Abstract
Purpose
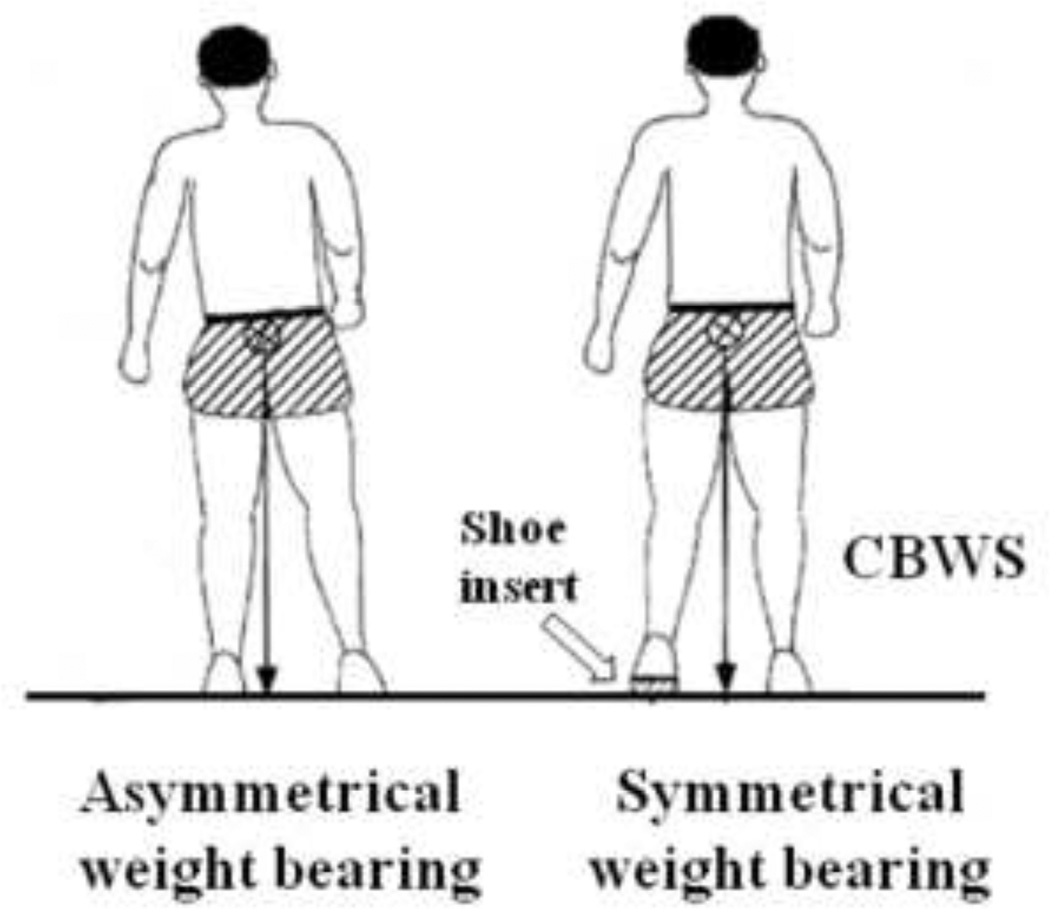
To evaluate the effectiveness of the Compelled Body Weight Shift (CBWS) therapy approach in the rehabilitation of individuals with chronic stroke. CBWS involves a forced shift of body weight towards a person’s affected side by means of a shoe insert that establishes a lift of the non-affected lower extremity.
Method
Eighteen individuals with chronic, unilateral stroke (mean age 57.7 ± 11.9 years, with a range of 35–75 years, mean time since stroke 6.7±3.9 years with a range of 1.1–14.1 years) who showed asymmetrical stance were randomly divided into two groups: the experimental group received a six-week physical therapy combined with CBWS therapy and the control group received only physical therapy. Both groups underwent a battery of identical tests (Fugl-Meyer assessment, Berg Balance Scale, weight bearing, and gait velocity) before the start of the rehabilitation intervention, following its completion, and three months after the end of therapy.
Results
After the intervention, weight bearing on the affected side (measured with the Balance Master®) increased in the experimental group to a larger degree compared to the control group (9.7% vs. 6.4%). Similarly, gait velocity increased 10.5% in the experimental group compared to the control group. Improvements in weight bearing and gait velocity were maintained in the experimental group after the three month retention period.
Conclusion
The study outcome revealed that a six-week intervention involving CBWS therapy could result in a long-lasting improvement of the symmetry of weight bearing and velocity of gait in individuals with chronic stroke.
Keywords: Stroke, weight bearing, rehabilitation, chronic
Introduction
Stroke is the leading cause of serious, long-term disability among adults. Annually, about 16 million first-ever strokes occur in the world, causing a total of 5.7 million deaths 1. In the United States, approximately 800,000 people sustain a stroke each year, and nearly 400,000 survive with some level of neurological impairment and disability 2. The estimated annual burden from stroke-related disability in US in 2007 was $40.9 billion 3.
It has previously been established that individuals with stroke-related hemiparesis frequently bear most of their body weight through their uninvolved lower extremity, showing distinct asymmetrical stance and weight bearing 4–7. Symmetrical stance and weight bearing has been recognized as a predictor of the ability to ambulate 8, 9, and it was shown that achieving symmetry of weight bearing is an important goal of rehabilitation and fall prevention 10.
