Abstract
Objective
To examine HIV-related knowledge, attitudes, and behaviors in at-risk college men who have sex with men (MSM), focusing on knowledge about acute HIV infection (AHI).
Participants and Methods
A one-time anonymous survey was administered to college students attending a lesbian, gay, bisexual, transgender, and queer (LGBTQ) conference in February 2012. This paper reports on a study sub-sample of MSM.
Results
A total of 100 MSM completed the survey. Participants had an average age of 20.4 years. Sixty-six percent reported condom use the last time they had sex. Only 46% had ever heard of symptoms related to AHI. Forty-two percent would likely seek medical care when showing acute symptoms in a setting consistent with AHI.
Conclusion
Despite having multiple risk factors for HIV infection, many MSM college students are unaware of AHI. HIV prevention programs should target this population and include information about signs, symptoms, and diagnosis of AHI.
Keywords: clinical medicine, community health, health education
Acute HIV infection (AHI) is the period of weeks to months following initial infection with HIV during which time more than half of all patients experience a brief, flu-like illness.1,2 Common presenting symptoms include fever, rash, fatigue, and sore throat.2 Although early symptoms of HIV are relatively common, these symptoms often go undetected by both infected individuals and healthcare providers. One important challenge in diagnosing AHI is that standard tests are often negative during the HIV antibody testing ‘window period’ and special tests such as an HIV RNA PCR (viral load) may be required.2 There is indication that AHI is a growing concern for college-age individuals, especially young men who have sex with men (MSM).3
For primary care providers, failure to diagnose AHI represents an important missed opportunity. AHI plays a significant role in forward transmission of HIV secondary to the high levels of virus found in the blood and other bodily fluids.4 As many as 50% of new HIV infections may result from acutely or recently infected individuals.5 Expanded efforts to identify and diagnose individuals with AHI may result in behavior changes that could substantially reduce HIV transmission. Furthermore, early diagnosis and treatment of HIV has been shown to improve long-term health outcomes of people living with HIV.6
There have been very few studies assessing knowledge and awareness of AHI by populations at-risk for HIV infection. Qualitative investigations evaluating recently diagnosed individuals found that most participants reported not knowing about AHI at the time of diagnosis, but those who did possess knowledge about AHI and experienced symptoms refrained from sexual risk behavior even before they received a clinical diagnosis of HIV infection.7 Other reports of high-risk, HIV-negative MSM found that 64% of participants could name at least one symptom of AHI but that only 39% of those who knew about AHI would seek care for flu-like symptoms.8
Subgroups of college students, in particular college-age MSM, may be at much higher risk for HIV infection than previously suspected.9,10 In 2009, 27% of all new HIV infections in the US were in MSM between the ages of 13 and 29.10 A fairly rigorous body of research looking at HIV-related knowledge among college students suggests that American college students are generally knowledgeable about HIV, but still engage in significant HIV risk behaviors.11 Although general knowledge about HIV among college students is well documented, there have been no prior studies that specifically assessed what college students know about AHI. In 2010, several college-aged MSM presented to student health centers in New England with suspected AHI3 which prompted concerns for an epidemic of acute infection among students. This study sought to examine levels of HIV-related knowledge, attitudes, and behaviors in at-risk MSM college students with a focus on knowledge about AHI.
Methods
Sampling
We administered a one-time survey in February 2012 to college and graduate students attending a conference on Lesbian, Bisexual, Transgender, Gay, and Queer (LGBTQ) issues. The conference was hosted at an Ivy League university and included students from all eight Ivy League schools. All conference attendees (420 in total), including both males and females, were invited to participate. To be included in the study, participants had to be: i) 18 years of age or older and ii) currently enrolled in college or graduate school. No one was excluded from participation on the basis of sexual behavior or identity. The survey was anonymous and did not ask for any personally identifiable information. Because young MSM are at significantly elevated risk for HIV infection, this paper reports on data from a study sub-sample of males who reported sex with another male in the past year (behavioral MSM, N=100). Most MSM in the study sub-sample (92%) were undergraduate college students. Sample characteristics, including participant demographics, are described in the Results section. Measures used to classify individuals as MSM for the purposes of constructing the analytic sample are described below under Measures.
