Abstract
Objective
To understand how changes in Medicaid nursing home (NH) reimbursement policy and rates affect a NH’s approach to end-of-life care (ie, its use of hospice).
Methods
This longitudinal study merged US NH decedents’ (1999 to 2004) resident assessment data (MDS) with Part A claims data to determine the proportion of a NH’s decedents using hospice. Freestanding NHs across the 48 contiguous US states were included. A NH-level analytic file was merged with NH survey (ie, OSCAR) and area resource file data, and with annual data on state Medicaid NH rates, case-mix reimbursement policies, and hospice certificate of need (CON). NH fixed-effect (within) regression analysis examined the effect of changing state policies, controlling for differing time trends in CON and case-mix states and for facility-level and county-level attributes. Models were stratified by urban/rural status.
Results
A $10 increase in the Medicaid rate resulted in a 0.41% [95% confidence interval (CI): 0.275, 0.553] increase in hospice use in urban NHs and a 0.37% decrease (95% CI: −0.676, −0.063) in rural NHs not adjacent to urban areas. There was a nonstatistically significant increase in rural NHs adjacent to urban areas. Introduction of case-mix reimbursement resulted in a 2.14% (95% CI: 1.388, 2.896) increase in hospice use in urban NHs, with comparable increases in rural NHs.
Conclusions
This study supports and extends previous research by showing changes in Medicaid NH reimbursement policies affect a NH’s approach to end-of-life care. It also shows how policy changes can have differing effects depending on a NH’s urban/rural status.
Keywords: Medicaid policy, hospice, nursing homes, access to care
Medicaid is an important payer of nursing home (NH) care, with 70% of all US NH days paid for by Medicaid.1 Therefore, it is likely that Medicaid NH reimbursement policies and rates influence NH care and management decisions. In fact, Medicaid reimbursement policy and rates have been found to be associated with NH hospitalizations.2 In addition, longitudinal analyses have found changes in state Medicaid reimbursement policies and rates result in changes in NH resident acuity,3 staffing levels,4 and resident outcomes.5 Whether Medicaid NH reimbursement policies and rates affect the use of Medicare hospice in NHs is unknown. However, given the important role of Medicare hospice in NHs and the variation in its use across states,6 an understanding of whether and how Medicaid reimbursement policies and rates affect hospice use is important.
Only a third of the half million older adults who died in NHs in 2006 received Medicare hospice.6 Yet, the provision of high-quality end-of-life care is a challenge for many NHs, and the experience of dying in NHs for many residents (and their families) is less than optimal.7–14 Dying NH residents who receive hospice compared with those who do not have fewer invasive treatments,15,16 better pain management,17,18 and fewer hospitalizations.19 In addition, families of NH residents who died report higher satisfaction with end-of-life care when residents do versus do not receive hospice care,7–9 and in NHs with a greater intensity of hospice use both hospice and nonhospice residents have higher-quality end-of-life care processes and fewer hospitalizations.20,21
Hospice care is also beneficial to NHs as hospice collaborations offer NHs an opportunity to provide intensive palliative care services to dying residents without acquiring additional palliative care staffing, particularly the staffing needed to provide psychosocial and spiritual support to dying residents and their families. In fact, the overwhelming majority of US NHs contract with hospices to obtain expertise and assistance in caring for NH residents at the end-of-life.22 Nursing homes can offer Medicare hospice care by developing collaborations (including formal contracts) with Medicare certified hospice providers.23 A Medicare beneficiary who resides in a NH is eligible for hospice care if his/her attending physician and the hospice medical director certify in writing that she/he has a prognosis of 6 months or less (if the disease runs its normal course). Use, however, not only varies across states but by numerous other factors.
