Abstract
Ovarian carcinoma (OC) is the most lethal gynecological malignancy. Response to platinum-based chemotherapy is poor in some patients and, thus, current research is focusing on new therapy options. The various histological types of OC are characterized by distinctive molecular genetic alterations that are relevant for ovarian tumorigenesis. The understanding of these molecular pathways is essential for the development of novel therapeutic strategies.
Purpose
We want to give an overview on the molecular genetic changes of the histopathological types of OC and their role as putative therapeutic targets.
In Depth Review of Existing Data
In 2012, the vascular endothelial growth factor (VEGF) inhibitor, bevacizumab, was approved for OC treatment. Bevacizumab has shown promising results as single agent and in combination with conventional chemotherapy, but its target is not distinctive when analyzed before treatment. At present, mammalian target of rapamycin (mTOR) inhibitors, poly-ADP-ribose polymerase (PARP) inhibitors and components of the EGFR pathway are in the focus of clinical research. Interestingly, some phytochemical substances show good synergistic effects when used in combination with chemotherapy.
Conclusion
Ongoing studies of targeted agents in conjunction with chemotherapy will show whether there are alternative options to bevacizumab available for OC patients. Novel targets which can be assessed before therapy to predict efficacy are needed. The assessment of therapeutic targets is continuously improved by molecular pathological analyses on tumor tissue. A careful selection of patients for personalized treatment will help to reduce putative side effects and toxicity.
Keywords: ovarian cancer, molecular carcinogenesis, targeted therapy
1. Pathology and Biology of Ovarian Carcinoma
In the past, ovarian carcinoma (OC) has been considered as one single disease. However, ovarian carcinoma comprises a variety of tumors with various histopathological features and expresses different biological behavior. Currently, therapy rather depends on tumor stage and grade than on the histological type [1]. It can be expected that a more individual approach of treating ovarian carcinoma will be selected in the future since several phase III studies investigating targeted therapies are underway [1]. The search for novel therapeutic targets is a growing focus of research and crucial for the development of new drugs [2].
The World Health Organization (WHO) classifies ovarian neoplasms according to their histological differentiation, namely epithelial, sex cord-stromal and germ cell neoplasms [3]. Epithelial ovarian tumors represent the largest group and are basically subdivided into serous, mucinous, endometrioid, clear cell and transitional cell tumors; the latter including Brenner tumors [3]. Among these groups of tumors, three categories are distinguished according to the biological behavior: benign, borderline and malignant. Several rare malignant neoplasms complete the category of epithelial ovarian tumors, such as mixed carcinoma, carcinosarcoma and undifferentiated carcinoma.
Among the borderline tumor category, the serous type and the endocervical variant of the mucinous type may present at advanced stages II and III and are associated with recurrence in about 10% of cases. Whereas, the other histological types are typically stage I and show a benign course. Serous neoplasms are the most frequent category, encompassing more than 50% of ovarian tumors. Serous carcinomas are currently separated into two histologically and biologically distinctive subtypes, low grade and high grade, based on the degree of nuclear atypia and the amount of mitoses. Low grade serous carcinomas are infrequent and typically associated with serous borderline tumors [1]. Recent investigations indicate that the tube is probably the place where serous ovarian carcinomas originate [4–6]. Especially the tubal fimbria seems to play an important role in carcinogenesis. There is evidence that the mechanism of tumor formation in the tube is basically very different compared to that of the ovary [4,7,8]. Primary mucinous carcinomas of the ovary account for about 10% of epithelial ovarian neoplasms [9] and are most common of the so-called intestinal/enteric type. Mucinous carcinomas are often associated with a mucinous cystadenoma and/or a mucinous borderline tumor, and are most frequently unilateral and diagnosed at stage I [1]. Endometrioid and clear cell carcinomas are frequently associated with endometriosis, which is generally considered a risk factor of ovarian carcinoma. In particular, 2% of clear cell carcinoma patients, 9% of endometrioid carcinoma patients, and, interestingly, also 2% of patients with low grade serous carcinoma show a history of endometriosis [10]. Most endometrioid carcinomas are well or moderately differentiated, i.e., low grade and only a small subset is poorly differentiated, i.e., high grade. The distinction of some histological types may be difficult, in particular between high grade endometrioid and high grade serous carcinomas and between true clear cell carcinomas and other types of carcinomas featuring areas of clear cells [11].
Recently, the differential diagnosis of ovarian carcinomas has been supported by immunohistochemistry by a selection of antibodies drawn from the molecular tumorigenesis. In particular, a panel of estrogen (ER) and progesterone (PR) receptors, p53, PTEN and Wilms Tumor Gene Product 1 (WT1) may be helpful to type carcinomas with indefinite histological features. Only serous carcinomas are generally WT1 positive and high grade serous carcinomas typically show diffuse intense p53 immunoreactivity [11]. On the other hand, endometrioid and clear cell carcinomas may show a loss of PTEN, which is usually caused by mutation. Immunoreactivity for ER and PR is typical for endometrioid and serous carcinomas and less intense or absent in clear cell and mucinous carcinomas. p53 is typically weak or negative in clear cell carcinoma, but may be positive in a subset of clear cell and poorly differentiated emdometrioid carcinomas; yet, in contrast to high grade serous carcinomas p53 shows a heterogeneous pattern. Finally, clear cell carcinoma is characterized by a frequent expression of hepatocyte nuclear factor 1 (HNF1) which is not found in the other histological subtypes.
2. In Depth Review of Existing Data
2.1. Different Molecular Genetic Pathways and Putative Molecular Targets in Ovarian Cancer
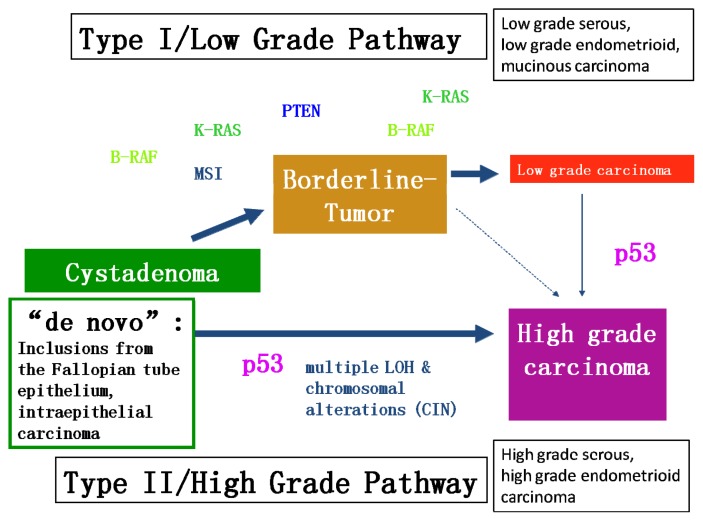
Recent studies have led to a new model of explanation for OC carcinogenesis (Figure 1). This dualistic model divides epithelial OC into two categories: Type I comprises low-grade serous, low-grade endometrioid, clear cell and mucinous carcinomas and Brenner tumors. They mostly present at stage I (tumor is confined to the ovaries) and feature certain mutations, for example K-Ras, B-Raf or PTEN. The tumorigenic pathway in type I carcinomas is characterized by the development through atypically proliferating or borderline tumors which can be considered as an adenoma-carcinoma sequence. The residues of the benign and/or the borderline stages are frequently found in association with the carcinoma. Type I tumors develop slowly over a longer period of time, are not associated with dramatic clinical symptoms and usually are detected by chance during routine examination. They show a favorable prognosis even at higher stages. Progression into type II carcinomas seems to occur only in a small subset of type I carcinomas, in particular low grade serous and endometrioid carcinomas. Apart from mutations of K-Ras, B-Raf and PTEN, type I carcinomas also feature microsatellite instability in about 15%. p53 mutations are rarely present in type I carcinomas but may occur during progression into type II carcinomas.
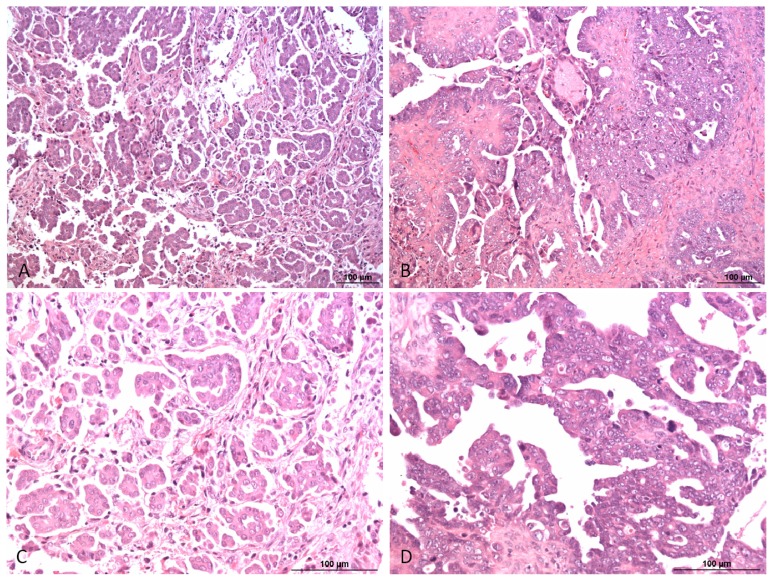
Figure 1.
