Abstract
Objectives
The aim was to examine the independent and joint associations of sitting time and physical activity with risk of incident cardiovascular disease (CVD).
Background
Sedentary behavior is recognized as a distinct construct beyond lack of leisure-time physical activity, but limited data exists on the interrelationship between these two components of energy balance.
Methods
Participants in the prospective Women’s Health Initiative Observational Study (N = 71,018), aged 50–79 and free of CVD at baseline (1993–1998), provided information on sedentary behavior, defined as hours of sitting per day, and usual physical activity at baseline and during follow-up through September 2010. First CVD (coronary heart disease or stroke) events were centrally adjudicated.
Results
Sitting ≥ 10 hours/day compared to ≤ 5 hours/day was associated with increased CVD risk (HR=1.18, 95% CI 1.09, 1.29) in multivariable models including physical activity. Low physical activity was also associated with higher CVD risk (P, trend <0.001). When women were cross-classified by sitting time and physical activity (P, interaction = 0.94), CVD risk was highest in inactive women (≤1.7 MET-hrs/week) who also reported ≥10 hrs/day of sitting. Results were similar for CHD and stroke when examined separately. Associations between prolonged sitting and risk of CVD were stronger in overweight versus normal weight women and women aged 70 years and older compared to younger women.
Conclusions
Prolonged sitting time was associated with increased CVD risk, independent of leisure-time physical activity, in postmenopausal women without a history of CVD. A combination of low physical activity and prolonged sitting augments CVD risk.
Keywords: cardiovascular disease, women, physical activity, sedentary behavior
INTRODUCTION
Lack of leisure-time physical activity is a major risk factor for coronary heart disease (CHD), stroke, and increased cardiovascular mortality (1 – 4). Humans are spending increasingly more time in sedentary behaviors and this global trend is likely to continue, given the increasing availability and popularity of personal computers and television, automation of chores at home, increase in sedentary occupations, and transportation trends (5 – 6). Time spent in sedentary behavior displaces time spent in higher-intensity activities, for example activities of daily living, contributing to an overall reduction in total energy expenditure (7).
Emerging evidence suggests that sedentary behavior has independent effects on human metabolism, physical function, and potentially on health outcomes from low leisure-time physical activity. Sedentary behavior defined in various ways (e.g. sitting, T.V. watching, energy expenditure of 1.0–1.5 METs) has been associated with increased risk of obesity, metabolic syndrome, type 2 diabetes and cardiovascular disease (CVD) mortality, suggesting that it be treated as a construct distinct from physical activity (8 – 9). Thus, even among individuals who meet current physical activity guidelines, excessive sedentary behavior may have adverse metabolic and prognostic implications, particularly in older adults (10).
Sitting, a unique aspect of human behavior, may not simply represent the extreme low end of the physical activity continuum (7). We previously reported that both low levels of recreational physical activity and higher sitting time were associated with elevated CVD risk in the Women’s Health Initiative Observational Study (WHI-OS) (4). However, the independent and joint associations of sedentary time and physical activity with CVD events were not reported. We now extend follow-up of the cohort for an additional 10 years, update sitting and activity variables during follow-up, and examine the interrelationship of sitting time and physical activity in detail. Thus, the purpose of this study was to examine the independent and joint associations of sedentary time and physical activity with risk of incident CVD in older women. Given the limited data available on this subject, the WHI-OS affords an excellent opportunity to elucidate the complex interplay of these two separate components of energy balance.
METHODS
Study Population
The multiethnic Women’s Health Initiative Observational Study (WHI-OS) cohort of 93,676 postmenopausal women, aged 50 – 79 years at study entry, was enrolled between 1994 and 1998 across 40 U.S. clinical centers. Details of the scientific rationale, study design, eligibility requirements, and baseline characteristics of the cohort have been previously published (11). Exclusion criteria included the presence of any medical condition associated with predicted survival of less than three years (e.g., class IV congestive heart failure, obstructive lung disease requiring supplemental oxygen, or severe chronic liver or kidney disease), alcoholism, mental illness, or dementia. Additional exclusions for the current analysis included history of CVD or cancer at baseline; reporting an inability to walk at least one block; or missing sedentary time or physical activity data, leaving 71,018 women for these analyses.
Exposure Assessment
Each WHI-OS participant had a baseline clinic visit at which she completed self-administered questionnaires related to medical history, physical activity, smoking, diet, and other lifestyle-related factors and had her height, weight, waist and hip circumferences, and blood pressure measured. Additionally, participants completed periodic health forms and repeated baseline clinic assessments three years after enrollment. All women provided written informed consent, and the study protocol was approved by the institutional review board of each center.
Sedentary behavior was assessed by questionnaire at baseline and twice during follow-up using the following question: “During a usual day and night, about how many hours do you spend sitting? Be sure to include the time you spend sitting at work, sitting at the table eating, driving or riding a car or bus, and sitting up watching TV or talking.” Eight categories were provided for the response, ranging from less than 4 hours per day to 16 or more hours per day.
Leisure-time physical activity was assessed at baseline and during follow-up by a detailed questionnaire on walking, including the frequency of walks outside the home, average duration, and pace of each walk, and other types of activity (strenuous, moderate, and mild), including the frequency (days per week) and duration of each type. Examples of strenuous activities, defined as activities that result in increased heart rate and sweating, were aerobics, aerobic dancing, jogging, tennis, and swimming laps. Examples of moderate activity included biking outdoors, using an exercise machine (such as a stationary bicycle or a treadmill), calisthenics, easy swimming, and popular or folk dancing. Examples of mild exercise were slow dancing, bowling, and golf. Each type of activity was assigned a metabolic equivalent task (MET) score based on its energy cost (12) and physical activity-related energy expenditure (MET-hr/wk) was computed as the summed product of frequency, duration, and intensity.