In NHs, Medicare hospice use has been found to vary by resident characteristics (eg, race, sex, diagnoses, other) and by NH-level (eg, profit and chain status, other) county-level (eg, NH bed occupancy, hospital beds, other) factors.24 Unique to NHs, given the lesser presence of physicians, hospice referral and the timing of referral is greatly influenced by NH staff members’ recognition of terminal decline, their beliefs about hospice, and their initiative in suggesting hospice to residents/families and physicians.25 Furthermore, it is likely that these staff processes and attributes conform to NH administrators’ attitudes and support for hospice, which are known to vary.26
Payer type can also be a major barrier to NH hospice use as terminally ill residents receiving Medicare Part A Skilled Nursing Facility (SNF) care cannot simultaneously access Medicare hospice (if SNF care is related to their terminal condition), but (Medicare eligible) Medicaid or private-pay residents can access hospice. For private-pay residents, residents and families may be hesitant to choose hospice as they would lose the (substantial) Medicare copayment for SNF care. For Medicaid residents, NHs differ in their willingness to suggest hospice for residents receiving Medicare SNF care since with hospice enrollment NH payment converts to the much lower Medicaid per diem versus the higher Medicare per diem. In addition, when dual-eligible residents elect hospice the NH’s Medicaid per diem payment rate is reduced to 95% of the allotted rate and paid directly to the hospice (who then “passes” the payment onto the NH). Therefore, hospice referral means NHs not only receive 5% less of their per diem rates when dual-eligible residents enroll in Medicare hospice, but they may also experience slower “pass-through” payments.
Given the above and the importance of Medicaid as a NH payer,1 it is possible that NHs may modify the magnitude of their hospice use in response to changes in Medicaid NH reimbursement policies and/or rates. Specifically, changes that result in higher NH per diem rates may decrease a NH’s willingness to promote the use of hospice as a 5% reduction applied to a higher base rate will result in greater revenue loss. Therefore, even though there are many benefits hospices bring to NHs (palliative care expertise, additional one-on-one care, payment for medications and durable medical equipment relating to terminal illnesses, other), we hypothesized that policy or rate changes resulting in higher Medicaid payment rates would result in lower rates of NH hospice use.
To examine the above beliefs we focused on 2 changes: a state’s introduction of Medicaid NH case-mix reimbursement and an increase in a state’s Medicaid NH per diem rate. Case-mix reimbursement results in higher payments to NHs when residents have higher acuity. Accordingly, previous research has found a state’s implementation of case-mix reimbursement results in a 2.5% increase in the average acuity of new NH admissions and in a 1.3% to 1.4% increase in average acuity for long-stay residents.3 Of note, although most dying residents do not receive rehabilitation services (which can result in higher payments in states using resource utilization groups for case-mix adjustment), dying residents are considered clinically complex and often require extensive services or special care which places them in higher reimbursement groups than many Medicaid NH residents. Therefore, given this higher acuity, of interest is whether the introduction of case-mix reimbursement results in decreases in NH hospice use (to retain 100% of the higher case-mix revenues) or rather in increases in use (to obtain hospice expertise and assistance in caring for higher acuity residents). Similarly, of interest is whether hospice use decreases when a state’s Medicaid NH per diem rates increase.
This research, by using data from 1999 to 2004 and a difference-in-differences analytic approach, tests the effect of the introduction of Medicaid case-mix policy and of NH rate increases on the use of Medicare hospice care in NHs. If changes in Medicaid reimbursement policies do affect the use of NH hospice then the differing use of hospice across states could be moderated somewhat through policy changes.
METHODS
Data Sources and Population
For years 1999 to 2004 in freestanding NHs in the 48 contiguous US states we used NH resident assessment (MDS) data, Medicare Part A claims data for hospice, hospital, home health, outpatient, and SNF care, and Medicare enrollment data (which includes vital statistics data) linked longitudinally to create a utilization history for all residents. This resident history file was then used to determine where study patients were located and the care they received in the days and weeks before death.27 Before creation of this file, this study was approved by the university’s institutional review board.
Nursing home decedents were defined as Medicare beneficiaries whose deaths occurred within 1 day of an identified NH stay or within 7 days of hospital transfer from a NH (as done in previous research).19 Nursing home hospice use was identified when dates on hospice claims overlapped with dates of NH stays. From these resident-level data, we created a NH-level analytic file which was merged with NH survey (ie, OSCAR) and area resource file (ARF) data, and with longitudinal yearly data on a state’s average Medicaid NH rate, the presence of Medicaid case-mix reimbursement, and the presence of hospice certificate of need (CON). These policy data were collected through a survey of state Medicaid departments, as described elsewhere.28
The final analytic file included NH-level data from freestanding NHs across the 48 contiguous US states with data for at least 3 years, having no >1 year with < 5 resident deaths, and having at least 2 years with >30 but < 500 beds. We excluded NHs with 500 or more beds as these NHs are often associated with states or municipalities and have a very different resident mix. Of note, there were only 1,437 facility year observations (1.85% of total) representing < 5 deaths.
