Abstract
Background
Alcohol addiction may reflect adaptations to stress, reward, and regulatory brain systems. While extensive research has identified both stress and impulsivity as independent risk factors for drinking, few studies have assessed the interactive relationship between stress and impulsivity in terms of hazardous drinking within a community sample of regular drinkers.
Methods
One hundred and thirty regular drinkers (56M/74F) from the local community were assessed for hazardous and harmful patterns of alcohol consumption using the Alcohol Use Disorders Identification Test (AUDIT). All participants were also administered the Barratt Impulsiveness Scale (BIS-11) as a measure of trait impulsivity and the Cumulative Stress/Adversity Checklist (CSC) as a comprehensive measure of cumulative adverse life events. Standard multiple regression models were used to ascertain the independent and interactive nature of both overall stress and impulsivity as well as specific types of stress and impulsivity on hazardous and harmful drinking.
Results
Recent life stress, cumulative traumatic stress, overall impulsivity, and nonplanning-related impulsivity as well as cognitive and motor-related impulsivity were all independently predictive of AUDIT scores. However, the interaction between cumulative stress and total impulsivity scores accounted for a significant amount of the variance, indicating that a high to moderate number of adverse events and a high trait impulsivity rating interacted to affect greater AUDIT scores. The subscale of cumulative life trauma accounted for the most variance in AUDIT scores among the stress and impulsivity subscales.
Conclusions
Findings highlight the interactive relationship between stress and impulsivity with regard to hazardous drinking. The specific importance of cumulative traumatic stress as a marker for problem drinking is also discussed.
Keywords: Impulsivity, Cumulative Stress, Alcohol Consumption, Trauma, Community Sample
The influence of environmental factors such as stress and individual difference traits such as impulsivity on the development and course of alcohol dependence are well established in both human and animal literature (Evenden, 1999a; Sinha, 2008). Neuroadaptations to stress systems have been shown to underlie the pathophysiology of alcohol, as well as stimulant, opioid, and nicotine addiction (Fox and Sinha, 2009 for review). Well-established human models of addiction such as stress-coping (Wills and Shiffman, 1985) and relapse prevention models (Marlatt and Gordon, 1985) have also presented problem drinking as a maladaptive coping response to life stressors. In addition, both animal and human studies have shown that impulsivity, in terms of impulsive choice and inhibitory failure, is also paramount to the acquisition and escalation of alcohol and substance abuse (Perry and Carroll, 2008 for review). Although both stress and impulsivity are independent risk factors for drinking, few studies have investigated the nature of their interactive relationship in terms of harmful and hazardous drinking patterns.
The interactive nature of stress regulatory mechanisms on drinking is highlighted by genetic research investigating the impact on drinking of various levels of life adversity and genetic markers implicated in regulatory behavior. For example, young adults exposed to high levels of psychosocial adversity and carrying the long variant of the serotonin transporter gene exhibit greater hazardous drinking compared with those carrying the short allele or not exposed to high levels of adversity (Laucht et al., 2009). This serotonin transporter gene polymorphism has also been shown to interact with rearing stress in nonhuman primates (Barr et al., 2004) as well as stressful life events in adolescents and young adults (Covault et al., 2007; Kaufman et al., 2007; Olsson et al., 2005) with regard to increased drinking patterns and greater nonprescription dug use. While these studies have assessed genetic markers linked to behaviors associated with impulsivity (Paaver et al., 2007; Wagner et al., 2009), a more direct relationship between various aspects of subjective trait impulsivity and cumulative life stress on problem drinking behaviors have not been evaluated within a local community sample of volunteers.
Therefore, current study examines the relationship between various types of stress and different aspects of impulsivity on alcohol use and alcohol-related problems as assessed by the Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 2001). Both epidemiological and clinical research has indicated that recent life stress (Perkins, 1999; Rutledge and Sher, 2001), cumulative adverse life events, including life traumas (Lloyd and Turner, 2008; Turner and Lloyd, 2003), and traumatic life experiences (Breslau et al., 2003; Reed et al., 2007) have all been positively associated with increases in drinking and substance abuse. However, diverse types of stress may differentially affect biopsychological markers associated with drinking vulnerability, showing certain stressors to be stronger indicators of problem drinking than others. For example, while traumatic or enduring stress has been associated with reduced cortisol response to stress exposure (Geracioti et al., 2008), daily stress has been associated with increased cortisol activity (Brantley et al., 1988; Roy et al., 2003;). Similarly, heart rate variability (HRV) and dopamine (DA) neurotransmission have also been shown to differ with regard to whether stressors are acute or chronic (Farah et al., 2004; Kalivas and Duffy, 1995; Lucas et al., 2004). In the current study, we use a comprehensive cumulative stress measure adapted from Turner and Wheaton (1995) to assess recent adverse life events as well as cumulative traumatic stress, major life events, and chronic stress.
Similarly, impulsivity is a multidimensional construct (Evenden, 1999b; de Wit, 2009) defined in the literature by a wide range of paradigms (Evenden, 1999a for review). In general, however, behavioral studies have indicated that impulsive choice (or failure to delay gratification) and response inhibition are most relevant to the transition from controlled to compulsive drinking (Evenden, 1999a; Perry and Carroll, 2008; Rubio et al., 2007). In the current study, we use the BIS-11 (Patton et al., 1995) a widely used and well standardized measure of impulse control likely to provide a reliable subjective index of these regulatory processes. While the Nonplanning subscale of the BIS has been associated with performance on delayed discounting tests as both may reflect an insensitivity to future gratification (de Wit et al., 2007), the Attention and Motor subscales have been shown to correlate with inhibitory control-related tasks including Go No Go and Trails B (Asahi et al., 2004; Keilp et al., 2005; Spinella, 2007).
We therefore aim to assess the effects of life adversity and trait impulsivity on alcohol use and alcohol-related problems, as measured by the AUDIT in a community sample. Establishing the nature and relative contribution of both stress and impulsivity to at-risk drinking within a community sample will help determine better tailored intervention programs focused on prevention and the progression of alcohol abuse.
METHOD
Participants
Recruitment
One hundred and thirty individuals (56M/74F) were drawn from a community sample in and around the New Haven area and recruited via advertisements placed either on-line or in local newspapers and community centers. All participants were recruited and screened for eligibility as part of the Human Subjects CORE of the Yale Stress Center. Following initial phone screening and intake assessments, participants were filtered into various human laboratory and imaging projects dependent upon specific criteria. Demographic, stress, impulsivity, and alcohol use assessments were conducted as part of the CORE battery of assessments for the Yale Stress Center studies.
Enrollment Eligibility
Eligibility was ascertained via an initial phone screen. All participants had to be between the ages of 18 and 50 and able to read and write in English to at least a sixth-grade level and meet stringent health requirements assessed by a research nurse specialist. Participants were excluded if they met current criteria for any DSM-IVTR psychiatric disorder or dependence criteria for any drug, with the exception of nicotine and alcohol. However, any participant requiring alcohol detoxification was excluded. Participants currently using prescription opiates, methadone, and medications for other acute or chronic psychiatric or medical conditions were also excluded. All participants gave both written and verbal informed consent, and the study was approved by the Human Investigation Committee of the Yale University School of Medicine.