Type I/low grade (A, C) and type II/high grade (B, D) serous ovarian carcinoma. High grade serous carcinoma is characterized by a significantly higher degree of nuclear atypia and higher number of mitosis compared to low grade serous carcinoma. The papillae are less well preserved in high grade compared to low grade serous carcinomas. HE, 100× (A, B) and 200× (C, D).
High-grade serous, high-grade endometrioid and undifferentiated carcinomas, as well as malignant mixed mesodermal tumors count among type II (Figure 2). They are all histologically high grade neoplasms with aggressive course and unfavorable prognosis. Typically, they are not or only exceptionally associated with borderline tumors and, therefore, considered to develop without a well-defined precursor lesion “de novo”. Type I and type II tumors also differ in molecular tumorigenesis (Figure 3). Unlike type I, type II carcinomas often present at advanced stage and have a high frequency of TP53 mutations, whereas mutations occurring in type I carcinomas are rarely found. Type II carcinomas also often feature alterations of the tumor suppressor genes breast cancer 1, early onset (BRCA1) and breast cancer 2, early onset (BRCA2) and are in general genetically unstable [12]. Also, the chromatin remodeling gene Rsf-1 has been recently demonstrated in high grade ovarian serous carcinomas. Abundant Rsf-1 expression can contribute to genomic instability, which favors tumor growth and has anti-apoptotic effects, which is typical for type II ovarian carcinomas [13].
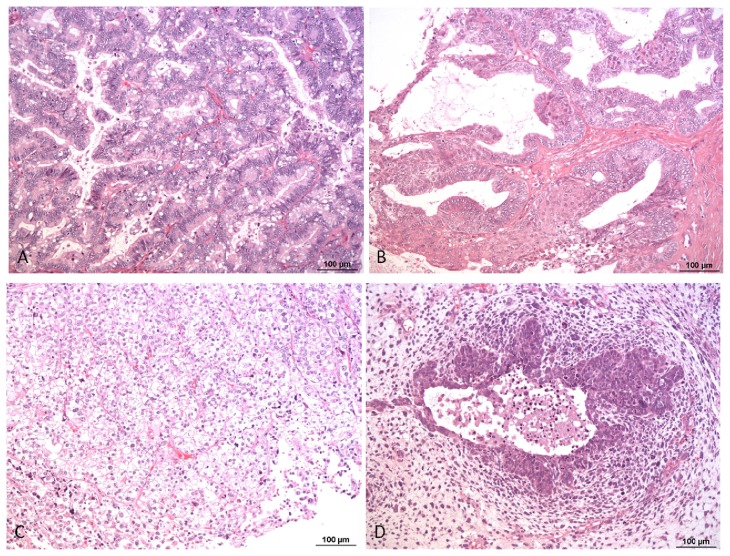
Figure 2.
Mucinous (A), endometrioid (B), clear cell carcinoma (C) and mixed malignant mesodermal tumor (MMMT) (D). HE, 100×.
Figure 3.
Molecular tumorigenesis of type I and type II ovarian carcinoma (modified according to Kurman, Shih 2004, Lax 2009).
Serous tumorigenesis has been a focus of research over the last two decades. Well defined precursor lesions were described for serous carcinomas of the endometrium and the Fallopian tube, named intraepithelial carcinoma (serous endometrial intraepithelial carcinoma (SEIC) and serous tubal intraepithelial carcinoma (STIC), respectively). These intraepithelial carcinomas are flat lesions consisting of highly atypical cells, which frequently harbor p53 mutations. Neoplastic cells with mutated p53 show either strong or flat negative immunoreactivity. In the past, it has been hypothesized that high grade ovarian serous carcinomas could develop from inclusion cysts by malignant transformation. Recently, a unifying model for ovarian and tubal neoplasms tried to synthesize the dualistic model of ovarian carcinoma with the role of the Fallopian tube in the development of serous carcinomas of the female genital tract [14]. According to this proposed model, most serous carcinomas develop from Fallopian tube epithelium that is implanted into the ovaries. High grade serous carcinomas either develop from tubal intraepithelial carcinoma (TIC), which typically occurs in the fimbria, or from malignant transformation of serous inclusion cysts in the ovary. In contrast, low grade serous carcinomas develop from serous inclusion cysts through borderline tumors. Endometrioid and clear cell carcinomas arise within endometriosis, which typically results from implantation of endometrial tissue into the ovaries. It has been further proposed that based on preliminary data mucinous and transitional (Brenner) tumors may arise from transitional-type epithelial nests at the tubal-mesothelial junction by a process of metaplasia [14]. Clear cell carcinomas are considered to develop in the background of endometriosis and frequently harbor mutations in the ARID1A gene [15].
Summing up these recent findings of carcinogenesis in the ovary, it is evident that OC is not a single disease but comprises a heterogeneous group of tumors that can be classified from their distinctive morphologic and molecular genetic features [14].
2.2. Putative Molecular Targets
2.2.1. BRCA1 and BRCA2
The BRCA1 and BRCA2 genes are located on chromosomes 17q21 and 13q12, respectively. Germ line mutations of these two genes are an important cause of hereditary breast cancer. The mutations are found at different sites of these genes and tremendously increase the risk of developing breast and ovarian cancer. In particular, in BRCA1 mutation carriers, the cumulative life time risk for breast cancer is about 70%; for ovarian cancer 40%; and, in BRCA2 mutation carriers, 50% for breast and 10% for ovarian cancer. It is currently estimated that about 30%–50% of hereditary breast and ovarian cancers develop in BRCA1 and 2 mutation carriers. This accounts for about 5%–10% of overall breast and ovarian carcinoma incidence [16]. In addition, the overall risk of developing any sort of cancer also seems to be elevated by 20%–60%. In BRCA1 and 2 germline mutation carriers, somatic inactivation of the remaining wild-type allele is required, which means that a somatic mutation has to be dominant [17,18].
BRCA1 and BRCA2 seem to be involved in the repair of DNA double strand breaks, and in the regulation of transcription [19,20]. In particular, BRCA1 repairs DNA breaks by homologous recombination, which is a repair mechanism widely used by cells. It allows the exchange of nucleotide sequences between two similar or identical molecules of DNA. BRCA1 moves to the locus of DNA break site, recruited there by the histone protein H2AX [21]. It was suggested, that BRCA1 and H2AX function as initiators of DNA break repair by making the respective foci accessible to ligating proteins [21]. BRCA1 also acts in the alternative non-homologous end-joining (NHEJ) pathway, while BRCA2 only works in the repair process of double strand breaks using homologous recombination [22]. The NHEJ pathway is highly conserved by direct repair of DNA strand breaks. Ineffective NHEJ and ineffective repair of DNA strand breaks by homologous recombination can lead to translocations and other hallmarks of cancer [23]. Despite being a highly effective DNA repair mechanism, homologous recombination might have the harmful side effect of altering BRCA1 and 2 gene function. It seems that cells which lack functioning BRCA1 or BRCA2 are more likely to accumulate chromosomal abnormalities such as aneuploidy or the amplification of the centrosome [24].
The somatic loss of the functional BRCA gene product was also observed in sporadic ovarian carcinomas. Loss of heterozygosity of the BRCA1 gene was found in 50%–70% of sporadic ovarian carcinomas and loss of heterozygosity of BRCA2 was found in 30%–50% [25,26]. This suggests that in the development of sporadic breast and ovarian carcinomas, the somatic loss of BRCA alleles might have an important pathophysiological role, similar to germline point mutations [27].
2.2.2. KRAS and BRAF Mutations Lead to the Activation of the MAPK/ERK Pathway
Mutations in KRAS and BRAF typically occur in the so-called type I ovarian carcinomas; in particular in low grade serous, mucinous and endometrioid carcinomas [28,29]. KRAS and BRAF mutations lead to constitutive activation of the MAPK/ERK pathway [30,31]. ERK activates downstream targets in the nucleus and cytoplasm [32,33]. Hormones and growth factors that trigger signaling via mitogen-activated protein kinases (MAPKs) use two classes of surface receptors, receptor tyrosine kinases (RTK) and G protein coupled receptors (GPCR). MAPKs are involved in the transduction of the signals of several cytokines, growth factors and proto-oncogenes [31].
For ovarian carcinomas, important hormones using the ERK pathway via G-protein coupled receptors are Gonadotropins and Gonadotropin-releasing hormones. In the beginning of their signal transduction cascade, the extracellular mitogen binds to the membrane receptor, which allows KRAS (which yields GTPase function) to exchange its guanosine diphosphate (GDP) for guanosine triphosphate (GTP) and to change to its active form. Thus, it can activate BRAF, which activates MEK and consecutively ERK is activated. ERK can subsequently activate transcription factors, such as myc or elk-1.