Procedures
Conference attendees were offered the opportunity to complete the one-time, self-administered survey at the time of conference registration. Interested individuals who were deemed eligible provided verbal informed consent. After survey completion, participants had the opportunity to attend an informational presentation about HIV by an infectious diseases specialist. Respondents were provided a $5 gift card as compensation for their time and participation in the study. Following the conference, all attendees received an informational email with basic facts about acute HIV symptoms and HIV testing. The survey instrument and research protocol were approved by the university Institutional Review Board.
Measures
The survey included questions about demographics, sexual behaviors, HIV testing behaviors, general knowledge about HIV, and AHI knowledge.
Demographics: Demographic items were adapted from the 2011 CDC Behavioral Risk Factor Surveillance System Survey (BRFSS).12
Sexual Behavior: Sexual behavior items were drawn from previously validated CDC surveillance studies.13 Key measures of sexual behavior included recent sexual activity (“During the past 12 months, have you had sex?” and “During the past 12 months, with how many people have you had sex?”), gender of recent sexual partners (“During the past 12 months, have you had sex with only males, only females, or with both males and females?”), and recent condom use (“Now, thinking about the last time you had sex, did you or your partner use a condom?”). Sexual orientation was assessed separately from sexual behavior using a one-item measure that has been previously validated for use in national health surveys: “Do you consider yourself to be one or more of the following (check all that apply): Straight, Gay or lesbian, Bisexual, Transgender.”14
HIV Testing Behavior: HIV testing behavior items were also adapted from CDC surveillance studies.15 HIV testing history was assessed through the following measure: “Have you ever been tested for HIV? Do not count tests you may have had as part of a blood donation. Include testing fluid from your mouth.”
General Knowledge about HIV: General HIV knowledge questions were based on previously validated, true/false questions assessing basic knowledge of HIV/AIDS (sample items included: “Coughing and sneezing DO NOT spread HIV” and “Using Vaseline or baby oil with condoms lowers the chance of getting HIV”).16 This measure, the Brief HIV Knowledge Questionnaire (HIV-KQ-18) has been psychometrically validated and used in a number of prior prevention programs and research studies. The HIV-KQ-18 was found to have strong internal consistency across several samples (alphas = .75-.89) and strong associations with longer validated HIV knowledge measures (r=.93-.97).16 The full scale is presented in Table 4.
- AHI Knowledge: There is no previously validated set of questions measuring knowledge about AHI. The study authors developed a 16-item AHI Knowledge Scale based on an extensive literature review and expert opinion of HIV/AIDS specialists, following procedures described in Carey et al.17 Items for this scale were generated to assess one of three sub-components of AHI knowledge:
- Signs and symptoms (sample item = “Flu-like symptoms can be a sign of recent HIV infection”). The AHI Signs and Symptoms subscale had an internal reliability of 0.61.
- Diagnosis (sample item = “An infected person can have an HIV test that is negative”). The AHI Diagnosis subscale had an internal reliability of 0.68.
- Transmissibility (sample item = “During the first few weeks after acquiring HIV, the virus is dormant or inactive and the risk of transmitting HIV is low”). The AHI Transmissibility subscale had an internal reliability of 0.57.
Table 4.
General Knowledge about HIV
| General HIV Knowledge | |
|---|---|
| Item |
Behavioral MSM
N=100 (% responding correctly) |
| A natural skin condom works better against HIV than does a latex condom. (False) |
59 (59%) |
| All pregnant women infected with HIV will have babies born with AIDS. (False) |
75 (75%) |
| There is a female condom that can help decrease a woman’s chance of getting HIV. (True) |
77 (77%) |
| Using Vaseline or baby oil with condoms lowers the chance of getting HIV. (False) |
81 (81%) |
| A person can get HIV from oral sex. (True) |
81 (81%) |
| Taking a test for HIV one week after having sex will tell a person if she or he has HIV. (False) |
83 (83%) |
| People are likely to get HIV by deep kissing, putting their tongue in their partner’s mouth, if their partner has HIV. (False) |
87 (87%) |
| A woman cannot get HIV if she has sex during her period. (False) |
87 (87%) |
| There is a vaccine that can stop adults from getting HIV. (False) |
89 (89%) |
| A person can get HIV by sitting in a hot tub or a swimming pool with a person who has HIV. (False) |
89 (89%) |
| A person can get HIV by sharing a glass of water with someone who has HIV. (False) |
89 (89%) |
| A person will NOT get HIV if she or he is taking antibiotics. (False) |
91 (91%) |
| Having sex with more than one partner can increase a person’s chance of being infected with HIV. (True) |
93 (93%) |
| Coughing and sneezing DO NOT spread HIV. (True) |
93 (93%) |
| A woman can get HIV if she has anal sex with a man. (True) |
93 (93%) |
| Pulling out the penis before a man climaxes/cums keeps a woman from getting HIV during sex. (False) |
94 (94%) |
| Showering, or washing one’s genitals/private parts, after sex keeps a person from getting HIV. (False) |
94 (94%) |
| People who have been infected with HIV quickly show serious signs of being infected. (False) |
95 (95%) |
Note. MSM=men who have sex with men
Table 3.
