Abstract
Background
Osteonecrosis of the femoral head secondary to treatment of developmental dysplasia of the hip (DDH) affects acetabular remodeling but the magnitude of this effect is unclear.
Questions/purposes
Using four measures of acetabular development, we (1) determined whether acetabular remodeling differed in hips with and without osteonecrosis; and (2) determined the impact of severity of osteonecrosis contributing to acetabular remodeling.
Methods
We retrospectively reviewed 95 patients (118 hips) treated for DDH by closed or open reduction with or without femoral osteotomy between 1992 and 2006. We evaluated serial radiographs from the time when a stable reduction had been achieved. In 902 radiographs taken over 19 years, we measured the acetabular index and three other indices of hip development. Patients were followed for a mean of 8 years (range, 1–19 years). At last followup, 86 of the 118 hips (73%) had osteonecrosis according to the criteria by Bucholz and Ogden.
Results
The acetabular index improved with time in all hips but the magnitude of improvement was larger in hips without osteonecrosis. The adjusted mean acetabular index at 14 years was 17° for hips with osteonecrosis (95% CI, 15°–18°) and 10° for hips without osteonecrosis (95% CI, 7°–13°). The lateral centering ratio improved after reduction to a normal value less than 0.85 in both groups but the rate of change with 0.06 versus 0.05 was higher in hips with osteonecrosis. The superior centering ratio was worse at all times in hips with osteonecrosis with a mean difference of 0.04. If only radiographic changes of Grades II and greater were considered osteonecrosis, the mean adjusted acetabular index at 14 years was 17.7° (15.6°–19.7°) for hips with osteonecrosis and 12.4° (10.3°–14.4°) for hips without osteonecrosis.
Conclusions
Although radiographic indices improved consistently with time in hips without osteonecrosis, hips with osteonecrosis had abnormal indices of acetabular remodeling throughout followup. Osteonecrosis of the femoral head inhibited acetabular remodeling.
Level of Evidence
Level III, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Osteonecrosis of the proximal femoral epiphysis secondary to treatment of developmental dysplasia of the hip (DDH) is a common complication with incidence rates ranging from 6% to 48% [5, 15]. It is presumed the disrupted blood supply of the proximal femoral epiphysis leads to cellular necrosis, resulting in a growth disturbance of the proximal femur [3, 6, 7, 12]. The degree of osteonecrosis may range from mild epiphyseal hypoplasia to severe deformity [7]. Consequences of osteonecrosis such as loss of femoral head sphericity or subluxation have been associated with premature osteoarthritis [8, 12]. Although osteonecrosis primarily affects the proximal femur, it has been suggested that it can produce a compromise in acetabular remodeling [5, 6, 8, 9], the degree to which this occurs is unclear. Understanding to what degree osteonecrosis worsens acetabular remodeling would allow more accurate anticipation of residual dysplasia and thus be helpful in planning additional treatment.
We therefore (1) determined whether acetabular remodeling differed in hips with and without osteonecrosis using four radiographic indices, and (2) determined the impact of severity of osteonecrosis contributing to acetabular remodeling.
Patients and Methods
Searching hospital admission databases and operating room logs, we identified 130 patients who were admitted for treatment of DDH from 1992 to 2006. Twenty-eight patients were excluded because of a pelvic osteotomy. For seven patients no radiographs were available. These exclusions left 95 patients (118 hips), of whom 79 (83%) were female. The right side was affected in 49 hips (42%). Twenty-three patients (24%) had bilateral dislocations. The mean age (SD) of patients at the index procedure was 19 months (range, 2–56 months). The mean age of patients at the latest radiographic followup was 10 years (range, 4–17 years). The minimum radiographic followup was 1 year (mean, 8 years; range, 1–15 years). No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. Part of this sample was reported in unrelated research [15, 21]. This retrospective cohort study was approved by the institutional review board.
Sample size calculation was based on the primary outcome, acetabular index, with the aim to detect a mean difference of at least 4°, which was considered clinically important [10, 11], and a definition of osteonecrosis that was based on Bucholz-Ogden Grades I to IV [7]. Based on univariate methods, 37 patients were required in each group. Statistical power was set at 80%.
We compared patients with and without osteonecrosis at baseline using chi-square and independent samples t-tests, and potential predictors of acetabular development. For nonnormally distributed data we applied the signed rank test. Patients who remained free of osteonecrosis were younger (p < 0.001) with a mean age of 13 months compared with a mean age of 21 months for patients who had osteonecrosis develop (mean difference, 8 months) (Table 1). Eighteen of 118 hips (15%) had a failed reduction at presentation. Of these, 15 (83%) showed signs of osteonecrosis during the later course (Table 2).
Table 1.
Group differences based on univariate analysis for 95 patients or 118 hips
| Variable | All hips or patients | Hips with osteonecrosis (n = 86) | Hips without osteonecrosis (n = 32) | p value or 95% CI* |
|---|---|---|---|---|
| Age at index surgery† (months) | 18.8 ± 11.2 | 20.7 ± 11.6 | 12.9 ± 7.4 | −7.8 (−11.39, −4.15) |
| Female gender | 79 (83%) | 75 (87%) | 27 (84%) | 1 |
| Bilateral DDH | 23 (24%) | 35 (41%) | 11 (34%) | 0.61 |
| Preoperative acetabular index† | 36.3 ± 7.8 | 36.9 ± 7.7 | 33.2 ± 6.0 | −3.7 (−8.0, 0.60) |
| Missing preoperative radiograph | 36 (31%) | 24 (28%) | 12 (38%) | 0.31 |
| Preceding failed reduction | 18 (15%) | 15 (17%) | 3 (9%) | 0.39 |
| Closed reduction†† | 45 (38%) | 28 (33%) | 17 (5%) | 0.03 |
| Open reduction†† | 12 (10%) | 8 (9%) | 3 (9%) | 0.97 |
| Open reduction and femoral osteotomy†† | 61 (52%) | 49 (57%) | 11 (34%) | 0.04 |
DDH = developmental dysplasia of the hip; †values are given as mean ± the standard deviation; ††Refers to the index procedure; * for continuous variables, the mean difference and 95% CI are given.