The N for this 6-year panel analysis was 13,111 facilities with 74,090 facility year observations. There were 9,161 facilities in urban counties, 2,464 in rural counties adjacent to urban areas (ie, rural adjacent), and 1,486 in rural counties not adjacent to urban areas (ie, rural nonadjacent).
Outcome Variable
The outcome variable of interest was the proportion of a NH’s decedents who received any NH hospice. For each study year, we determined this proportion by dividing the number of a NH’s decedents who received any NH hospice care by the NH’s total number of decedents.
State Medicaid Reimbursement Policies
We examined 2 state-level time-varying variables. The first was the yearly state-average Medicaid per diem rate, which was inflation adjusted to 2004 dollars (scaled to $10 per unit increments) using the annual Consumer Price Index published by the Bureau of Labor Statistics. The second variable reflected a state’s use of case-mix adjusted Medicaid reimbursement in a given year (yes/no).
Control Variables
We controlled for numerous NH-level attributes that change over time. Nursing home-level variables were drawn from the OSCAR database and from variables aggregated from person-level MDS data. From OSCAR data, we included a NH’s percentage of occupancy, 2 continuous variables reflecting the percentage of a NH’s residents whose payer was Medicaid or Medicare, and we created 3 continuous variables reflecting registered nurse, licensed practical nurse, and nursing assistant hours per patient day. In addition, we controlled for the presence each year of any special care unit and any physician extenders (nurse practitioners or physician assistants) on staff.
Using MDS admission assessment data, we computed and controlled for a NH’s annual admission case-mix severity index.3 As residents newly admitted to a NH are more likely to be Medicare beneficiaries (ie, receiving Medicare Part A SNF care), inclusion of this variable controlled for case-mix increases associated with the admission of these Medicare residents (who cannot simultaneously access hospice). This variable was scaled by its standard deviation (SD) so a unit change represented 1 SD.
As a state’s population density was previously found to be associated with the proportion of a state’s NHs contracting with hospice,29 we controlled for a NH’s urban/rural status. At the county level, we used ARF urban/rural continuum codes for 2003 to identify whether a NH was located in an urban area (ie, codes 1–3 indicating a metropolitan area) or a rural adjacent or nonadjacent area. Using ARF data we also included continuous variables to control for the number of hospital and NH beds available per 100 persons 65+ and physicians per 10,000 persons 65+.
A year variable captured the secular trend, and the yearly number of hospices providing care in a county’s NHs (derived from claims data) captured provider growth (both variables scaled to be 0 in 1999). Last, we allowed for differing secular trends in hospice CON and case-mix states by including 2 additional year indicators interacted with the CON and case-mix indicators (scaled to 0 in 1999). For these variables, states were identified as CON or case-mix states if they had either policy in any of the study years. It was important to control for differing trends in CON states as this policy constrains the market entry of new hospice providers, and thus is associated with lower hospice use.29
Statistical Analyses
Nursing home panel fixed-effect regression analysis (using the within-panel estimator) and V.11 of Stata software30 examined the effect of changing state policies, controlling for differing time trends in CON and case-mix states and for facility-level and county-level attributes. Panel fixed-effect models control for unobserved time-invariant NH characteristics that may influence hospice enrollment in NHs, and allow for a difference-in-difference model causal interpretation of our results. As interactions between a NH’s urban/rural status and numerous variables (including the Medicaid rate outcome) were observed, stratified analyses were conducted. To account for differences in sample size used to calculate our facility level outcome, all regression models used facility weights based on the total number of confirmed annual decedents in each facility.
RESULTS
Twenty-nine states had case-mix adjusted reimbursement in 1999 with the total being 35 in 2004. In the study time period, seven states introduced case-mix payment and 1 discontinued its use. In 1999, the average overall Medicaid rate was $107.80 (SD, 21.6) and in 2004 it was $131.60 (SD, 25.5).