The MAPK pathway has oncogenic potential, either through permanent signaling activity as a result of KRAS or BRAF mutation, or by involvement of induction of cell replication. Since activation or overexpression of upstream factors like KRAS or BRAF can lead to constitutive activation of ERK, this may in turn activate downstream protein kinases or transcription factors that are likely to enhance tumor development [32,33].
MAPKs also play a role in the stimulation of ovarian cancer cell growth by membrane receptor signals for Gonadotropins. Gonadotropins are a group of hormones to which belong the follicle stimulating hormone (FSH), the luteinizing hormone (LH) and human chorionic gonadotropin (hCG). FSH and LH receptors are often expressed on ovarian carcinoma cells, and may therefore contribute to signaling transduction by MAPK [34,35].
2.2.3. EGFR and the Consecutive Activation of AKT
Epidermal growth factor receptor (EGFR) is expressed in 70% of ovarian carcinomas [36]. It can be activated by various ligands, such as EGF and TGF [37] and plays a role in enhancing and inhibiting tumor survival [38–40]. EGFR is also involved in tumor infiltration, metastasis and angiogenesis [41,42]. AKT is a major downstream factor of EGFR signaling [43]. Upon ligand binding to EGFR, AKT is activated by phosphorylation at Ser473 [43]. AKT is regularly overexpressed in OC and is associated with poor prognosis and aggressive tumor behavior [44,45]. Since the EGFR/AKT pathway is involved in various aspects of cancer proliferation like angiogenesis and metastasis, it is currently considered as an attractive target for therapeutic intervention.
2.2.4. Integrin Inhibitors
Lately, research has been done on the application of integrin inhibitors as potential therapeutic agents in ovarian carcinoma. The initial step in ovarian carcinoma dissemination occurs by the attachment of carcinoma cells onto the peritoneal surface via integrins, and therefore targeting integrins seems a rational therapy approach. However, no integrin inhibitors have shown favorable effects so far [46].
2.2.5. GRP78 Expression
Another recent article proposes GRP78 as a drug delivery system targeting ovarian carcinoma cells. GRP78 upregulation is a cellular mechanism of response, caused by endoplasmic reticulum stress, which is commonly found in tumor cells. Since GRP78 is abundantly found on ovarian carcinoma cell surfaces, the authors suggest the use of GRP78 as a delivery system for cytotoxic substances [47].
2.2.6. The p38alpha Pathway
The p38alpha pathway has recently been the focus of cancer research. Small compound inhibitors of p38alpha have already been evaluated in clinical trials showing promising results and may present a future therapeutic option for ovarian carcinoma. [48].
3. Diagnosis of Ovarian Cancer: Biomarkers and Imaging Techniques
For the diagnosis of ovarian tumors Doppler ultrasound, MRT and computed tomography as well as the assessment of biomarkers may be used. Early detection of OC is necessary to improve overall-survival, since only 25% of ovarian cancers are detected at stage I [49]. Among the serum markers, CA-125 receives the most attention, but sensitivity and specificity are not high enough for its role as a single screening test. Its sensitivity can be enhanced by using a panel of biomarkers. In addition, monitoring of biomarkers over time may be of value [49]. At present, the combination of transvaginal sonography and the evaluation of biomarkers are standard for OC diagnosis. An algorithm has been developed based on serial CA-125 values which refers patients at high risk for OC to transvaginal sonography [50].
Nearly 2% of adnexal masses turn out to be carcinomas or borderline tumors [51]. According to Marret, every suspicious ovarian mass would need expert sonography. Transvaginal sonography has considerable advantages compared to conventional transabdominal sonography. It is important to look for papillary formations inside ovarian cysts and for non-hyperechoic solid components, since these features are strong predictors of malignancy [51]. The evaluation of tumor vascularity by Doppler energy is especially useful to distinguish benign from malignant lesions [51]. Conventional ultrasound supplemented with three-dimensional (3D) ultrasound and three-dimensional power-Doppler (3DPD) ultrasound seems to be useful for the preoperative distinction of ovarian lesions [52].
CA-125 is the most valuable tumor marker for ovarian cancer. According to a study in which patients with ovarian metastases were compared to patients with primary OC, a CA-125 level >170 U/mL predicted primary ovarian cancer in >95% of the patients. In this study, CT imaging was also performed. In patients with primary OC, the CT scan rather than ultrasound showed omental involvement of the ovarian tumor mass and ascites, in comparison to ovarian metastases [53].
Additionally, it seems necessary to evaluate biomarkers to achieve higher levels of diagnostic sensitivity and specificity. Currently, more than 30 biomarkers are tested alone and also in combination with CA-125, e.g., mesothelin, osteopontin or kallikrein [50]. Mass spectroscopy of a patient’s serum is a novel approach to diagnosis. A specific pattern of peaks in the mass spectroscopy has been found, that is predictive for OC [50]. Relevant cancer markers are now determined by several study groups and put on platforms to permit the simultaneous assessment of a panel of markers using only small volumes of serum [50]. It has been demonstrated that the diagnostic value to predict malignancy is higher when a combination of biomarkers, as e.g., Human Epididymal Protein 4 (HE4), CA-125 and carcino-embryonic antigen (CEA) are determined. These factors also have to take into account the patient’s age, compared to the determination of CA-125 alone [54].
Recent data indicate that the folate-receptor 1 (FOLR1) is significantly elevated in the serum of OC patients compared to healthy controls and patients with benign gynecological tumors. FOLR1 strongly correlated with CA-125 and may be a potential candidate to serve as a biomarker for OC [55].
Recently, a method has been developed to quantify cancer biomarkers in biological fluids using small optical microresonators that support whispering gallery mode resonance. These optical microresonators are emerging as a new promising and powerful method for the detection of biomarkers in complex biological fluids by biosensing. Huckabay et al. report a method which allows detecting the OC marker CA-125 in buffer via whispering gallery mode imaging using a technique based on fluorescence imaging. In addition, the OC markers osteopontin and prolactin have also been investigated [56].
There is also a new optical imaging technique, partial wave spectroscopic microscopy that can assess the nanoscale macromolecular fluctuations of density within cells using a biomarker. The authors, who developed this novel technique, investigated endometrial and endocervical columnar cells referring to the concept of field carcinogenesis. This evaluation shows that there is a significant increase of the investigated biomarkers in columnar epithelial cells of OC patients compared to the controls [57].
Summing up, diagnosis of OC shall be made using imaging techniques, first of all transvaginal sonography, plus measuring a panel of biomarkers [49].
4. Treatment Modalities
Currently, therapy of ovarian carcinoma is based on maximum primary surgical debulking and adjuvant chemotherapy including platinum and a taxane [58,59]. However, the recurrence rate is high despite of adequate primary treatment [60]. This is mainly due to late diagnosis since 70% of the cases are diagnosed at advanced stage (FIGO Stages IIB–IV) [61]. Nevertheless, only 10%–15% of ovarian carcinoma patients achieve long-term remission and overall five-year survival is lower than 25% [62–65]. In late stage disease, five-year survival is less than 40%. In contrast, five year survival is considerably higher in stage I–II disease with more than 80% [61].
Unfavorable prognosis is in part caused by the early development of chemotherapy resistance [66]. Even though initial response is as high as 70% to 80%, most patients ultimately die of recurrence [64,65]. Treatment of clear cell carcinomas by chemotherapy is particularly problematic as they may be chemoresistant [67,68].
Second-line treatment is needed in the majority of patients. Platinum sensitivity is a good predictor of response. Platinum refractory disease” and “platinum-resistant” disease has a bad prognosis while patients with a long interval between diagnosis and recurrence show a better survival. This disease is defined as “platinum sensitive”.
For recurrent ovarian carcinoma patients with partial platinum sensitivity, i.e., recurrence between 6 and 12 months after the end of platinum-based therapy, trabectedin, a marine-derived anticancer agent, has shown preferential activity [69]. It acts via binding to a DNA minor-groove [70].
The monoclonal antibody bevacizumab, a VEGF inhibitor, is approved for ovarian cancer in the first line and in platinum-sensitive recurrence [60,71,72]. Bevacizumab causes hypertension in a significant proportion of patients. The greatest effect of bevacizumab was seen in patients with a high risk for progression, i.e., extensive disease and significant residual tumors. Bevacizumab can decrease ascites in ovarian carcinoma [73].
The mammalian target of rapamycin (mTOR) is responsible for cell growth and proliferation, interacting with VEGF and platelet derived growth factor (PDGF); the latter results in activated angiogenesis [74]. In clear cell ovarian carcinoma mTOR inhibitors have single-agent activity [75]. MTOR-inhibitors might be particularly effective in combination with bevacizumab since synergistic effects have been detected [76–78].