Table 2.
Details of 18 patients who presented with preceding procedures
| Patient | Side | Sex | Number of preceding procedures | Nature of preceding procedure | Index procedure | Grade of osteonecrosis* |
|---|---|---|---|---|---|---|
| 1 | R | F | 1 | OR | OR and VDRO | II |
| 2 | L | F | 1 | CR | OR and VDRO | I |
| 3 | R | F | 1 | CR | OR and VDRO | II |
| 4 | L | F | 1 | OR and VDRO | OR and VDRO | I |
| 5 | R | F | 1 | CR | OR | I |
| 6 | L | M | 2 | CR, OR, and VDRO | OR | II |
| 7 | R | F | 1 | OR and VDRO | OR and VDRO | III |
| 8 | R | F | 2 | CR, OR | OR and VDRO | II |
| 9 | L | F | 1 | OR and VDRO | OR and VDRO | IV |
| 10 | R | F | 2 | OR, OR, and VDRO | OR and VDRO | IV |
| 11 | L | F | 1 | OR and VDRO | OR and VDRO | II |
| 12 | L | F | 1 | CR, OR | OR and VDRO | I |
| 13 | L | F | 2 | CR, CR | OR and VDRO | II |
| 14 | R | F | 1 | CR | OR and VDRO | I |
| 15 | L | F | 2 | CR, OR, and VDRO | OR and VDRO | None |
| 16 | L | F | 1 | CR | CR | I |
| 17 | R | M | 1 | CR | OR | None |
| 18 | R | F | 1 | CR | OR | None |
* According to Bucholz and Ogden [7]; OR = open reduction; CR = closed reduction; VDRO = varus derotation osteotomy.
All patients were treated by one of two surgeons (AR, DHJ) at an urban teaching hospital. They underwent either a closed or open reduction of the hip with or without a simultaneous osteotomy of the proximal femur. The same surgical techniques were used for all patients and have been described in detail elsewhere [21].
All data were obtained from medical records and stored radiographs. Typically, AP radiographs of the pelvis were obtained for routine followup at 6 weeks; 3, 6, 12, and 18 months; and yearly thereafter. On average, each patient had a set of 6 ± 2 postoperative radiographs with a total of 902 radiographs available for the sample. One investigator (YG) abstracted all medical records to identify diagnosis, sex, laterality, date of reduction of the hip in our institution, and details of any preceding interventions performed elsewhere. A consistent radiographic protocol was used with all patients being evaluated on the basis of a supine radiograph of the pelvis, centered on the hips, with both feet in 15° internal rotation. With use of a digital imaging system (Fujifilm FCR XG 5000; Fujifilm, Bedford, UK), age-dependent exposure parameters were 60 to 80 kV, 4 to 40 mA/s, and a focus-to-film distance of 150 cm.
One of us (YG) performed all radiographic measurements on all radiographs that were available during the postoperative course. Patient identifiers were removed and radiographs were mixed before grading. Measurements were not taken from rotated radiographs showing obliquity of the iliac wings or lumbar pedicles. Such radiographs were excluded. Radiographs were analyzed electronically (Sienet Sky; Siemens Medical Solutions, Erlangen, Germany). The intrarater reliability (intraclass correlation coefficient) was high with a value of 0.94 (95% CI, 0.86–0.96) for the acetabular index. The mean difference in the measurement of the acetabular index between the two ratings was 0.9° ± 2.8°. One-third of all radiographs were independently evaluated by a second rater (NN) who followed the same principles. The interrater reliability between the two raters was excellent with intraclass correlation coefficients of 0.90 (95% CI, 0.82–0.95) for acetabular index, 0.98 (0.96–0.99) for lateral and 0.80 (0.65–0.89) for superior centering ratio.
Sequential recording of the acetabular index has been used to assess acetabular development in children older than 10 years [2, 10, 21]. Normal values have been established for several age groups [22]. If the triradiate cartilage was fused, we followed the descriptions of Tönnis [23]: a horizontal line was drawn through the lower end point of the sclerotic line of the acetabular roof, and from there a second line was drawn tangent to the superior acetabular rim. These two lines gave an angle that was measured in the same way as the Hilgenreiner acetabular angle in radiographs with an open triradiate cartilage. To ensure these measures were accurate, we also measured the acetabular angle of Sharp [18] in all radiographs. The angle of Sharp has been recommended for hips with a closed triradiate cartilage [18]. This step was performed to improve the quality of data acquisition and to minimize measurement bias. We expected both indices would correlate with one another and that analyses based on each of these two indices would give similar regression coefficients in the comparison of hips with and without osteonecrosis.