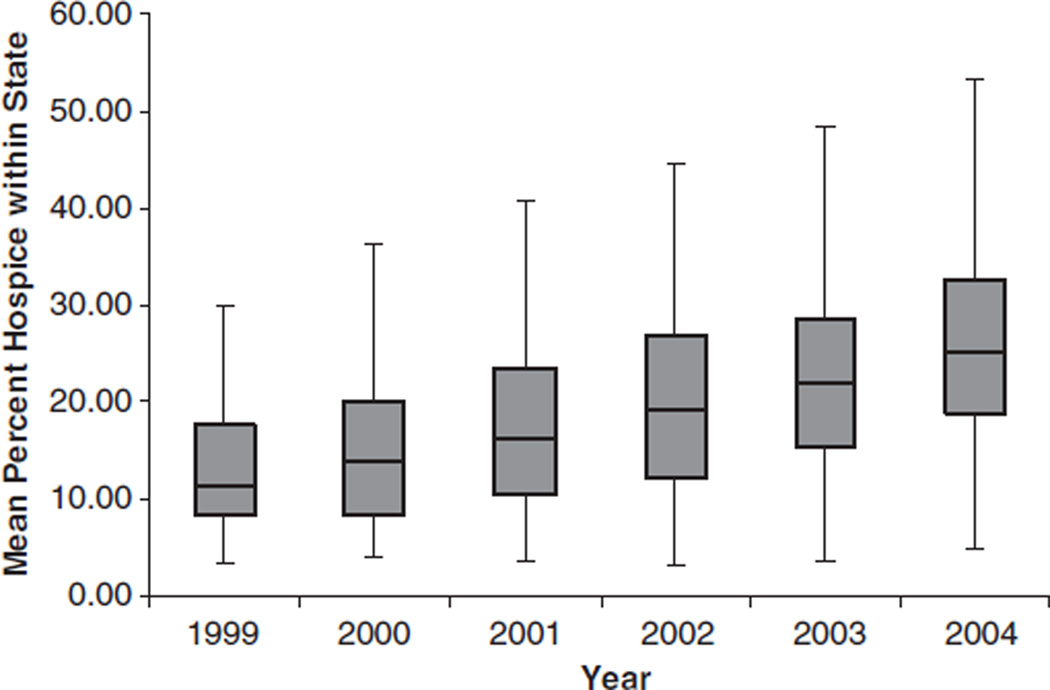
On the basis of state-level aggregates, a median of 10.7% and a mean of 12.4% of NH decedents received NH hospice in 1999; this rose to 25.1% and 25.6% (respectively) by 2004 (Fig. 1). Mean and median rates of hospice use were consistently higher in non-CON states. For example, in 2004, the median was 28.0% and the mean was 27.7% in non-CON states, whereas the median was 20.8% and the mean 20.0% in CON states (data not shown). Rates were also higher in urban versus rural settings. Over the study years, a mean of 21.6% of decedents in urban NHs received hospice; this mean was 15.1% in rural adjacent and 12.6% in rural nonadjacent counties.
FIGURE 1.
Proportion of a state‘s nursing home decedents receiving Medicare hospice in the nursing home.
Controlling for NH-level and county-level factors, secular trends, and for differing secular trends in case-mix or hospice CON states, the fixed-effect regression analyses showed a $10 increase in a state’s Medicaid rate resulted in differing hospice use in urban versus rural NHs (Table 1). In urban NHs, this increase resulted in a 0.41% (95% CI: 0.275, 0.553) increase in hospice use, and would have resulted in an estimated 1753 more decedents receiving hospice each year if all states had a $10 increase in Medicaid rates. In contrast, in rural nonadjacent NHs a $10 increase resulted in a decrease of 0.37% (95% CI: −0.676, −0.063), and would have resulted in an estimated 176 fewer decedents receiving hospice each year if all states had a $10 increase in Medicaid rates.
TABLE 1.
Panel Data Fixed-Effects Regression Analysis—Medicaid Policy and Rates and NH Hospice Usea
| Variables of Interest | Urban (N=42,902) Coef (95% CI) |
Rural Adjacent to Urban (N=11,364) Coef (95% CI) |
Rural Not Adjacent to Urban (N=6,713) Coef (95% CI) |
|---|---|---|---|
| Medicaid rate (a $10 increase) | 0.41 (0.275, 0.553)* | 0.11 (−0.144, 0.368) | −0.37 (−0.676, −0.063)‡ |
| Medicaid case-mix reimbursement (introduction) | 2.14 (1.388, 2.896)* | 2.06 (1.033, 3.095)* | 1.74 (0.350, 3.126)‡ |
| Secular Trends | |||
| Per year | 3.03 (2.864, 3.198)* | 2.75 (2.392, 3.109)* | 2.30 (1.914, 2.689)* |
| Per year in state with any medicaid case-mix | −0.11 (−0.267, 0.050) | −0.04 (−0.370, 0.297) | 0.12 (−0.251, 0.500) |
| Per year in states with any hospice CON | −0.45 (−0.616, −0.291)* | −0.79 (−1.091, −0.488)* | −1.16 (−1.547, −0.776)* |
| Case-mix admission severity† (increase of 1 standard deviation) | −0.58 (−0.820, −0.335)* | −0.43 (−0.799, −0.053)‡ | −0.13 (−0.571, 0.305) |
| Hospice providers in county (increase of 1 provider) | 0.08 (0.024, 0.134)§ | 1.06 (0.890, 1.227)* | 1.82 (1.512, 2.132)* |
Controlling for a nursing home’s occupancy rate; proportion of residents on Medicaid or Medicare, registered nurse, licensed practical nurse, and nursing assistant hours per patient day; presence of any special care unit; and at the county level, hospital and nursing home beds per 100 persons 65+ and physicians per 10,000 persons 65+.