Weight bearing asymmetry and impaired balance may be a consequence of a learned disuse of how to load the affected leg. For example, following a stroke, a person with hemiparesis may initially be unable or reluctant to bear weight through the affected limb due to significant paresis. Later, continued weight-bearing asymmetry may remain and foster further disuse, despite the probability that improved motor function in the lower limb has occurred. In this circumstance, it is tempting to apply the constraint-induced movement therapy approach (CIMT) (that allows reducing "learned disuse" of the affected extremity 11 and maximize neuroplasticity 12, 13) to normalize weight bearing over the impaired lower limb. However, CIMT, as it was initially designed, cannot be used in gait rehabilitation for individuals with hemiparesis because restraint of the intact lower extremity will not allow ambulation.
On the other hand, the outcome of a single-case study showed that the Compelled Body-Weight Shift (CBWS) therapy, which forces loading the affected limb during treatment and daily activities, could improve the symmetry of weight bearing and the velocity of gait in individuals with hemiparesis 14. The CBWS therapy, involves lifting the non-affected lower extremity through the use of a shoe insert over a period of several weeks (Fig. 1). During this time, more symmetrical weight bearing is facilitated while patients participate in physical therapy and regular daily activities. Moreover, it was recently shown that gait retraining in individuals with stroke provided with an insole wedge combined with the auditory feedback resulted in improved gait velocity as compared to control subjects 15. While the effect of forceful weight shift was documented, the study outcome did not distinguish between the effects of the insole wedge and the auditory feedback.
Fig. 1.
Schematic representation of a stroke-related asymmetry of stance and weight bearing in a person with right hemiplegia (left) and the role of the Compelled Body Weight Shift (CBWS) approach in restoring symmetry (right).
Moreover, little is known about whether the use of CBWS rehabilitation could be transferred to a long-lasting improvement of symmetry of stance and gait in individuals with hemiparesis. We hypothesized that rehabilitation utilizing the CBWS technique will result in the improvement of weight bearing symmetry and gait velocity. We also hypothesized that individuals treated using CBWS technique will retain improved symmetry of weight bearing and gait velocity three months after the completion of treatment.
Methods
Participants
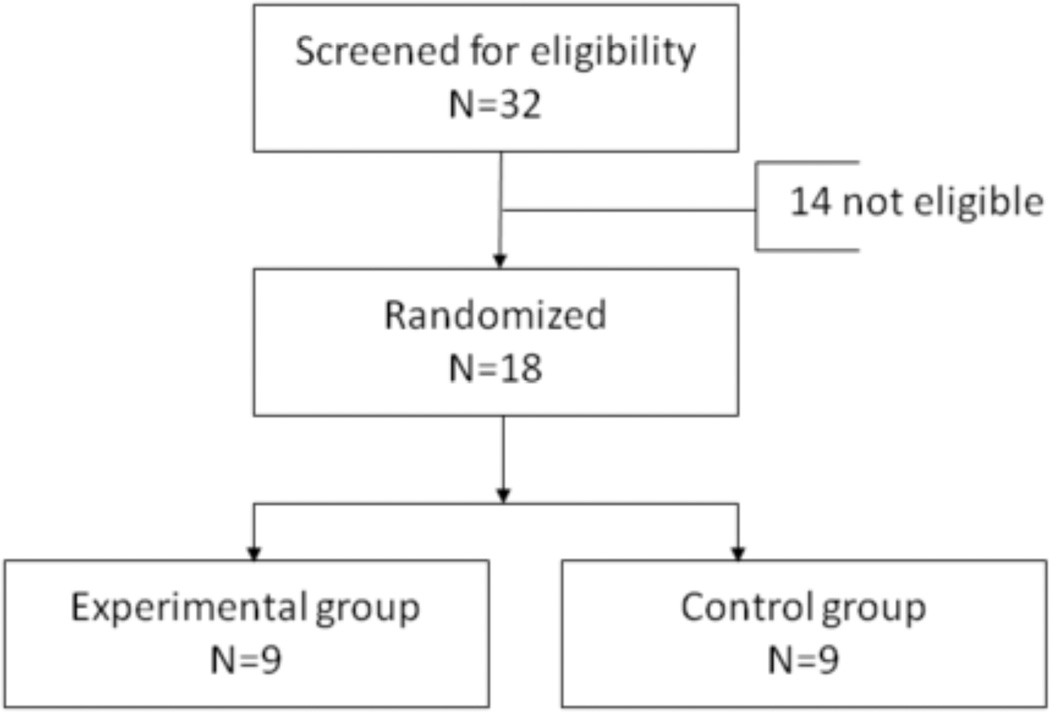
A convenience sample of thirty two individuals who sustained a stroke and who exhibited asymmetrical stance was recruited after being referred by their attending physicians and the treatment team (Fig. 2). Stroke diagnosis was established at the acute care hospital by attending neurologists based upon clinical presentation, neurological findings, and imaging studies. The inclusion criteria for the study were: unilateral chronic stroke with asymmetrical stance, ability to stand and walk with minimal assist and ability to understand and follow instructions. The exclusion criteria were: serious or unstable medical conditions, history of other neurological diseases (i.e. Parkinson’s disease, multiple sclerosis), fixed contractures or deformity, and leg length discrepancy. Based on the results of the weight bearing assessments, eighteen individuals with stroke (mean age 57.7 ± 11.9 years, with a range of 35–75 years, 14 males and 4 females) were selected to participate in the study. Nine patients had a right hemispheric lesion and nine patients had a lesion on the left side. The main time from the stroke onset was 6.7±3.9 years with a range of 1.1 to 14.1 years. By studying stroke patients who had a single insult more than one year ago, we tried to eliminate the possible confounding effect of spontaneous recovery: there are literature reports suggesting that a recovery plateau is reached by five months after insult 16, 17 and no additional motor recovery should be expected more than six to twelve months after the stroke occurs 18, 19. All of the subjects had a stroke more than one year ago and were ambulatory with assistive devices. The participants were randomly assigned to the experimental and control groups. The experimental group (5 right and 4 left CVAs) received CBWS therapy combined with physical therapy for a period of six weeks. The control group (4 right and 5 left CVAs) received only six weeks of physical therapy. The study protocol was approved by the Marianjoy Rehabilitation Hospital Institutional Review Board. Prior to giving written consent to participate, each subject was informed about the study procedures.