We determined hip stability by means of lateral and superior centering ratios [17]. These ratios quantify femoral head concentricity in the horizontal and vertical planes, respectively [18]; therefore, they are a measure of congruity of reduction. Normal values are 0.10 to 0.20 for the superior and 0.60 to 0.85 for the lateral centering ratio [17]. Subluxation of the hip was defined as a superior centering ratio less than 0.10 on the latest postoperative radiograph [18].
Using the most recent radiograph, all radiographs were evaluated according to Bucholz and Ogden [7] for the presence of osteonecrosis. In Grade I, changes are limited to the femoral head with hypoplasia of the epiphysis. In Grade II, the proximal femur develops coxa valga. Grade III is characterized by shortening of the entire femoral neck, trochanteric overgrowth, and deformity of the epiphysis. In Grade IV, coxa vara of the proximal femur is seen. Radiographs were graded for the presence of osteonecrosis in consensus by two raters (AR, JHW) not involved in any of the radiographic measurements and blinded to all other radiographic and clinical information. The most recent radiograph was used to determine the presence of osteonecrosis because a long-enough followup is essential for a firm diagnosis. Of 118 hips, 86 (73%) had radiographic signs of osteonecrosis on the latest followup radiograph and 32 (27%) did not. Grade I osteonecrosis occurred in 29 (34%) hips; Grade II in 33 (38%) hips; Grade III in 19 (22%) hips; and Grade IV in five (6%) hips.
We decided a priori to adjust all models for ‘age at surgery’. Because acetabular development depends on the stability of the reduced hip, we adjusted the primary outcome (acetabular index) for the variable ‘superior centering ratio’, which is an indicator of stability and subluxation. This strategy ensured that the observed effect was not biased by subluxation. We used generalized linear mixed models to evaluate the effect of osteonecrosis on sequential radiographs, with the interaction of osteonecrosis and years since hip reduction as the main interest. Transformation of some covariates improved the fit of the data; fractional polynomials [17] provided the best fit for lateral and superior centering ratios. Based on Akaike’s information criterion [1], we fitted models of Degree 2 with powers 0.5, 0.5 for ‘lateral centering ratio’ and with powers 0, 3 for ‘superior centering ratio’. In post hoc analyses, we generated estimated means at several times for the main outcome and calculated the mean difference based on osteonecrosis. We performed sensitivity analyses for the primary outcome whereby we classified Bucholz-Ogden Grade I as normal. We performed subgroup analyses based on Bucholz-Ogden Grades I to IV. Missing data did not exceed 10%, except for ‘superior centering ratio’, where as much as 20% of the data was missing. We used chained equation multiple imputation [25] to generate five imputed data sets to obtain pooled estimates. The regression coefficients were nearly identical to the original data set and all conclusions remained unchanged. Because mixed-effect models can be used when some data points are missing [26], we report all regression coefficients with no imputations made. All hypothesis testing was two-sided. Analyses were performed with STATA 11 (StataCorp, College Station, TX, USA).