Standardized.
P < 0.001.
P < 0.05.
P < 0.01.
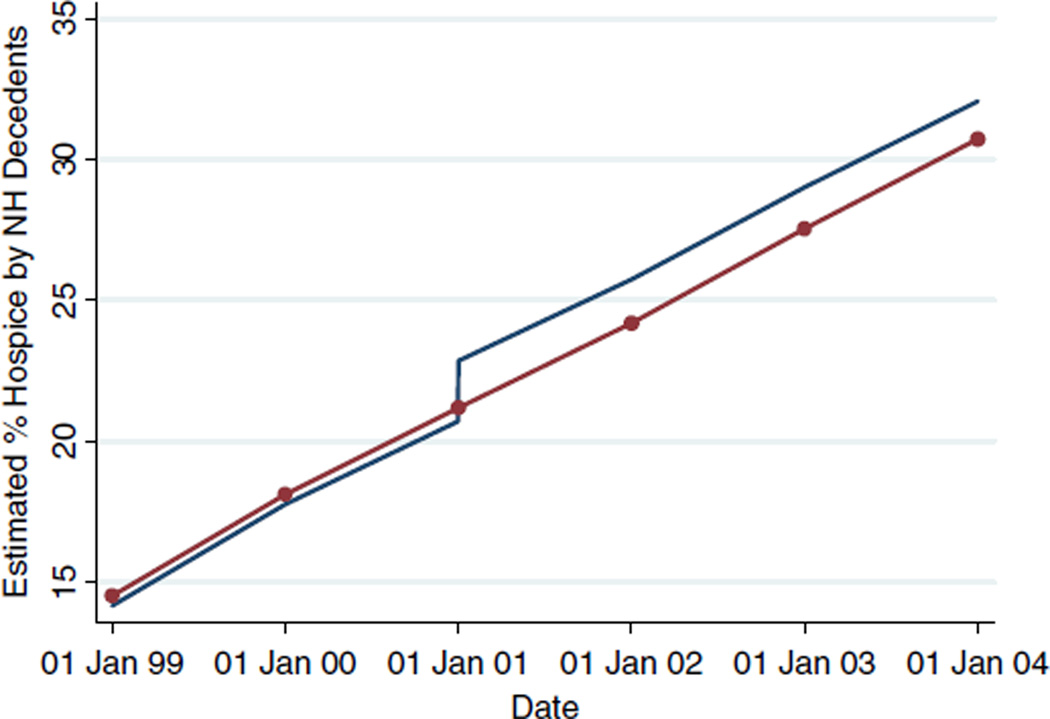
The introduction of Medicaid case-mix reimbursement resulted in a 2.1% increase in hospice use in urban NHs (95% CIs: 1.388, 2.896). Increases were similar but somewhat lower in rural adjacent and nonadjacent counties (Table 1). Controlling for mean values of model variables, Fig. 2 illustrates the increase in NH hospice use in Iowa in 2001, when it introduced Medicaid case-mix reimbursement, and compares this longitudinal use to use in states that did not introduce or have Medicaid case-mix during the study period. As depicted, the 2 percent increase accompanying the introduction of case-mix reimbursement in Iowa is sustained in the years subsequent to the policy change (Fig. 2). Given this, if all states without case-mix reimbursement in 2000 switched to this policy in 2001 an estimated 3925 additional decedents would have received hospice in 2001, and in subsequent years.
FIGURE 2.
The effect of the introduction of Medicaid case-mix reimbursement: Iowa nursing home hospice use (with case-mix introduction in 2001) versus non-Certificate of Need states not introducing case-mix.