Fig. 2.
Flow diagram showing the assignment of subjects.
Procedure
Subjects included in the experimental group were provided with the 0.6 cm full-shoe insoles fabricated from medium hardness ethylene vinyl acetate covered with a layer of Poron®. No shoe lift was provided to the subjects included in the control group. Thus, to achieve the compelled body weight shift towards the affected side, each participant included in the experimental group wore the shoes with the installed innersole on the unaffected lower extremity during all daily activities throughout the duration of the six weeks training program. The selection of the six weeks was based on the outcome of our single case study that showed the effect compelled weight shift-based therapy on weight bearing and gait velocity14. The shoe lift was removed after the end of training. The subjects in both of the groups received a similar six weeks of physical therapy, ones a week for 60 minutes. The treatment focused on facilitating muscle strength, symmetrical weight bearing, and balance. Muscle strengthening activities included progressive resistance exercises with Thera-Band® resistive bands with up to 15 repetitions and NuStep® exercise machine. Weight bearing exercises involved a bathroom scale and were performed with the subject standing in such a way that his/her affected leg was on the platform of the scale while the unaffected leg was on a wooden block adjacent to the scale. The wooden block height, length, and width were similar to the dimensions of the scale. A bathroom scale and a mirror were used to provide feedback on weight bearing and posture to the patients. In addition, the patients practiced sit-to-stand and stand-to-sit maneuvers with emphasis on equal weight bearing on both the sides. Balance exercises included weight shifts on the affected side and pre-gait activities such as stepping forward, sideways, and stepping on a stool. Gait activities involved walking using the patient’s own assistive device. Both, the patients and their caregivers were trained on how to perform these exercises at home and were required to perform them daily for 60 minutes. Copies of all of the prescribed exercises were given to the patients and their caregivers, and they were required to provide a time log of their daily exercise activity at home. Each subject had a bathroom scale and a mirror at home and used them daily.
All participants undertook a battery of identical tests three times each, before the start of rehabilitation intervention, after its completion, and three months after the end of the intervention. The following tests were implemented.
Weight bearing on the affected side (WB) was assessed using the Balance Master computerized force platform system (Balance Master®, NeuroCom International, Clackamas, OR). This system consists of two force platforms connected to a personal computer allowing the independent measurement of vertical forces between the feet and surface of the platforms 20. The subjects stood on the two force platforms positioning their feet according to the manufacturer's protocol (each medial malleolus was aligned with the transverse force platform line, and the outside border of the heel was aligned with the height-appropriate line marked on the force platform). The percentage of the body weight carried by each lower extremity (WB) was calculated. The subjects were instructed to stand upright with their arms by their sides and to keep their eyes open while looking straight ahead. The WB was assessed three times and the measurements took two-to-three minutes.
Gait velocity was obtained by measuring the time of crossing a 10 meters distance while subjects walked over the linoleum floor in the hallway adjacent to the physical therapy gym. The mean of the three walking trials was obtained. The subjects used the same footwear and the same assistive devices during all three tests. No lift insert was used during any tests.
The level of motor recovery was assessed using the Fugl-Meyer Test (FMT) 21. Five domains of the Fugl-Meyer test for lower extremity (motor control, sensory function, balance, joint range of motion, and joint pain) were used for this study. A 3- point (0–2) scale was applied to each item in the evaluation, with the total possible score for the entire test being 100 points. This test has been shown to be valid and reliable for assessing recovery of function 22, 23, is correlated with the capacity to perform ADL activities 21, and is considered the gold standard for measuring motor recovery poststroke 24, 25.
To quantitatively assess balance, the Berg Balance Scale (BBS) was used. BBS assesses a subject’s performance on fourteen common items in everyday life. The items evaluate the ability to maintain positions of increasing difficulty by decreasing the base of support. Each item is graded on a 5-point scale, from 0 to 4; with the possible maximum total score being 56 26. This test has been shown to be correlated with other tests of mobility and balance, including the Tinetti Mobility Index and the Get Up and Go tests 27, and it is considered to be a valid and reliable tool 28.
Data Analysis
The values of the weight bearing (WB), gait velocity, FMT, and BBS scores were obtained for each subject during each of the three tests; for each test the group average values were calculated.
A repeated measures ANOVA was performed separately for these four measures, followed by the LCD post hoc analysis. Significance levels for multiple comparisons were adjusted with the Bonferroni corrections.
Results
No adverse effect of the treatment intervention was observed either in the experimental or control groups.
