Abstract
Widespread concern about illicit drugs as an aspect of workplace performance potentially diminishes attention on employee alcohol use. Alcohol is the dominant drug contributing to poor job performance; it also accounts for a third of the worldwide public health burden. Evidence from public roadways – a workplace for many – provides an example for work-related risk exposure and performance lapses. In most developed countries, alcohol is involved in 20-35% of fatal crashes; drugs other than alcohol are less prominently involved in fatalities. Alcohol biomarkers can improve detection by extending the timeframe for estimating problematic exposure levels and thereby provide better information for managers. But what levels and which markers are right for the workplace? In this report, an established high-sensitivity proxy for alcohol-driving risk proclivity is used: an average 8 months of failed blood alcohol concentration (BAC) breath tests from alcohol ignition interlock devices. Higher BAC test fail rates are known to presage higher rates of future impaired-driving convictions (DUI). Drivers in alcohol interlock programs log 5-7 daily BAC tests; in 12 months, this yields thousands of samples. Also, higher program entry levels of alcohol biomarkers predict a higher likelihood of failed interlock BAC tests during subsequent months. This report summarizes selected biomarkers’ potential for workplace screening. Markers include phosphatidylethanol (PEth), percent carbohydrate deficient transferrin (%CDT), gammaglutamyltransferase (GGT), gamma %CDT (γ%CDT), and ethylglucuronide (EtG) in hair. Clinical cutoff levels and median/mean levels of these markers in abstinent people, the general population, DUI drivers, and rehabilitation clinics are summarized for context.
Keywords: alcohol, biomarkers, DUI, workplace, public safety
Alcohol and Illicit Drug Use Prevalence in a General Population
When focusing on the workplace consequences and prevalence of drug abuse, as researchers, we should remember to keep alcohol use in its proper position at the top of the drug risk hierarchy. Cocaine and heroin lead all other illicit drugs in the likelihood of causing dependence among users, and those drugs carry a higher likelihood of dependence than are found among alcohol users. Nonetheless alcohol, despite a proportionally lower per user dependence risk, has a population prevalence that exceeds all illicit drug dependencies by 5 to 1. In the United States, Grant, Dawson and Moss[1] disaggregated data from the large National Epidemiological Survey on Alcohol and Drug Related Conditionsb (NESARC) of adults (age 18+) and produced 12-month prevalence estimates and conditional probabilities of dependence for alcohol, tobacco, and 9 types of illicit drugs. Their projections are based on an estimated 209 million adults in the US population. They report 65% of US adults drink alcohol (136 million) with 5.8% of drinkers (7.9 million) meeting DSM IV (Diagnostic and Statistical Manual 4 of the American Psychiatric Association) criteria for dependence in the past year (similar to ICD-10 criteria). By contrast 1.6 million, less than 1% of adults, are dependent on all other types of illicit drugs. Based on NESARC, among USA adults there are roughly 5 times more who are dependent on alcohol than on illicit drugs, and adults are well over 10 times more likely to use alcohol than illicit drugs.
Dependence, however, is not the core problem either in workplace safety or in road safety, but it is one metric available for estimating problem magnitude. The real problem is about the number of people who place themselves and others at risk due to their use of impairing substances, whether or not they are dependent. Kreitman[2] showed that while low- to moderate-volume drinkers are more common and have lower individual risk of alcohol-related harm relative to high-volume drinkers, the number of lower-risk drinkers relative to higher-risk drinkers makes that subpopulation a greater contributor to the societal risk. Work by Stockwell et al.[3] endorses and extends this insight. In a medical context, dependence is the central problem of interest; however, in a public health and safety context – workplace or otherwise – the central concern is performance and risk exposure by employees, customers, and the general public. Because of the prevalence of use and abuse, alcohol remains the most significant public drug hazard. The roadways are the global commons, bringing together commercial, public, and private travelers. Everyone depends on the safe practices of others; this is true whether the roads are the workplace of commercial and government operators or just for leisure travel. Program administrators have an incentive to use the best methods of risk surveillance available to keep our roadways safe. This reasoning can be extended to all workplaces, and general workplace drug issues can be informed by looking at alcohol risk on the roadways.