Results
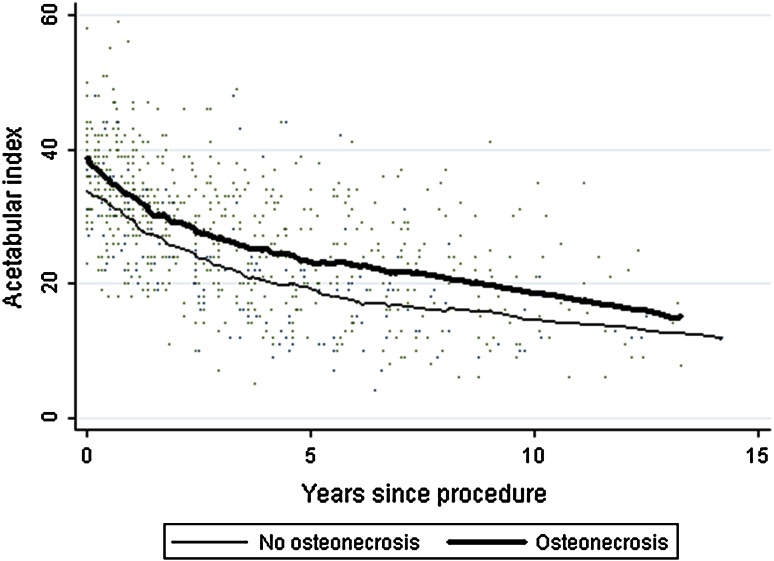
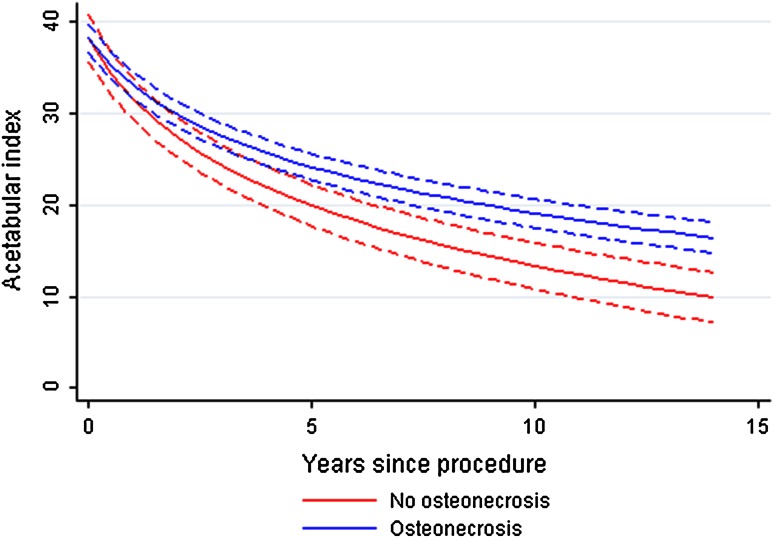
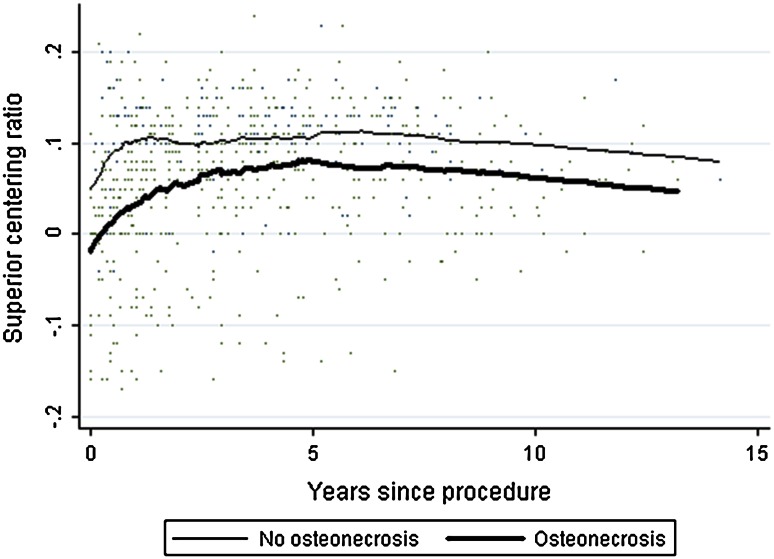
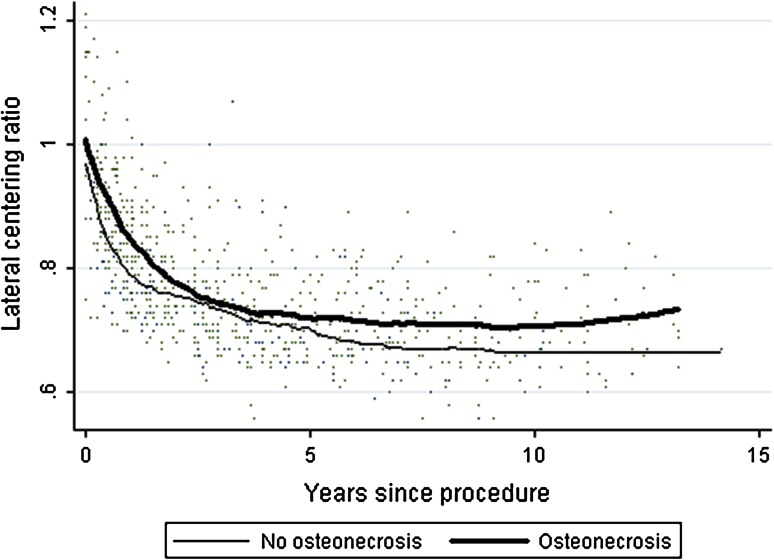
Although the mean acetabular index was similar for hips with (37°) and without (33°) osteonecrosis preoperatively (mean difference, 4°; 95% CI, 1°–8°; p = 0.09), it remained higher (p < 0.001) at all times in hips with osteonecrosis and improved to normal values in those without osteonecrosis (Fig. 1). At 14 years, the mean acetabular index adjusted for age at surgery and for superior centering ratio was 17° (range, 15°–18°) for hips with osteonecrosis and 10° (range, 7°–13°) for hips without osteonecrosis (mean difference, 7°; 95% CI, 1°–12°) (Fig. 2). The superior centering ratio improved after reduction in both groups but was lower (p = 0.009) at all times in hips with osteonecrosis. On average, hips without osteonecrosis reached the 0.1 mark within 2 years of hip reduction, whereas hips with osteonecrosis did not. In both groups, the superior centering ratio declined mildly at 10 years (Fig. 3). The lateral centering ratio improved within one year of reduction to a normal value of less than 0.85 in both groups; however, hips with osteonecrosis had increased values (p < 0.001) during the followup (Fig. 4).
Fig. 1.
The graph shows the effect of osteonecrosis on the development of the acetabular index in the period after hip reduction. The lines represent the group trends for hips with and without osteonecrosis according to individual patient profiles. A smoothing spline was used to estimate the group trends as a function of time. Month 0 represents the first postoperative radiograph. Although the index declined in both groups with time, the decline was smaller in hips with osteonecrosis (p < 0.001).
Fig. 2.
The development of the acetabular index based on modeled data adjusted for the superior centering ratio is shown. The mean values for each postoperative time for hips with and without osteonecrosis are shown. The dotted lines represent the 95% CIs. The adjusted acetabular index at 14 years was 16.5° for hips with osteonecrosis and 9.9° for hips without osteonecrosis.
Fig. 3.
The graph shows the development of the superior centering ratio with time. The lines represent the group trends for hips with and without osteonecrosis according to individual patient profiles. A smoothing spline was used to estimate the group trends as a function of time. Month 0 represents the first postoperative radiograph. The ratio was different between the two groups at all times (p = 0.009). Hips without osteonecrosis reached the normal value of 0.1 within 2 years of hip reduction, whereas hips with osteonecrosis did not.
Fig. 4.