Ascertainment of End Points
The primary endpoints for this analysis were incident coronary heart disease (CHD), including nonfatal myocardial infarction (MI) and fatal CHD, and stroke. These endpoints were also combined to examine the associations of sedentary behavior and physical activity with incident CVD. Outcomes were identified on the basis of annual mailed questionnaires (response rates > 95%), with permission to obtain and review medical records. Physicians blinded to exposure data confirmed self-reported diagnoses.
Nonfatal MI was confirmed according to standardized criteria of diagnostic ECG changes, elevated cardiac enzymes, or both (13). Stroke was confirmed by diagnosis of a typical neurological defect of sudden or rapid onset lasting ≥ 24 hours or until death attributed to a cerebrovascular event. Fatal CHD was confirmed by documentation in hospital or autopsy records or if coronary disease was listed as the cause of death on death certificates and evidence of previous coronary disease was available.
Statistical Analysis
All analyses were performed using SAS statistical software, version 9.3 (SAS Institute Inc, Cary, North Carolina). Eligible participants contributed person-time from return of baseline questionnaires to the first diagnosis of CVD, death from any cause, loss to follow-up, or September 2010.
Baseline descriptive characteristics were compared according to categories of sitting time and physical activity using linear models. For each baseline covariate, medians of sitting time or physical activity categories were modeled as a function of the covariate of interest, adjusted for age, with the P-value from the resulting type 3 test used to determine statistical significance for the covariate presented.
Cox proportional hazards models were used to estimate hazards ratios (HR) and 95% confidence intervals (CI) for outcomes. Given the strong association between age and CVD, all models were stratified on age in years using the STRATA statement for PHREG in SAS. Tests for linear trend were computed by using the medians for categories modeled as an ordinal variable. Statistical significance was defined as p < 0.05. The possibility of non-linear relations between sitting time, physical activity, and CVD were examined non-parametrically with restricted cubic splines (14). Tests for non-linearity used the likelihood ratio test, comparing the model with only the linear term to the model with linear and cubic spline terms.
To assess independent associations of sitting time and physical activity with CVD risk, both exposures were included simultaneously in the model. Simple updated levels of sitting time and physical activity, in which outcomes were predicted from the most recent questionnaire, were used. For example, events that occurred between baseline and year 3 of follow-up were examined in relation to exposures reported on the baseline questionnaire, events occurring between year 3 and year 6 of follow-up were examined in relation to exposures reported on the year 3 questionnaire, and so forth. Sitting time and physical activity were first examined as categorical variables and then as a continuous variables to show the impact on outcomes per 1-unit increment of each exposure. Sitting was categorized as ≤ 5, 5.1–9.9, and ≥ 10 hours per day, which were approximate tertiles based on distribution of the data. For physical activity, women were classified into four categories: inactive (≤ 1.7 MET-hrs/wk), low (1.8 – 8.3 MET-hrs/wk), medium (8.4 – 20 MET-hrs/wk), and high activity (> 20 MET-hrs/wk), with accumulating 150 min/week of moderate-intensity exercise, i.e. the minimum dose of activity recommended by the federal government (15), being equivalent to at least 8.4 MET-hrs/wk of exercise. To assess the joint association of sitting time and physical activity with risk of CVD, participants were cross-classified into 12 groups according to the levels of sitting time and physical activity. The interaction was assessed by the difference in −2 log likelihood between the model containing the cross-classified sitting time-physical activity variables and the main effects model.
All multivariable models were stratified by age in years and included the following covariates: race/ethnic group, family income, education, marital status, smoking, parental history of premature MI, depression, alcohol intake, hours of sleep, intake of total calories, saturated fat, and fiber. Covariates that were reassessed during follow-up were updated over time using the most recent value. Secondary analyses were additionally adjusted for history of hypertension, diabetes, high cholesterol levels, and body mass index (BMI).
Whether associations between sedentary time and CVD were modified by BMI (< 25 vs. ≥ 25 kg/m2), age (< 70 vs. ≥ 70 years), or employment status (employed vs. unemployed) was also examined. Interactions were tested by examining the difference in −2 log likelihood between the model containing interactions with the potential effect modifiers and the main effects model.
As a secondary analysis, the association between change in sitting time and CVD risk was examined. Change in sitting time between baseline and year 3 was used to examine events that occurred between year 3 and year 6 of follow-up; change in sitting time between year 3 and year 6 was used to examine events that occurred from year 6 on. Change in sitting time was examined as a continuous variable and using the following categories: decreased sitting by more than 2 hours/day, no change, and increased sitting by more than 2 hours/day.
RESULTS
During a median follow-up of 12.2 years (interquartile range: 8.7 – 14.0 years), 2411 incident cases of CHD, 2050 incident strokes, and 4235 first CVD events were documented. Baseline sitting time and physical activity in relation to other potential risk factors for CVD are presented in Table 1. Women who reported ≥ 10 hours/day of sitting were more likely to be White, to have attended college, and to have a higher income compared to women who reported ≤ 5 hours/day of sitting; whereas, the opposite was true of women reporting less physical activity compared to highly active women. Additionally, greater time spent sitting and less physical activity were positively associated with current smoking, higher BMI, and self-reported depression (Table 1).