Procedure
Potential subjects completed an initial screening over the telephone to determine eligibility based on inclusion/exclusion criteria. Following initial eligibility screening, participants were scheduled two, 2-hour assessment and evaluation sessions conducted at the Yale Stress Center at 2 Church Street South. During the first session, participants met with research assistants to complete informed consent forms for both the current and subsequent studies as well as complete medical, substance abuse, and psychiatric health assessments including the Cornell Medical Index, the Structured Clinical Interview for the Diagnostic and Statistical Manual (SCID; First et al., 1997), and a physical health assessment. During a subsequent intake session, participants again met with the same research assistant to complete baseline demographic questionnaires, measures of IQ (Shipley), alcohol use (AUDIT), stress (CSC), and impulsivity (BIS-11). Following this, participants received a physical examination with a research nurse specialist assessing cardiovascular, renal, hepatic, pancreatic, hematopoietic, and thyroid function to ensure all participants were in good health. During both appointments, subjects underwent breath alcohol testing and urine toxicology screens to confirm self-report of alcohol and drug information.
Assessments
Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 2001)
The AUDIT is a 10-item screening instrument designed to identify drinking behaviors and distinguish between low-risk drinkers and individuals with hazardous and harmful patterns of alcohol consumption to provide the appropriate intervention. Factor analysis has indicated that the AUDIT loads onto two main factors (Donovan et al., 2006; Reinert and Allen, 2002); a consumption factor relating to drinking behaviors (Items 1 to 3; e.g., “How often do you have six or more drinks on one occasion?” with item response: 0 = Never, 1 = Less than monthly, 2 = Monthly, 3 = Weekly, 4 = Daily, or almost daily) the other relating to the adverse consequences of drinking (Items 4 to 10; e.g., “Have you or someone else been injured as a result of your drinking?” with item response: 0 = No, 2 = Yes, but not in the last year, 3 = Yes, during the last year). While hazardous drinking is defined as a pattern of alcohol consumption that increases the risk of harmful consequences, harmful use is defined as alcohol use that results in physical, mental, and/or social consequences (WHO, 1992). Decades of research has found the AUDIT to be an accurate measure of assessing risk of alcohol problems across gender, age, and cultures (Allen et al., 1997; Saunders et al., 1993). It has been found to correlate both with the Michigan Alcohol Screening Test (MAST) (Bohn et al., 1995) and the CAGE (Hays et al., 1995) as well as future indicators of alcohol-related problems (Claussen and Aasland, 1993). It has been found to have high test–retest reliability (Daeppen et al., 2000) and internal consistency reliability (Ivis et al., 2000).
Barratt Impulsiveness Scale (BIS-11; Patton et al., 1995)
The BIS-11 is a 30-item self-report questionnaire which provides a total score of general impulsivity, by summing three nonoverlapping second-order subscales which demonstrate good reliability (Spinella, 2007). These comprise, Attentional Impulsivity (AI; instability of attention and decision making), Motor Impulsivity (MI: acting without thinking), and Nonplanning Impulsivity (NPI: inability to plan ahead). These subscales are comprised of 6 first-order factors: attention (AI—I do not pay attention), motor (MI—I do things without thinking), self-control (NPI—I plan trips well ahead of time), Cognitive Complexity (NPI—I like to think about complex problems), Perseverance (MI—I can only think about one problem at a time), and Cognitive Instability (AI—I have “racing” thoughts). The BIS-11 is widely used in both research and clinical settings and is highly associated with many clinical disorders characterized by impulsive behavior. These include substance abuse (Lane et al., 2007; Lejuez et al., 2007), pathological gambling (Fuentes et al., 2006; Sáez-Abad and Bertolín-Guillén, 2008), borderline personality disorder (Fossati et al., 2004), aggression (Houston et al., 2003), and eating disorders (Nasser et al., 2004). The scale has also been associated with both structural and functional neuroadaptations within the prefrontal cortex (Spinella, 2004; for review). The BIS shows good test–retest reliability and demonstrates high convergent validity with similar self-report measures including the Zuckerman Sensation-Seeking Scale, the Eysenck Impulsiveness Scale, and the Behavioral Inhibition/Activation Scales (Stanford et al., 2009). The BIS-11 uses a four-point Likert scale ranging from 1 (rarely/never) to 4 (almost always). Higher scores indicate higher levels of impulsiveness. Scores between 52 and 72 are within normal impulsivity limits (Stanford et al., 2009)
The Cumulative Stress/Adversity Checklist (CSC, Adapted from Turner and Wheaton, 1995)
This 140-item event interview is a comprehensive measure of cumulative adversity that covers major life and recent life events, life trauma, and chronic stressors. Recent life events are also included. Recent Life Events: comprise a checklist of 33 items referring to discreet stressful events occurring in the previous 12 months. These are broadly divided into items referring to exits from the social field (i.e., death, divorce, relationships ending) and undesirable events both interpersonal and financial (i.e., being attacked, financial crises, robberies). Major Life Events: this section includes 11 items relating to social adversities, not typically violent in nature, but which differ from standard life events because of their severity and potentially long-term consequences (Turner and Lloyd, 2003). Examples of items are parental divorce and failing a grade in school. Life Traumas: this section comprises 34 items relating to life trauma, witnessed violence, and traumatic news. Life trauma includes events that imply force or coercion and include physical, emotional, and/or sexual abuse, including rape and being injured with a weapon. Witnessed violence contains items which involve being present in dangerous or upsetting situations, such as seeing some get shot or attacked with a weapon. Traumatic news is comprised of items which involve not being present, but rather hearing news about someone else being killed, abused, or injured. Chronic Life events: this section comprises 62 items relating to continuous stressors or ongoing life problems. Items refer to longer-term inter-personal, social, and financial relationships and responsibilities including work and home environment and relationships with family and significant others. In all cases, a higher score relates to a higher number of stressful events.
Statistical Analyses
All analyses were conducted using SAS software (version 9.1; SAS Institute, Cary, NC). To test the separate and interactive effects of cumulative stress and impulsivity and their subscales on the AUDIT score, we conducted three multiple regression analyses. In all regression equations, the AUDIT total score was the dependent variable.
In the initial regression model, we conducted a series of individual linear regressions using total Stress, total Impulsivity and all component sub-scales (i.e., nonplanning, cognitive, motor, cumulative chronic life stress, cumulative major life stress, cumulative traumatic stress, and recent life stress) as predictors to identify independent contribution of each on the AUDIT scores.
In the second regression model, Stress (total CSC score), Impulsivity (total BIS score), and the Stress × Impulsivity interaction term were all entered as predictor variables. A standard regression procedure was used.
In the third regression model, all significant stress and impulsivity subscales (from the independent regressions in Model 1) were entered simultaneously into the model to identify the most robust predictor(s) of hazardous and harmful drinking. A standard regression procedure was used.