The development of the lateral centering ratio with time is shown. The lines represent the group trends for hips with and without osteonecrosis according to individual patient profiles. A smoothing spline was used to estimate the group trends as a function of time. Month 0 represents the first postoperative radiograph. The ratio declined in both groups equally until the age of 5 years but showed greater (p < 0.001) improvement in hips without osteonecrosis.
If only radiographic changes of Grades II and greater were considered osteonecrosis, the acetabular index remained higher (p = 0.001) at all times in hips with osteonecrosis. Using this definition of osteonecrosis, the mean adjusted acetabular index at 14 years was 17.7° (range, 15.6°–19.7°) for hips with osteonecrosis and 12.4° (range, 10.3°–14.4°) for hips without osteonecrosis (Table 3). Subgroup analyses showed that Grade III (p = 0.0001) and Grade II (p = 0.001) osteonecrosis were associated with the most compromised acetabular indices with time (Table 4).
Table 3.
Results of multivariate analysis for all outcomes
| Variable | Parameter estimate | p value |
|---|---|---|
| Acetabular index | ||
| Intercept (SE) | 45.93 (1.65) | < 0.001 |
| Age at reduction (years) | −1.72 | 0.01 |
| Year (log) | −11.21 | < 0.001 |
| Osteonecrosis (Grades I–IV) | −0.53 | 0.73 |
| Osteonecrosis × year | 2.60 | < 0.001 |
| SCR (per 0.1 unit) | −4.21 | < 0.001 |
| SCR × SCR | −0.52 | 0.003 |
| Sharp angle | ||
| Intercept (SE) | 58.24 (1.36) | < 0.001 |
| Age at reduction | −0.59 | 0.30 |
| Year (log) | −4.96 | < 0.000 |
| Osteonecrosis | −1.57 | 0.21 |
| Osteonecrosis × year | 1.83 | 0.002 |
| SCR (per 0.1 unit) | −1.66 | < 0.001 |
| SCR × SCR | 0.10 | < 0.001 |
| Lateral centering ratio | ||
| Intercept (SE) | 0.97 (0.03) | < 0.001 |
| Age at reduction | −0.004 | 0.66 |
| Year (^0.5) | 0.03 | 0.01 |
| Repeat reduction | 0.04 | 0.01 |
| Osteonecrosis | 0.05 | < 0.001 |
| Osteonecrosis × year | −0.14 | < 0.001 |
| Superior centering ratio | ||
| Intercept (SE) | 0.16 (0.02) | < 0.001 |
| Age at reduction | −0.02 | 0.03 |
| Osteonecrosis | −0.04 | 0.009 |
| Year (log) | 0.02 | < 0.001 |
| Year (^3) | 0.03 | < 0.001 |
| Acetabular index sensitivity* | ||
| Intercept (SE) | 45.11 (1.43) | < 0.001 |
| Age at reduction | −1.63 | 0.02 |
| Year (log) | −10.11 | < 0.001 |
| Osteonecrosis (Grades II–IV) | −0.31 | 0.82 |
| Osteonecrosis × year | 1.84 | 0.55 |
| SCR (per 0.1 unit) | −4.08 | < 0.001 |
| SCR × SCR | −0.50 | 0.004 |
* Sensitivity analysis based on a definition of osteonecrosis that excluded Bucholz-Ogden Grade I; SCR = superior centering ratio.
Table 4.
Effect of severity of osteonecrosis on development of acetabular index with time
| Bucholz-Ogden grades | Number of hips | Regression coefficient | Standard error | p value |
|---|---|---|---|---|
| I | 29 | 1.93 | 0.78 | 0.014 |
| II | 33 | 2.59 | 0.80 | 0.001 |
| III | 19 | 3.35 | 0.82 | 0.000 |
| IV | 5 | 2.31 | 1.84 | 0.211 |
Discussion
It has been suggested that osteonecrosis of the femoral epiphysis secondary to treatment of DDH can affect acetabular remodeling [5, 6, 8, 9], but there are no robust data from longitudinal studies describing the magnitude of this effect. Understanding this effect would allow for more accurate anticipation of residual dysplasia and thus be helpful in planning additional treatment. Using four measures of acetabular development we therefore (1) determined whether acetabular remodeling differed in hips with and without osteonecrosis using four radiographic indices, and (2) determined the affect of severity of osteonecrosis contributing to acetabular remodeling.
There are potential limitations of this study. First, although sequential recordings of the acetabular index are commonly used to assess acetabular development, the variability in its measurement is of concern. Skaggs et al. [20] reported the mean difference of measurements of the acetabular index ranged between 2.3° and 5.1°. Such variability could influence measurement consistency. We performed several steps to ensure consistency of radiographic measurements: (1) we used three other radiographic indices of acetabular development and did not rely on the acetabular index alone; (2) we ensured adequate reliability of the rater; (3) all radiographic measurements were performed according to a set protocol. Some hips had a closed triradiate cartilage; for these cases we used a method described by Tönnis [23] that allowed measuring an angle equivalent to the Hilgenreiner acetabular index. Other studies also have used the acetabular index in children older than 10 years [10, 11, 21]. Additionally, the acetabular angle of Sharp [18] was measured on all radiographs and it confirmed the analysis of the acetabular index: the angle of Sharp remained higher (p = 0.002) in the osteonecrosis group (Table 3). Second, digital imaging software had been introduced at approximately the time of followup, so for some patients, it was necessary to use a mixture of digital images and hard-copy radiographs, which potentially leads to additional problems resulting from inconsistencies in the magnification factors used. However, the number of hard-copy films consistently concerned only the years before 2002, with those of the most recent followup period being measured electronically. Finally, hips were unevenly distributed with only 6% of hips showing Grade IV osteonecrosis. This compromised subgroup analyses in that no robust conclusions could be made for Grade IV osteonecrosis. However, the controversy regarding the clinical relevance of radiographic changes concerns Grade I, of which we observed an adequate number. Fourth, although our observations suggest the remodeling differences are the result of the osteonecrosis, we cannot presume other causal factors played no role in the differences. The most obvious factors are the degree of dysplasia at baseline, the age at reduction, and the concentricity of reduction (subluxation) during followup. We controlled the analyses for these variables. To test the affect of any form of surgical treatment, we adjusted the final models for this factor. However, the direction and magnitude of the regression coefficient remained unchanged and therefore we reported adjusted estimates for age at reduction and superior centering ratio. Fifth, in grading osteonecrosis only the most recent radiograph was used for each patient to ensure a long-enough followup time. We therefore cannot say how many hips had radiographic signs of osteonecrosis before hip reduction and whether this could have influenced acetabulum remodeling. However, we believe that such an effect, if existing, would be negligible and that osteonecrosis cannot be measured reliably with radiographs at this stage.