Poly-ADP-ribose polymerase inhibitors (PARP inhibitors) belong to a family of multifunctional enzymes with promising effects in ovarian carcinomas featuring BRCA1 or 2 mutations. These drugs block base excision repair and lead to the accumulation of DNA single-strand breaks. The latter subsequently cause DNA double-strand breaks at replication forks [69]. In normal cells these double-strand breaks are repaired in the presence of the tumor suppressor proteins BRCA1 and 2 [69]. In the absence of these proteins the lesions cannot be repaired, resulting in cell death. Thus, PARP inhibitors are suitable for the treatment of tumors with dysfunctional DNA repair. Three phase II studies with the PARP inhibitors olaparib and iniparib have demonstrated activity in platinum-sensitive ovarian carcinoma [78–81]. A preliminary study has demonstrated that ovarian carcinoma patients with BRCA1 or 2 mutations respond better to olaparib than those without mutations [80]. Olaparib seems to be associated with improved progression-free survival after conventional chemotherapy [79] and therapeutic response in both platinum-resistant and platinum-refractory disease [82].
Research is also focusing on epidermal growth factor receptor (EGFR) dependent pathways [58]. The EGFR receptor is overexpressed in 30%–98% of ovarian carcinoma [83]. The EGFR antibody cetuximab and the EGFR tyrosine kinase inhibitors lapatinib and erlotinib have not shown clinically significant activity in ovarian carcinoma yet [84,85] but may cause severe toxic and hematologic side effects [86,87].
Reports on Her2 expression in OC show divergent results [74]. Both overexpression and amplification are more prevalent in high-grade serous carcinomas, whereas low-grade serous and endometrioid carcinomas usually do not overexpress Her2 [88]. A few studies have shown moderate activity of anti-Her2 therapy with trastuzumab and pertuzumab [89,90]. Anti-Her2 therapy has shown particular activity in patients with Her2 overexpression in preliminary studies [90].
Farletuzumab is a humanized, IgG monoclonal antibody with high affinity for folate receptor alpha, a 38 kDa protein that is overexpressed in about 90% of OC [91]. The degree of folate receptor alpha expression correlates with tumor stage and grade [92]. In normal tissue, folate receptor alpha is largely absent, making it a relevant and attractive therapeutic target [91,93]. Farletuzumab has shown good antitumoral activity in preclinical xenograft models and has shown promising results in early phase trials [91,92]. A phase 1 dose escalation study has shown no dose-limiting toxic side effects or severe adverse effects [92]. A phase 2 efficacy and safety study using a combination of farletuzumab with carboplatin and taxane in patients with platinum-sensitive OC showed improved response rates and a longer time to progression [92]. The combination of farletuzumab, carboplatin and Pegylated Liposomal Doxorubicine (PLD) has a good safety profile, according to a study with platinum-sensitive OC patients following first or second relapse [92].
Malignant ascites affects about 10% of patients suffering from recurrent OC [94]. The concomitant symptoms include abdominal pressure, dyspnea, bloating, pelvic pain and bowel or bladder dysfunction. Treatment options for malignant ascites in OC patients include the use of antiangiogenic agents, namely bevacizumab and vascular endothelial growth factor inhibitors and also nonangiogenic drugs such as catumaxomab [94]. Catumaxomab is a rat/murine hybrid bispecific (anti-human epithelial cell adhesion molecule [EpCAM] and anti-CD3) monoclonal antibody [95]. Treatment of malignant ascites with paracentesis alone is much less effective than paracentesis followed by intraperitoneal catumaxomab treatment. Paracentesis-free survival was significantly longer, according to a phase II/III trial with patients suffering from recurrent, symptomatic malignant ascites [95]. Additionally, catumaxomab treatment was associated with a reduction of ascites signs and symptoms and with delayed deterioration regarding health-related quality of life. Generally, catumaxomab is well tolerated. The most frequent adverse effects include cytokine-release-related symptoms, but these were mostly mild and manageable with standard antipyretics [95].
Epigenetic changes in cells, such as hypoacetylation of histones and abnormal DNA methylation, may also promote tumorigenesis and lead to chemotherapy resistance. A phase II study with decitabine, an agent leading to DNA hypomethylation, has shown effectivity in platinum-resistant disease [78,96]. Currently, the histone deacetylase inhibitor belinostat and the proteosome inhibitor carfilzomib are evaluated [73].
The MAPK/ERK pathway can contribute to therapy induced tumor-growth suppression. In particular, the synthetic retinoid CD437 seems to be capable of inhibiting growth and inducing apoptosis in the ovarian cancer cell line CA-OV-3. In addition, p38, which influences growth inhibition, seems to be induced independently [97]. The response of cancer cells to the chemotherapeutic drug cisplatin is dependent on MAPKs, by induction or suppression of apoptosis [98].
The MAPKs and BRAF are involved in cellular growth regulation and can trigger carcinogenesis [73]. In low-grade ovarian carcinoma, BRAF mutations are frequently found and lead to activation of the MAPK-pathway [73]. Thus, the BRAF/MAPK pathway is a potential therapeutic target. BRAF inhibitors such as vemurafenib and dabrafenib and the MEK inhibitor trametinib have shown significant activity in BRAF-mutated melanoma. The MET tyrosine kinase cell surface receptor is linked to this pathway and its inhibition leads to the suppression of RAF and MAP kinase activity. Recently, the MET inhibitor cabozantinib has shown efficacy in ovarian carcinoma independently from platinum sensitivity [78].
Recently, some anti-inflammatory phytochemicals have been tested, which may change the immunosuppressive microenvironment [73]. Such phytochemicals are mainly natural colorants extracted from fruits or vegetables. They have an inhibitory effect on the arachidonic acid pathway and therefore act similarly to non-steroidal anti-rheumatics [99]. Phytochemicals include the following flavonoids: apigenin, baicalein, genistein, luteolin, quercetin, wogonin curcumin, and the antioxidants epigallocatechingallate and oridonin. They repress NF-kappaB, a proinflammatory transcription factor and inhibit proinflammatory cytokines [73,100–102]. NF-κB has a paradoxic role in carcinogenesis. On one hand activated NF-κB promotes apoptosis, but on the other hand, inhibition of NF-κB may lead to pro-apoptotic effects and inhibits chemotherapy-resistant ovarian carcinoma cell growth [103]. Anti-inflammatory phytochemicals also stabilize p53, a tumor suppressor gene [73,104]. These effects may result in the prevention or delay of resistance to chemotherapy [73]. Apigenin, genistein, kaempferol, luteolin, and quercetin have been demonstrated to inhibit VEGF in vitro [73,105]. Oridonin and wogonin may also contribute to the suppression of cancer stem cells by down-regulating the surface marker EpCAM [73].
The role of non-steroidal anti-inflammatory drugs (NSAIDs) in ovarian carcinoma is incompletely understood. There is epidemiological evidence for an association of increased NSAID/aspirin intake and the prevention of colon cancer [73,106]. A meta-analysis and one prospective cohort study on the association of NSAID intake and ovarian carcinoma risk did not find a risk reduction [73,107]. In another trial, the beneficial effect of NSAIDs in the prevention of ovarian carcinogenesis was demonstrated [73,108].
A potential next-generation therapy for ovarian carcinoma is the use of microRNA therapeutics [73]. In mouse models, let-7 has been demonstrated to repress cell proliferation in breast cancer cells [109,110]. However, at present, their mechanisms of action are poorly understood [73].
5. Discussion and Conclusion
Ongoing studies of targeted agents in conjunction with chemotherapy will reveal whether other options than bevacizumab will be effective in ovarian carcinoma. Since these agents are expensive and may also cause significant toxicity, novel specific biomarkers are urgently needed to predict their efficacy and to justify their use. Mouse models are good candidates to test new approaches to ovarian carcinoma therapy.
The fact that different histological types of ovarian carcinoma feature specific signaling characteristics, may be used to target molecular objectives and to provide individualized therapy options [111]. There is growing evidence that epithelial ovarian cancer is a heterogeneous disease that needs a tailored approach based on the underlying molecular genetic changes. Several drugs targeting components of the phosphoinositide 3-kinase/protein kinase B (PKB)/Akt (PI3K/Akt) pathway have already been designed and some have also been tested in clinical trials [111]. However, since there is minimal experience with these drugs and only a few patients are willing to take the risk of testing, mouse models have been established to gain more preclinical information. Wu et al. have developed a mouse model of endometrioid adenocarcinoma by inactivating the tumor suppressor genes PTEN and Adenomatous polyposis coli (APC) in the murine ovarian epithelium [59]. For this purpose, the “Cre/lox” system was used. In the ovarian carcinoma mouse model, the mice had loxP sites in the introns of the PTEN and APC genes. A virus expressing the Cre recombinase was injected into the murine ovarian bursa. Subsequently, the mice developed tumors that were similar to human ovarian endometrioid tumors. In these mice, the neoplasms rapidly progressed and all mice died within 19 weeks after Cre had been delivered to the ovarian epithelium. Treatment with Rapamycin, an inhibitor of mTOR (a downstream effector of AKT) distinctly showed growth inhibition of the cancers in the mouse model [111]. The effects on tumor growth were investigated with non-invasive methods taking advantage of bioluminescence imaging. In the future, such mouse models are expected to provide further insight into the biology of OC and to reveal new putative points of action for targeted treatment.