Acute HIV Infection (AHI) Knowledge
| AHI Signs and Symptoms | |
|---|---|
| Item |
Behavioral MSM
N=100 (% responding correctly) |
| Over 90% of people with HIV experience no symptoms in the first few weeks to months after becoming infected. (False) |
6 (6%) |
| A rash can be a sign of recent HIV infection. (True) |
44 (44%) |
| The symptoms of recent HIV infection can look a lot like those of mononucleosis (‘mono’ or ‘kissing disease’). (True) |
46 (46%) |
| The symptoms of recent HIV infection are very different from the symptoms of the common cold or flu. (False) |
64 (64%) |
| Flu-like symptoms can be a sign of recent HIV infection. (True) |
68 (68%) |
| Someone recently infected with HIV may have no symptoms. (True) |
94 (94%) |
| AHI Diagnosis | |
| The best way to detect acute or early HIV infection is a Western Blot test. (False) |
19 (19%) |
| Acute or early HIV infection is best identified by checking a plasma RNA or viral load. (True) |
24 (24%) |
| A positive HIV antibody test, but indeterminate Western Blot test may suggest acute HIV infection. (True) |
25 (25%) |
| The most common HIV test (the HIV ELISA test) measures levels of HIV virus in the blood. (False) |
33 (33%) |
| The most common HIV test (the HIV ELISA test) may not detect very early HIV infection. (True) |
77 (77%) |
| An infected person can have an HIV test that is negative. (True) |
78 (78%) |
| The most common HIV test (the HIV ELISA test) is positive in most HIV+ people by six months after they become infected. (True) |
80 (80%) |
| If you test negative for HIV one month after sex with an HIV+ person, this means you do not have HIV. (False) |
83 (83%) |
| AHI Transmissibility | |
| The risk of transmitting HIV immediately after becoming infected is high. (True) |
45 (45%) |
| During the first few weeks after acquiring HIV, the virus is dormant or inactive and the risk of transmitting HIV is low. (False) |
56 (56%) |
Note. MSM=men who have sex with men
Analysis
Descriptive statistics were used to characterize the socio-demographics and sexual health behaviors of the study sample of behavioral MSM. We characterized HIV knowledge based on the percent responding correctly to each item in the AHI Knowledge Scale, along with the general HIV knowledge items. Following the procedures described in Carey et al,17 the AHI knowledge and general HIV knowledge scales were scored by adding up the number of correct responses to the true/false items. For both scales, “don’t know” responses were coded as incorrect. Reliability coefficients for sub-scales were examined and intercorrelations between subscales and general HIV knowledge were conducted, guided by procedures described by Ping.18 Finally, we described participants’ self-reported responses to suspected AHI.
Results
Description of study sample
Table 1 highlights the socio-demographic characteristics of the study sample. Out of 233 male and female respondents who agreed to participate and who initiated the survey, 113 were males who reported sex with another male in the past year. One hundred of those MSM respondents provided complete data and were included in the final analytic sample. Respondents were 53% white, and 14% Hispanic. All respondents self-identified as LGBTQ (gay = 87%, bisexual = 9%, transgender = 0%, queer or other = 4%). Most (92%) of the respondents were undergraduates, with relatively equal representation of freshmen, sophomores, juniors and seniors. The mean age of survey respondents was 20.4 years (range 18-25).
Table 1.