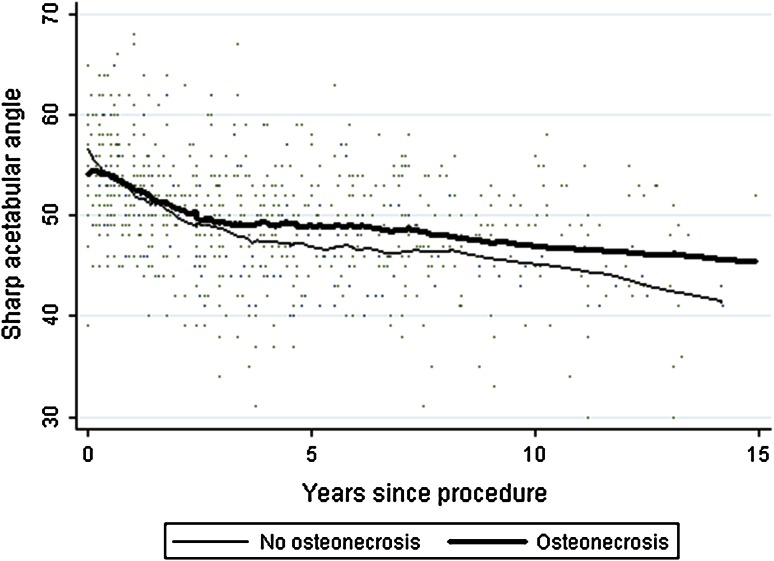
We found an effect of osteonecrosis on acetabular remodeling, confirmed by four radiographic indices, of which all showed the same trends. The magnitude of the effect was moderate. The mean difference in the acetabular index between hips with and without osteonecrosis was 6° at age 10 years with an upper 95% confidence limit of 10° (Table 5). In evaluating interventions for DDH, others regarded a difference of 4° as clinically important [10, 11, 21]. According to Tönnis [22], a normal acetabular index is less than 16° at the age of 7 years. In our study, it was 22° at this age for patients with osteonecrosis compared with 17° for those without osteonecrosis. Hips without osteonecrosis met Tönnis’ criteria of normality, whereas hips with osteonecrosis did not. These estimates were statistically controlled for subluxation and for the acetabular index at baseline. Therefore, the effect seen is the effect of the osteonecrosis on acetabular development during the entire period of followup. The robustness of these results was confirmed by a secondary analysis based on the acetabular angle of Sharp [18]. This angle correlated with the acetabular index and showed the same effects comparing the two groups (Fig. 5). Sibinski et al. [19] noted that residual acetabular dysplasia was more common if DDH was complicated by osteonecrosis. Nakamura et al. [14] reported on 130 hips with DDH. For patients who did not have osteonecrosis develop, 97% had Severin Grade I or II hips at 14 years, with only 44% Grade I or II hips in patients with osteonecrosis. Both of these studies were limited in that they failed to present robust longitudinal data based on multivariate analysis. Bar-On et al. [4] reported better femoral head sphericity and better modified Severin grades if patients with DDH and osteonecrosis received pelvic osteotomies at the age of 5 to 7 years. In their view, such early intervention guarantees better long-term outcomes of DDH complicated by osteonecrosis. Although we did not measure femoral head remodeling and sphericity in the current study, we can partly confirm the findings of Bar-On et al. [4] in that in the current study, acetabular index, Sharp angle, and superior and lateral centering ratios were worse in hips with osteonecrosis. Considering that the mean acetabular index at 14 years was 17° for hips with osteonecrosis (as compared with 10°), the rationale for early pelvic osteotomy seems plausible. However, our study does not provide any confirmation that early osteotomy would improve remodeling; this question ideally should be studied in a randomized trial. The incidence of osteonecrosis in our study was higher than in similar studies reported previously (Table 6). In contrast to other studies, we classified mild changes as Grade I osteonecrosis, which could partly explain the higher incidence. Lateral and superior centering ratios indicate femoral head concentricity in lateral and horizontal planes. In their longitudinal analysis of hips after femoral or pelvic osteotomy, Spence et al. [21] found these ratios changed in the same direction as the acetabular index and that a combination of these indices with the acetabular index is a useful indicator for overall hip development. We found similar ratios: acetabular index, lateral and superior centering ratios all were worse in hips with osteonecrosis throughout followup. For the superior centering ratio, values greater than 0.1 are considered normal [21] but hips with osteonecrosis remained below this threshold throughout followup (Fig. 3).