Further development of our understanding of ovarian cancer pathogenesis and a deeper knowledge of the underlying molecular alterations will be crucial for a successful implementation of targeted therapy of ovarian carcinoma. It will be the pathologists’ role to analyze tumor tissue for key molecular targets in ovarian carcinoma, as is today routinely performed for targeted therapy of colorectal and non-small cell lung carcinoma and melanoma.
Acknowledgements
We thank the “Kurt und Senta Herrmann-Stiftung” (to J.H.) for supporting this work. The research also received support from the Innovative Medicines Initiative Joint Undertaking under grant agreement n° [115234], composed of financial contribution from the European Union’s Seventh Framework Programme (FP7/2007-2013) and EFPIA companies (to J.H.).
References
- 1.McCluggage W.G. Morphological subtypes of ovarian carcinoma: A review with emphasis on new developments and pathogenesis. Pathology. 2011;43:420–432. doi: 10.1097/PAT.0b013e328348a6e7. [DOI] [PubMed] [Google Scholar]
- 2.Shih I., Ho C.M., Nakayama K., Salani R. Pathogenesis and new therapeutic targets of ovarian cancer. J. Oncol. 2012;2012:867512. doi: 10.1155/2012/867512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaku T., Ogawa S., Kawano Y., Ohishi Y., Kobayashi H., Hirakawa T., Nakano H. Histological classification of ovarian cancer. Med. Electron. Microsc. 2003;36:9–17. doi: 10.1007/s007950300002. [DOI] [PubMed] [Google Scholar]
- 4.Lax S. Serous genital carcinoma: Molecular pathogenesis and the role of tubal fimbria. Pathologe. 2009;30:210–216. doi: 10.1007/s00292-009-1215-3. [DOI] [PubMed] [Google Scholar]
- 5.Levanon K., Crum C., Drapkin R. New insights into the pathogenesis of serous ovarian cancer and its clinical impact. J. Clin. Oncol. 2008;26:5284–5293. doi: 10.1200/JCO.2008.18.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callahan M.J., Crum C.P., Medeiros F., Kindelberger D.W., Elvin J.A., Garber J.E., Feltmate C.M., Berkowitz R.S., Muto M.G. Primary fallopian tube malignancies in BRCA-positive women undergoing surgery for ovarian cancer risk reduction. J. Clin. Oncol. 2007;25:3985–3990. doi: 10.1200/JCO.2007.12.2622. [DOI] [PubMed] [Google Scholar]
- 7.Crum C.P., McKeon F.D., Xian W. BRCA, the oviduct, and the space and time continuum of pelvic serous carcinogenesis. Int. J. Gynecol. Cancer. 2012;22:S29–S34. doi: 10.1097/IGC.0b013e31824d7269. [DOI] [PubMed] [Google Scholar]
- 8.Crum C.P., McKeon F.D., Xian W. The oviduct and ovarian cancer: Causality, clinical implications, and “targeted prevention”. Clin. Obstet. Gynecol. 2012;55:24–35. doi: 10.1097/GRF.0b013e31824b1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harrison M.L., Jameson C., Gore M.E. Mucinous ovarian cancer. Int. J. Gynecol. Cancer. 2008;18:209–214. doi: 10.1111/j.1525-1438.2007.01022.x. [DOI] [PubMed] [Google Scholar]
- 10.Pearce C.L., Templeman C., Rossing M.A., Lee A., Near A.M., Webb P.M., Nagle C.M., Doherty J.A., Cushing-Haugen K.L., Wicklund K.G., et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: A pooled analysis of case-control studies. Lancet Oncol. 2012;13:385–394. doi: 10.1016/S1470-2045(11)70404-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCluggage W.G. My approach to and thoughts on the typing of ovarian carcinomas. J. Clin. Pathol. 2008;61:152–163. doi: 10.1136/jcp.2007.049478. [DOI] [PubMed] [Google Scholar]
- 12.Kurman R.J., Shih I. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer—Shifting the paradigm. Hum. Pathol. 2011;42:918–931. doi: 10.1016/j.humpath.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kshirsagar M., Jiang W., Shih I. DNA damage response is prominent in ovarian high-grade serous carcinomas, especially those with Rsf-1 (HBXAP) overexpression. J. Oncol. 2012;2012:621685. doi: 10.1155/2012/621685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurman R.J., Shih I. The origin and pathogenesis of epithelial ovarian cancer: A proposed unifying theory. Am. J. Surg. Pathol. 2010;34:433–443. doi: 10.1097/PAS.0b013e3181cf3d79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiegand K.C., Shah S.P., Al-Agha O.M., Zhao Y., Tse K., Zeng T., Senz J., McConechy M.K., Anglesio M.S., Kalloger S.E., et al. ARID1A Mutations in Endometriosis-Associated Ovarian Carcinomas. N. Engl. J. Med. 2010;363:1532–1543. doi: 10.1056/NEJMoa1008433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Szabo C.I., King M.C. Inherited breast and ovarian cancer. Hum. Mol. Genet. 1995;4:1811–1817. doi: 10.1093/hmg/4.suppl_1.1811. [DOI] [PubMed] [Google Scholar]
- 17.Collins N., McManus R., Wooster R., Mangion J., Seal S., Lakhani S.R., Ormiston W., Daly P.A., Ford D., Easton D.F. Consistent loss of the wild type allele in breast cancers from a family linked to the BRCA2 gene on chromosome 13q12–13. Oncogene. 1995;10:1673–1675. [PubMed] [Google Scholar]
- 18.Smith S.A., Easton D.F., Evans D.G., Ponder B.A. Allele losses in the region 17q12–21 in familial breast and ovarian cancer involve the wild-type chromosome. Nat. Genet. 1992;2:128–131. doi: 10.1038/ng1092-128. [DOI] [PubMed] [Google Scholar]
- 19.Scully R., Livingston D.M. In search of the tumour-suppressor functions of BRCA1 and BRCA2. Nature. 2000;408:429–432. doi: 10.1038/35044000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scully R., Puget N., Vlasakova K. DNA polymerase stalling, sister chromatid recombination and the BRCA genes. Oncogene. 2000;19:6176–6183. doi: 10.1038/sj.onc.1203971. [DOI] [PubMed] [Google Scholar]
- 21.Paull T.T., Rogakou E.P., Yamazaki V., Kirchgessner C.U., Gellert M., Bonner W.M. A critical role for histone H2AX in recruitment of repair factors to nuclear foci after DNA damage. Curr. Biol. 2000;10:886–895. doi: 10.1016/s0960-9822(00)00610-2. [DOI] [PubMed] [Google Scholar]
- 22.Bau D.T., Fu Y.P., Chen S.T., Cheng T.C., Yu J.C., Wu P.E., Shen C.Y. Breast cancer risk and the DNA double-strand break end-joining capacity of nonhomologous end-joining genes are affected by BRCA1. Cancer Res. 2004;64:5013–5019. doi: 10.1158/0008-5472.CAN-04-0403. [DOI] [PubMed] [Google Scholar]
- 23.Espejel S., Franco S., Rodriguez-Perales S., Bouffler S.D., Cigudosa J.C., Blasco M.A. Mammalian Ku86 mediates chromosomal fusions and apoptosis caused by critically short telomeres. EMBO J. 2002;21:2207–2219. doi: 10.1093/emboj/21.9.2207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Deng C.X., Scott F. Role of the tumor suppressor gene brca1 in genetic stability and mammary gland tumor formation. Oncogene. 2000;19:1059–1064. doi: 10.1038/sj.onc.1203269. [DOI] [PubMed] [Google Scholar]
- 25.Futreal P.A., Liu Q., Shattuck-Eidens D., Cochran C., Harshman K., Tavtigian S., Bennett L.M., Haugen-Strano A., Swensen J., Miki Y. BRCA1 mutations in primary breast and ovarian carcinomas. Science. 1994;266:120–122. doi: 10.1126/science.7939630. [DOI] [PubMed] [Google Scholar]
- 26.Cleton-Jansen A.M., Collins N., Lakhani S.R., Weissenbach J., Devilee P., Cornelisse C.J., Stratton M.R. Loss of heterozygosity in sporadic breast tumours at the BRCA2 locus on chromosome 13q12–q13. Br. J. Cancer. 1995;72:1241–1244. doi: 10.1038/bjc.1995.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Welcsh P.L., King M.C. BRCA1 and BRCA2 and the genetics of breast and ovarian cancer. Hum. Mol. Genet. 2001;10:705–713. doi: 10.1093/hmg/10.7.705. [DOI] [PubMed] [Google Scholar]
- 28.Singer G., Oldt R., III, Cohen Y., Wang B.G., Sidransky D., Kurman R.J., Shih I. Mutations in BRAF and KRAS characterize the development of low-grade ovarian serous carcinoma. J. Natl. Cancer Inst. 2003;95:484–486. doi: 10.1093/jnci/95.6.484. [DOI] [PubMed] [Google Scholar]