Alcohol Risk and Control on the Roadways
People convicted of driving under the influence (DUI) of alcohol for the first time (first DUI offenders) comprise about 60-75% of all DUI arrests in most US states. Although DUI arrest is only a low-sensitivity proxy for public risk exposure, it does suggest that among DUI offenders, first-time DUI offenders contribute a significant share of overall alcohol road risk relative to repeat offenders. The chance of any alcohol-impaired driver actually being arrested is very low, particularly in countries like the US, Canada, and the UK that do not conduct random roadside breath testing. In the US, the likelihood of arrest for operating while alcohol impaired are estimated to range from about 1 chance in 300 in a high-enforcement area[4] to about 1 chance in 1700[5] nationally.
In North America, and increasingly in Europe and Australia, alcohol ignition interlock devices are used to control DUI offenders after arrest and adjudication. Canada and the US have had active programs for more than 20 years. In the US, with approximately 1.4 million DUI arrests per annum (estimated 1 million convictions), there were 212,000 interlocks in service in 2010 with a brisk growth rate of about 10% per year. As of 2011, all 50 US states now have an interlock program for DUI offenders, and Canada has an interlock program in all 10 provinces, as well as in the Yukon and Northwest territories. Interlocks require that a driver produce a low-BAC (breath estimate of blood alcohol concentration) or alcohol-free breath sample before a vehicle’s engine can be started.
In Europe, only Sweden has an active nationwide alcohol interlock program,c and the Swedish program has been underway since the 1990s. Unlike the US and Canada that focus their interlock programs almost exclusively on convicted DUI offenders, the majority of Sweden’s interlocks are installed on public transport vehicles or commercial vehicles. Some Swedish DUI offenders also get interlocks, but the Swedes’ strong emphasis on workplace vehicle interlocks is unique. Much of Sweden’s program is for primary or general prevention, wherein drivers of trucks or public conveyances, such as buses, are required to provide operator breath samples at the beginning of travel. As of 2011, more than 75,000 interlocks are used in the Swedish program; 47% of all buses have interlocks and 23% of trains. Sweden has set a near-term goal of achieving a 75% installation rate on all publicly owned vehicles.[6] The Swedes have embraced the alcohol interlock as a workplace intervention (when the workplace is a vehicle). Sweden has a population of about 9 million; per capita, there is an interlock for every 120 people. This rate is 10 times higher than the per capita interlock installation rate in the USA where perhaps 99% of interlocks are installed on the vehicles of alcohol offenders but rarely in “safety sensitive” workplace vehicles as a precautionary measure.
Interlock BAC Data
In addition to preventing operation of a vehicle when someone is impaired by alcohol, the interlock device is also an excellent source of predictive information about drivers who use them. Interlocks log all start attempts and store a record of all breath tests taken as well as a record of compliance with procedures such as retest requests and anti-circumvention protocols. Research by PIRE (Pacific Institute for Research and Evaluation in Calverton, Maryland) over the past 20 years[7] [8] [9] [10] [11] [12] has shown that the rate of failed BAC tests strongly predicts the likelihood of post-interlock re-arrest. That is, the interlock device log files can provide a high-sensitivity estimate of the future likelihood of impaired driving among convicted DUI offenders. In Québec, Canada, and New Mexico USA, for example, interlock users who had the top 10% highest rates of failed interlock BAC tests while in the interlock program had, after device removal, a 20-25% reconviction rate for impaired driving within 24 months – this is up to 5 times higher than the average DUI conviction rate,[10] [11] and 10 times higher than the rate for those who had no failed tests. Accordingly, the BAC test failure rate is an excellent high-sensitivity proxy for future alcohol road risk.