Of interest, during our study period there was an approximate 3% annual increase in hospice use in urban NHs, and slightly lower but similar annual increases in rural NHs (Table 1). In addition, in states having any hospice CON annual increases in hospice use were lower (Table 1). Additionally, a 1 SD increase in a NH’s admission case-mix severity score resulted in a decrease in hospice use of 0.58% (95% CI: −0.820, −0.335) in urban NHs and in a decrease of 0.43 (95% CI: −0.799, −0.053) in rural adjacent NHs. Last, the addition of 1 hospice provider (within a county) had a larger effect in rural versus urban NHs, with the largest effect observed in rural NHs not adjacent to urban areas.
CONCLUSIONS
Changes in Medicaid NH reimbursement policy and rates influence a NH’s approach to end-of-life care (ie, its rate of hospice use). Increases in a state’s average NH per diem payment significantly affects NH use of hospice but this effect is in opposing directions in urban versus rural nonadjacent NHs. In urban settings, a $10 increase in a state’s average Medicaid payment in a given year resulted in an approximate half percent increase in NH hospice use. However, in rural nonadjacent areas a $10 increase resulted in an approximate half percent decrease in use. Although the magnitude of these effect sizes is small, the divergent effects observed underscore how the effects of Medicaid payment changes may differ based on a NH’s geographic setting. In contrast, with a state’s introduction of Medicaid case-mix reimbursement there were similar responses in urban and rural NHs; an approximate 2 percent increase in hospice use.
The increase in Medicaid rates (in urban settings) and the introduction of case-mix reimbursement both had a positive effect on hospice use, even when controlling for numerous factors including secular trends and increases in hospice providers. Given changes in the amount and possibly the timing of Medicaid NH per diem payments when dual-eligible residents elect hospice and the importance of Medicaid as a NH payer, we had expected to observe a decline in hospice use with rate increases and with the introduction of case-mix reimbursement. In rural nonadjacent NHs we observed this expected decrease (in relation to rate increases) but this was not the case for urban NHs. Revenue constraints for both NHs and hospices in rural settings most likely combine to explain this markedly different effect.
Hospice use is known to be lower as the rurality of a geographic area increases,31 and proximity to a hospice alone does not account for this lower use.31,32 Rural nonadjacent hospices are smaller than urban hospices, and this small size, together with other factors including longer travel distances and lower Medicare payment rates combine to result in less financial flexibility. Previous research has found that some hospices pay NHs 100% of their Medicaid NH per diems (rather than the 95% they are paid) and may pay NHs prompter than Medicaid (ie, pay NHs before they receive Medicaid payment).33 Hospices with favorable cash flows and greater reserves are more likely to adopt such practices, and rural nonadjacent hospices are the least likely of hospices to have these attributes. In addition, from the NH perspective, lower access to higher paying Medicare Part A SNF residents in rural areas means that the potential 5% loss in Medicaid revenues when a resident enrolls in hospice has a likely larger impact on a rural NH’s revenue stream.
Both urban and rural NHs increased hospice use in response to the introduction of Medicaid case-mix payment. This increase (rather than the expected decrease) may result in part from the higher resident acuity known to accompany the introduction of Medicaid case-mix reimbursement3 and the higher acuity associated with residents nearing their end-of-life. With case-mix introduction, therefore, it appears the advantages of having hospice expertise and assistance to care for higher acuity residents outweighs any revenue losses.
Some limitations of our study data should be noted. First, we categorized the presence of a Medicaid case-mix system as yes/no, but there are many nuances of case-mix reimbursement systems that may result in differing effects. For example, states use differing methods to determine case-mix severity (resource utilization groups, other) and they update case-mix payment rates at differing time intervals.3 In addition, there are some states that do not follow the federal guidance regarding pass-through (to hospices) of NH Medicaid payments, and we did not additionally control for this as these practices and their timing (start and stop dates) are not entirely clear. Future research should focus on the details of state case-mix reimbursement systems and direct and pass-through payments, possibly through a series of detailed case studies,34 to understand how various features may differentially affect NH hospice use. These or other studies could also be designed to gain an understanding of the extent to which other nonfinancial factors (ie, the quality and volume of hospice services and the quality of the NH hospice collaboration) influence a NH’s intensity of hospice use.33
In addition to the above, we may have under controlled for unobserved NH time-varying covariates. However, the fixed-effects model used and its autoregressive error term, while not solving entirely the problem, reduces substantially any bias that may result from such an exclusion. Last, our model includes NH residents in a given year based on their year of death rather than on their year of hospice enrollment, which introduces some measurement error if hospice admission occurred in a year before the year of death. However, only 16% of all decedents were admitted to hospice in a year before death; therefore, given that the vast majority of residents died in the same year as that of their hospice admission, any bias introduced should be minimal.