Table 5.
Predicted values for the acetabular index in the postoperative period
| Year | Osteonecrosis | No osteonecrosis | Difference | |||
|---|---|---|---|---|---|---|
| Mean | 95% CI | Mean | 95% CI | Mean | 95% CI | |
| 0.5 | 35.27 | 33.78–36.76 | 34.38 | 32.02–36.75 | 0.88 | −3.03 to 4.79 |
| 1 | 33.07 | 31.62–34.51 | 31.52 | 29.26–33.78 | 1.54 | −2.05 to 5.14 |
| 2 | 29.86 | 28.45–31.27 | 27.35 | 25.18–29.53 | 2.51 | −0.85 to 5.87 |
| 3 | 27.53 | 26.13–28.94 | 24.32 | 22.15–26.49 | 3.21 | −0.14 to 6.57 |
| 4 | 25.70 | 24.28–27.13 | 21.94 | 19.73–24.14 | 3.77 | 0.33–7.21 |
| 5 | 24.19 | 22.75–25.64 | 19.97 | 17.72–22.22 | 4.22 | 0.64–7.80 |
| 6 | 22.91 | 21.44–24.38 | 18.30 | 15.99–20.61 | 4.61 | 0.87–8.35 |
| 7 | 21.79 | 20.30–23.29 | 16.84 | 14.48–19.21 | 4.95 | 1.03–8.87 |
| 8 | 20.80 | 19.28–22.32 | 13.13 | 13.13–17.98 | 5.25 | 1.14–9.35 |
| 9 | 19.92 | 18.37–21.46 | 14.40 | 11.91–16.89 | 5.51 | 1.23–9.80 |
| 10 | 19.11 | 17.54–20.68 | 13.35 | 10.81–15.90 | 5.76 | 1.28–10.23 |
| 11 | 18.03 | 16.42–19.64 | 11.94 | 9.32–14.57 | 5.98 | 1.32–10.64 |
| 12 | 17.70 | 16.08–19.32 | 11.52 | 8.86–14.17 | 6.18 | 1.34–11.02 |
| 13 | 17.07 | 15.42–18.72 | 10.70 | 7.99–13.40 | 6.37 | 1.36–11.39 |
| 14 | 16.48 | 14.82–18.15 | 9.94 | 7.18–12.69 | 6.55 | 1.36–11.74 |
Fig. 5.
The graph shows the development of the Sharp acetabular angle. The lines represent the group trends for hips with and without osteonecrosis according to individual patient profiles. A smoothing spline was used to estimate the group trends as a function of time. Month 0 represents the first postoperative radiograph. Hips without osteonecrosis showed better values (p = 0.002), whereas the difference becomes most apparent at Year 11.
Table 6.
Comparison of studies
| Study | Number of patients | Number of hips | Followup (years) | Mean age at hip reduction (months) | Hips with osteonecrosis | Preoperative acetabular index (mean ± SD in degrees) | Acetabular index at final followup (mean ± SD in degrees) | Treatment methods |
|---|---|---|---|---|---|---|---|---|
| Albinana et al. [2] | 58 | 72 | 14 | 16 | None included | 40.4 ± 7.6 | 20.8 ± 5.2 | Open reduction |
| Morcuende et al. [13] | 76 | 93 | 11 | 14 | 43%* | 39.0 ± 6.1 | 21.0 ± 13.6 | Open reduction |
| Ucar et al. [24] | 30 | 44 | 20 | 11 | 20% | 44.6 ± 6.6 | 22.6 ± 6.5 | Open reduction |
| Current study | 95 | 118 | 8 | 19 | 73% | 36.3 ± 7.8 | 14.8–18.2† 7.2–12.7‡ |
Open reduction +/− femoral osteotomy |
* Only Bucholz and Ogden Grades II to IV were reported; †95% CI for hips with osteonecrosis; ‡95% CI for hips without osteonecrosis.
In the study by Malvitz and Weinstein [12], Grades II to IV osteonecrosis was associated with compromised acetabular development but not so Grade I. We did not observe this in our study. Sensitivity analysis of the main outcome, acetabular index, using a definition of osteonecrosis that only included Grades II to IV, showed the estimates of effects did not change substantially. A more detailed analysis, although underpowered, showed the strongest effect of osteonecrosis on the development of the acetabular index with time was seen in Grade III followed by Grade II osteonecrosis. The effect of Grade IV osteonecrosis remained uncertain as a result of the limited numbers of such hips in this study. We note the high prevalence of osteonecrosis in our study, which we explain by a meticulous inclusion of all Grade I changes according to Bucholz and Ogden and by the high number of cases of failed treatment before referral.
Acetabular remodeling, as quantified by four radiographic indices, was moderately compromised in hips with osteonecrosis, regardless if Grade I was classified as osteonecrosis or normal. Our patients’ results are generalizable to those of other similar patients with DDH, undergoing closed or open reduction without a pelvic osteotomy. Additional research is needed to determine the importance of our findings in the longer term, especially regarding the need for secondary procedures to improve acetabular cover and the occurrence of premature osteoarthritis.
Acknowledgments
We thank John H. Wedge OC MD FRCS(C) for help in grading radiographs for the presence of osteonecrosis and David H. Jones FRCS for permission to include his former patients in this study.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Institute of Health, University College London, and Great Ormond Street Hospital for Children, London, UK.