Table 1.
Age-standardized baseline characteristics* of participants in the Women’s Health Initiative Observational Study according to categories of sitting time and physical activity.
| Sitting Time (hrs/day) | Physical Activity (MET-hrs/week) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| ≤ 5 | 5.1 – 9.9 | ≥10 | P-value | High (> 20) | Medium (8.4 – 20) | Low (1.8 – 8.3) | Inactive (≤ 1.7) | P-value | |
| N | 24,691 | 28,953 | 17,374 | 18,205 | 21,653 | 18,299 | 12,861 | ||
|
| |||||||||
| Age, years | 63.8 (7.1) | 63.7 (7.2) | 60.9 (7.2) | <.001 | 62.8 (7.2) | 63.2 (7.2) | 63.2 (7.3) | 62.7 (7.4) | 0.09 |
| Sitting time, hrs/day | 3.7 (1.2) | 7.4 (1.0) | 11.9 (1.7) | ------ | 6.5 (3.1) | 7.2 (3.2) | 7.5 (3.4) | 7.8 (3.6) | <.001 |
| Physical activity, MET-hrs/wk | 16.4 (16.4) | 14.1 (14.0) | 11.1 (12.0) | <.001 | 33.9 (14.1) | 13.6 (3.3) | 4.9 (1.9) | 0.3 (0.5) | ------ |
| Race/Ethnicity, % | <.001 | <.001 | |||||||
| White | 80 | 86 | 85 | 87 | 86 | 82 | 78 | ||
| African American | 9 | 7 | 7 | 6 | 6 | 8 | 11 | ||
| Hispanic/Latino | 6 | 3 | 2 | 3 | 3 | 4 | 5 | ||
| Other | 5 | 5 | 5 | 5 | 4 | 5 | 5 | ||
| Smoking Status, % | <.001 | <.001 | |||||||
| Current | 6 | 6 | 7 | 4 | 5 | 7 | 10 | ||
| Former | 40 | 42 | 45 | 47 | 43 | 39 | 38 | ||
| Never | 54 | 52 | 48 | 49 | 52 | 54 | 53 | ||
| Marital Status, % | <.001 | <.001 | |||||||
| Married | 68 | 65 | 55 | 66 | 65 | 62 | 61 | ||
| Single, Divorced, Widowed | 32 | 35 | 45 | 33.4 | 35.0 | 38 | 39 | ||
| Education Level, % | <.001 | <.001 | |||||||
| High school or less | 24 | 19 | 17 | 14 | 17 | 23 | 30 | ||
| Vocational training | 11 | 9 | 8 | 8 | 9 | 10 | 11 | ||
| College | 65 | 72 | 75 | 78 | 74 | 67 | 59 | ||
| Income, % | <.001 | <.001 | |||||||
| <$20,000 | 17 | 13 | 12 | 10 | 12 | 16 | 20 | ||
| $20,000–$74,999 | 62 | 64 | 65 | 61 | 64 | 66 | 65 | ||
| ≥$75,000 | 21 | 22 | 22 | 29 | 24 | 18 | 15 | ||
| Body Mass Index (kg/m2) | 26.5 (5.3) | 27.0 (5.6) | 27.7 (6.2) | <.001 | 25.4 (4.7) | 26.4 (5.2) | 27.7 (5.9) | 29.2 (6.6) | <.001 |
| Waist-to-Hip Ratio | 0.80 (0.08) | 0.80 (0.08) | 0.81 (0.08) | <.001 | 0.79 (0.08) | 0.80 (0.08) | 0.81 (0.08) | 0.82 (0.08) | <.001 |
| Family history of MI, % | 40 | 42 | 43 | <.001 | 41 | 42 | 42 | 40 | 0.91 |
| Hours of sleep | 6.9 (1.1) | 6.9 (1.1) | 6.8 (1.1) | <.001 | 6.9 (1.0) | 6.9 (1.0) | 6.8 (1.1) | 6.8 (1.2) | <.001 |
| Depression, % | 9 | 9 | 10 | <.001 | 7 | 8 | 10 | 13 | <.001 |
| Systolic Blood Pressure, mmHg | 126.4 (17.9) | 126.2(17.7) | 126.0 (17.6) | 0.01 | 124.9(17.9) | 125.4 (17.7) | 127.1(17.7) | 128.2(17.6) | <.001 |
| Diastolic Blood Pressure, mmHg | 74.9 (9.2) | 74.9 (9.2) | 74.8 (9.3) | 0.19 | 74.5 (9.2) | 74.6 (9.2) | 75.2 (9.3) | 75.5 (9.4) | <.001 |
| History of hypertension, % | 21 | 22 | 23 | 0.001 | 17 | 20 | 25 | 28 | <.001 |
| History of diabetes. % | 2 | 2 | 3 | 0.07 | 2 | 2 | 3 | 4 | <.001 |
| History of hyperlipidemia, % | 7 | 7 | 8 | 0.04 | 6 | 8 | 8 | 7 | <.001 |
| Aspirin use, % | 19 | 21 | 19 | 0.76 | 20 | 21 | 20 | 19 | 0.12 |
| Alcohol consumption, % | <.001 | <.001 | |||||||
| None | 13 | 10 | 9 | 8 | 10 | 12 | 15 | ||
| <1 /week | 30 | 33 | 34 | 29 | 32 | 33 | 35 | ||
| 1–7 /week | 26 | 28 | 26 | 32 | 28 | 25 | 18 | ||
| >7 /week | 12 | 13 | 13 | 16 | 14 | 11 | 10 | ||
| Past drinker | 18 | 17 | 18 | 15 | 15 | 19 | 23 | ||
| Total energy intake, kcal/day | 1499 (728) | 1562 (637) | 1608 (705) | <.001 | 1543 (643) | 1539 (651) | 1549 (685) | 1577 (781) | <.001 |
| % calories from saturated fat | 9.7 (3.3) | 10.0 (3.3) | 10.2 (3.4) | <.001 | 8.9 (3.1) | 9.7 (3.2) | 10.4 (3.2) | 11.2 (3.4) | <.001 |
| Fiber, g/day | 16.1 (7.7) | 16.5 (7.2) | 16.4 (7.4) | 0.004 | 18.0 (7.6) | 16.8 (7.3) | 15.6 (7.0) | 14.3 (7.0) | <.001 |
MET = metabolic equivalent task; MI = myocardial infarction.