- 29.Nakayama K., Nakayama N., Kurman R.J., Cope L., Pohl G., Samuels Y., Velculescu V.E., Wang T.L., Shih I. Sequence mutations and amplification of PIK3CA and AKT2 genes in purified ovarian serous neoplasms. Cancer. Biol. Ther. 2006;5:779–785. doi: 10.4161/cbt.5.7.2751. [DOI] [PubMed] [Google Scholar]
- 30.Wan P.T., Garnett M.J., Roe S.M., Lee S., Niculescu-Duvaz D., Good V.M., Jones C.M., Marshall C.J., Springer C.J., Barford D., et al. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell. 2004;116:855–867. doi: 10.1016/s0092-8674(04)00215-6. [DOI] [PubMed] [Google Scholar]
- 31.Olson J.M., Hallahan A.R. P38 MAP kinase: A convergence point in cancer therapy. Trends Mol. Med. 2004;10:125–129. doi: 10.1016/j.molmed.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Peyssonnaux C., Eychene A. The Raf/MEK/ERK pathway: New concepts of activation. Biol. Cell. 2001;93:53–62. doi: 10.1016/s0248-4900(01)01125-x. [DOI] [PubMed] [Google Scholar]
- 33.Allen L.F., Sebolt-Leopold J., Meyer M.B. CI-1040 (PD184352), a targeted signal transduction inhibitor of MEK (MAPKK) Semin. Oncol. 2003;30:105–116. doi: 10.1053/j.seminoncol.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 34.Zheng W., Lu J.J., Luo F., Zheng Y., Feng Y., Felix J.C., Lauchlan S.C., Pike M.C. Ovarian epithelial tumor growth promotion by follicle-stimulating hormone and inhibition of the effect by luteinizing hormone. Gynecol. Oncol. 2000;76:80–88. doi: 10.1006/gyno.1999.5628. [DOI] [PubMed] [Google Scholar]
- 35.Choi K.C., Kang S.K., Tai C.J., Auersperg N., Leung P.C. Follicle-stimulating hormone activates mitogen-activated protein kinase in preneoplastic and neoplastic ovarian surface epithelial cells. J. Clin. Endocrinol. Metab. 2002;87:2245–2253. doi: 10.1210/jcem.87.5.8506. [DOI] [PubMed] [Google Scholar]
- 36.Zeineldin R., Muller C.Y., Stack M.S., Hudson L.G. Targeting the EGF receptor for ovarian cancer therapy. J. Oncol. 2010;2010:414676. doi: 10.1155/2010/414676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nicholson R.I., Gee J.M., Harper M.E. EGFR and cancer prognosis. Eur. J. Cancer. 2001;37:S9–S15. doi: 10.1016/s0959-8049(01)00231-3. [DOI] [PubMed] [Google Scholar]
- 38.Fontanini G., Vignati S., Bigini D., Mussi A., Lucchi H., Angeletti C.A., Pingitore R., Pepe S., Basolo F., Bevilacqua G. Epidermal growth factor receptor (EGFr) expression in non-small cell lung carcinomas correlates with metastatic involvement of hilar and mediastinal lymph nodes in the squamous subtype. Eur. J. Cancer. 1995;31A:178–183. doi: 10.1016/0959-8049(93)00421-m. [DOI] [PubMed] [Google Scholar]
- 39.Jorissen R.N., Walker F., Pouliot N., Garrett T.P., Ward C.W., Burgess A.W. Epidermal growth factor receptor: Mechanisms of activation and signalling. Exp. Cell Res. 2003;284:31–53. doi: 10.1016/s0014-4827(02)00098-8. [DOI] [PubMed] [Google Scholar]
- 40.Turner T., Chen P., Goodly L.J., Wells A. EGF receptor signaling enhances in vivo invasiveness of du-145 human prostate carcinoma cells. Clin. Exp. Metastasis. 1996;14:409–418. doi: 10.1007/BF00123400. [DOI] [PubMed] [Google Scholar]
- 41.Casanova M.L., Larcher F., Casanova B., Murillas R., Fernandez-Acenero M.J., Villanueva C., Martinez-Palacio J., Ullrich A., Conti C.J., Jorcano J.L. A critical role for ras-mediated, epidermal growth factor receptor-dependent angiogenesis in mouse skin carcinogenesis. Cancer Res. 2002;62:3402–3407. [PubMed] [Google Scholar]
- 42.Lu Z., Jiang G., Blume-Jensen P., Hunter T. Epidermal growth factor-induced tumor cell invasion and metastasis initiated by dephosphorylation and downregulation of focal adhesion kinase. Mol. Cell. Biol. 2001;21:4016–4031. doi: 10.1128/MCB.21.12.4016-4031.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perrimon N. Signalling pathways initiated by receptor protein tyrosine kinases in drosophila. Curr. Opin. Cell Biol. 1994;6:260–266. doi: 10.1016/0955-0674(94)90145-7. [DOI] [PubMed] [Google Scholar]
- 44.Altomare D.A., Wang H.Q., Skele K.L., de Rienzo A., Klein-Szanto A.J., Godwin A.K., Testa J.R. AKT and mTOR phosphorylation is frequently detected in ovarian cancer and can be targeted to disrupt ovarian tumor cell growth. Oncogene. 2004;23:5853–5857. doi: 10.1038/sj.onc.1207721. [DOI] [PubMed] [Google Scholar]
- 45.Gao N., Flynn D.C., Zhang Z., Zhong X.S., Walker V., Liu K.J., Shi X., Jiang B.H. G1 cell cycle progression and the expression of G1 cyclins are regulated by PI3K/AKT/mTOR/p70S6K1 signaling in human ovarian cancer cells. Am. J. Physiol. Cell. Physiol. 2004;287:C281–C291. doi: 10.1152/ajpcell.00422.2003. [DOI] [PubMed] [Google Scholar]
- 46.Sawada K., Ohyagi-Hara C., Kimura T., Morishige K. Integrin inhibitors as a therapeutic agent for ovarian cancer. J. Oncol. 2012;2012:915140. doi: 10.1155/2012/915140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Delie F., Petignat P., Cohen M. GRP78 protein expression in ovarian cancer patients and perspectives for a drug-targeting approach. J. Oncol. 2012;2012:468615. doi: 10.1155/2012/468615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grossi V., Simone C. Special agents hunting down women silent killer: The emerging role of the p38alpha kinase. J. Oncol. 2012;2012:382159. doi: 10.1155/2012/382159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Badgwell D., Bast R.C., Jr Early detection of ovarian cancer. Dis. Markers. 2007;23:397–410. doi: 10.1155/2007/309382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bast R.C., Jr Early detection of ovarian cancer: New technologies in pursuit of a disease that is neither common nor rare. Trans. Am. Clin. Climatol. Assoc. 2004;115:233–247. ; discussion 247–248. [PMC free article] [PubMed] [Google Scholar]
- 51.Marret H. Doppler ultrasonography in the diagnosis of ovarian cysts: Indications, pertinence and diagnostic criteria. J. Gynecol. Obstet. Biol. Reprod. (Paris) 2001;30:S20–S33. [PubMed] [Google Scholar]
- 52.Vrachnis N., Sifakis S., Samoli E., Kappou D., Pavlakis K., Iliodromiti Z., Botsis D. Three-dimensional ultrasound and three-dimensional power doppler improve the preoperative evaluation of complex benign ovarian lesions. Clin. Exp. Obstet. Gynecol. 2012;39:474–478. [PubMed] [Google Scholar]
- 53.Bruchim I., Ben-Harim Z., Piura E., Tepper R., Fishman A. Preoperative clinical and radiological features of metastatic ovarian tumors. Arch. Gynecol. Obstet. 2013 doi: 10.1007/s00404-013-2776-1. [DOI] [PubMed] [Google Scholar]
- 54.Kondalsamy-Chennakesavan S., Hackethal A., Bowtell D., Obermair A. On behalf of the Australian Ovarian Cancer Study Group. Differentiating stage 1 epithelial ovarian cancer from benign ovarian tumours using a combination of tumour markers HE4, CA125, and CEA and patient’s age. Gynecol. Oncol. 2013 doi: 10.1016/j.ygyno.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 55.Leung F., Dimitromanolakis A., Kobayashi H., Diamandis E.P., Kulasingam V. Folate-receptor 1 (FOLR1) protein is elevated in the serum of ovarian cancer patients. Clin. Biochem. 2013 doi: 10.1016/j.clinbiochem.2013.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Huckabay H.A., Wildgen S.M., Dunn R.C. Label-free detection of ovarian cancer biomarkers using whispering gallery mode imaging. Biosens. Bioelectron. 2013;45C:223–229. doi: 10.1016/j.bios.2013.01.072. [DOI] [PubMed] [Google Scholar]