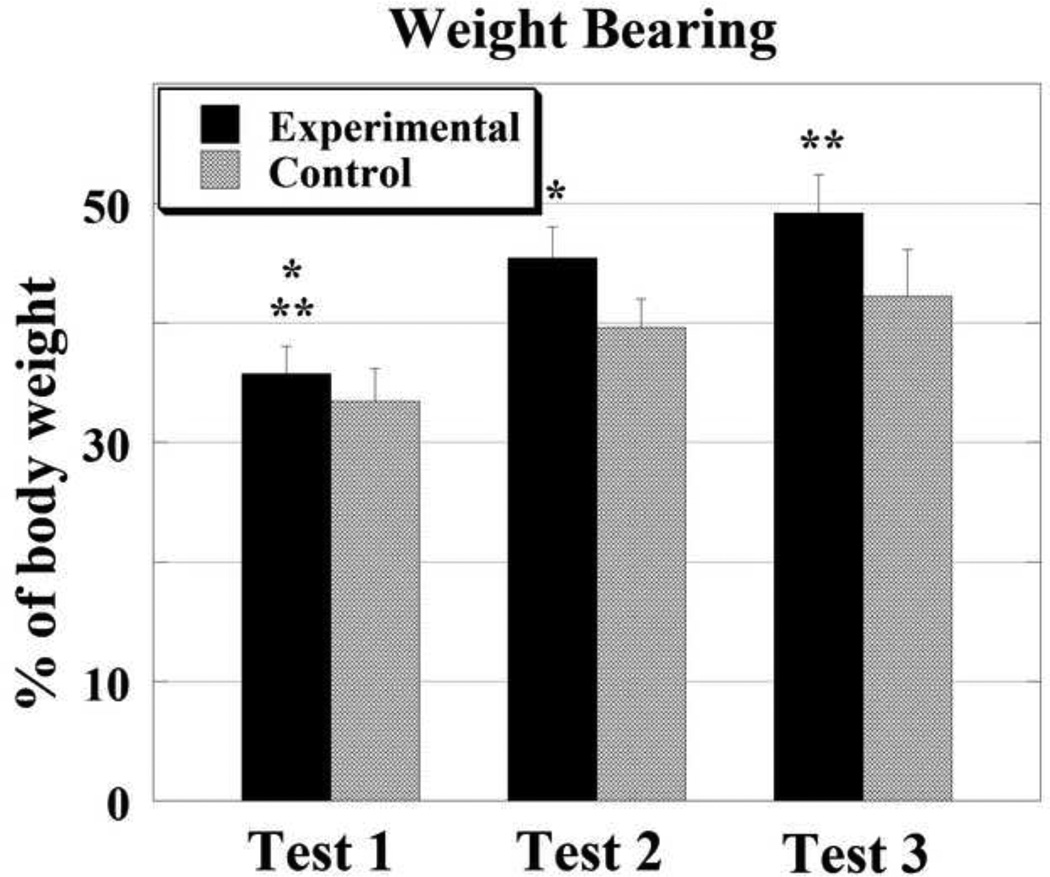
Weight bearing
The average of the three measurements of weight bearing on the affected side are shown in Fig. 3. All subjects demonstrated asymmetrical weight bearing at the time of the first test. Weight bearing on the affected side of the individuals included in the experimental group was 35.7±2.3 and it was 33.4±2.8 % of the body weight in the control group. The difference between the groups was not statistically significant. The average weight bearing on the affected side increased with the intervention in both of the groups. After completion of the six-week treatment, it reached 45.4±2.6 in the experimental group and 39.6±2.64 in the control group. Weight bearing continued to improve in the experimental group, during the retention period, reaching a normal weight distribution of 49.2±3.2 % of the body weight while it stayed almost the same in the control group (42.2.±3.9). ANOVA revealed the effect of the time of the test (p< 0.05) and the effect of the group was just under the level of statistical significance (p=0.07). Post hoc analysis uncovered that the changes in weight bearing measured during the three tests were statistically significant in the experimental group (p<0.01) while that was not the case for the control group (p=0.19).
Fig. 3.
Weight bearing measured on the affected side is shown with SE bars. The measurements were performed before the start of treatment (Test 1), after the treatment was completed (Test 2), and in 12 weeks after the end of treatment (Test 3). Weight bearing scale is in percent of the body weight. Asterisks indicate statistical significance (p<0.05).
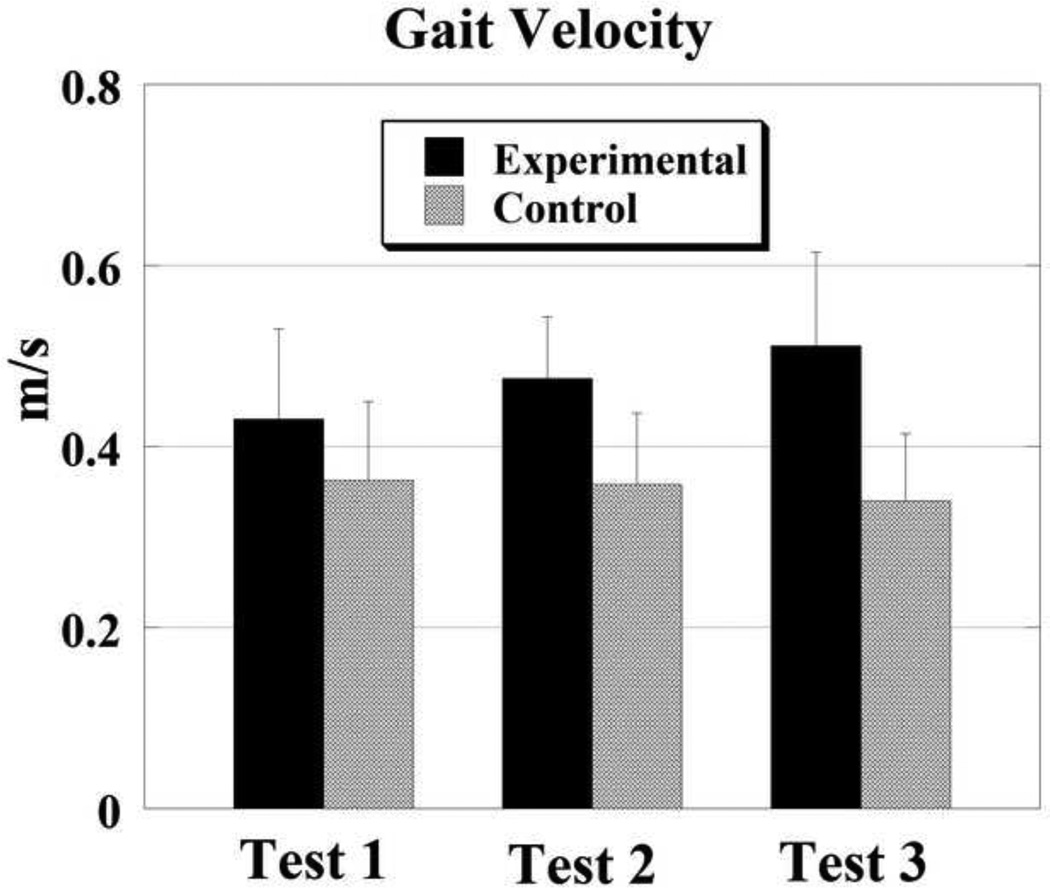
Gait velocity
The results of the measurements of gait velocity are shown in Fig. 4. Before the start of the treatment, individuals included in the experimental group and those included in the control group demonstrated gait velocity of 0.43±0.1 and 0.36±0.89 m/s respectively. The difference between the groups was not statistically significant (p=0.7). After treatment, gait velocity increased in the experimental group reaching 0.488±0.7 m/s and it did not change in the control group (0.36±0.8 m/s). The results of the third test revealed that gait velocity increased in the experimental group further reaching 0.51±0.10 m/s. At the same time, gait velocity decreased during the retention period in the control group to 0.34±0.7 m/s. ANOVA revealed no effect of groups or treatment.