All values are means (SD) for continuous variables or frequencies for categorical variables, standardized to the age distribution of the study population (with the exception of age)
In multivariable-adjusted analyses, increased sitting time and decreased physical activity were positively associated with risk of CHD and stroke (Table 2). As the results for CHD and stroke were similar, the end points were combined to examine total CVD. In multivariable models that included physical activity, the hazard ratio (HR) for total CVD comparing ≥ 10 hours/day of sitting time to ≤ 5 hours/day was 1.18 (95% CI 1.09, 1.29) (P for trend < 0.001). With high physical activity, i.e. > 20 MET-hrs/wk, as the reference group, the CVD risks for medium (8.4 – 20 MET-hrs/wk), low (1.8 – 8.3 MET-hrs/wk) activity, and inactive (≤ 1.7 MET-hrs/wk) groups were 1.16 (1.06, 1.27), 1.30 (1.18, 1.42), and 1.47 (1.33, 1.62), respectively (P for trend <0.001). All associations were mildly attenuated after adjustment for BMI and history of comorbidities, but remained statistically significant (Table 2). When examined as continuous variables, each hour/day of sitting time was associated with 2% higher risk of CVD (HR = 1.02, 95% CI 1.01, 1.03) and each MET-hour/week of physical activity with a 1% lower risk of CVD (HR = 0.990, 95% CI 0.987, 0.992). There was no evidence of non-linearity when applying restricted cubic splines to the association between sitting time (p= 0.87) or physical activity (p = 0.60) and risk of CVD.
Table 2.
Hazard ratios (95% confidence intervals) for the association between sitting time, physical activity, and risk of coronary heart disease (CHD)*, stroke†, or total cardiovascular disease (CVD)‡
| Sitting Time (hours/day) | Physical Activity (MET-hour/week) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| ≤5 | 5.1–9.9 | ≥10 | P for trend | High (> 20) | Medium (8.4 – 20) | Low (1.8 – 8.3) | Inactive (≤ 1.7) | P for trend | |
| CHD* | |||||||||
| Cases | 902 | 1019 | 490 | 416 | 663 | 667 | 665 | ||
| Person-years | 319,776 | 331,577 | 153,884 | 204,913 | 235,822 | 197,848 | 166,654 | ||
| Age-adjusted | 1.00 | 1.03 (0.95, 1.13) | 1.28 (1.15,1.43) | <.001 | 1.00 | 1.30 (1.15,1.47) | 1.55 (1.37, 1.76) | 1.97 (1.74, 2.22) | <.001 |
| Multivariable-adjusted§ | 1.00 | 1.02 (0.94,1.12) | 1.18 (1.05,1.32) | 0.005 | 1.00 | 1.23 (1.09,1.39) | 1.36 (1.20,1.54) | 1.57 (1.38, 1.79) | <.001 |
| MV§ + BMI | 1.00 | 1.01 (0.92,1.11) | 1.14 (1.02,1.28) | 0.02 | 1.00 | 1.22 (1.08,1.38) | 1.32 (1.16, 1.50) | 1.49 (1.31, 1.70) | <.001 |
| MV§ + BMI, comorbidities¶ | 1.00 | 1.00 (0.92, 1.10) | 1.13 (1.01, 1.26) | 0.04 | 1.00 | 1.20 (1.06, 1.36) | 1.28 (1.13, 1.45) | 1.43 (1.25, 1.63) | <.001 |
|
| |||||||||
| Stroke† | |||||||||
| Cases | 763 | 876 | 411 | 399 | 561 | 563 | 527 | ||
| Person-years | 320,330 | 332,260 | 154,220 | 205,519 | 236,427 | 198,065 | 166,798 | ||
| Age-adjusted | 1.00 | 1.05 (0.95,1.16) | 1.28 (1.14,1.45) | <.001 | 1.00 | 1.14 (1.00,1.30) | 1.35 (1.19,1.54) | 1.61 (1.41, 1.83) | <.001 |
