1525. doi: 10.2106/JBJS.I.00980. [DOI] [PubMed] [Google Scholar]
- 3.Bolland BJ, Culliford DJ, Langton DJ, Millington JP, Arden NK, Latham JM. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg Br. 2011;93:608–615. doi: 10.1302/0301-620X.93B5.26309. [DOI] [PubMed] [Google Scholar]
- 4.Botti TP, Gent J, Martell JM, Manning DW. Trunion fracture of a fully porous-coated femoral stem: case report. J Arthroplasty. 2005;20:943–945. doi: 10.1016/j.arth.2005.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Brown SA, Flemming CA, Kawalec JS, Placko HE, Vassaux C, Merritt K, Payer JH, Kraay MJ. Fretting corrosion accelerates crevice corrosion of modular hip tapers. J Appl Biomater. 1995;6:19–26. doi: 10.1002/jab.770060104. [DOI] [PubMed] [Google Scholar]
- 6.Collier JP, Surprenant VA, Jensen RE, Mayor MB. Corrosion at the interface of cobalt-alloy heads on titanium-alloy stems. Clin Orthop Relat Res. 1991;271:305–312. [PubMed] [Google Scholar]
- 7.Collier JP, Surprenant VA, Jensen RE, Mayor MB, Surprenant HP. Corrosion between the components of modular femoral hip prostheses. J Bone Joint Surg Br. 1992;74:511–517. doi: 10.1302/0301-620X.74B4.1624507. [DOI] [PubMed] [Google Scholar]
- 8.Cook SD, Barrack RL, Clemow AJ. Corrosion and wear at the modular interface of uncemented femoral stems. J Bone Joint Surg Br. 1994;76:68–72. [PubMed] [Google Scholar]
- 9.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. doi: 10.2106/JBJS.K.01352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cossey AJ, Goodwin MI. Failure of Austin Moore hemiarthroplasty: total hip replacement as a treatment strategy. Injury. 2002;33:19–21. doi: 10.1016/S0020-1383(01)00096-1. [DOI] [PubMed] [Google Scholar]
- 11.Garbuz DS, Tanzer M, Greidanus NV, Masri BA, Duncan CP. The John Charnley Award: Metal-on-metal hip resurfacing versus large-diameter head metal-on-metal total hip arthroplasty: a randomized clinical trail. Clin Orthop Relat Res. 2010;468:318–325. doi: 10.1007/s11999-009-1029-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gilbert JL, Buckley CA, Jacobs JJ. In vivo corrosion of modular hip prosthesis components in mixed and similar metal combinations: the effect of crevice, stress, motion, and alloy coupling. J Biomed Mater Res. 1993;27:1533–1544. doi: 10.1002/jbm.820271210. [DOI] [PubMed] [Google Scholar]
- 13.Gilbert JL, Buckley CA, Jacobs JJ, Bertin KC, Zernich MR. Intergranular corrosion-fatigue failure of cobalt-alloy femoral stems: a failure analysis of two impants. J Bone Joint Surg Am. 1994;76:110–115. doi: 10.2106/00004623-199401000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Gilbert JL, Mehta M, Pinder B. Fretting crevice corrosion of stainless steel stem-CoCr femoral head connections: comparisons of materials, initial moistrure, and offset length. J Biomed Mater Res B Appl Biomater. 2009;88:162–173. doi: 10.1002/jbm.b.31164. [DOI] [PubMed] [Google Scholar]
- 15.Goldberg JR, Gilbert JL. In vitro corrosion testing of modular hip tapers. J Biomed Mater Res B Appl Biomater. 2003;64:78–93. doi: 10.1002/jbm.b.10526. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg JR, Gilbert JL, Jacobs JJ, Bauer TW, Paprosky W, Leurgans S. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002;401:149–161. doi: 10.1097/00003086-200208000-00018. [DOI] [PubMed] [Google Scholar]
- 17.Kaltsas DS, Klugman DJ. Acetabular erosion: a comparison between the Austin Moore and Monk hard top prostheses. Injury. 1986;17:230–236. doi: 10.1016/0020-1383(86)90226-3. [DOI] [PubMed] [Google Scholar]
- 18.Kop AM, Swarts E. Corrosion of a hip stem with a modular neck taper junction: a retrieval study of 16 cases. J Arthroplasty. 2009;24:1019–1023. doi: 10.1016/j.arth.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Lam LO, Stoffel K, Kop A, Swarts E. Catastrophic failure of 4 cobalt-alloy Omnifit hip arthroplasty femoral components. Acta Orthop. 2008;79:18–21. doi: 10.1080/17453670710014707. [DOI] [PubMed] [Google Scholar]
- 20.Langton DJ, Jameson SS, Joyce TJ, Gandhi JN, Sidaginamale R, Mereddy P, Lord J, Nargol AV. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br. 2011;93:1011–1016. doi: 10.1302/0301-620X.93B8.26040. [DOI] [PubMed] [Google Scholar]
- 21.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 22.Lewis G. Geometric element analysis of fretting in a model of a modular femoral component of a hip implant. Biomed Mater Eng. 2004;14:43–51. [PubMed] [Google Scholar]
- 23.Lieberman JR, Rimnac CM, Garvin KL, Klein RW, Salvati EA. An analysis of the head-neck taper interface in retrieved hip prostheses. Clin Orthop Relat Res. 1994;300:162–167. [PubMed] [Google Scholar]
- 24.Phillips TW. Thompson hemiarthroplasty and acetabular erosion. J Bone Joint Surg Am. 1989;71:913–917. [PubMed] [Google Scholar]
- 25.Shareef N, Levine D. Effect of manufacturing tolerances on the micromotion at the Morse taper interface in modular hip implants using the finite element technique. Biomaterials. 1996;17:623–630. doi: 10.1016/0142-9612(96)88713-8. [DOI] [PubMed] [Google Scholar]
- 26.Soreide O, Lillestol J, Aiho A, Hvidsten K. Acetabular protrusion following endoprostetic hip surgery: a multifactorial study. Acta Orthop Scand. 1980;51:943–948. doi: 10.3109/17453678008990899. [DOI] [PubMed] [Google Scholar]
- 27.Warwick D, Hubble M, Sarris I, Strange J. Revision of failed hemiarthroplasty for fractures at the hip. Int Orthop. 1998;22:165–168. doi: 10.1007/s002640050233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wright G, Sporer S, Urban R, Jacobs J. Fracture of a modular femoral neck after total hip arthroplasty: a case report. J Bone Joint Surg Am. 2010;92:1518–1521. doi: 10.2106/JBJS.I.01033. [DOI] [PMC free article] [PubMed] [Google Scholar]