Related to the overall rate of failed BAC tests serving as an advance indicator of post-interlock (after removal) alcohol-impaired driving, the interlock drivers with the highest rates of failed interlock BAC tests in the morning hours (7 to 9 AM weekdays and 10 AM to noon weekends) are more likely to later be re-arrested for DUI after interlock removal. In fact, even though most vehicle start attempts occur in late afternoon, the morning hours are the time of day most likely to result in failed interlock BAC tests. Although this may seem counterintuitive, it appears that the drinking of drivers the night before result in BAC levels high enough to still be elevated above the lockout level the following morning. At an average rate of alcohol metabolism, .017 g/dL/hr (grams/deciliter/hour), BAC continues to rise for an hour or more after drinking ceases, so if the peak BAC occurs at 1 AM at a level near that of the average arrested alcohol-impaired driver (i.e., ~.16 g/dL), it would require approximately 8 to 9 hours to zero out. Accordingly, those who drink to just an average BAC level for a DUI offender during the evening hours will occasionally awaken to start their cars in the morning and be locked out. PIRE researchers[9] [10] believe that these failed BAC tests in the morning reflect drivers with substantial commitments to heavy drinking, and failed BAC tests in the morning hours enter into a regression model of factors explaining DUI recidivism, even after accounting for overall rates of failed BAC tests. This finding could also serve as a supportive basis for using simple breath BAC testing in safety sensitive occupations at the beginning of work shifts.
In recent work, Marques et al. [12] have used the interlock BAC fail test rate to estimate the relationship between 3 methods for estimating driver alcohol risk. These include levels of different alcohol biomarkers, records of prior DUI offenses, and a panel of psychometric assessments. Biological specimens included the blood, hair, and urine for measurement of 9 alcohol biomarkers among DUI offenders who use alcohol interlock devices. Drivers with the highest rates of failed interlock BAC tests also showed significantly higher program entry levels of alcohol biomarkers. Alcohol biomarkers accounted for more variance than prior DUI convictions or psychometric assessments.
To render this information useful to the discussion of workplace drug and alcohol performance problems, this report compares biomarker levels from DUI offenders and alcoholism clinic patients in an attempt to define a preliminary panel of biomarkers that may be of use for estimating problem levels of drinking among operators of workplace vehicles or possibly other workplace equipment. The use of interlock BAC test records is an important development because until now most efforts to evaluate, or score, biomarker adequacy and cutoff levels has been based on self-reported drinking and/or clinical judgment. Subjective judgment and self-report assessments are important aspects of categorizing alcohol problem magnitude, but these are not a fully satisfying basis for evaluating the adequacy of objective indicators, such as alcohol biomarkers retrieved from body matrices. Most clinical research studies of alcohol biomarkers evaluate specificity and sensitivity on ROC (Receiver Operator Characteristic) curves by relying on either clinical judgment, or a score of 8 or above on the self-reported AUDIT (Alcohol Use Disorders Inventory), for setting the criterion. Use of BAC test failure rates as a criterion is unconventional and not yet widely available; nonetheless, it provides an objective extended time series for scoring actual behavior. The decision to regard an employee as a risk due to excessive drinking is necessarily a somewhat subjective process that is made less arbitrary by having objective indicators to complement subjective indicators. Failed interlock BAC test rates and alcohol biomarkers can provide that objectivity.
Alcohol Biomarkers
This brief report is not intended to be an authoritative summary of alcohol biomarkers. There are many excellent sources that can be easily retrieved; some of these appear below.
Alcohol biomarkers can be indirect or direct indicators of drinking. Direct markers are usually products of minor ethanol metabolic pathways and/or are formed only in the presence of ethanol. Examples include ethanol itself, ethylglucuronide (EtG), phosphatidylethanol (PEth), and fatty acid ethyl esters (FAEE). All these markers have excellent sensitivity and specificity, directly reflect levels of consumed alcohol, and persist in body fluids for days or weeks longer than ethanol itself. Clinical studies and the basic science can be found in any of several papers.[13] [14] [15] [16] Direct markers can be measured in urine, blood, or hair. EtG measured in urine or blood adds 1 or 2 days to ethanol detection following acute dosing, whereas PEth, when found in heavy drinkers can take weeks to fall to zero following drinking cessation.[16] When measured in hair samples, EtG provides a long-term exposure indicator [17] and can serve as objective alternatives to confessional estimates of historical alcohol use. Recent data show EtG in hair to be a stable indicator of use over several months of prior alcohol use[18] [19] and is now an acceptable alternative to more conventional alcohol markers in Germany for making driver fitness judgments.[20] Regarding PEth, Marques et al.[12] reported PEth to be the single alcohol marker among 9 others to have the strongest intercorrelation with other alcohol markers, the largest F ratio distinguishing 3 risk groups of drivers, and the strongest relationship with ~ 16 subscales from 3 different psychometric assessments in a DUI study.