References
- 1.Akaike H. A new look at the statistical model identification. IEEE Trans. 1974;19:716–723. [Google Scholar]
- 2.Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip. J Bone Joint Surg Br. 2004;86:876–886. doi: 10.1302/0301-620X.86B6.14441. [DOI] [PubMed] [Google Scholar]
- 3.Atsumi T, Kuroki Y. Role of impairment of blood supply of the femoral head in the pathogenesis of idiopathic osteonecrosis. Clin Orthop Relat Res. 1992;277:22–30. [PubMed] [Google Scholar]
- 4.Bar-On E, Huo MH, DeLuca PA. Early innominate osteotomy as a treatment for avascular necrosis complicating developmental hip dysplasia. J Pediatr Orthop B. 1997;6:138–145. doi: 10.1097/01202412-199704000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Brougham DI, Broughton NS, Cole WG, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70:733–736. doi: 10.1302/0301-620X.70B5.3192570. [DOI] [PubMed] [Google Scholar]
- 6.Brougham DI, Broughton NS, Cole WG, Menelaus MB. Avascular necrosis following closed reduction of congenital dislocation of the hip: review of influencing factors and long-term follow-up. J Bone Joint Surg Br. 1990;72:557–562. doi: 10.1302/0301-620X.72B4.2380203. [DOI] [PubMed] [Google Scholar]
- 7.Bucholz RW, Ogden JA. Patterns of ischemic necrosis of the proximal femur in nonoperatively treated congenital hip disease. The Hip: Proceedings of the Sixth Open Scientific Meeting of the Hip Society. St Louis, MO: Mosby; 1978:43–63.
- 8.Cooperman DR, Wallensten R, Stulberg SD. Post-reduction avascular necrosis in congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62:247–258. [PubMed] [Google Scholar]
- 9.Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;175:79–85. [PubMed] [Google Scholar]
- 10.Harris NH, Lloyd-Roberts GC, Gallien R. Acetabular development in congenital dislocation of the hip: with special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy. J Bone Joint Surg Br. 1975;57:46–52. [PubMed] [Google Scholar]
- 11.Lindstrom JR, Ponseti IV, Wenger DR. Acetabular development after reduction in congenital dislocation of the hip. J Bone Joint Surg Am. 1979;61:112–118. [PubMed] [Google Scholar]
- 12.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip: functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792. doi: 10.2106/00004623-199412000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Morcuende J, Meyer MD, Dolan LA, Weinstein SL. Long-term outcome after open reduction through an anteromedial approach for congenital dislocation of the hip. J Bone Joint Surg Am. 1997;79:810–817. doi: 10.2106/00004623-199706000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Nakamura J, Kamegaya M, Saisu T, Someya M, Koizumi W, Moriya H. Treatment for developmental dysplasia of the hip using the Pavlik harness: long-term results. J Bone Joint Surg Br. 2007;89:230–235. doi: 10.1302/0301-620X.89B2.18057. [DOI] [PubMed] [Google Scholar]
- 15.Roposch A, Liu LQ, Offiah A, Wedge JH. Functional outcomes in children with osteonecrosis secondary to developmental dysplasia of the hip. J Bone Joint Surg Am. 2011;93:e145. doi: 10.2106/JBJS.J.01623. [DOI] [PubMed] [Google Scholar]
- 16.Roposch A, Stohr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip: a meta-analysis. J Bone Joint Surg Am. 2009;91:911–918. doi: 10.2106/JBJS.H.00096. [DOI] [PubMed] [Google Scholar]
- 17.Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol. 1999;28:964–974. doi: 10.1093/ije/28.5.964. [DOI] [PubMed] [Google Scholar]
- 18.Sharp IK. Acetabular dysplasia: the acetabular angle. J Bone Joint Surg Br. 1961;43:268–272. [Google Scholar]
- 19.Sibinski M, Synder M, Pruszczynski B. [Hip joint development after closed reduction complicated by growth disturbance of the capital femoral epiphysis][in Polish] Chir Nazardow Ruchu Orto Pol. 2006;71:33–36. [PubMed] [Google Scholar]
- 20.Skaggs DL, Kaminsky C, Tolo VT, Kay RM, Reynolds RA. Variability in measurement of acetabular index in normal and dysplastic hips, before and after reduction. J Pediatr Orthop. 1998;18:799–801. [PubMed] [Google Scholar]
- 21.Spence G, Hocking R, Wedge JH, Roposch A. Effect of innominate and femoral varus derotation osteotomy on acetabular development in developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:2622–2636. doi: 10.2106/JBJS.H.01392. [DOI] [PubMed] [Google Scholar]
- 22.Tönnis D. Normal values of the hip joint for evaluation of x-rays in children and adults. Clin Orthop Relat Res. 1976;119:39–47. [PubMed] [Google Scholar]
- 23.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. 1. Berlin, Germany: Springer-Verlag; 1987. [Google Scholar]
- 24.Ucar DH, Isiklar ZU, Stanitski CL, Kandemir U, Tumer Y. Open reduction through a medial approach in developmental dislocation of the hip: a follow-up study to skeletal maturity. J Pediatr Orthop. 2004;24:493–500. doi: 10.1097/01241398-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 25.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30:377–399. doi: 10.1002/sim.4067. [DOI] [PubMed] [Google Scholar]
- 26.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44:1049–1060. doi: 10.2307/2531734. [DOI] [PubMed] [Google Scholar]