Socio-demographic characteristics of survey respondents
| Characteristics |
Behavioral MSM
N=100, (%) |
|---|---|
| Gender | |
| Male | 100 (100%) |
| Female | |
| Other | |
| Race | |
| White | 53 (53%) |
| Black | 13 (13%) |
| Asian-American | 19 (19%) |
| American Indian/Alaska Native |
1 (1%) |
| Other or Multiple | 12 (12%) |
| No response selected | 1 (1%) |
| Ethnicity | |
| Hispanic | 14 (14%) |
| Non-Hispanic | 86 (86%) |
| Orientation | |
| Gay | 87 (87%) |
| Bisexual | 9 (9%) |
| Other or Multiple | 4 (4%) |
| Year in college | |
| 1st year | 21 (21%) |
| 2nd year | 20 (20%) |
| 3rd year | 25 (25%) |
| 4th year | 24 (24%) |
| 5th year | 2 (2%) |
| Graduate Student | 8 (8%) |
| Age | |
| Mean age (range) | 20.4 (18-25) |
Note. MSM = men who have sex with men
Sexual Health Behaviors
Self-reported HIV risk and HIV testing behaviors are shown in Table 2. All respondents in the analytic sample (N=100) reported being sexually active in the last 12 months. Sixty-six percent (N=66) reported using a condom at the time of their last sexual encounter. The majority of respondents (77%) reported sex with multiple partners in the past year. The mean number of partners reported in the last six months was 4.9 (range 1-20). Overall, 15% (N=15) of respondents had ever been treated for a sexually transmitted infection (STI), 1% (N=1) had used intravenous (IV) drugs, and 3% (N=3) reported having given or received money in exchange for drugs or sex in the last year.
Table 2.
Sexual Behaviors and HIV Testing History
| Behaviors |
Behavioral MSM
N=100, (%) |
|---|---|
| Had sex in last 12 months | 100 (100%) |
| Used condom with last sexual encounter |
66 (66%) |
| Mean number of sex partners in last 6 months (SD) |
4.9 (4.0) |
| Ever used IV drugs | 1 (1%) |
| Ever been treated for a sexually transmitted infection |
15 (15%) |
| Given or received money in exchange for drugs or sex in the last year |
3 (3%) |
| Had more than one sex partner in the last year |
77 (77%) |
| Have tested positive for HIV |
1 (1%) |
| Ever tested for HIV | 77 (77%) |
| Personally know anyone with HIV |
40 (40%) |
Note. MSM = men who have sex with men
Seventy-seven percent (N=77) had previously been tested for HIV. Only one respondent (1%) reported having tested positive for HIV.
General Awareness about Acute HIV Infection
Overall awareness of AHI was assessed through a single-item measure: “Before taking this survey, had you ever heard that there can be symptoms of recent HIV infection? Some people call this ‘acute HIV’ or ‘primary HIV’ infection.” Only 46% (N=46) of respondents stated that they had heard of AHI.
Knowledge about Acute HIV Infection
Table 3 demonstrates participant knowledge about AHI transmission, diagnosis, and symptoms, as measured by the 16-item AHI Knowledge Scale. Respondents were allowed to respond “true,” “false,” or “don’t know” to each item; they were instructed to choose “don’t know” for items they were unsure about.
Subscale 1 - AHI Signs and Symptoms
The survey assessed participant knowledge about signs and symptoms of AHI using six items. Two items were focused on knowledge about existence of signs and symptoms. Ninety-four percent (N=94) incorrectly believed that “over 90% of people with HIV experience no symptoms in the first few weeks to months after becoming infected.” Ninety-four percent (N=94) were aware that “someone recently infected with HIV may have no symptoms.” The other four items focused on knowledge about the characteristics of common AHI symptoms. Forty-four percent (N=44) of respondents correctly identified rash as a sign of recent HIV infection, while 68% (N=68) knew that flu-like symptoms could be a sign.
Subscale 2 - AHI Diagnosis
The next set of items measured participant knowledge about AHI diagnosis. The first four items asked about advanced diagnostic tools to detect HIV during the “window period” when HIV antibody tests may be falsely negative. Student knowledge about these diagnostic tools was low; only 24% (N=24) knew that “acute or early HIV infection is best identified by checking a plasma RNA or viral load.” The next four items measured participant knowledge about the existence of an HIV testing window period. A majority of participants (77%, N=77) were aware that “the most common HIV test (the HIV ELISA test) may not detect very early HIV infection,” and 78% knew that “an infected person can have an HIV test that is negative” (N=78).