Fig. 4.
Gait velocity prior to starting treatment (Test 1), immediately after the end of treatment (Test 2) and 12 weeks after treatment was finished (Test 3).
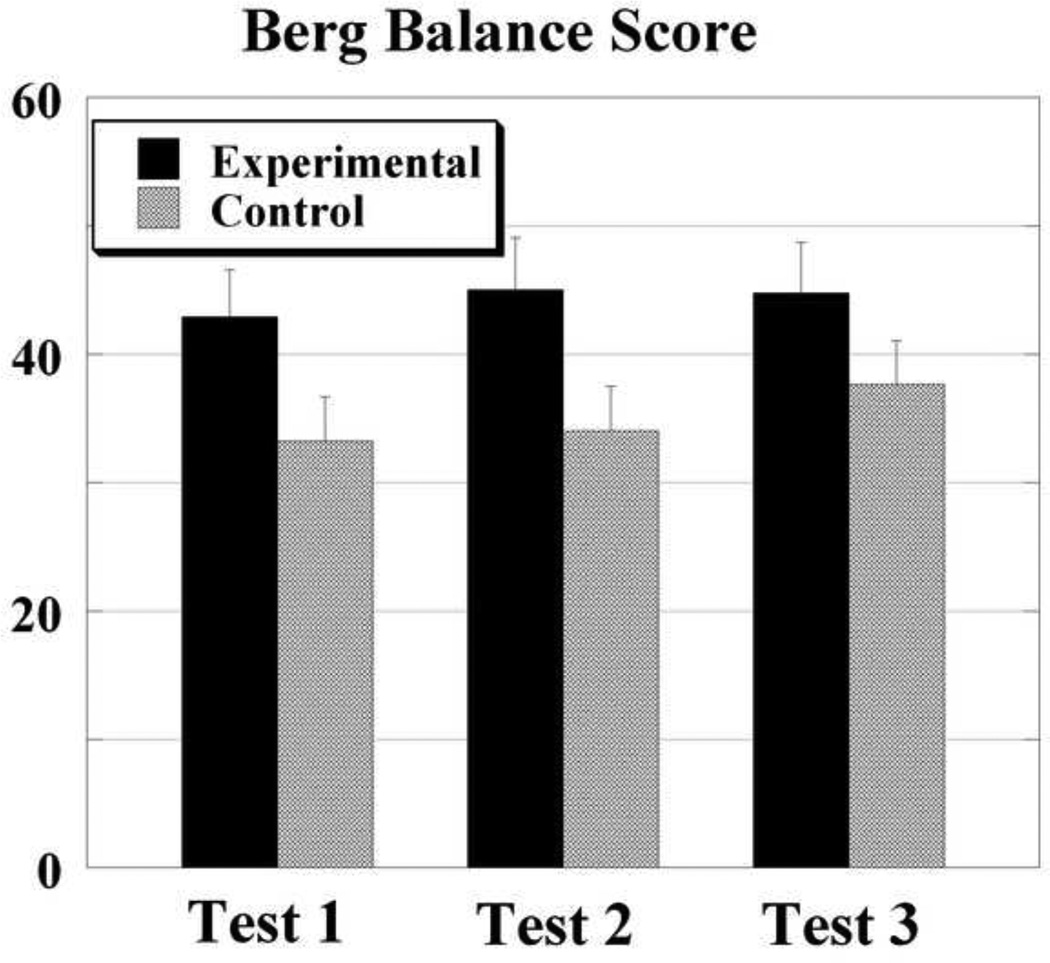
Berg Balance Test
The averaged results of the three Berg Balance test scores are shown in Fig. 5. Before the start of treatment, the BBS of the individuals included in the experimental group was 42.9±3.7 and it was 33.2±3.5 in the control group. The scores on the BBS increased with training in both groups of subjects. After completion of the six-week training program, it reached 45.0±4.1 in the experimental group and 34.0±3.5 in the control group. The score during the retention test was 44.8±4.0 in the experimental group and it was 37.7±3.4 in the control group. ANOVA revealed that the effect of the treatment was significant (p< 0.05) while the differences between the groups were just below the level of significance (p=0.08).
Fig. 5.