| Multivariable-adjusted§ | 1.00 | 1.05 (0.95,1.15) | 1.21 (1.07,1.37) | 0.003 | 1.00 | 1.10 (0.97,1.25) | 1.24 (1.08,1.41) | 1.39 (1.21, 1.59) | <.001 |
| MV§ + BMI | 1.00 | 1.04 (0.94,1.15) | 1.19 (1.05,1.35) | 0.006 | 1.00 | 1.09 (0.96,1.24) | 1.21 (1.06,1.39) | 1.35 (1.17, 1.55) | <.001 |
| MV§ + BMI, comorbidities¶ | 1.00 | 1.03 (0.94,1.14) | 1.18 (1.04,1.34) | 0.008 | 1.00 | 1.08 (0.95,1.23) | 1.19 (1.04,1.36) | 1.30 (1.13, 1.50) | <.001 |
|
| |||||||||
| Total CVD‡ | |||||||||
| Cases | 1581 | 1805 | 849 | 782 | 1161 | 1172 | 1120 | ||
| Person-years | 317,343 | 328,936 | 152,656 | 203,907 | 234,178 | 196,071 | 164,779 | ||
| Age-adjusted | 1.00 | 1.05 (0.98,1.12) | 1.27 (1.17,1.38) | <.001 | 1.00 | 1.21 (1.11,1.33) | 1.45 (1.33,1.59) | 1.77 (1.61, 1.94) | <.001 |
| Multivariable-adjusted§ | 1.00 | 1.04 (0.97,1.11) | 1.18 (1.09,1.29) | <.001 | 1.00 | 1.16 (1.06,1.27) | 1.30 (1.18,1.42) | 1.47 (1.33, 1.62) | <.001 |
| MV§ + BMI | 1.00 | 1.03 (0.96,1.10) | 1.16 (1.06,1.26) | 0.001 | 1.00 | 1.15 (1.05,1.26) | 1.26 (1.15,1.39) | 1.40 (1.27, 1.55) | <.001 |
| MV§ + BMI, comorbidities¶ | 1.00 | 1.02 (0.95, 1.09) | 1.15 (1.05, 1.25) | 0.002 | 1.00 | 1.13 (1.04, 1.24) | 1.23 (1.12, 1.35) | 1.35 (1.23, 1.49) | <.001 |
MET = metabolic equivalent task ; MV = multivariable ; BMI = body mass index.
CHD : Nonfatal myocardial infarction and fatal coronary heart disease
Stroke: Nonfatal and fatal stroke
CVD: Nonfatal MI, fatal CHD, nonfatal and fatal stroke
The multivariable model was stratified by age and includes sedentary time and physical activity simultaneously as well as race, education, income, marital status, smoking, family history of myocardial infarction, depression, alcohol intake, hours of sleep, intake of total calories, saturated fat, fiber
History of hypertension, diabetes, or high cholesterol at baseline
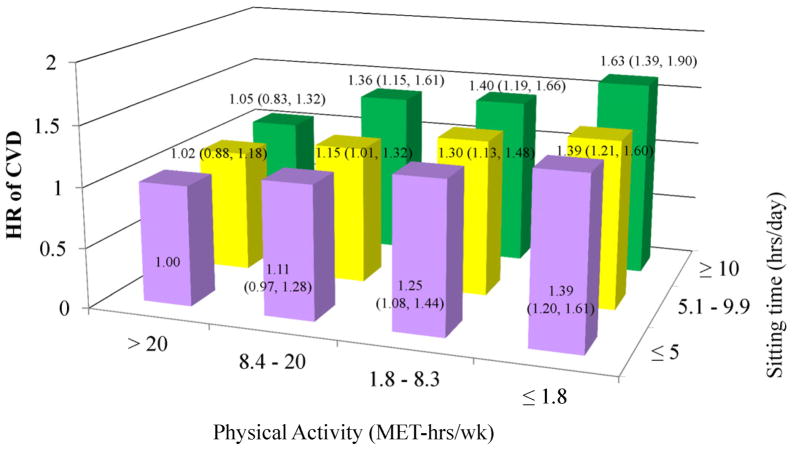
When participants were cross-classified based on both sitting time and leisure-time physical activity, only 18% of the high activity group reported sitting for ≥ 10 hours/day compared to 32% of physically inactive group. Except in the most active women, more time spent sitting increased CVD risk in each physical activity group (Figure 1), with CVD risk being highest in physically inactive women who also reported ≥ 10 hrs/day of sitting (HR = 1.63, 95% CI = 1.39, 1.90); however, the interaction between sitting time and physical activity was not statistically significant (P for interaction = 0.94).
Figure 1. Multivariable-adjusted hazard ratios for total cardiovascular disease for the joint association between sedentary time and physical activity.
The multivariable model was stratified by age and includes race, education, income, marital status, smoking, family history of myocardial infarction, depression, alcohol intake, hours of sleep, intake of total calories, saturated fat, fiber, and body mass index. The P for interaction is 0.94. HR = hazard ratio; CVD = cardiovascular disease; MET = metabolic equivalent task.