Subscale 3 - AHI Transmissibility
The last domain examined what students knew about the high transmissibility of AHI. Fifty-six percent (N=56) of students correctly identified the following item as false: “During the first few weeks after acquiring HIV, the virus is dormant or inactive and the risk of transmitting HIV is low.” Forty-five percent (N=45) correctly identified a similar item as true: “The risk of transmitting HIV immediately after becoming infected is high.”
General Knowledge about HIV
General knowledge about HIV in the study population was assessed to provide context and comparison with AHI knowledge. We administered an 18-item measure of general HIV knowledge, the Brief HIV Knowledge Questionnaire (HIV-KQ-18).16 Using the same true/false question format as the AHI Knowledge Scale, this measure assesses basic knowledge about modes of HIV transmission, prevention, and symptoms, but does not specifically ask about AHI. Overall, general HIV knowledge was high. As shown in Table 4, all items except one had >70% correct response rates. Ninety-three percent of respondents (N=93) knew that “coughing and sneezing do not spread HIV,” and 93% (N=93) knew that “having sex with more than one partner can increase a person’s chance of being infected with HIV.” One item assessed student knowledge about the ‘window period’ for HIV testing. Seventeen percent of respondents (N=17) incorrectly believed that “taking a test for HIV one week after having sex will tell a person if she or he has HIV.” Overall internal reliability of the general HIV knowledge items was 0.72.
Table 5 shows the correlation between each of the AHI knowledge subscales and General HIV knowledge in the full study sample. All measures were correlated at the p < .05 level. The correlation between the overall AHI Knowledge measure and the General HIV Knowledge measure was 0.25, indicating less than 10% shared variance across these measures. Each of the AHI Knowledge sub-scales had a correlation of less than 0.30 with the General HIV Knowledge measure.
Table 5.
Correlations between AHI Knowledge (overall measure and sub-scales) and General HIV Knowledge
| General HIV Knowledge |
AHI Transmission sub-scale |
AHI Symptoms sub- scale |
AHI Diagnosis sub- scale |
|
|---|---|---|---|---|
| AHI Knowledge (overall scale) |
0.25* | -- | -- | -- |
| AHI Transmission sub-scale |
0.08 | -- | -- | -- |
| AHI Symptoms sub- scale |
0.25* | 0.21* | -- | -- |
| AHI Diagnosis sub-scale |
0.19 | 0.08 | 0.42*** | -- |
Note. AHI = Acute HIV Infection
indicates p-value <.05
indicates p-value <.01
indicates p-value <.001
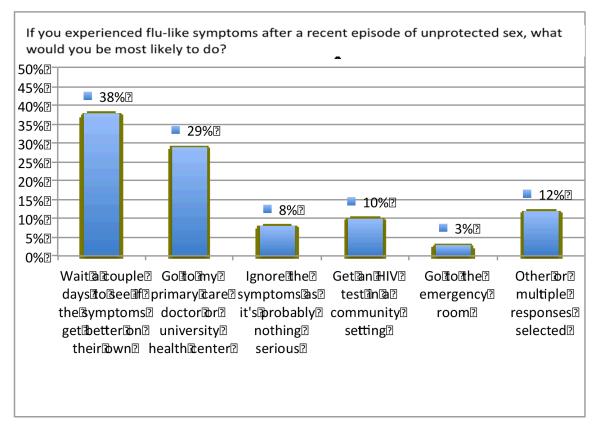
Intention to seek care in response to AHI symptoms
As shown in Figure 1, participants were presented with a hypothetical scenario in which AHI might be suspected and asked how they would react: “If you experienced flu-like symptoms after a recent episode of unprotected sex, what would you be most likely to do?” Overall, 42% (N=42) reported they would seek some sort of medical attention by going to a primary care physician, the emergency room, or an HIV testing center. The most frequently selected response, chosen by 38% (N=38) of respondents, was “wait a couple of days to see if the symptoms get better on their own before seeking any advice.” Another 8% (N=8) responded that they would “ignore the symptoms as it’s probably nothing serious.”
Figure 1.
Intention to seek medical care following AHI symptoms (N=100). Note. AHI = acute HIV infection
Comment
Despite having multiple risk factors for HIV infection, including sex with multiple partners and recent unprotected sex, many MSM college students are unaware of AHI. Overall, fewer than half of respondents had ever heard of AHI before taking the survey.