Regression Assumptions
Multicollinearity was assessed using tolerance coefficients and variance inflation factors (VIF) for each model. AUDIT scores and predictors were also mean-centered to further reduce the chances of multicollinearity among predictor variables following square root transformation (Enders and Tofighi, 2007). Standard threshold values of Tolerance >0.01, or VIF not exceeding 10, were applied. To assess error variance and the presence of heteroscedasticity, residuals were plotted against fitted values for all models. In addition, the Bartlett test was used to determine homoscedasticity assumptions. Normal probability plots of the residuals were used to examine approximate normal assumption.
RESULTS
Participants
All participant demographic data are presented in Table 1.
Table 1.
Showing Sample Demographics and Assessment Scores
| N = 130 | |
|---|---|
| Demographic variables | |
| Age* | 33.4 (9.69) |
| Years of education* | 14.5 (2.34) |
| Gender—% male | 56 (43.08%) |
| Race (%) | |
| African American | 34 (26.15%) |
| Caucasian | 82 (63.08%) |
| Hispanic | 5 (3.85%) |
| Asian | 2 (1.54%) |
| Other | 7 (5.38%) |
| Martial status (%) | |
| Never married | 87 (66.92%) |
| Married | 30 (23.08%) |
| Divorced | 11 (8.46%) |
| Cohabitating | 2 (1.54%) |
| Psychiatric history | |
| Lifetime prevalence of PTSD | 1 (0.77%) |
| Lifetime other anxiety disorders | 3 (2.31%) |
| Lifetime mood disorders | 13 (10%) |
| Alcohol use | |
| Audit score* | 7.2 (7.69) |
| No. of years of alcohol use* | 10.3 (8.93) |
| No. of days drinking in last month* | 7.6 (8.4) |
| Total no. of drinks in last month* | 42.6 (121.9) |
| Assessments | |
| Total impulsiveness* | 61.2 (12.42) |
| Nonplanning impulsiveness* | 23.1 (5.11) |
| Cognitive impulsiveness* | 16.8 (5.15) |
| Motor impulsiveness* | 21.3 (4.64) |
| Total stress* | 67.4 (17.76) |
| Major life events* | 2.1 (1.79) |
| Life traumas* | 6.6 (4.27) |
| Recent life events* | 2.7 (2.30) |
| Chronic stressors* | 55.8 (14.43) |
PTSD, post-traumatic stress disorder.
Mean values (standard deviations). All other measures reported in frequency (%).
Regression Assumptions
Both tolerance coefficients and VIF scores indicated no serious problems regarding multicollinearity. To account for skewed distribution, data from the AUDIT scale were transformed using the square root (√) calculation. When residuals were plotted against the fitted values, graphs indicated homoscedasticity, and Bartlett’s test for homogeneity of residual variance was insignificant at the p = 0.05 level for all regression models.
Regression Analyses (Findings From All Regression Models Displayed in Table 2)
Table 2.
Showing Findings From All Regression Models
| Individual linear regressions for each predictor on AUDIT score; model 1 | R2 (Adjusted) | β | SE | p |
|---|---|---|---|---|
| Total stress | 0.005 | 0.009 | 0.007 | 0.195 |
| Recent life events | 0.019 | 0.095 | 0.050 | 0.061 |
| Cumulative major life events | 0.001 | 0.07 | 0.065 | 0.284 |
| Cumulative trauma | 0.100 | 0.101 | 0.026 | <.0001 |
| Chronic life events | −0.008 | 0.001 | 0.008 | 0.946 |
| Total impulsivity | 0.057 | 0.027 | 0.009 | 0.004 |
| Nonplanning | 0.048 | 0.061 | 0.002 | 0.007 |
| Cognitive | 0.042 | 0.057 | 0.022 | 0.011 |
| Motor | 0.027 | 0.053 | 0.025 | 0.033 |
| Regression model 2 | R2 (Adjusted) | Predictors | β | SE | p | VIF | TC |
|---|---|---|---|---|---|---|---|
| Standard procedure | 0.0853 | Total stress | 0.0060 | 0.0063 | 0.3432 | 1.0140 | 0.986 |
| Total impulsivity | 0.0274 | 0.0091 | 0.0030 | 1.0181 | 0.982 | ||
| Stress × impulsivity | 0.0014 | 0.0006 | 0.0286 | 1.0057 | 0.994 |
| Regression model 3 | R2 (Adjusted) | Predictors | β | SE | p | VIF | TC |
|---|---|---|---|---|---|---|---|
| Standard procedure | 0.118 | Trauma | 0.0894 | 0.0263 | 0.0009 | 1.0492 | 0.9532 |
| Nonplanning impulsivity | 0.0318 | 0.0295 | 0.2832 | 1.9000 | 0.5263 | ||
| Cognitive impulsivity | 0.0231 | 0.0293 | 0.4324 | 1.9033 | 0.5254 | ||
| Motor impulsivity | 0.0030 | 0.0300 | 0.9200 | 1.6234 | 0.6160 |
All predictor variables are centered. The significance values are in bold. SE, standard error; TC, tolerance coefficients; VIF, variance inflation factors.
Regression Model 1
After conducting individual linear regressions of all subscales and total scores onto AUDIT scores, the following predictors showed significant main effects in predicting AUDIT scores: cumulative trauma (β = 0.10, t = 3.91, p < 0.001); total Impulsivity (β = 0.06, t = 2.97, p = 0.004); nonplanning-related impulsivity (β = 0.05, t = 2.75, p = 0.007); cognitive impulsivity (β = 0.04, t = 2.59, p = 0.01); motor impulsivity (β = 0.19, t = 2.15, p = 0.03).
Regression Model 2
Findings from the second regression model, using centered data, indicated that the interaction term (total Stress × total Impulsivity) was a significant predictor of AUDIT score after controlling for the main effect of total Impulsivity and total Stress (β = 0.001, t = 2.21, p < 0.03; tolerance coefficient: 0.99). When the interactive term was included, total Impulsivity was independently predictive of AUDIT scores after controlling for total Stress (β = 0.03, t = 3.03, p = 0.003; tolerance coefficient: 0.98; VIF: 1.02). Total Stress was not independently predictive of AUDIT. However, it is important to note that interpretation of independent Impulsivity and Stress effects is difficult in a regression model including a multiplicative interaction term (Cohen, 1978; Friedrich, 1982). The overall model accounted for 9%of the variance in AUDIT scores.