Averaged results of the Berg Balance test scores obtained prior to start of treatment (Test 1), immediately after the end of treatment (Test 2) and 12 weeks after treatment was finished (Test 3).
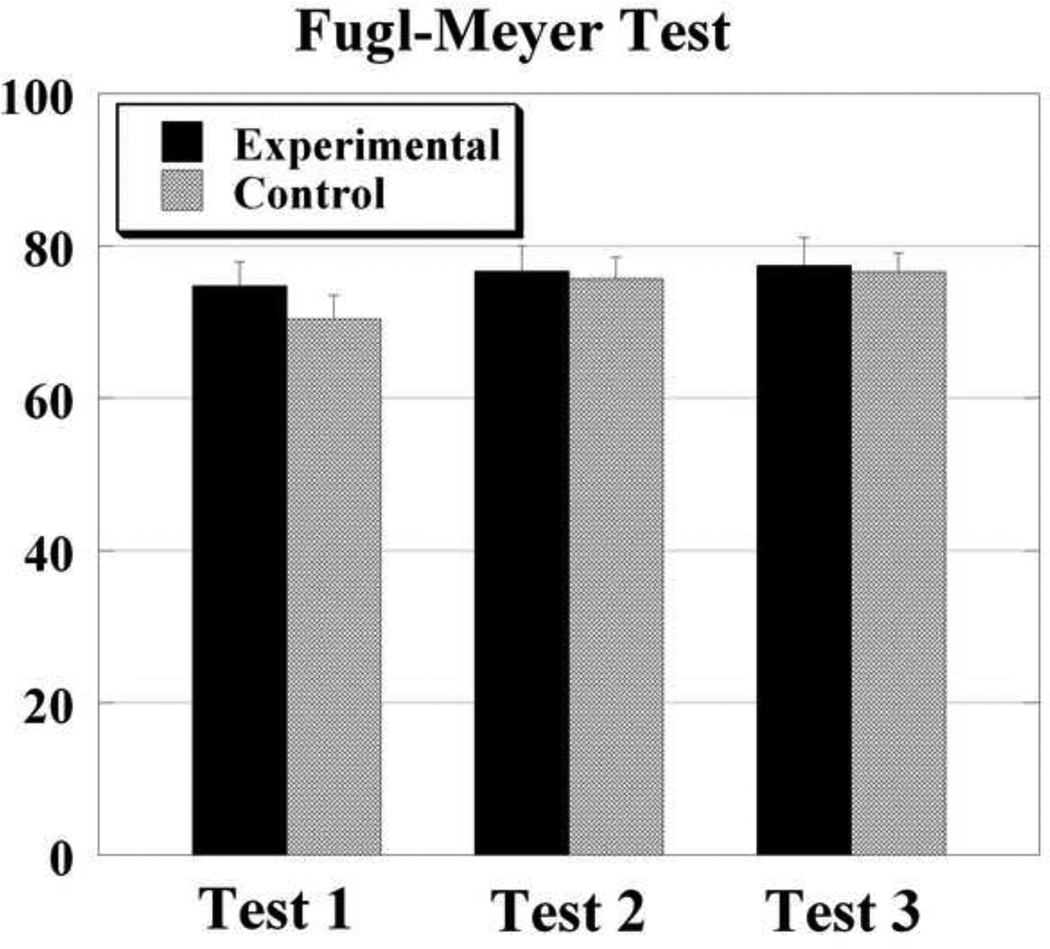
The Fugl-Meyer Test
The results of the assessment of motor recovery are shown in Fig. 6. Before the start of treatment, individuals included in the experimental group and those included in the control group demonstrated FMT scores of 74.7±3.1 and 70.4±3.1 respectively. The difference between the groups was not statistically significant (p=0.1). After treatment, FMT scores were 76.7±3.30 in the experimental and 75.7±2.9 in the control group. The results of the third FMT assessment revealed that the scores were preserved after the end of the retention period: 77.4±3.6 and 76.6±2.6 in the experimental and control groups respectively. ANOVA revealed that there was a significant effect of the treatment (p< 0.001) while the differences between the groups were not statistically significant (p=0.39).
Fig. 6.
The outcome of the Fugl-Meyer Test of motor recovery is shown for the three tests.
Discussion
The main finding in the current study was the improvement in the symmetry of weight bearing and clinically observed improvement in gait velocity when the subjects underwent treatment involving a CBWS approach, the compelled shift of body weight towards the subject’s affected side. The study outcome supports the first hypothesis that implementing a shoe lift on the unaffected side during rehabilitation improves the symmetry of weight bearing and gait velocity. The second hypothesis was also supported as the patients provided with the shoe lift maintained the improvement in symmetrical weight bearing and gait three months after the completion of the treatment.
1. The post-treatment effect of CBWS
Prior studies demonstrated that a lift to the non-affected side was associated with the immediate improvement in the symmetry of weight bearing in individuals with acute and chronic stroke 6, 14. Thus, it was reported that a 1.2 cm lift promoted improvement in weight bearing on the affected side from 39.9% to 47% 6 and from 38.8% to 48% 14. Moreover, a provision of a five degree wedge on the unaffected side resulted in restoring the symmetry of weight bearing in individuals with acute stroke 6. In addition, a 0.9 cm shoe lift on the non affected side improved static and dynamic postural control in individuals with acute stroke 29. The outcome of these studies however, did not provide information about whether or not the achieved improvement in weight bearing symmetry remains beyond one experimental session. It was shown in a single patient that prolonged use of the shoe lift was beneficial in the improvement of weight bearing symmetry and gait velocity 14.