Respondents demonstrated important knowledge gaps in all three domains of AHI knowledge. The majority of respondents incorrectly believed that “over 90% of people with HIV experience no symptoms in the first few weeks to months after becoming infected.” According to clinical studies, up to 90% of people actually do experience symptoms.2 It is important for at-risk MSM students to be aware that there are signs and symptoms of AHI and to know what they may be so that they can seek appropriate medical attention if they experience symptoms that could be due to AHI. The survey also assessed participant knowledge about specific signs and symptoms that may be indicative of AHI. It is encouraging that most participants (68%) correctly identified flu-like symptoms as a possible sign of AHI. Nevertheless, we hypothesize that some correct responses to this item may reflect inconsistent knowledge or guessing, given that only 46% of participants stated they had ever heard about early HIV symptoms prior to taking the survey.
Most participants were aware that commonly performed HIV antibody tests like the HIV ELISA test may be unable to detect AHI. However, it is concerning that 22% did not know that “an infected person can have an HIV test that is negative.” Respondents also demonstrated inconsistent knowledge about the high transmissibility of AHI, with significant variation in the percent of students responding correctly to two similar items. Knowledge about the ‘window period’ for HIV antibody testing and about the transmissibility of AHI is essential given that HIV is easily transmitted during the early period of HIV infection – a time when many newly infected individuals may be unaware of their HIV status. Given the highly infectious nature of AHI, false belief that a negative HIV test is definitive evidence of one’s HIV status could have significant ramifications.
The recent approval of the OraQuick At-Home HIV test by the US Food and Drug Administration19 amplifies these concerns. It has been suggested that individuals testing at home without receiving post-test counseling and education could overlook the HIV antibody test ‘window period’ and make decisions around having unprotected sex on the basis of negative test results.20 As the at-home HIV test enters the market, raising awareness about AHI and the HIV testing ‘window period’ in communities at risk for HIV will become increasingly important.
When we asked how students might respond to a situation where AHI could be suspected, only 42% reported they would be likely to seek some sort of medical attention. AHI symptoms may be relatively short-lived, meaning that individuals who “wait and see” if their symptoms subside could easily allow a recent infection to go undiagnosed. After the acute period, HIV infection can be asymptomatic for years, during which time an infected individual may unknowingly transmit the virus to others until ultimately presenting late in the course of disease (i.e. AIDS). Failure to diagnose HIV during this early symptomatic period may be a missed opportunity with important public health implications.
These findings indicate that scientific insights about AHI accumulated during the past decade have not reached at-risk MSM college students, representing a critical lag in information dissemination. The high levels of general HIV knowledge suggest that basic information about HIV is reaching this population, but that MSM college students have specific deficits in knowledge about AHI. This deficit may extend to other high-risk populations, including other MSM. Prior published reports of AHI knowledge in at-risk MSM found that many MSM lacked knowledge about important aspects of AHI.7,8
HIV prevention programs targeted at MSM college students should include education and counseling about early symptoms of HIV, as well as how to diagnose and manage AHI. Educational materials should include information about the HIV testing ‘window period’ and the high infectiousness of AHI. By learning that HIV is easily transmitted during AHI (when common HIV tests may be negative due to a delay in antibody production), individuals may be able to better appreciate that unsafe sex is still risky even after one has received a negative HIV test result. Prevention programs should strike a balance between promoting testing in symptomatic individuals with high-risk exposures and emphasizing that HIV may present without symptoms, making routine HIV testing imperative.
Given that AHI symptoms are relatively non-specific, college health educators should be careful to avoid promoting anxiety about flu-like symptoms in students unlikely to have been exposed to HIV. Messaging about AHI should target at-risk groups of college students, including MSM. Presenting this information to a general college student audience might only promote unnecessary fear in students at low risk for contracting HIV. Health education messages about AHI targeted at MSM students should be simple and straightforward, and should not be designed to arouse fear. They should reassure students that AHI is an uncommon cause of flu-like symptoms relative to other common causes, such as influenza and mononucleosis. Future health education research should examine optimal strategies for communicating with at-risk young MSM about important aspects of AHI transmission, diagnosis, and symptoms.
Among survey participants who would seek care for symptoms that could be due to AHI, most stated that they would see their primary care physician or student health center provider. Prior research has shown that in clinical practice, AHI symptoms are often mistakenly attributed to more common viral illnesses like influenza or mononucleosis.2 Future studies should examine level of provider knowledge, particularly among primary care physicians and college health center providers, about how to recognize AHI symptoms and test for AHI. Improved efforts to diagnose AHI will likely require raising awareness in at-risk populations, including MSM, in addition to improving the capacity of health care providers to better diagnose AHI when infected individuals present to clinic.