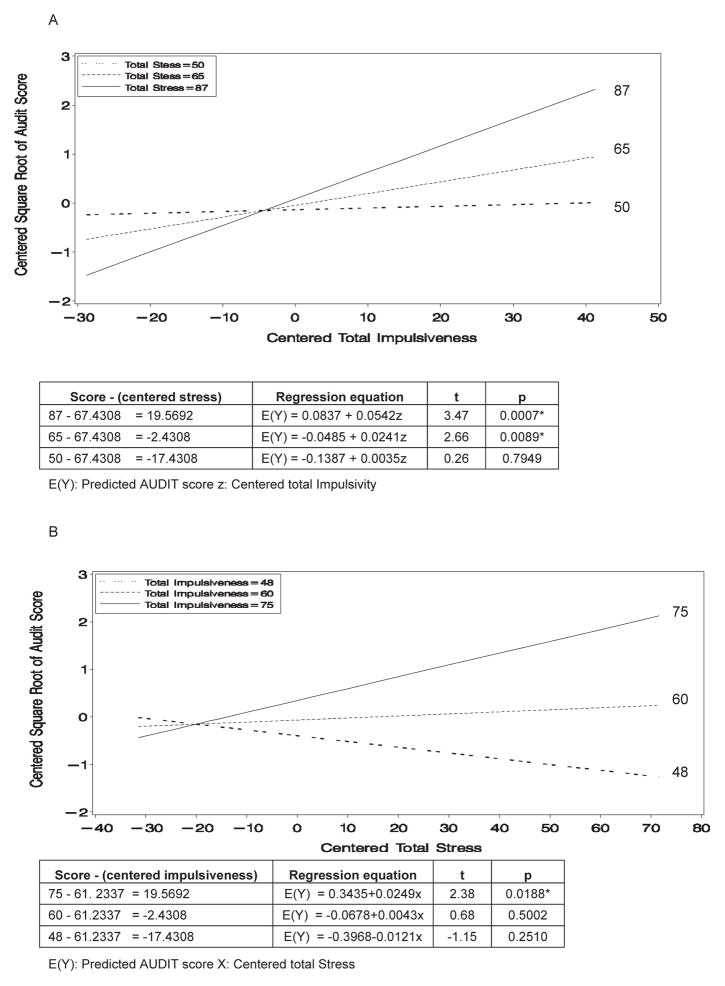
Three critical values for low, moderate, and high total Stress and Impulsivity were used to plot an interaction graph showing the regression of AUDIT scores onto one predictor at a critical value of the other predictor. Total Stress and total Impulsivity scores were grouped into low (n = 44 CSC; n = 43 BIS), moderate (n = 43 CSC; n = 45 BIS), and high (n = 43 CSC; n = 42 BIS) tertiles using the PROC RANK statement available in SAS (SAS Institute). The mean score for each tertile was then used to represent the critical values of each scale (Fig. 1A, B).
Fig. 1.
Line graphs illustrating the effects of Total Stress × Total Impulsivity on AUDIT scores. (A) The simple slopes of the regression of trait impulsivity on AUDIT score at high, medium, and low levels of stress. (B) The simple slopes of the regression of stress on AUDIT score at high, medium, and low levels of trait impulsivity.
In Fig. 1A, the graph show simple slopes representing the regression of the AUDIT score on total Impulsivity at the three critical mean values of total Stress (i.e., high stress, 87; moderate stress, 65; low stress, 50). The graph shows that the high total Stress score of 87 produced a regression slope for total Impulsivity in relation to AUDIT of 0.054 (p = 0.007). For the moderate total Stress score of 65, the regression slope for total Impulsivity in relation to AUDIT score was 0.024 (p = 0.089). A low total Stress score of 50 produced a slope of 0.0035 (ns). Findings indicate that the slopes reflecting the regression of AUDIT scores onto total Impulsivity scores increase as total Stress increases.
In Fig. 1B, the simple slopes represent the regression of the AUDIT score on total Stress at the three critical mean values of total Impulsivity (i.e., high impulsivity, 75; moderate impulsivity, 60; low impulsivity, 48). A high total Impulsivity score of 75 produced a regression slope for total Stress in relation to AUDIT score of 0.025 (p < 0.02). Again, the regression slopes for moderate and lower scores were much lower. For a total Impulsivity score of 60, the slope was 0.004 (ns), and for a total Impulsivity score of 48, the slope was 0.012 (ns). This indicates that the slopes reflecting the regression of AUDIT scores onto total Stress scores increase as the total Impulsivity score increases.
The critical values for low, moderate, and high total Stress and Impulsivity were also used to plot bar graphs (Fig. 2) to better illustrate that individuals who reported a combination of high total Stress and high total Impulsivity were more likely to report hazardous drinking levels on the AUDIT (ie > 8).
Fig. 2.
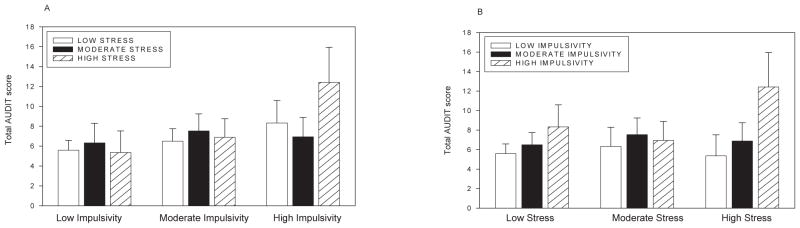
Bar graphs illustrating the effects of Total Stress × Total Impulsivity on AUDIT scores. (A) Bar graphs showing AUDIT scores by low, moderate, and high total Stress and total Impulsivity scores: impulsivity groups shown on x-axis. (B) Bar graphs showing AUDIT scores by low, moderate, and high total Stress and Total Impulsivity scores: stress groups shown on x-axis. Footnote: low, moderate, and high groups (divided based on tertiles) were used only to better display the interaction term. Multiple regressions were performed on continuous data.
Regression Model 3
Findings from the third regression model, using centered data, indicated that cumulative trauma (β = 0.0,894, t = 3.41, p = 0.009; tolerance coefficient: 0.95; VIF: 1.05) was the only significant predictor of AUDIT score after controlling for all other subscales.
DISCUSSION
Current findings replicated previous data to show that certain types of environmental stress, particularly cumulative life traumas and trait impulsivity, and its subscales were each significantly associated with AUDIT scores in a sample of healthy volunteers recruited from the local community. More importantly, a separate model that evaluated the modulatory effects of total stress and impulsivity showed that overall life adversity and trait impulsivity have an interactive effect on AUDIT scores. Impulsivity was shown to be a significant indicator of hazardous drinking in individuals reporting high and moderate levels of adverse life stress but not in those reporting low levels of stress. In addition, adverse life events were a significant indicator of drinking in individuals reporting high levels of impulsivity but not moderate or low levels. This complex interaction as illustrated in Fig. 2 indicates individuals reporting a high number of adverse life events alongside low and moderate levels of impulsivity were more likely to demonstrate AUDIT scores lower than 8. Importantly, these findings suggest that it may be the interactive effects of both a high number of stressful life events along with moderate to high trait impulsivity which increases the likelihood of harmful and/or hazardous drinking (AUDIT > 8).