Indirect alcohol markers are often thought to be indicators of alcohol disease, such as alcohol dependence or alcoholism. Among the indirect type of blood alcohol markers, many are either insensitive or nonspecific. The latter include liver enzymes alanine aminotransferase (ALT), aspartate aminotransferase (AST), and mean red cell volume (MCV). There are at least two, however, that are good indirect markers of longer-term ethanol use: gammaglutamyltransferase (GGT) and carbohydrate deficient transferrin (CDT). GGT is a liver enzyme that is often elevated after chronic alcohol consumption but is best when used in combination with other markers, as it can also be elevated because of diseases unrelated to alcohol use (e.g., biliary disease). In healthy people, CDT is quite specific to alcohol use. CDT is an iron transport protein (transferrin) that has lost some of its carbohydrate containing sialic acid end groups as a result of regular ethanol exposure, the amount of carbohydrate deficiency strongly reflects ethanol exposure and the transferrin becomes increasingly deficient after regular consumption of about 60 g ethanol per day. The relative percentage of carbohydrate deficiency (%CDT) of transferrin, even more so than total CDT, is thought by some experts[21] to improve the utility of the marker by overcoming some age and gender-related variation that is uncontrolled when measuring total CDT. Indirect markers often decline within a few weeks after alcohol use ceases.[22] Unlike the other indirect markers noted above, GGT, and %CDT have both acceptable to good specificity and moderate to good sensitivity. Sillanaukee and Olsen[23] demonstrated that a log combination of GGT and CDT (1.3*ln CDT + 0.8 * ln GGT), that they dubbed gamma CDT or γCDT, provides a better estimate of alcohol exposure than either marker alone. Later, Antilla et al.,[24] also in Finland, reported that the log transformation formula works as well with %CDT and GGT to yield γ%CDT. Berner et al.,[25] in a large German study, found distinct advantages to combining the GGT and %CDT markers to improve sensitivity, especially for women. As with Antilla et al.[24] and Berner et al.,[25] Marques et al.[26] found the combined marker, γ%CDT, to have higher predictive validity for detecting the highest-risk group in an interlock DUI population than did either marker alone.
The biomarker levels of 287 interlock-using DUI offenders were studied in three risk groups based on differing rates of failed BAC tests. Risk categories were defined as the 27% who had zero failed BAC tests, the 53% with a low level of failed BAC tests (less than 1%), and the 20% with a high rate of failed tests (more than 3%). Failure in this case was defined as tests greater than or equal to .04 g/dL when attempting to start a vehicle. Those with the high rates of failed BAC tests had significantly (P<.0001) higher levels of alcohol biomarkers, including PEth, GGT, %CDT, and γ%CDT.[12] [26] A subset of these drivers (n=121) also provided hair samples for the measurement of EtG in hair.
Categorizing Problem Drinking Based on Alcohol Biomarkers
The question addressed here is what levels of different alcohol biomarkers might be indicative of problem drinking among employees at the workplace? This is approached by cataloguing values from different subpopulations. These subpopulations are:
People who can be considered alcohol free or abstinent;
Those who fall into a group of light social drinkers or an average level of a marker measured in a general population;
Those who are DUI offenders and in an alcohol ignition interlock program;
A subset of DUI offenders known to be a higher-risk segment of the drinking-driver population based on their high fail rates on interlock tests;
People who enter an alcohol dependence rehabilitation clinic as an outpatient, or patients who otherwise have lower measured levels than known inpatients; and
Patients who are specifically admitted to a hospital or residential treatment center for inpatient treatment services for alcohol dependence.