This study provides important insight into how changes in Medicaid NH reimbursement policies affect hospice use in NHs. It also underscores and provides a concrete example of how changes in Medicaid NH reimbursement policy can differentially affect urban and rural adjacent and nonadjacent NHs. Decisions regarding NH hospice enrollment are complex and involve residents/families, NHs, and physicians. This study demonstrates that state policies impact the NH’s approach to providing end-of-life care to its residents.
Acknowledgments
This study was funded by the Shaping Long Term Care in America Project funded by the National Institute on Aging (P01AG027296) and by the Agency for Health Care Research and Quality (R03HS016918).
Footnotes
Conflict of Interest: None.
REFERENCES
- 1.Rhoades J, Sommers J, editors. Expenses and Sources of Payment for Nursing Home Residents. Rockville, MD: Agency for Healthcare Research and Quality 2000; 1996. MEPS Research Findings No 13. AHRQ Pub No. 01-0010; [Google Scholar]
- 2.Intrator O, Grabowski DC, Zinn J, et al. Hospitalization of nursing home residents: the effects of states’ Medicaid payment and bed-hold policies. Health Serv Res. 2007;42:1651–1671. doi: 10.1111/j.1475-6773.2006.00670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Feng Z, Grabowski DC, Intrator O, et al. The effect of state Medicaid case-mix payment on nursing home resident acuity. Health Serv Res. 2006;41(4 Pt 1):1317–1336. doi: 10.1111/j.1475-6773.2006.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Feng Z, Grabowski D, Intrator O, et al. Medicaid payment rates, case-mix reimbursement, and nursing home staffing—1996–2004. Med Care. 2008;46:33–40. doi: 10.1097/MLR.0b013e3181484197. [DOI] [PubMed] [Google Scholar]
- 5.Mor V, Gruneir A, Feng Z, et al. The effect of state policies on nursing home resident outcomes. J Am Geriatr Soc. 2011;59:3–9. doi: 10.1111/j.1532-5415.2010.03230.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller SC, Lima J, Gozalo P, et al. The growth of hospice care in U.S. nursing homes. J Am Geriatr Soc. 2010;58:1481–1488. doi: 10.1111/j.1532-5415.2010.02968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wetle T, Teno J, Shield R, et al., editors. End of Life in Nursing Homes: Experiences and Policy Recommendations. Washington, D.C.: AARP Public Policy Institute; 2004. [Google Scholar]
- 8.Hanson LC, Henderson M, Menon M. As individual as death itself: a focus group study of terminal care in nursing homes. J Palliat Med. 2002;5:117–125. doi: 10.1089/10966210252785088. [DOI] [PubMed] [Google Scholar]
- 9.Baer WM, Hanson LC. Families’ perception of the added value of hospice in the nursing home. J Am Geriatr Soc. 2000;48:879–882. doi: 10.1111/j.1532-5415.2000.tb06883.x. [DOI] [PubMed] [Google Scholar]
- 10.Bernabei R, Gambassi G, Lapane K, et al. Management of pain in elderly patients with cancer. SAGE Study Group: Systematic Assessment of Geriatric Drug Use via Epidemiology. JAMA. 1998;279:1877–1882. doi: 10.1001/jama.279.23.1877. [DOI] [PubMed] [Google Scholar]
- 11.Ferrell BR, Dean GE, Grant M, et al. An institutional commitment to pain management. J Clin Oncol. 1995;13:2158–2165. doi: 10.1200/JCO.1995.13.9.2158. [DOI] [PubMed] [Google Scholar]
- 12.Parmelee PA, Smith B, Katz IR. Pain complaints and cognitive status among elderly institution residents. J Am Geriatr Soc. 1993;41:517–522. doi: 10.1111/j.1532-5415.1993.tb01888.x. [DOI] [PubMed] [Google Scholar]
- 13.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 14.Zerzan J, Stearns S, Hanson L. Access to palliative care and hospice in nursing homes. JAMA. 2000;284:2489–2494. doi: 10.1001/jama.284.19.2489. [DOI] [PubMed] [Google Scholar]