Findings from the independent regression models show that within the community sample, cumulative traumatic stress and recent life events were predictive of AUDIT score, although the latter only approached statistical significance. Similarly, overall impulsivity and all impulsivity subscales, including a lack of forethought (nonplanning), acting without thinking (motor), and attentional instability (attention), were independently predictive of hazardous drinking patterns. The association between cumulative and recent adverse life events and drinking has been well established in adolescent and adult populations (Clark et al., 1997; Lloyd and Turner, 2008; Perkins, 1999; Sinha, 2008; Turner and Lloyd, 2003;), as well as clinical populations comprising individuals with mood and anxiety disorders (Brady and Sinha, 2005). Similarly, trait impulsivity has been associated with drinking in individuals with either alcohol use disorders (Charney et al., 2010) or impulse control-related disorders including bulimia (Sysko and Hildebrandt, 2009), borderline personality disorder (Wilson et al., 2006), and pathological gambling (Chambers and Potenza, 2003). Current findings are therefore unique in that they illustrate first that specific aspects of environmental stress as well as trait impulsivity may also be important independent predictors of problem drinking within a nonclinical and nondependent sample of community drinkers. Second, that the interaction between experiencing a high number of adverse life events in general and demonstrating high to moderate levels of trait impulsivity may also represent an integral relationship associated with hazardous drinking in nondependent community volunteers. As such, it is possible that high adverse life events and moderate to high trait impulsivity may be associated with the developmental progression to, as well as maintenance of alcoholism, although a lack of prospective data means that the temporal order of this association is impossible to ascertain in the current study.
The nature of the interactive relationship between stress and impulsivity is consistent with both experimental and clinical research that highlights the effects of stress on impulsivity and self-control. An earlier body of social cognitive research shows that laboratory-induced stress was found to decrease cognitive performance, sustained attention and flexibility, and inhibition of prepotent responding (Cohen, 1980; Glass et al., 1969, 1971; Hockey, 1970; Sinha, 2001), thereby increasing the chance of impulsive behaviors. Similarly, other research in adolescents and adults has shown stress and negative affect to decrease self-control and ability to delay gratification (Mischel et al., 1989; Muraven & Baumeister, 2000; Swann, 2003; Tice et al., 2001). In a more direct examination of subjective stress and impulsivity, Fields and colleagues (2009) recently assessed the relationship between subjective stress and delayed discounting in smoking and nonsmoking adolescents and showed that while stress and delay discounting scores each were associated with smoking, delay discounting mediated the relationship between stress and smoking in adolescents. Previous evidence also indicates the moderating effects of impulsivity on the stress-negative affect model of alcohol consumption (Hussong and Chassin, 1994). In the latter study, impulsivity was shown to moderate the effects of depression on drinking where depressed and impulsive young adults drank significantly more heavily than depressed nonimpulsive adolescents and nondepressed adolescents (Hussong and Chassin, 1994). The current findings are consistent with this growing body of evidence which suggests that the interactive effect of total cumulative stress and impulsivity is associated with higher levels of alcohol consumption and alcohol-related problems.
When all the subscales of cumulative stress and impulsivity were included in the model, experiencing a high number of life traumas was the most robust independent predictor of AUDIT scores. While much prior research has documented high rates of alcohol dependence following post-traumatic stress disorder (PTSD) (Driessen et al., 2008; Jacobsen et al., 2001; McFarlane, 1998) and childhood trauma (De Bellis, 2002; Hyman et al., 2005; Waldrop et al., 2007), these studies focus predominantly on stress hyperreactivity relating to a specific traumatic experiences and a PTSD diagnosis. In contrast, findings from this study indicate that the experience of high cumulative exposures to traumatic life events (such as being physically abused or injured by a spouse/boyfriend/girlfriend; witnessing a serious accident or disaster where someone else was hurt very badly or killed; being attacked), even without PTSD diagnosis, is one of the most robust predictors of susceptibility to alcohol-related problems. This is particularly important as epidemiological studies show that experiencing multiple traumatic events are not uncommon (Shevlin et al., 2007; Turner and Lloyd, 2003). Moreover, current findings are consistent with other recent studies which highlight the importance of cumulative multiple trauma experiences as risk factors for subsequent PTSD, psychosis, depression, anxiety, postinjury drinking in adolescents, and many other health aspects including problem drinking (Breslau et al., 2003; Dunn et al., 2008; Schnurr and Green, 2004; Shevlin et al., 2007; Tanskanen et al., 2004).
It is interesting to note that in regression 3 when all significant subscales of stress and impulsivity were entered into the model, only life trauma remained significant. This suggests that life trauma possibly shares some variance with impulsivity subscales and its entry into the model makes impulsivity subscales nonsignificant. Higher number of traumatic events through the life span may increase the stress load on the individual throughout the life span weakening both brain and physiological processes and increasing the likelihood of poor executive function and greater maladaptive behaviors (McEwen, 2007; Sinha, 2008). Indeed, evidence from adolescent and adult samples indicates that high levels of trauma and stress are associated with poor behavioral and emotional control and higher levels of alcohol and substance abuse (Clark et al., 1997; De Bellis, 2002; Fishbein et al., 2006; Simons, 2003; Wills et al., 2002, 2006, 2007). These previous data combined with the current findings indicate that the specific effects of childhood and adult traumatic life experiences on the development of impulsive traits and impulsivity would be important area of study in future research.
Conclusions regarding the relationship between stress and impulsivity with regard to alcohol consumption in the current study are limited by several factors. First, the cross-sectional design employed in this study does not allow for conclusions to be drawn regarding the temporal ordering of stress, impulsivity, and alcohol use within this sample of regular drinkers. As preclinical studies and prospective research in alcohol-dependent humans provide support for the fact that increased levels of stress and impulsivity culminate in increased drinking (Deckel and Hesselbrock, 1996; King et al., 2009; Sinha, 2008) and further that alcohol use increases impulsivity and stress system dysregulation (Olmstead, 2006; Perry and Carroll, 2008 for review), conclusions cannot be made regarding causality. Second, the study relies solely on self-report measures of stress and impulsivity, and future research assessing comparative subjective, biological, and behavioral markers of both in relation to alcohol consumption is encouraged.
Despite these limitations, our study is among the first to demonstrate that an interactive relationship between cumulative life stress and trait impulsivity contributes significantly to hazardous drinking in a community sample of regular drinkers. Findings also indicate that cumulative traumatic life events account for the majority of the variance in the effects of different types of stress and impulsivity on higher AUDIT scores. These data support the need for future studies using longitudinal predictive models to fully assess the separate and interactive effects of stress and impulsivity on alcohol consumption and development of alcohol use disorders.
Acknowledgments
We thank the staff at the Yale Stress Center at Yale University School of Medicine for their assistance in completing this study.
This research was supported by NIH grants: R01-AA13892 (Sinha), PLI—DA024859 (Sinha) UL1-DE019586 (Sinha) and the NIH Roadmap for Medical Research Common Fund.