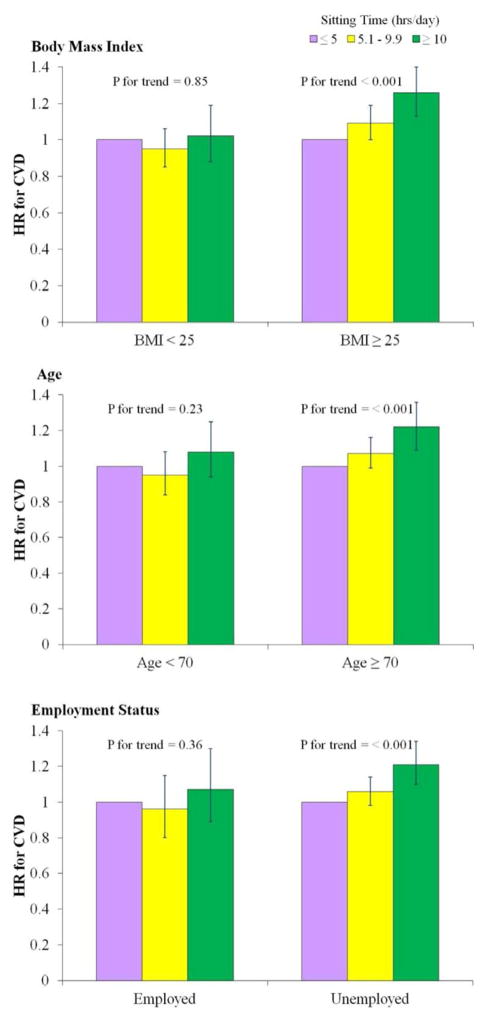
There were significant interactions of sitting time with CVD risk within subgroups defined by BMI and age, but not by employment status (Figure 2; P for interaction=0.044, 0.026, and 0.22, respectively). Time spent sitting was associated with increased CVD risk in women with BMI ≥ 25 (HR = 1.26, 95% CI 1.13, 1.40 for sitting ≥ 10 hrs/day; P for trend <0.001), but not in women with BMI < 25 (HR = 1.02, 95% CI 0.88, 1.19; P for trend = 0.85). Sitting time was also associated with a higher CVD risk among women aged 70 years and older (HR = 1.22, 95% CI 1.09, 1.36 for sitting ≥ 10 hrs/day; P for trend <0.001), but not among younger women (HR = 1.08, 95% CI 0.94, 1.25; P for trend = 0.23). Although the interaction was not statistically significant (P for interaction = 0.22), more sitting time was associated with higher CVD risk in unemployed women (HR = 1.21, 95% CI 1.10, 1.34; P for trend <0.001), but not employed women (HR = 1.07, 95% CI 0.89, 1.30; P for trend = 0.36).
Figure 2. Multivariable-adjusted hazard ratios for total cardiovascular disease according to sedentary time in subgroups defined by body mass index (BMI), age, and employment status.
The multivariable model was stratified by age and includes physical activity, race, education, income, marital status, smoking, family history of myocardial infarction, depression, alcohol intake, hours of sleep, intake of total calories, saturated fat, fiber. The P for interaction for BMI is 0.04, age is 0.03, and employment is 0.22. HR = hazard ratio; CVD = cardiovascular disease; BMI = body mass index.
Finally, an increase in sitting time over a three year period was associated with an increased risk of CVD. Compared to participants who reported no change in sitting time, the HR for participants who increased sitting time by more than 2 hours/day was 1.18 (95% CI 1.07, 1.31) after adjusting for covariates, while the HR for participants who decreased sitting time by more than 2 hours/day was 1.01 (95% CI 0.91, 1.13). When examined continuously, a 1 hour/day increase in sitting time over a three-year period was associated with a 1.4% increase in CVD risk (HR = 1.014, 95% CI, 1.001, 1.027, p = 0.03) in the multivariable-adjusted model.
DISCUSSION
In this large, prospective study of postmenopausal U.S. women, prolonged sitting time was associated with increased risk of incident CHD, stroke, and total CVD, independent of leisure-time physical activity; however, low levels of leisure-time physical activity were also strongly associated with increased CVD risk, after adjusting for sitting time. Women who were physically inactive and reported ≥ 10 hours per day of sitting time, comprising 6% of our study population, were at 63% greater CVD risk than highly active women who reported sitting ≤ 5 hours per day, after adjusting for several cardiovascular risk factors. Associations between prolonged sitting and risk of CVD were stronger in overweight and obese versus normal weight women and women aged 70 years and older compared to younger women.
Few studies have examined the association between sitting time and risk of incident cardiovascular disease; to date, the outcome of interest has been largely limited to CVD mortality (4, 10, 16 – 18). Thus, the current analysis, which includes incident CHD and stroke separately in relationship to sitting time and physical activity habits within a large well-characterized cohort of older postmenopausal women, as well as combined CVD events, is an important contribution to the literature. Our results are also consistent with prior studies which have reported an increased risk of CVD mortality as time spent sitting increases, independent of usual leisure-time physical activity.
The association between physical activity, hours spent sitting, and CVD has been previously reported among WHI-OS participants (4). Manson and colleagues reported that high levels of recreational physical activity were associated with 30–40% reductions in CVD risk over a mean 3.2 years of follow-up; and, using baseline measures of sitting time, women who spent at least 16 hours per day sitting had an increased CVD risk (HR=1.68, 95% CI 1.07, 2.64), compared to those who spent less than 4 hours per day sitting. The joint effects of sitting time and physical activity were not reported in this previous study.
Although the interaction between sitting time and physical activity was not statistically significant in the present analysis, clinically significant attenuation of CVD risk was found in all women, except for those in the high activity group, who reported sitting less than 5 hours per day. As the least active women were also the most likely to report prolonged time spent sitting, reducing sitting time could potentially reduce CVD risk substantially among less active women. The finding that the association between prolonged sitting and CVD is attenuated among the most active women is similar to studies of mortality (16, 18) and shows that it may be beneficial to participate in regular exercise despite engaging in other potentially detrimental behaviors, like prolonged sitting. The most active group in our study reported > 20 MET-hrs/week of physical activity, which exceeds the physical activity guidelines substantially. However, women engaging in 8.4 – 20 MET-hrs/wk of physical activity, which meets the physical activity guidelines, were still at increased CVD risk if they reported prolonged sitting.