The severity sequence in this list and the levels of alcohol marker are directly related. Inpatients are those who are undergoing the most restrictive type of treatment and usually are the heaviest drinkers with the most intractable dependence. The data in Table 1 were compiled from several published research studies (literature citations are shown below the table). Normative values in unadjusted skewed distributions (skew is typical for distributions anchored at zero) are often better represented by the median value than the mean; however, the mean is also a useful indicator of dispersion, especially upper-end spread. Accordingly, Table 1 shows both a group median and a group mean available from the published studies. Of the five markers shown, the only one with a symmetrical/normal distribution is the log transformed γ%CDT.
TABLE 1.
Median and mean levels of 5 alcohol biomarkers from 6 types of samples reported in 8 studies
| Marker | Abstinent | General Population |
DUI overall sample average |
DUI high-risk group |
Alcohol Clinic Outpatient/lower |
Alcohol Clinic Inpatient/higher |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| median | mean | Median | mean | median | mean | median | mean | Median | mean | median | mean | |
| PEth μmol/liter | undetectable | Low | low | 0.5 | 0.7 | 1.0 | 1.5 | 2.9 | 3.4 | 7.5 | 7.7 | |
| GGT U/liter1 | 12 | 24 | 35 | 28 | 48 | 40 | 92 | 78 | 199 | 102 | 307 | |
| % CDT2 | 1.6 | 1.9 | 2.1 | 2.5 | 2.7 | 2.9 | 3.2 | 2.3 | 3.9 | 4.3 | 6.0 | |
| y%cdt3 | 2.75 | 3.3* | 3.4 | 3.9 | 4.0 | 4.6 | 4.6 | 4.6* | 5.4 | 5.6* | 6.9* | |
| Hair EtG pg/mg4 | <7 5 | low6 | low6 | 23 | 53 | 33 | 69 | 108 | 159 7 | 214 | 388 8 | |
Estimate calculated from sample statistics for GGT, %CDT.
Clinical cutoff recognized GGT 50-70 U/l depending on source.
Clinical cutoffs recognized %CDT > 2.6%.
Calculated cutoff γ %CDT ~ 4.4-4.7 based on published cutoffs for GGT and %CDT.
Cutoff for excessive/problem drinking from hair EtG > 30 pg/mg by EWDTS.
Accepted as criterion for abstinence by EWDTS; other studies report lower levels in abstainers.
Kronstrand et al.[28] studied 7 men having 2 drinks/day for 3 months resulting in just 4 positives with EtG ranging 5-11 pg/mg; similarly, Yegles et al.[35] reported moderate social drinkers with hair EtG < 2 pg/mg.
Mean calculated from raw data provided in Yegles et al.[35] from patients in treatment.
Mean calculated from clinic patients raw data provided in H0iseth.[15]
Gammaglutamyltransferase (GGT): Berner et al.[25]; Marques et al.[12]; Antilla et al.[24]; Aradottir et al.[14]
Percent carbohydrate deficient transferrin (%CDT): Antilla et al.[24]; Marques et al.[12]; Aradottir et al.[14]
The studies selected for inclusion in Table 1 were generally found to be typical of the levels reported by others. Although there are differing approaches to measuring each marker, the values and studies included in Table 1 generally represent uniform measurement approaches so there is a basis for comparison across studies. For example, the marker %CDT rather than total CDT was chosen. Accordingly, the Antilla et al.[24] log normalization and combination method was selected for calculation of gamma %CDT (γ%CDT) rather than the method of Sillanaukee and Olson[23] that first calculated γCDT. Total PEth in μmol/liter are all based on the HPLC (high performance liquid chromatography) evaporative light scattering detection method developed at the Lund University laboratory in Sweden, rather than the LC/MS/MS (liquid chromatography/ tandem mass spectrometry) method that targets specific subspecies of PEth. The measurement of EtG in hair has been conducted by slightly different methods. Several of the hair EtG analyses in studies summarized in Table 1 were performed by Michel Yegles in Luxembourg via GC/MS (gas chromatography/mass spectrometry). Other methods are also used; the values shown for inpatient alcoholics came from Høiseth et al.[15] who used LC/MS/MS following the methods described by Morini et al.[27] Høiseth commented that her maximum values of hair EtG were somewhat higher than other reports. The Kronstrand et al.[28] study of hair EtG among social drinkers was done by LC/MS/MS. Their subjects consumed a fixed daily amount of alcohol, and this helped to define the lower end of the continuum. Agius and colleagues[18] recently reported a headspace solid phase microextraction method in combination with a GC/MS/MS (gas chromatography/ tandem mass spectrometry) procedure to measure hair EtG.