- 15.Miller SC, Gozalo P, Mor V, editors. Outcomes and Utilization for Hospice and Non-hospice Nursing Facility Decedents Synthesis and Analysis of Medicare’s Hospice Benefit. Washington, D.C.: Office of Disability, Aging, and Long Term Care Policy in the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 16.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529–1538. doi: 10.1056/NEJMoa0902234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller SC, Mor V, Teno J. Hospice enrollment and pain assessment and management in nursing homes. J Pain Symptom Manage. 2003;26:791–799. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 18.Miller SC, Mor V, Wu N, et al. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? J Am Geriatr Soc. 2002;50:507–515. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- 19.Gozalo P, Miller SC. Hospice enrollment and evaluation of its causal effect on hospitalization of dying nursing home patients. Health Serv Res. 2007;42:587–610. doi: 10.1111/j.1475-6773.2006.00623.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller SC, Gozalo P, Mor V. Hospice enrollment and hospitalization of dying nursing home patients. Am J Med. 2001;111:38–44. doi: 10.1016/s0002-9343(01)00747-1. [DOI] [PubMed] [Google Scholar]
- 21.Zheng NT, Temkin-Greener H. End-of-life care in nursing homes: the importance of CNA staff communication. J Am Med Dir Assoc. 2010;11:494–499. doi: 10.1016/j.jamda.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miller SC, Han B. End-of-life care in U.S. nursing homes: nursing homes with special programs and trained staff for hospice or palliative/end-of-life care. J Palliat Med. 2008;11:866–877. doi: 10.1089/jpm.2007.0278. [DOI] [PubMed] [Google Scholar]
- 23.Gage B, Miller SC, Coppola K, et al., editors. Important Questions for Hospice in the Next Century Synthesis and Analysis of Medicare’s Hospice Benefit. Washington, D.C.: Office of Disability, Aging, and Long Term Care Policy in the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2000. [Google Scholar]
- 24.Lepore MJ, Miller SC, Gozalo P. Hospice use among urban black and white U.S. nursing home decedents in 2006. Gerontologist. 2011;51:251–260. doi: 10.1093/geront/gnq093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Welch LC, Miller SC, Martin EW, et al. Referral and timing of referral to hospice care in nursing homes: the significant role of staff members. Gerontologist. 2008;48:477–484. doi: 10.1093/geront/48.4.477. [DOI] [PubMed] [Google Scholar]
- 26.Dobbs DJ, Hanson L, Zimmerman S, et al. Hospice attitudes among assisted living and nursing home administrators, and the long-term care hospice attitudes scale. J Palliat Med. 2006;9:1388–1400. doi: 10.1089/jpm.2006.9.1388. [DOI] [PubMed] [Google Scholar]
- 27.Intrator O, Hiris J, Berg K, et al. The Residential History File: studying nursing home residents’ long-term care histories. Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Grabowski DC, Feng Z, Intrator O, et al. Recent trends in state nursing home payment policies. Health Aff(Millwood) 2004:W4–W73. doi: 10.1377/hlthaff.w4.363. Suppl ****Web Exclusives. [DOI] [PubMed] [Google Scholar]
- 29.Miller SC, Mor V. The opportunity for collaborative care provision: the presence of nursing home/hospice collaborations in the U.S. states. J Pain Symptom Manage. 2004;28:537–547. doi: 10.1016/j.jpainsymman.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 30.StataCorp. Stata Statistical Sofware: Release 11. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 31.Virnig BA, Moscovice IS, Durham SB, et al. Do rural elders have limited access to Medicare hospice services? J Am Geriatr Soc. 2004;52:731–735. doi: 10.1111/j.1532-5415.2004.52213.x. [DOI] [PubMed] [Google Scholar]
- 32.Carlson MD, Bradley EH, Du Q, et al. Geographic access to hospice in the United States. J Palliat Med. 2010;13:1331–1338. doi: 10.1089/jpm.2010.0209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller SC. A model for successful nursing home-hospice partnerships. J Palliat Med. 2010;13:525–533. doi: 10.1089/jpm.2009.0296. [DOI] [PubMed] [Google Scholar]
- 34.Miller EA, Mor V, Grabowski DC, et al. The devil’s in the details: trading policy goals for complexity in Medicaid nursing home reimbursement. J Health Polit Policy Law. 2009;34:93–135. doi: 10.1215/03616878-2008-993. [DOI] [PubMed] [Google Scholar]