The association between prolonged sitting time and increased CVD risk was significant only in overweight women and women 70 years and older. Previous studies (16, 18) have reported similar results where the positive association between time spent sitting and mortality was stronger in overweight and obese versus normal weight individuals. These findings emphasize the importance of limiting time spent sitting, particularly in overweight and obese individuals. The fact that the association between sitting time and CVD was stronger in older compared to younger women may be due to sitting time including both occupational and leisure sitting in this study. Thus, in older women, sitting may comprise more television watching as they are more likely to be retired compared to younger women. Television watching has previously been found to be more detrimental than overall sitting time (10).
Additionally, increasing sitting time over a three-year period was associated with a higher risk of CVD. Reducing time spent sitting, however, was not associated with CVD risk in this study. This finding may indicate that change in sitting time needs to be assessed over a longer period of time. Alternatively, a better measurement of sitting time, like accelerometers, or a randomized controlled trial may be necessary to truly examine the effect of changing sedentary behaviors.
Physiological responses associated with prolonged sitting, such as suppression of skeletal muscle lipoprotein lipase (LPL) activity, which is necessary for triglyceride uptake and high-density lipoprotein cholesterol production, and reduced glucose uptake (9, 18, 19) might explain the independent effect of sedentary behavior on CVD risk factors, and also on CVD risk. Sedentary behavior may also be related to overweight and obesity through increased energy intake and decreased energy expenditure (20).
In addition to reducing sitting time, taking breaks during prolonged periods of sitting, i.e. by standing up and taking short walks, might be beneficial in lowering CVD risk. In accelerometer studies, having a higher number of breaks in sedentary time was inversely associated with waist circumference, BMI, triglycerides, 2-h plasma glucose, and C-reactive protein independent of total time spent sitting and physical activity (21, 22). Additionally, a recent randomized trial showed that interrupting sitting time with short bouts of light- or moderate-intensity activity lowers postprandial glucose and insulin levels in overweight adults (23).
Strengths of our study include its prospective design, the large, multi-ethnic, geographically diverse cohort of postmenopausal women, detailed assessment of physical activity, and availability of several relevant covariates for analysis. Additionally, this study is the first to investigate the association with CVD using serially obtained measurements of sitting time and physical activity, thereby enabling us to update exposure status during follow-up. We were also able to assess the independent associations between sitting time and usual recreational physical activity with CVD risk.
Our study also has several limitations, including the fact that analyses were limited to postmenopausal women; therefore, findings cannot necessarily be generalized to men or younger women. Sitting time and physical activity were self-reported, although it is worth noting that physical activity measures were validated in this cohort (11, 24). Moreover, measurement error is unlikely to bias our results because sedentary time and physical activity were assessed prospectively so any reporting errors would be non-differential with respect to subsequent disease status. Nonetheless, device-based measures of sitting time and physical activity, like accelerometers, may provide more accurate assessments of these variables. Another limitation of this study is that we were unable to examine the associations with different types of sedentary behavior, like television watching or transportation, as the questionnaire only assessed total sitting time. Finally, as with most such studies, the possibility of residual confounding by other lifestyle and behavioral factors must be considered.
In conclusion, the findings from this large, multi-ethnic group of postmenopausal women indicate that prolonged sitting time significantly increases risk of CVD, independent of leisure-time physical activity. Given the projected population growth of U.S. women 65 years of age and older, and the relatively high prevalence of physical inactivity, the present findings have important public health implications. Reducing sitting time among older women who are less active could potentially reduce risk of CHD and stroke, major causes of morbidity in older women. Moreover, for individuals who are unable, or averse, to exercise, amount of time spent sitting may be more amenable to change than increasing levels of physical activity.
Acknowledgments
Funding/Support:
The WHI program is funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, U.S. Department of Health and Human Services through contracts HHSN268201100046C, HHSN268201100001C, HHSN268201100002C, HHSN268201100003C, HHSN268201100004C, and HHSN271201100004C. Dr. Chomistek was supported by grants CA152904 from the National Cancer Institute, HL035464 from the National Heart, Lung, and Blood Institute, and an institutional training grant (DK007703-17) from the National Institute of Diabetes and Digestive and Kidney Diseases.
The authors thank the WHI investigators and staff for their dedication and the study participants for their continued cooperation and participation. A listing of WHI investigators can be found at https://cleo.whi.org/researchers/Documents%20%20Write%20a%20Paper/WHI%20Investigator%20Short%20List.pdf.