Alcohol treatment researchers who study alcohol biomarkers have established most of the cutoff boundaries that clinicians use for making judgments about problem levels of drinking. Those levels—> 2.6 %CDT, GGT 50-70 U/liter, a calculated γ%CDT of 4.6, and hair EtG >30 pg/mg—all suggest chronic or excessive alcohol use. As is evident in Table 1, these cutoffs are often near the levels found in the median or mean values of the high-risk DUI offenders group. Those average levels mean that about a quarter to a half of the high-risk DUI offender group are above the clinical cutoffs. Some individual values are well into the clinical alcoholism ranges. This conceptualizes the order of things needing attention in the workplace. In the US, for example, an alcohol-impaired driving fatality occurs on average every 48 minutes.[29] Although the biomarker levels found for DUI offenders are often less than the averages of people who are in treatment for alcohol dependence, their levels are above those of average social drinkers. To some extent, those convicted of impaired driving help illustrate the boundary might be, above the line for public safety or health concerns, but still near or below the clinical range of alcohol dependence. The levels of alcohol biomarkers among DUI offenders may help inform workplace alcohol use problem level cutoffs.
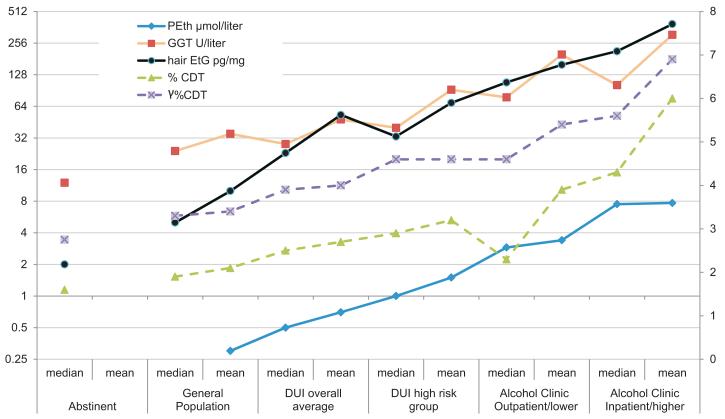
The marker values are shown in Table 1 and are represented graphically in Figure 1. In Figure 1, three of the markers—PEth, GGT, hair EtG—shown with solid lines, reference the Y1 axis to the left (log base 2); the two markers with dashed lines (%CDT and γ%CDT) reference the linear Y2 axis to the right. The values near zero for hair EtG, as shown in Table 1 and its notes, are represented in the graph as estimated values. Although the hair EtG cutoff for abstinence is 7 pg/mg proposed by Pragst and Yegles[17] and adopted by EWDTS (European Workplace Drug Testing Society),[30] the Kronstrand et al.[28] study suggests that social drinkers, or those who consume 2 daily drinks for 3 months, have EtG actually below the EWDTS cutoff for teetotalers. Accordingly, in the chart, abstinence is coded as 2 pg/mg and social drinkers/general population at 5 and 10 pg/mg, respectively, for median and mean. Some of these differences in minimal measured levels may be methodological or reflect the binge or non-binge drinking of study subjects.
Figure 1.
Median and mean levels of 5 alcohol biomarkers from 6 categories of alcohol consumers. Marker levels with solid lines reference left axis; marker levels with dashed lines reference right axis.