A potential challenge in diagnosing AHI is that HIV RNA testing may be unavailable or too costly to implement at many student health centers and community clinics. Clinicians need to take a complete sexual history and be aware of HIV risk factors in all of their patients in order to accurately determine when testing for AHI is warranted. RNA testing in patients with a flu-like illness should be used judiciously and should only conducted in the context of a full clinical picture suggestive of AHI. If cost of an HIV RNA test is prohibitive, repeat HIV antibody testing should be performed at one and three months.
This paper provides preliminary evidence for the construct validity of a new measure of AHI knowledge distinct from prior validated measures assessing general knowledge about HIV/AIDS. According to psychometric theory, correlations of less than 0.70 between related constructs suggest that the constructs are sufficiently different to be considered separately.18,21 In our study, each of the three sub-domains of AHI knowledge as well as the overall AHI knowledge measure had a correlation of less than 0.50 with the general HIV knowledge measure. This indicates that the AHI Knowledge Scale measures components of HIV knowledge distinct from those measured by previously validated general HIV knowledge measures. Validation of a new tool for assessing AHI knowledge in young MSM will require collecting data from additional, diverse samples of young MSM and performing further statistical tests, including a confirmatory factor analysis.
Limitations
These findings are subject to several methodological limitations common to small observational studies. Given the single setting and convenience-sampling design, our findings are not generalizable to all MSM college students. MSM college students attending Ivy League institutions may have higher levels of health literacy than other populations of young MSM. It is unknown whether AHI knowledge levels differ in other adolescent or college student populations. Future research should examine AHI knowledge in similar age peers in order to examine differences in knowledge levels by environment, and to promote validation of an AHI knowledge measure by confirmatory factor analysis. Participation bias, reporting bias and social desirability bias may challenge interpretations of reported HIV risk behaviors; however, the anonymous nature of the survey may help mitigate these biases. Finally, we did not collect data on specific sexual acts (oral vs. vaginal vs. anal sex) and thus were unable to stratify responses based on type of reported unprotected sex. As described in the methods section, respondents were asked about sexual activity and number of sex partners generally without reference to specific sexual acts. Future studies should further disentangle risk by type of sexual act, and sex act by partner gender/sex.
Conclusion
This is among the first known studies of AHI knowledge in a college student sample. In light of recent research showing that up to one-half of all HIV transmissions may be from individuals who were recently infected and of the high risk for HIV in college-age MSM, the importance of educating at-risk college student populations about AHI cannot be understated. Past work has shown that individuals who know their HIV status are less likely to engage in behaviors that put others at risk, while early diagnosis and treatment of HIV has been shown to improve long-term clinical outcomes.6 The period of AHI offers a window of opportunity for diagnosing HIV, since many individuals who present with AHI may be asymptomatic for up to 10 years after they experience these initial symptoms. Public health efforts to help at-risk individuals and providers better recognize these symptoms could be beneficial both in reducing HIV transmission and improving quality-of-life for individuals infected with HIV.
Acknowledgments
This research has been supported by Rhode Island Public Health Institute and facilitated by the infrastructure and resources provided by the Lifespan/Tufts/Brown Center for AIDS Research (Grant Number P30AI042853 from the National Institute of Allergy And Infectious Diseases). Philip A. Chan is supported by a grant (1K23AI096923-01) from the National Institute of Allergy And Infectious Diseases at the National Institutes of Health. The authors wish to thank Dominic Wu for his invaluable assistance with survey instrument development and participant recruitment.