- 57.Damania D., Roy H.K., Kunte D., Hurteau J.A., Subramanian H., Cherkezyan L., Krosnjar N., Shah M., Backman V. Insights into the field carcinogenesis of ovarian cancer based on the nanocytology of endocervical and endometrial epithelial cells. Int. J. Cancer. 2013 doi: 10.1002/ijc.28122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Han E.S., Lin P., Wakabayashi M. Current status on biologic therapies in the treatment of epithelial ovarian cancer. Curr. Treat. Opt. Oncol. 2009;10:54–66. doi: 10.1007/s11864-009-0100-x. [DOI] [PubMed] [Google Scholar]
- 59.Markman M. Pharmaceutical management of ovarian cancer: Current status. Drugs. 2008;68:771–789. doi: 10.2165/00003495-200868060-00004. [DOI] [PubMed] [Google Scholar]
- 60.Han E.S., Monk B.J. Bevacizumab in the treatment of ovarian cancer. Expert Rev. Anticancer Ther. 2007;7:1339–1345. doi: 10.1586/14737140.7.10.1339. [DOI] [PubMed] [Google Scholar]
- 61.Burges A., Schmalfeldt B. Ovarian cancer: Diagnosis and treatment. Dtsch. Arztebl Int. 2011;108:635–641. doi: 10.3238/arztebl.2011.0635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Neijt J.P., ten Bokkel Huinink W.W., van der Burg M.E., van Oosterom A.T., Willemse P.H., Vermorken J.B., van Lindert A.C., Heintz A.P., Aartsen E., van Lent M. Long-term survival in ovarian cancer. Mature data from the netherlands joint study group for ovarian cancer. Eur. J. Cancer. 1991;27:1367–1372. doi: 10.1016/0277-5379(91)90011-2. [DOI] [PubMed] [Google Scholar]
- 63.Copeland L.J., Vaccarello L., Lewandowski G.S. Second-look laparotomy in epithelial ovarian cancer. Obstet. Gynecol. Clin. North Am. 1994;21:155–166. [PubMed] [Google Scholar]
- 64.Rubin S.C., Hoskins W.J., Hakes T.B., Markman M., Cain J.M., Lewis J.L., Jr Recurrence after negative second-look laparotomy for ovarian cancer: Analysis of risk factors. Am. J. Obstet. Gynecol. 1988;159:1094–1098. doi: 10.1016/0002-9378(88)90420-6. [DOI] [PubMed] [Google Scholar]
- 65.Zhang L., Conejo-Garcia J.R., Katsaros D., Gimotty P.A., Massobrio M., Regnani G., Makrigiannakis A., Gray H., Schlienger K., Liebman M.N., et al. Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N. Engl. J. Med. 2003;348:203–213. doi: 10.1056/NEJMoa020177. [DOI] [PubMed] [Google Scholar]
- 66.Armstrong D.K. Relapsed ovarian cancer: Challenges and management strategies for a chronic disease. Oncologist. 2002;7:20–28. doi: 10.1634/theoncologist.7-suppl_5-20. [DOI] [PubMed] [Google Scholar]
- 67.Morgan R.J., Jr, Alvarez R.D., Armstrong D.K., Burger R.A., Castells M., Chen L.M., Copeland L., Crispens M.A., Gershenson D., Gray H., et al. Ovarian cancer, version 3.2012. J. Natl. Compr. Cancer Netw. 2012;10:1339–1349. doi: 10.6004/jnccn.2012.0140. [DOI] [PubMed] [Google Scholar]
- 68.National Comprehensive Cancer Network (NCCN) NCCN Clinical Practice Guidelines in Oncology. National Comprehensive Cancer Network, Inc; Washington, DC, USA: 2006. [Google Scholar]
- 69.Kim A., Ueda Y., Naka T., Enomoto T. Therapeutic strategies in epithelial ovarian cancer. J. Exp. Clin. Cancer Res. 2012;31:14. doi: 10.1186/1756-9966-31-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Monk B.J., Herzog T.J., Kaye S.B., Krasner C.N., Vermorken J.B., Muggia F.M., Pujade-Lauraine E., Lisyanskaya A.S., Makhson A.N., Rolski J., et al. Trabectedin plus pegylated liposomal doxorubicin in recurrent ovarian cancer. J. Clin. Oncol. 2010;28:3107–3114. doi: 10.1200/JCO.2009.25.4037. [DOI] [PubMed] [Google Scholar]
- 71.Perren T.J., Swart A.M., Pfisterer J., Ledermann J.A., Pujade-Lauraine E., Kristensen G., Carey M.S., Beale P., Cervantes A., Kurzeder C., et al. A phase 3 trial of bevacizumab in ovarian cancer. N. Engl. J. Med. 2011;365:2484–2496. doi: 10.1056/NEJMoa1103799. [DOI] [PubMed] [Google Scholar]
- 72.Aghajanian C., Blank S.V., Goff B.A., Judson P.L., Teneriello M.G., Husain A., Sovak M.A., Yi J., Nycum L.R. OCEANS: A randomized, double-blind, placebo-controlled phase III trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent epithelial ovarian, primary peritoneal, or fallopian tube cancer. J. Clin. Oncol. 2012;30:2039–2045. doi: 10.1200/JCO.2012.42.0505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen S.S., Michael A., Butler-Manuel S.A. Advances in the treatment of ovarian cancer: A potential role of antiinflammatory phytochemicals. Discov. Med. 2012;13:7–17. [PubMed] [Google Scholar]
- 74.Tagawa T., Morgan R., Yen Y., Mortimer J. Ovarian cancer: Opportunity for targeted therapy. J. Oncol. 2012;2012:682480. doi: 10.1155/2012/682480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mabuchi S., Kawase C., Altomare D.A., Morishige K., Sawada K., Hayashi M., Tsujimoto M., Yamoto M., Klein-Szanto A.J., Schilder R.J., et al. MTOR is a promising therapeutic target both in cisplatin-sensitive and cisplatin-resistant clear cell carcinoma of the ovary. Clin. Cancer Res. 2009;15:5404–5413. doi: 10.1158/1078-0432.CCR-09-0365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Moroney J., Fu S., Moulder S., Falchook G., Helgason T., Levenback C., Hong D., Naing A., Wheler J., Kurzrock R. Phase I study of the antiangiogenic antibody bevacizumab and the mTOR/hypoxia-inducible factor inhibitor temsirolimus combined with liposomal doxorubicin: Tolerance and biological activity. Clin. Cancer Res. 2012;18:5796–5805. doi: 10.1158/1078-0432.CCR-12-1158. [DOI] [PubMed] [Google Scholar]
- 77.Alvarez E.A., Brady W.E., Walker J., Rotmensch J., Zhou X.C., Kendrick J.E., Yamada S.D., Schilder J.M., Cohn D., Harrison C.R., et al. Phase II trial of combination bevacizumab and temsirolimus in the treatment of recurrent or persistent endometrial carcinoma: A gynecologic oncology group study. Gynecol. Oncol. 2012;129:22–27. doi: 10.1016/j.ygyno.2012.12.022. [DOI] [PubMed] [Google Scholar]
- 78.Tewari K.S. American Society of Clinical Oncology 2012 Annual Meeting: highlights from the gynecologic oncology track. Int. J. Gynecol. Cancer. 2012;22:1634–1639. doi: 10.1097/IGC.0b013e318270febe. [DOI] [PubMed] [Google Scholar]
- 79.Ledermann J.A., Harter P., Gourley C., Friedlander M., Vergote I.B., Rustin G.J.S., Scott C., Meier W., Shapira-Frommer R., Safra T., et al. Phase II randomized placebo-controlled study of olaparib (AZD2281) in patients with platinum-sensitive relapsed serous ovarian cancer (PSR SOC) J. Clin. Oncol. 2011;29:5003. [Google Scholar]
- 80.Gelmon K.A., Tischkowitz M., Mackay H., Swenerton K., Robidoux A., Tonkin K., Hirte H., Huntsman D., Clemons M., Gilks B., et al. Olaparib in patients with recurrent high-grade serous or poorly differentiated ovarian carcinoma or triple-negative breast cancer: A phase 2, multicentre, open-label, non-randomised study. Lancet Oncol. 2011;12:852–861. doi: 10.1016/S1470-2045(11)70214-5. [DOI] [PubMed] [Google Scholar]
- 81.Sessa C. Update on PARP1 inhibitors in ovarian cancer. Ann. Oncol. 2011;22:viii72–viii76. doi: 10.1093/annonc/mdr528. [DOI] [PubMed] [Google Scholar]
- 82.Fong P.C., Yap T.A., Boss D.S., Carden C.P., Mergui-Roelvink M., Gourley C., de Greve J., Lubinski J., Shanley S., Messiou C., et al. Poly(ADP)-ribose polymerase inhibition: Frequent durable responses in BRCA carrier ovarian cancer correlating with platinum-free interval. J. Clin. Oncol. 2010;28:2512–2519. doi: 10.1200/JCO.2009.26.9589. [DOI] [PubMed] [Google Scholar]