Footnotes
No claim to original U.S. government works
References
- Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the Alcohol Use Disorders Identification Test (AUDIT) Alcohol Clin Exp Res. 1997;21:613–619. Review. [PubMed] [Google Scholar]
- Asahi S, Okamoto Y, Okada G, Yamawaki S, Yokota N. Negative correlation between right prefrontal activity during response inhibition and impulsiveness: a fMRI study. Eur Arch Psychiatry Clin Neurosci. 2004;254:245– 251. doi: 10.1007/s00406-004-0488-z. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. Guidelines for use in primary care. 2. World Health Organization. Department of Mental Heath and Substance Dependence; 2001. AUDIT. The Alcohol Use Disorders Identification Test. [Google Scholar]
- Barr CS, Newman TK, Lindell S, Shannon C, Champoux M, Lesch KP, Suomi SJ, Goldman D, Higley JD. Interaction between serotonin transporter gene variation and rearing condition in alcohol preference and consumption in female primates. Arch Gen Psychiatry. 2004;61:1146–1152. doi: 10.1001/archpsyc.61.11.1146. [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The Alcohol Use Disorders Identification Test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol. 1995;56:423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am J Psychiatry. 2005;162:1483–1493. doi: 10.1176/appi.ajp.162.8.1483. Review. [DOI] [PubMed] [Google Scholar]
- Brantley PJ, Dietz LS, McKnight GT, Jones GN, Tulley R. Convergence between the Daily Stress Inventory and endocrine measures of stress. J Consult Clin Psychol. 1988;56:549–551. doi: 10.1037//0022-006x.56.4.549. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Schultz LR. Posttraumatic stress disorder and the incidence of nicotine, alcohol, and other drug disorders in persons who have experienced trauma. Arch Gen Psychiatry. 2003;60:289–294. doi: 10.1001/archpsyc.60.3.289. [DOI] [PubMed] [Google Scholar]
- Chambers RA, Potenza MN. Neurodevelopment, impulsivity, and adolescent gambling. J Gambl Stud. 2003;19:53–84. doi: 10.1023/a:1021275130071. Review. [DOI] [PubMed] [Google Scholar]
- Charney DA, Zikos E, Gill KJ. Early recovery from alcohol dependence: factors that promote or impede abstinence. J Subst Abuse Treat. 2010;38:42–50. doi: 10.1016/j.jsat.2009.06.002. [DOI] [PubMed] [Google Scholar]
- Clark DB, Lesnick L, Hegedus AM. Traumas and other adverse life events in adolescents with alcohol abuse and dependence. J Am Acad Child Adolesc Psychiatry. 1997;36:1744–1751. doi: 10.1097/00004583-199712000-00023. [DOI] [PubMed] [Google Scholar]
- Claussen B, Aasland OG. The Alcohol Use Disorders Identification Test (AUDIT) in a routine health examination of long-term unemployed. Addiction. 1993;88:363–368. doi: 10.1111/j.1360-0443.1993.tb00823.x. [DOI] [PubMed] [Google Scholar]
- Cohen J. Partialed products are interactions; partialed powers are curve components. Psychol Bull. 1978;85:858–866. [Google Scholar]
- Cohen S. Aftereffects of stress on human performance and social behavior: a review of research and theory. Psychol Bull. 1980;88:82–108. [PubMed] [Google Scholar]
- Covault J, Tennen H, Armeli S, Conner TS, Herman AI, Cillessen AH, Kranzler HR. Interactive effects of the serotonin transporter 5-HTTLPR polymorphism and stressful life events on college student drinking and drug use. Biol Psychiatry. 2007;61:609–616. doi: 10.1016/j.biopsych.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Yersin B, Landry U, Pécoud A, Decrey H. Reliability and validity of the Alcohol Use Disorders Identification Test (AUDIT) imbedded within a general health risk screening questionnaire: results of a survey in 332 primary care patients. Alcohol Clin Exp Res. 2000;24:659–665. [PubMed] [Google Scholar]
- De Bellis MD. Developmental traumatology: a contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology. 2002;27:155– 170. doi: 10.1016/s0306-4530(01)00042-7. [DOI] [PubMed] [Google Scholar]
- Deckel AW, Hesselbrock V. Behavioral and cognitive measurements predict scores on the MAST: a 3-year prospective study. Alcohol Clin Exp Res. 1996;20:1173–1178. doi: 10.1111/j.1530-0277.1996.tb01107.x. [DOI] [PubMed] [Google Scholar]
- Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among outpatients with alcohol dependence in the COMBINE study. Addiction. 2006;101:1696–1704. doi: 10.1111/j.1360-0443.2006.01606.x. [DOI] [PubMed] [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, Kemper U, Koesters G, Chodzinski C, Schneider U, Broese T, Dette C, Havemann-Reinicke U TRAUMAB-Study Group . Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multicenter study. Alcohol Clin Exp Res. 2008;32:481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Dunn C, Rivara FP, Donovan D, Fan MY, Russo J, Jurkovich G, Zatzick D. Predicting adolescent alcohol drinking patterns after major injury. J Trauma. 2008;65:736–740. doi: 10.1097/TA.0b013e31817de40f. [DOI] [PubMed] [Google Scholar]
- Enders CK, Tofighi D. Centering predictor variables in cross-sectional multilevel models: a new look at an old issue. Psychol Methods. 2007;12:121–138. doi: 10.1037/1082-989X.12.2.121. [DOI] [PubMed] [Google Scholar]
- Evenden JL. Impulsivity: a discussion of clinical and experimental findings. J Psychopharmacol. 1999a;13:180–192. doi: 10.1177/026988119901300211. Review. [DOI] [PubMed] [Google Scholar]
- Evenden JL. Varieties of impulsivity. Psychopharmacology (Berl) 1999b;146:348–361. doi: 10.1007/pl00005481. Review. [DOI] [PubMed] [Google Scholar]
- Farah VM, Joaquim LF, Bernatova I, Morris M. Acute and chronic stress influence blood pressure variability in mice. Physiol Behav. 2004;83:135– 142. doi: 10.1016/j.physbeh.2004.08.004. [DOI] [PubMed] [Google Scholar]
- Fields S, Leraas K, Collins C, Reynolds B. Delay discounting as a mediator of the relationship between perceived stress and cigarette smoking status in adolescents. Behav Pharmacol. 2009;20:455–460. doi: 10.1097/FBP.0b013e328330dcff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for the DSM-IV Axis I Disorders – Patient Edition (SCID-I/P Version 2.0, 4/97 revision) New York State Psychiatric Institute; New York: 1997. [Google Scholar]
- Fishbein DH, Herman-Stahl M, Eldreth D, Paschall MJ, Hyde C, Hubal R, Hubbard S, Williams J, Ialongo N. Mediators of the stress-substance-use relationship in urban male adolescents. Prev Sci. 2006;7:113–126. doi: 10.1007/s11121-006-0027-4. [DOI] [PubMed] [Google Scholar]
- Fossati A, Barratt ES, Carretta I, Leonardi B, Grazioli F, Maffei C. Predicting borderline and antisocial personality disorder features in nonclinical subjects using measures of impulsivity and aggressiveness. Psychiatry Res. 2004;125:161–170. doi: 10.1016/j.psychres.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Fox HC, Sinha R. In: Stress, Neuroendcrine Response and Addiction in Women, in Women and Addiction: A Comprehensive Textbook. Brady K, Greenfield S, editors. Gulidford Press; NY: 2009. pp. 65–83. [Google Scholar]