The outcome of the current study extends previous findings to a group of individuals with chronic stroke who after six weeks of treatment involving CWBS improved their symmetry of weight bearing. It is important to note that the increase in weight bearing on the affected side was observed in the control group of subjects as well, however, the rate of the increase in weight bearing with treatment was much smaller in the control group. Thus, weight bearing increased in the experimental group by 27.2% compared to the pre-treatment level, while it increased in the control group only by 18.6%. Since control subjects were not provided with a lift insert and both groups participated in a similar treatment, the 8.6% difference in the improvement of the weight bearing on the affected side in the experimental group points to the effect of the lift insert.
There was a clinically observed 10.5% improvement in gait velocity following treatment in the experimental group whereas gait velocity in the control group decreased by 1.4%.This result contrasts with the previously published data on the lack of improvement of walking function after the re-training of symmetrical weight bearing using a feedback device 30. Our approach was different, as compelled weight bearing was achieved during the entire time of treatment, during all daily activities including ambulation. The clinically observed improvement in gait velocity suggests that the compelled shift of body weight had a positive effect on the ability of the patient to overcome the learned disuse of the affected leg. It is also important to mention that there was a difference in baseline gait velocity between the groups: the experimental group started out as "limited community ambulators" with gait speed of 0.43 m/s and the control group started out as "household ambulators" with gait speed of 0.36 m/s. Based on gait speed norms, neither group changed ambulation categories during treatment however, the experimental group achieved the minimal clinically important difference (MCID)31 by the end of the retention period.
2. The long-term effect of CBWS
The study outcome demonstrated that the improvement in bearing weight on the affected side was achieved as a result of the implementation of the CWBS therapy. Moreover, weight bearing symmetry continued to improve during the retention period: the weight bearing on the affected side in the experimental group increased by 8.4% while in the control group it increased only 6.5%. Gait velocity during the retention period increased in the experimental group by 7.6% while it decreased in the control group by 5.1%.
Improvement in the gait velocity observed in the experimental group could be explained by the fact that the subjects provided with the shoe insert were able to better utilize their paretic leg during the retention period and as a result demonstrated improvement in their gait velocity. This conclusion is supported by previous literature which stated that the improved ability to load the paretic limb, had resulted in the improved symmetry of stance 30 and the ability to rise from a chair in individuals with chronic stroke 32.
3. The effect of CWST on motor recovery and balance scores
While the improvements in the FMT and BBS test scores were seen in both subject groups, the effect of treatment was not statistically significant. Moreover, MCID for the FMT and BBS test scores was not met by either group. A possible explanation for the observed lack of effectiveness of the CWST on the improvement of the motor recovery and balance clinical test scores relates to the fact that all the study participants were in the chronic stage: the mean time from stroke onset was 6.7±3.9 years. It is known that subjects who are more than twelve months post stroke do not show improvement in motor recovery 19. Moreover, based on Copenhagen Stroke Study reports, motor recovery should not be expected more than five months after insult 16. Other studies provide a support to a conclusion that motor recovery should not be expected more than six to twelve months after injury 33.
4. Conclusion
The study outcome revealed that an intervention involving CBWS therapy could result in a long-lasting improvement of the symmetry of weight bearing and velocity of gait in individuals with chronic stroke. The study limitations include a relatively small number of individuals with chronic stroke and the use of one size of the shoe inserts. Future studies involving larger sample size are needed to investigate the effect of CBWS therapy in individuals with acute stroke and the effect of different thickness of the shoe insoles.
Acknowledgement
This work was supported by the NIH grant HD-50457. We would like to thank the patients for their exceptional cooperation.
Footnotes
No conflict of interests declared.
References
- 1.Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. 2007;6:182–187. doi: 10.1016/S1474-4422(07)70031-5. [DOI] [PubMed] [Google Scholar]
- 2.Kelly-Hayes M, Robertson JT, Broderick JP, et al. The American Heart Association Stroke Outcome Classification. Stroke. 1998;29:1274–1280. doi: 10.1161/01.str.29.6.1274. [DOI] [PubMed] [Google Scholar]
- 3.Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics--2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bohannon RW, Larkin PA. Lower extremity weight bearing under various standing conditions in independently ambulatory patients with hemiparesis. Physical therapy. 1985;65:1323–1325. doi: 10.1093/ptj/65.9.1323. [DOI] [PubMed] [Google Scholar]
- 5.Eng JJ, Chu KS. Reliability and comparison of weight-bearing ability during standing tasks for individuals with chronic stroke. Archives of physical medicine and rehabilitation. 2002;83:1138–1144. doi: 10.1053/apmr.2002.33644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rodriguez GM, Aruin AS. The effect of shoe wedges and lifts on symmetry of stance and weight bearing in hemiparetic individuals. Archives of physical medicine and rehabilitation. 2002;83:478–482. doi: 10.1053/apmr.2002.31197. [DOI] [PubMed] [Google Scholar]