- 83.Gui T., Shen K. The epidermal growth factor receptor as a therapeutic target in epithelial ovarian cancer. Cancer Epidemiol. 2012;36:490–496. doi: 10.1016/j.canep.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 84.Konner J., Schilder R.J., DeRosa F.A., Gerst S.R., Tew W.P., Sabbatini P.J., Hensley M.L., Spriggs D.R., Aghajanian C.A. A phase II study of cetuximab/paclitaxel/carboplatin for the initial treatment of advanced-stage ovarian, primary peritoneal, or fallopian tube cancer. Gynecol. Oncol. 2008;110:140–145. doi: 10.1016/j.ygyno.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 85.Vasey P.A., Gore M., Wilson R., Rustin G., Gabra H., Guastalla J.P., Lauraine E.P., Paul J., Carty K., Kaye S., et al. A phase Ib trial of docetaxel, carboplatin and erlotinib in ovarian, fallopian tube and primary peritoneal cancers. Br. J. Cancer. 2008;98:1774–1780. doi: 10.1038/sj.bjc.6604371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Weroha S.J., Oberg A.L., Ziegler K.L., Dakhilm S.R., Rowland K.M., Hartmann L.C., Moore D.F., Jr, Keeney G.L., Peethambaram P.P., Haluska P. Phase II trial of lapatinib and topotecan (LapTop) in patients with platinum-refractory/resistant ovarian and primary peritoneal carcinoma. Gynecol. Oncol. 2011;122:116–120. doi: 10.1016/j.ygyno.2011.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Secord A.A., Blessing J.A., Armstrong D.K., Rodgers W.H., Miner Z., Barnes M.N., Lewandowski G., Mannel R.S. Gynecologic Oncology Group. Phase II trial of cetuximab and carboplatin in relapsed platinum-sensitive ovarian cancer and evaluation of epidermal growth factor receptor expression: A gynecologic oncology group study. Gynecol. Oncol. 2008;108:493–499. doi: 10.1016/j.ygyno.2007.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mano M.S., Awada A., di Leo A., Durbecq V., Paesmans M., Cardoso F., Larsimont D., Piccart M. Rates of topoisomerase II-Alpha and HER-2 gene amplification and expression in epithelial ovarian carcinoma. Gynecol. Oncol. 2004;92:887–895. doi: 10.1016/j.ygyno.2003.12.010. [DOI] [PubMed] [Google Scholar]
- 89.Bookman M.A., Darcy K.M., Clarke-Pearson D., Boothby R.A., Horowitz I.R. Evaluation of monoclonal humanized anti-HER2 antibody, trastuzumab, in patients with recurrent or refractory ovarian or primary peritoneal carcinoma with overexpression of HER2: A phase II trial of the gynecologic oncology group. J. Clin. Oncol. 2003;21:283–290. doi: 10.1200/JCO.2003.10.104. [DOI] [PubMed] [Google Scholar]
- 90.Gordon M.S., Matei D., Aghajanian C., Matulonis U.A., Brewer M., Fleming G.F., Hainsworth J.D., Garcia A.A., Pegram M.D., Schilder R.J., et al. Clinical activity of pertuzumab (rhuMAb 2C4), a HER dimerization inhibitor, in advanced ovarian cancer: Potential predictive relationship with tumor HER2 activation status. J. Clin. Oncol. 2006;24:4324–4332. doi: 10.1200/JCO.2005.05.4221. [DOI] [PubMed] [Google Scholar]
- 91.Spannuth W.A., Sood A.K., Coleman R.L. Farletuzumab in epithelial ovarian carcinoma. Expert Opin. Biol. Ther. 2010;10:431–437. doi: 10.1517/14712591003592069. [DOI] [PubMed] [Google Scholar]
- 92.Jelovac D., Armstrong D.K. Role of farletuzumab in epithelial ovarian carcinoma. Curr. Pharm. Des. 2012;18:3812–3815. doi: 10.2174/138161212802002698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Farrell C., Schweizer C., Wustner J., Weil S., Namiki M., Nakano T., Nakai K., Phillips M.D. Population pharmacokinetics of farletuzumab, a humanized monoclonal antibody against folate receptor alpha, in epithelial ovarian cancer. Cancer Chemother. Pharmacol. 2012;70:727–734. doi: 10.1007/s00280-012-1959-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Eskander R.N., Tewari K.S. Emerging treatment options for management of malignant ascites in patients with ovarian cancer. Int. J. Womens Health. 2012;4:395–404. doi: 10.2147/IJWH.S29467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Frampton J.E. Catumaxomab: In malignant ascites. Drugs. 2012;72:1399–1410. doi: 10.2165/11209040-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 96.Matei D., Fang F., Shen C., Schilder J., Arnold A., Zeng Y., Berry W.A., Huang T., Nephew K.P. Epigenetic resensitization to platinum in ovarian cancer. Cancer Res. 2012;72:2197–2205. doi: 10.1158/0008-5472.CAN-11-3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Holmes W.F., Soprano D.R., Soprano K.J. Early events in the induction of apoptosis in ovarian carcinoma cells by CD437: Activation of the p38 MAP kinase signal pathway. Oncogene. 2003;22:6377–6386. doi: 10.1038/sj.onc.1206694. [DOI] [PubMed] [Google Scholar]
- 98.Brozovic A., Osmak M. Activation of mitogen-activated protein kinases by cisplatin and their role in cisplatin-resistance. Cancer Lett. 2007;251:1–16. doi: 10.1016/j.canlet.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 99.Chen S. Natural products triggering biological targets—A review of the anti-inflammatory phytochemicals targeting the arachidonic acid pathway in allergy asthma and rheumatoid arthritis. Curr. Drug Targets. 2011;12:288–301. doi: 10.2174/138945011794815347. [DOI] [PubMed] [Google Scholar]
- 100.Liu Z., Ouyang L., Peng H., Zhang W.Z. Oridonin: Targeting programmed cell death pathways as an anti-tumour agent. Cell Prolif. 2012;45:499–507. doi: 10.1111/j.1365-2184.2012.00849.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Habtemariam S. Natural inhibitors of tumour necrosis factor-alpha production, secretion and function. Planta Med. 2000;66:303–313. doi: 10.1055/s-2000-8660. [DOI] [PubMed] [Google Scholar]
- 102.Piao H.Z., Jin S.A., Chun H.S., Lee J.C., Kim W.K. Neuroprotective effect of wogonin: Potential roles of inflammatory cytokines. Arch. Pharm. Res. 2004;27:930–936. doi: 10.1007/BF02975846. [DOI] [PubMed] [Google Scholar]
- 103.Kim D.S., Park S.S., Nam B.H., Kim I.H., Kim S.Y. Reversal of drug resistance in breast cancer cells by transglutaminase 2 inhibition and nuclear factor-kappaB inactivation. Cancer Res. 2006;66:10936–10943. doi: 10.1158/0008-5472.CAN-06-1521. [DOI] [PubMed] [Google Scholar]
- 104.Jung E.M., Lim J.H., Lee T.J., Park J.W., Choi K.S., Kwon T.K. Curcumin sensitizes tumor necrosis factor-related apoptosis-inducing ligand (TRAIL)-induced apoptosis through reactive oxygen species-mediated upregulation of death receptor 5 (DR5) Carcinogenesis. 2005;26:1905–1913. doi: 10.1093/carcin/bgi167. [DOI] [PubMed] [Google Scholar]
- 105.Fang J., Xia C., Cao Z., Zheng J.Z., Reed E., Jiang B.H. Apigenin inhibits VEGF and HIF-1 expression via PI3K/AKT/p70S6K1 and HDM2/p53 pathways. FASEB J. 2005;19:342–353. doi: 10.1096/fj.04-2175com. [DOI] [PubMed] [Google Scholar]
- 106.Lanas A., Ferrandez A. NSAIDs and the colon. Curr. Opin. Gastroenterol. 2009;25:44–49. doi: 10.1097/MOG.0b013e3283157c4d. [DOI] [PubMed] [Google Scholar]
- 107.Bonovas S., Filioussi K., Sitaras N.M. Do nonsteroidal anti-inflammatory drugs affect the risk of developing ovarian cancer? A meta-analysis. Br. J. Clin. Pharmacol. 2005;60:194–203. doi: 10.1111/j.1365-2125.2005.02386.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Wernli K.J., Newcomb P.A., Hampton J.M., Trentham-Dietz A., Egan K.M. Inverse association of NSAID use and ovarian cancer in relation to oral contraceptive use and parity. Br. J. Cancer. 2008;98:1781–1783. doi: 10.1038/sj.bjc.6604392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sempere L.F., Christensen M., Silahtaroglu A., Bak M., Heath C.V., Schwartz G., Wells W., Kauppinen S., Cole C.N. Altered microRNA expression confined to specific epithelial cell subpopulations in breast cancer. Cancer Res. 2007;67:11612–11620. doi: 10.1158/0008-5472.CAN-07-5019. [DOI] [PubMed] [Google Scholar]
- 110.Yu F., Yao H., Zhu P., Zhang X., Pan Q., Gong C., Huang Y., Hu X., Su F., Lieberman J., et al. Let-7 Regulates self renewal and tumorigenicity of breast cancer cells. Cell. 2007;131:1109–1123. doi: 10.1016/j.cell.2007.10.054. [DOI] [PubMed] [Google Scholar]
- 111.Cho K.R. Ovarian cancer update: Lessons from morphology, molecules, and mice. Arch. Pathol. Lab. Med. 2009;133:1775–1781. doi: 10.5858/133.11.1775. [DOI] [PMC free article] [PubMed] [Google Scholar]