ABBREVIATIONS
- BMI
body mass index
- CHD
coronary heart disease
- CVD
cardiovascular disease
- CI
confidence interval
- HR
hazard ratio
- MET
metabolic equivalent task
- MI
myocardial infarction
- OS
observational study
- WHI
Women’s Health Initiative
Footnotes
Relationship with Industry: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Archer E, Blair SN. Physical activity and prevention of cardiovascular disease: from evolution to epidemiology. Prog Cardiovasc Disease. 2011;53:387–396. doi: 10.1016/j.pcad.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Sattelmair J, Pertman J, Ding EL, Kohl H, 3rd, Haskell W, Lee IM. Dose-response between physical activity and risk of coronary heart disease: a meta-analysis. Circulation. 2011;124(7):789–95. doi: 10.1161/CIRCULATIONAHA.110.010710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eaton CB, Medalie JH, Flocke SA, Yaari BA, Zyzanski SJ, Goldbourt U. Self-reported physical activity predicts long-term coronary heart disease death and all-cause mortality: Twenty-one year follow-up of the Israeli Ischemic Heart Disease Study. Arch Fam Med. 1995;4:323–329. doi: 10.1001/archfami.4.4.323. [DOI] [PubMed] [Google Scholar]
- 4.Manson JE, Greenland P, LaCroix AZ, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–25. doi: 10.1056/NEJMoa021067. [DOI] [PubMed] [Google Scholar]
- 5.Lanningham-Foster L, Nysse LJ, Levine JA. Labor saved, calories lost: the energetic impact of domestic labor-saving devices. Obes Res. 2003;11(10):1178–81. doi: 10.1038/oby.2003.162. [DOI] [PubMed] [Google Scholar]
- 6.Church TS, Thomas DM, Tudor-Locke C, et al. Trends over 5 decades in U.S. occupation-related physical activity and their associations with obesity. PLoS. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Owen N, Healy GN, Matthews CE, Dunstan DW. Too much sitting: the population health science of sedentary behavior. Exerc Sport Sci Rev. 2010 Jul;38(3):105–13. doi: 10.1097/JES.0b013e3181e373a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Healy GN, Dunstan DW, Salmon J, Shaw JE, Zimmet PZ, Owen N. Television time and continuous metabolic risk in physically active adults. Med Sci Sports Exerc. 2008;40(4):639–45. doi: 10.1249/MSS.0b013e3181607421. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton MT, Hamilton DG, Zderic TW. Exercise physiology versus inactivity physiology: an essential concept for understanding lipoprotein lipase regulation. Exerc Sport Sci Rev. 2004;32:161–166. doi: 10.1097/00003677-200410000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews CE, George SM, Moore SC, et al. Amount of time spent in sedentary behaviors and cause-specific mortality in US adults. Am J Clin Nutr. 2012;95:437–45. doi: 10.3945/ajcn.111.019620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M. The Women’s Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol. 2003;13(9 Suppl):S107–21. doi: 10.1016/s1047-2797(03)00047-4. [DOI] [PubMed] [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 13.Curb JD, McTiernan A, Heckbert SR, et al. Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol. 2003;13(9 Suppl):S122–28. doi: 10.1016/s1047-2797(03)00048-6. [DOI] [PubMed] [Google Scholar]
- 14.Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med. 1989;8(5):551–561. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- 15.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. p. 683. [Google Scholar]
- 16.Katzmarzyk PT, Church TS, Craig CL, Bouchard C. Sitting time and mortality from all causes, cardiovascular disease, and cancer. Med Sci Sports Exerc. 2009;41:998–1005. doi: 10.1249/MSS.0b013e3181930355. [DOI] [PubMed] [Google Scholar]
- 17.Patel AV, Bernstein L, Deka A, et al. Leisure time spent sitting in relation to total mortality in a prospective cohort of US adults. Am J Epidemiol. 2010;172:419–29. doi: 10.1093/aje/kwq155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warren TY, Barry V, Hooker SP, Sui X, Church TS, Blain SN. Sedentary behaviors increase risk of cardiovascular disease mortality in men. Med Sci Sports Exerc. 2010;42:879–85. doi: 10.1249/MSS.0b013e3181c3aa7e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zderic TW, Hamilton MT. Physical inactivity amplifies the sensitivity of skeletal muscle to the lipid-induced downregulation of lipoprotein lipase activity. J Appl Physiol. 2006;100:249–257. doi: 10.1152/japplphysiol.00925.2005. [DOI] [PubMed] [Google Scholar]
- 20.Bey L, Hamilton MT. Suppression of skeletal muscle lipoprotein lipase activity during physical inactivity: a molecular reason to maintain daily low-intensity activity. J Physiol. 2003;551:673– 682. doi: 10.1113/jphysiol.2003.045591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton MT, Hamilton DG, Zderic TW. Role of low energy expenditure and sitting in obesity, metabolic syndrome, type 2 diabetes, and cardiovascular disease. Diabetes. 2007;56(11):2655–67. doi: 10.2337/db07-0882. [DOI] [PubMed] [Google Scholar]
- 22.Healy GN, Dunstan DW, Salmon J, et al. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care. 2008;31(4):661–6. doi: 10.2337/dc07-2046. [DOI] [PubMed] [Google Scholar]
- 23.Healy GN, Matthews CE, Dunstan DW, Winkler EA, Owen N. Sedentary time and cardio-metabolic biomarkers in US adults: NHANES 2003–06. Eur Heart J. 2011;32:590–97. doi: 10.1093/eurheartj/ehq451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dunstan DW, Kingwell BA, Larsen R, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35:976–983. doi: 10.2337/dc11-1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Meyer AM, Evenson KR, Morimoto L, Siscovick D, White E. Test-retest reliability of the Women’s Health Initiative Physical Activity Questionnaire. Med Sci Sports Exerc. 2009;41(3):530–8. doi: 10.1249/MSS.0b013e31818ace55. [DOI] [PMC free article] [PubMed] [Google Scholar]