- 7.Tessem S, Hagstrom N, Fallang B. Weight distribution in standing and sitting positions, and weight transfer during reaching tasks, in seated stroke subjects and healthy subjects. Physiother Res Int. 2007;12:82–94. doi: 10.1002/pri.362. [DOI] [PubMed] [Google Scholar]
- 8.Nichols DS. Balance retraining after stroke using force platform biofeedback. Physical therapy. 1997;77:553–558. doi: 10.1093/ptj/77.5.553. [DOI] [PubMed] [Google Scholar]
- 9.Walker C, Brouwer BJ, Culham EG. Use of visual feedback in retraining balance following acute stroke. Physical therapy. 2000;80:886–895. [PubMed] [Google Scholar]
- 10.Sackley CM. Falls, sway, and symmetry of weight-bearing after stroke. International disability studies. 1991;13:1–4. doi: 10.3109/03790799109166267. [DOI] [PubMed] [Google Scholar]
- 11.Taub E, Uswatte G, Pidikiti R. Constraint-Induced Movement Therapy: a new family of techniques with broad application to physical rehabilitation--a clinical review. J Rehabil Res Dev. 1999;36:237–251. [PubMed] [Google Scholar]
- 12.Dancause N, Nudo RJ. Shaping plasticity to enhance recovery after injury. Progress in brain research. 2011;192:273–295. doi: 10.1016/B978-0-444-53355-5.00015-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nudo RJ. Adaptive plasticity in motor cortex: implications for rehabilitation after brain injury. J Rehabil Med. 2003:7–10. doi: 10.1080/16501960310010070. [DOI] [PubMed] [Google Scholar]
- 14.Aruin AS, Hanke T, Chaudhuri G, Harvey R, Rao N. Compelled weightbearing in persons with hemiparesis following stroke: the effect of a lift insert and goal-directed balance exercise. Journal of rehabilitation research and development. 2000;37:65–72. [PubMed] [Google Scholar]
- 15.Sungkarat S, Fisher BE, Kovindha A. Efficacy of an insole shoe wedge and augmented pressure sensor for gait training in individuals with stroke: a randomized controlled trial. Clin Rehabil. 2011;25:360–369. doi: 10.1177/0269215510386125. [DOI] [PubMed] [Google Scholar]
- 16.Jorgensen HS, Nakayama H, Raaschou HO, Vive-Larsen J, Stoier M, Olsen TS. Outcome and time course of recovery in stroke. Part II: Time course of recovery. The Copenhagen Stroke Study. Arch Phys Med Rehabil. 1995;76:406–412. doi: 10.1016/s0003-9993(95)80568-0. [DOI] [PubMed] [Google Scholar]
- 17.Parker VM, Wade DT, Langton Hewer R. Loss of arm function after stroke: measurement, frequency, and recovery. Int Rehabil Med. 1986;8:69–73. doi: 10.3109/03790798609166178. [DOI] [PubMed] [Google Scholar]
- 18.DeLisa J, Gans B, Bockeneck W. Rehabilitation medicine: principle and practice. Philadelphia: Lippincott, Williams & Wilkins; 1999. Ch. 77. [Google Scholar]
- 19.Newman M. The process of recovery after hemiplegia. Stroke. 1972;3:702–710. doi: 10.1161/01.str.3.6.702. [DOI] [PubMed] [Google Scholar]
- 20.Liston RA, Brouwer BJ. Reliability and validity of measures obtained from stroke patients using the Balance Master. Arch Phys Med Rehabil. 1996;77:425–430. doi: 10.1016/s0003-9993(96)90028-3. [DOI] [PubMed] [Google Scholar]
- 21.Fugl-Meyer AR, Jaasko L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7:13–31. [PubMed] [Google Scholar]
- 22.Duncan PW, Propst M, Nelson SG. Reliability of the Fugl-Meyer assessment of sensorimotor recovery following cerebrovascular accident. Phys Ther. 1983;63:1606–1610. doi: 10.1093/ptj/63.10.1606. [DOI] [PubMed] [Google Scholar]
- 23.Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Phys Ther. 1993;73:447–454. doi: 10.1093/ptj/73.7.447. [DOI] [PubMed] [Google Scholar]
- 24.Gresham G, Duncan P, Stason W, et al. Guideline Report. Rockville, MD: U.S. Department of Health and Human Services. Agency for Health Care Policy and Research; 1995. Post-Stroke Rehabilitation. [Google Scholar]
- 25.Gladstone DJ, Danells CJ, Black SE. The fugl-meyer assessment of motor recovery after stroke: a critical review of its measurement properties. Neurorehabil Neural Repair. 2002;16:232–240. doi: 10.1177/154596802401105171. [DOI] [PubMed] [Google Scholar]
- 26.Berg K, Wood-Dauphinee S, Williams JI. The Balance Scale: reliability assessment with elderly residents and patients with an acute stroke. Scand J Rehabil Med. 1995;27:27–36. [PubMed] [Google Scholar]
- 27.Berg KO, Wood-Dauphinee SL, Williams JI, Maki B. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–S11. [PubMed] [Google Scholar]
- 28.Shumway-Cook A, Baldwin M, Polissar NL, Gruber W. Predicting the probability for falls in community-dwelling older adults. Phys Ther. 1997;77:812–819. doi: 10.1093/ptj/77.8.812. [DOI] [PubMed] [Google Scholar]
- 29.Chaudhuri S, Aruin AS. The effect of shoe lifts on static and dynamic postural control in individuals with hemiparesis. Arch Phys Med Rehabil. 2000;81:1498–1503. doi: 10.1053/apmr.2000.17827. [DOI] [PubMed] [Google Scholar]
- 30.Winstein CJ, Gardner ER, McNeal DR, Barto PS, Nicholson DE. Standing balance training: effect on balance and locomotion in hemiparetic adults. Archives of physical medicine and rehabilitation. 1989;70:755–762. [PubMed] [Google Scholar]
- 31.Baker R, McGinley JL, Schwartz M, Thomason P, Rodda J, Graham HK. The minimal clinically important difference for the Gait Profile Score. Gait & posture. 2012 doi: 10.1016/j.gaitpost.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 32.Lomaglio MJ, Eng JJ. Muscle strength and weight-bearing symmetry relate to sit-to-stand performance in individuals with stroke. Gait Posture. 2005;22:126–131. doi: 10.1016/j.gaitpost.2004.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Page SJ, Gater DR, Bach YRP. Reconsidering the motor recovery plateau in stroke rehabilitation. Arch Phys Med Rehabil. 2004;85:1377–1381. doi: 10.1016/j.apmr.2003.12.031. [DOI] [PubMed] [Google Scholar]