References
- 1.Pilcher CD, Fiscus SA, Nguyen TQ, et al. Detection of acute infections during HIV testing in North Carolina. N Engl J Med. 2005 May 5;352(18):1873–1883. doi: 10.1056/NEJMoa042291. [DOI] [PubMed] [Google Scholar]
- 2.Chu C, Selwyn PA. Diagnosis and initial management of acute HIV infection. Am Fam Physician. 2010 May 15;81(10):1239–1244. [PubMed] [Google Scholar]
- 3.Chan PA, Kazi S, Rana A, et al. [retrieved August 1, 2012];New HIV infections at Southern New England academic institutions: Implications for prevention. AIDS Res Hum Retroviruses. 2012 doi: 10.1089/aid.2012.0130. Epub ahead of print. from http://www.ncbi.nlm.nih.gov/pubmed/22724920. [DOI] [PMC free article] [PubMed]
- 4.Pilcher CD, Tien HC, Eron JJ, Jr., et al. Brief but efficient: acute HIV infection and the sexual transmission of HIV. J Infect Dis. 2004 May 15;189(10):1785–1792. doi: 10.1086/386333. [DOI] [PubMed] [Google Scholar]
- 5.Brenner BG, Roger M, Routy JP, et al. High rates of forward transmission events after acute/early HIV-1 infection. J Infect Dis. 2007 Apr 1;195(7):951–959. doi: 10.1086/512088. [DOI] [PubMed] [Google Scholar]
- 6.Sterne JA, May M, Costagliola D, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009 Apr 18;373(9672):1352–1363. doi: 10.1016/S0140-6736(09)60612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Remien RH, Higgins JA, Correale J, et al. Lack of understanding of acute HIV infection among newly-infected persons-implications for prevention and public health: The NIMH Multisite Acute HIV Infection Study: II. AIDS Behav. 2009 Dec;13(6):1046–1053. doi: 10.1007/s10461-009-9581-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stekler J, Collier AC, Holmes KK, Golden MR. Primary HIV infection education: knowledge and attitudes of HIV-negative men who have sex with men attending a public health sexually transmitted disease clinic. J Acquir Immune Defic Syndr. 2006 May;42(1):123–126. doi: 10.1097/01.qai.0000218357.82970.67. [DOI] [PubMed] [Google Scholar]
- 9.Hightow LB, MacDonald PD, Pilcher CD, et al. The unexpected movement of the HIV epidemic in the Southeastern United States: transmission among college students. J Acquir Immune Defic Syndr. 2005 Apr 15;38(5):531–537. doi: 10.1097/01.qai.0000155037.10628.cb. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention [Accessed October 21, 2011];Fact Sheet–HIV/AIDS among youth. 2008 Available at http://www.cdc.gov/hiv/resources/factsheet/youth.htm.
- 11.Lewis J, Miguez-Burbano M, Malow R. HIV Risk Behavior Among College Students in the United States. College Student Journal. 2009;43(2):475–491. [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) [Accessed December 11, 2012];Behavioral Risk Factor Surveillance System Survey Questionnaire. 2011 Available at http://www.cdc.gov/brfss/questionnaires/english.htm.
- 13.U.S. Centers for Disease Control HIV/STD Behavioral Surveillance Working Group [Accessed December 11, 2012];Core Measures for HIV/STD Risk Behavior and Prevention: Questionnaire-Based Measurement for Surveys and Other Data System: Sexual Behavior Questions. 2001 Available at http://chipts.ucla.edu/resources/?did=196.
- 14.National Coalition for LGBT Health [Accessed December 11, 2012];LGBT Inclusion in Federal Health Surveys. 2010 Available at http://lgbthealth.webolutionary.com/sites/default/files/LGBT%20Inclusion%20in%20Surveys_0.pdf.
- 15.U.S. Centers for Disease Control HIV/STD Behavioral Surveillance Working Group [Accessed December 11, 2012];Core Measures for HIV/STD Risk Behavior and Prevention: Questionnaire-Based Measurement for Surveys and Other Data System: HIV Testing Questions. 2001 Available at http://chipts.ucla.edu/resources/?did=268.
- 16.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS education and prevention: official publication of the International Society for AIDS Education. 2002 Apr;14(2):172–182. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1(1):61–74. [Google Scholar]
- 18.Ping RA. [Accessed August 1, 2012];Testing latent variable models with survey data. 2004 Available at http://home.att.net/~rpingjr/lv1/toc1.htm.
- 19.Roehr B. FDA approves “instant” HIV home test. BMJ. 2012;345:e4636. doi: 10.1136/bmj.e4636. [DOI] [PubMed] [Google Scholar]
- 20.Carballo-Diéguez A, Frasca T, Dolezal C, Balan I. Will Gay and Bisexually Active Men at High Risk of Infection Use Over-the-Counter Rapid HIV Tests to Screen Sexual Partners? J Sex Res. 2012;49(4):379–387. doi: 10.1080/00224499.2011.647117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nunnally JC. Psychometric theory. McGraw-Hill; New York: 1978. (1978) [Google Scholar]