- Friedrich RJ. In defense of multiplicative terms in multiple regression equations. Am J Pol Sci. 1982;26:797–833. [Google Scholar]
- Fuentes D, Tavares H, Artes R, Gorenstein C. Self-reported and neuropsychological measures of impulsivity in pathological gambling. J Int Neuropsychol Soc. 2006;12:907–912. doi: 10.1017/S1355617706061091. [DOI] [PubMed] [Google Scholar]
- Geracioti TD, Jr, Baker DG, Kasckow JW, Strawn JR, Jeffrey Mulchahey J, Dashevsky BA, Horn PS, Ekhator NN. Effects of trauma-related audiovisual stimulation on cerebrospinal fluid norepinephrine and corticotropin-releasing hormone concentrations in post-traumatic stress disorder. Psychoneuroendocrinology. 2008;33:416–424. doi: 10.1016/j.psyneuen.2007.12.012. [DOI] [PubMed] [Google Scholar]
- Glass DC, Reim B, Singer JE. Behavioral consequences of adaptation to controllable and uncontrollable noise. J Exp Soc Psychol. 1971;7:244–257. [Google Scholar]
- Glass DC, Singer JE, Friedman LN. Psychic cost of adaptation to an environmental stressor. J Person Soc Psychol. 1969;12:200–210. doi: 10.1037/h0027629. [DOI] [PubMed] [Google Scholar]
- Hays RD, Merz JF, Nicholas R. Response burden, reliability, and validity of the CAGE, Short MAST, and AUDIT alcohol screening measures. Behavior Research Methods, Instruments, and Computers. 1995;27:277–280. [Google Scholar]
- Hockey GRJ. Effect of loud noise on attentional selectivity. Q J Exp Psychol. 1970;22:28–36. [Google Scholar]
- Houston RJ, Stanford MS, Villemarette-Pittman NR, Conklin SM, Helfritz LE. Neurobiological correlates and clinical implications of aggressive subtypes. Journal of Forensic Neuropsychology. 2003;3:67–87. [Google Scholar]
- Hussong AM, Chassin L. The stress-negative affect model of adolescent alcohol use: disaggregating negative affect. J Stud Alcohol. 1994;55:707–718. doi: 10.15288/jsa.1994.55.707. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Garcia M, Kemp K, Mazure CM, Sinha R. A gender specific psychometric analysis of the early trauma inventory short form in cocaine dependent adults. Addict Behav. 2005;30:847–852. doi: 10.1016/j.addbeh.2004.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivis FJ, Adlaf EM, Rehm J. Incorporating the AUDIT into a general population telephone survey: a methodological experiment. Drug Alcohol Depend. 2000;60:97–104. doi: 10.1016/s0376-8716(99)00145-3. [DOI] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. 2001;158:1184–1190. doi: 10.1176/appi.ajp.158.8.1184. Review. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Duffy P. Selective activation of dopamine transmission in the shell of the nucleus accumbens by stress. Brain Res. 1995;675:325–328. doi: 10.1016/0006-8993(95)00013-g. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Crouse-Artus M, Lipschitz D, Krystal JH, Gelernter J. Genetic and environmental predictors of early alcohol use. Biol Psychiatry. 2007;61:1228–1234. doi: 10.1016/j.biopsych.2006.06.039. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Sakeim HA, Mann JJ. Correlates of trait impulsiveness in performance measures and neuropsychological tests. Psychiatry Res. 2005;135:191–201. doi: 10.1016/j.psychres.2005.03.006. [DOI] [PubMed] [Google Scholar]
- King KM, Molina BS, Chassin L. Prospective relations between growth in drinking and familial stressors across adolescence. J Abnorm Psychol. 2009;118:610–622. doi: 10.1037/a0016315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lane SD, Moeller FG, Steinberg JL, Buzby M, Kosten TR. Performance of cocaine dependent individuals and controls on a response inhibition task with varying levels of difficulty. Am J Drug Alcohol Abuse. 2007;33:717–726. doi: 10.1080/00952990701522724. [DOI] [PubMed] [Google Scholar]
- Laucht M, Treutlein J, Schmid B, Blomeyer D, Becker K, Buchmann AF, Schmidt MH, Esser G, Jennen-Steinmetz C, Rietschel M, Zimmermann US, Banaschewski T. Impact of psychosocial adversity on alcohol intake in young adults: moderation by the LL genotype of the serotonin transporter polymorphism. Biol Psychiatry. 2009;15:66. doi: 10.1016/j.biopsych.2009.02.010. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Bornovalova MA, Reynolds EK, Daughters SB, Curtin JJ. Risk factors in the relationship between gender and crack/cocaine. Exp Clin Psychopharmacol. 2007;15:165–175. doi: 10.1037/1064-1297.15.2.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd DA, Turner RJ. Cumulative lifetime adversities and alcohol dependence in adolescence and young adulthood. Drug Alcohol Depend. 2008;93:217–226. doi: 10.1016/j.drugalcdep.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas LR, Celen Z, Tamashiro KL, Blanchard RJ, Blanchard DC, Markham C, Sakai RR, McEwen BS. Repeated exposure to social stress has long-term effects on indirect markers of dopaminergic activity in brain regions associated with motivated behavior. Neuroscience. 2004;124:449–457. doi: 10.1016/j.neuroscience.2003.12.009. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. Guilford Press; New York: 1985. [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. Review. [DOI] [PubMed] [Google Scholar]
- McFarlane AC. Epidemiological evidence about the relationship between PTSD and alcohol abuse: the nature of the association. Addict Behav. 1998;23:813–825. doi: 10.1016/s0306-4603(98)00098-7. [DOI] [PubMed] [Google Scholar]
- Mischel W, Shoda Y, Rodriguez MI. Delay of gratification in children. Science. 1989;244:933–938. doi: 10.1126/science.2658056. Review. [DOI] [PubMed] [Google Scholar]
- Muraven M, Baumeister RF. Self-regulation and depletion of limited resources: does self-control resemble a muscle? Psychol Bull. 2000;126:247–259. doi: 10.1037/0033-2909.126.2.247. Review. [DOI] [PubMed] [Google Scholar]
- Nasser JA, Gluck ME, Geliebter A. Impulsivity and test meal intake in obese binge eating women. Appetite. 2004;43:303–307. doi: 10.1016/j.appet.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Olmstead MC. Animal models of drug addiction: where do we go from here? Q J Exp Psychol. 2006;59:625–653. doi: 10.1080/17470210500356308. [DOI] [PubMed] [Google Scholar]
- Olsson CA, Byrnes GB, Lotfi-Miri M, Collins V, Williamson R, Patton C, Anney RJ. Association between 5-HTTLPR genotypes and persisting patterns of anxiety and alcohol use: results from a 10-year longitudinal study of adolescent mental health. Mol Psychiatry. 2005;10:868–876. doi: 10.1038/sj.mp.4001677. [DOI] [PubMed] [Google Scholar]
- Paaver M, Nordquist N, Parik J, Harro M, Oreland L, Harro J. Platelet MAO activity and the 5-HTT gene promoter polymorphism are associated with impulsivity and cognitive style in visual information processing. Psychopharmacology (Berl) 2007;194:545–554. doi: 10.1007/s00213-007-0867-z. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;6:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Perkins HW. Stress-motivated drinking in collegiate and postcollegiate young adulthood: life course and gender patterns. J Stud Alcohol. 1999;60:219– 227. doi: 10.15288/jsa.1999.60.219. [DOI] [PubMed] [Google Scholar]
- Perry JL, Carroll ME. The role of impulsive behavior in drug use. Psychopharmacology (Berl) 2008;200:1–26. doi: 10.1007/s00213-008-1173-0. Review. [DOI] [PubMed] [Google Scholar]
- Reed PL, Anthony JC, Breslau N. Incidence of drug problems in young adults exposed to trauma and posttraumatic stress disorder: do early life experiences and predispositions matter? Arch Gen Psychiatry. 2007;64:1435– 1442. doi: 10.1001/archpsyc.64.12.1435. [DOI] [PubMed] [Google Scholar]
- Reinert DF, Allen JP. The Alcohol Use Disorders Identification Test (AUDIT): a review of recent research. Alcohol Clin Exp Res. 2002;26:272–279. Review. [PubMed] [Google Scholar]
- Roy M, Kirschbaum C, Steptoe A. Intraindividual variation in recent stress exposure as a moderator of cortisol and testosterone levels. Ann Behav Med. 2003;26:194–200. doi: 10.1207/S15324796ABM2603_04. [DOI] [PubMed] [Google Scholar]
- Rubio G, Jiménez M, Rodríguez-Jiménez R, Martínez I, Iribarren MM, Jiménez-Arriero MA, Ponce G, Avila C. Varieties of impulsivity in males with alcohol dependence: the role of Cluster-B personality disorder. Alcohol Clin Exp Res. 2007;31:1826–1832. doi: 10.1111/j.1530-0277.2007.00506.x. [DOI] [PubMed] [Google Scholar]
- Rutledge PC, Sher KJ. Heavy drinking from the freshman year into early young adulthood: the roles of stress, tension-reduction drinking motives, gender and personality. J Stud Alcohol. 2001;62:457–466. doi: 10.15288/jsa.2001.62.457. [DOI] [PubMed] [Google Scholar]
- Sáez-Abad C, Bertolín-Guillén JM. Personality traits and disorders in pathological gamblers versus normal controls. J Addict Dis. 2008;27:33–40. doi: 10.1300/J069v27n01_04. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Green BL. Understanding relationships among trauma, post-tramatic stress disorder, and health outcomes. Adv Mind Body Med. 2004;20:18–29. Review. [PubMed] [Google Scholar]
- Shevlin M, Dorahy MJ, Adamson G. Trauma and psychosis: an analysis of the National Comorbidity Survey. Am J Psychiatry. 2007;164:166–169. doi: 10.1176/ajp.2007.164.1.166. [DOI] [PubMed] [Google Scholar]
- Simons JS. Differential prediction of alcohol use and problems: the role of biopsychological and social-environmental variables. Am J Drug Alcohol Abuse. 2003;29:861–879. doi: 10.1081/ada-120026265. [DOI] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl) 2001;158:343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105–130. doi: 10.1196/annals.1441.030. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinella M. Neurobehavioral correlates of impulsivity: evidence of prefrontal involvement. Int J Neurosci. 2004;114:95–104. doi: 10.1080/00207450490249347. [DOI] [PubMed] [Google Scholar]
- Spinella M. Normative data and a short form of the Barratt Impulsiveness Scale. Int J Neurosci. 2007;117:359–368. doi: 10.1080/00207450600588881. [DOI] [PubMed] [Google Scholar]
- Stanford MS, Mathias CW, Dougherty DM, Lake SL, Anderson NE, Patton JH. Fifty years of the Barratt Impulsiveness Scale: An update and review. Pers Individ Dif. 2009;47:385–395. [Google Scholar]
- Swann AC. Neuroreceptor mechanisms of aggression and its treatment. J Clin Psychiatry. 2003;64(Suppl 4):26–35. Review. [PubMed] [Google Scholar]
- Sysko R, Hildebrandt T. Cognitive-behavioural therapy for individuals with bulimia nervosa and a co-occurring substance use disorder. Eur Eat Disord Rev. 2009;17:89–100. doi: 10.1002/erv.906. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanskanen A, Hintikka J, Honkalampi K, Haatainen K, Koivumaa-Honkanen H, Viinamäki H. Impact of multiple traumatic experiences on the persistence of depressive symptoms–a population-based study. Nord J Psychiatry. 2004;58:459–464. doi: 10.1080/08039480410011687. [DOI] [PubMed] [Google Scholar]
- Tice DM, Bratslavsky E, Baumeister RF. Emotional distress regulation takes precedence over impulse control: if you feel bad, do it! J Pers Soc Psychol. 2001;80:53–67. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Cumulative adversity and drug dependence in young adults: racial/ethnic contrasts. Addiction. 2003;98:305–315. doi: 10.1046/j.1360-0443.2003.00312.x. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Wheaton B. In: Checklist measurement of stressful life events, in Measuring Stress. Cohen S, Kessler R, Underwood Gordon L, editors. Oxford University Press; New York: 1995. pp. 29–58. [Google Scholar]
- Wagner S, Baskaya O, Lieb K, Dahmen N, Tadić A. The 5-HTTLPR polymorphism modulates the association of serious life events (SLE) and impulsivity in patients with Borderline Personality Disorder. J Psychiatr Res. 2009;43:1067–1072. doi: 10.1016/j.jpsychires.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Waldrop AE, Ana EJ, Saladin ME, McRae AL, Brady KT. Differences in early onset alcohol use and heavy drinking among persons with childhood and adulthood trauma. Am J Addict. 2007;16:439–442. doi: 10.1080/10550490701643484. [DOI] [PubMed] [Google Scholar]
- Wills TA, Isasi CR, Mendoza D, Ainette MG. Self-control constructs related to measures of dietary intake and physical activity in adolescents. J Adolesc Health. 2007;41:551–558. doi: 10.1016/j.jadohealth.2007.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Yaeger AM. Stress and smoking in adolescence: a test of directional hypotheses. Health Psychol. 2002;21:122–130. [PubMed] [Google Scholar]
- Wills TA, Shiffman S. Coping and substance abuse: a conceptual framework. In: Shiffman S, Wills TA, editors. Coping and Substance Use. Academic Press; Orlando, FL: 1985. pp. 3–24. [Google Scholar]
- Wills TA, Walker C, Mendoza D, Ainette MG. Behavioral and emotional self-control: relations to substance use in samples of middle and high school students. Psychol Addict Behav. 2006;20:265–278. doi: 10.1037/0893-164X.20.3.265. [DOI] [PubMed] [Google Scholar]
- Wilson ST, Fertuck EA, Kwitel A, Stanley MC, Stanley B. Impulsivity, suicidality and alcohol use disorders in adolescents and young adults with borderline personality disorder. Int J Adolesc Med Health. 2006;18:189–196. doi: 10.1515/ijamh.2006.18.1.189. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addict Biol. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit H, Flory JD, Acheson A, McCloskey M, Manuck SB. IQ and nonplanning impulsivity are independently associated with delay discounting in middle-aged adults. Pers Individ Dif. 2007;42:111–121. [Google Scholar]
- World Health Organization. International Classification of Diseases, in Mental and Behavioural Disorders Due to Psychoactive Substance Use. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]