Discussion
If employers want to identify drug-related impediments to better workplace performance, they will want to seriously consider the potential role of alcohol biomarkers, more so than just the measurement of alcohol itself, as a way to estimate problem magnitude. Alcohol has a short half life, and the impact of regular excessive use of alcohol on job performance extends well beyond the period that the BAC is elevated. Alcoholism, or alcohol dependence, are not preconditions for impaired workplace performance, but regular or episodic heavy consumption of alcohol is. The biggest workplace in the world – the public roadways – provides sufficient evidence to establish the central role played by alcohol in fatal accidents. In the USA, there is a fatal alcohol-involved crash every 48 minutes. The nations of the European Union have a higher population base (~500 million to the USA ~310 million) and, according to Rehm et al.,[31] a higher per capita consumption of alcohol (e.g., 12-15 liters EU relative to 9-12 liters for the USA). Unlike the USA, many nations of the EU already use alcohol biomarkers as part of the driver fitness evaluations before license restitution. Workplaces, especially those that are safety sensitive, might do well to follow that lead.
There are many alcohol biomarkers available for evaluation. The most common specimens used for the analysis of alcohol biomarkers come from urine, blood, and hair. A major distinction of alcohol marker types is indirect or direct. Indirect markers are usually an enzyme or other physiological product or indicator that reflects longer-term change in the body as a consequence of repeated exposure to alcohol. Direct markers are often a product of a minor metabolic pathway of alcohol or some other change that is specifically related to the level of alcohol consumption. Both types are important in different ways and both are important to consider in a panel of markers. The 5 markers included in this report were the best mix of direct/indirect and medium/long-term indicators in the Marques et al., [12] DUI study and may not be the best in all situations. The best markers to use depend on the questions that need an answer. For example, markers found in blood or urine can be analytically precise but reflect a short exposure interval, those recovered from hair are excellent objective alternatives to self-reported consumption history but can be less precise.
A caveat with measuring markers in hair is the potential variability in measurement due to influences on the exposed hair shaft as well as sample preparation methods. Research in the past decade has shown there are two credible long-term direct alcohol markers that can be measured in hair: EtG and fatty acid ethyl esters (FAEE). There is some suggestion in the literature that there is a benefit from combining measurements of both EtG and FAEE in hair. [32] Recent studies, however, indicate that EtG in hair seems to be a better marker than FAEE, especially for documenting alcohol abstinence assessment. [33] [34] The Marques et al. [12] DUI study findings are in accord with that conclusion, showing significant differences by interlock risk group with EtG in hair but not FAEE. The FAEE results were in the righ direction, but were highly variable and had less statistical power due to 1/3 fewer cases for analysis than with EtG samples.
A caveat with hair is potential variability in measurement due to influences on the exposed hair shaft and sample preparation methods.[34] Hair samples can yield two good long-term direct alcohol markers, EtG and fatty acid ethyl esters (FAEE). In the Marques et al. DUI study, the hair FAEE results were less consistent than the hair EtG, possibly because there were a third fewer samples measured and because EtG in hair is an inherently less variable marker.[33] The research literature suggests there may be a benefit from combining measurements of both EtG and FAEE in hair.[32]
The five alcohol biomarkers summarized in this review were among the best performing markers in the Marques et al.[12] [26] DUI study. Other excellent markers from that study, which are not summarized here, are EtG or EtS (ethyl sulfate) in the urine. The window of detection of EtG and EtS in urine, at approximately 2 days after acute dosing, may not be long enough to make them significantly more useful than the measurement of alcohol per se. Nonetheless, both urine EtG and EtS are very sensitive and specific markers that are exceptionally useful when the detection question is targeted to recent alcohol usage. The markers represented in Table 1 and Figure 1 reflect a detection window of at least one or more weeks and are therefore somewhat less affected by a single episode of acute dosing. The EWDTS provides useful guidelines for the collecting and measuring specimens and methods for the measurement of ethanol product in hair.[30]
Research studies of alcohol biomarkers usually report measured values as sample mean, sample median, or the proportion of a sample above and below a specific cutoff. The tabled and charted data provide the medians and means and allow somewhat for appraisal of cutoffs in reference to published reports by clinical alcoholism researchers. It should be cautioned that the data shown represent values in study samples reported in the literature, not a mathematical combining of multiple studies. Accordingly, the values shown are not definitive representations of the median and mean alcohol biomarkers that will be found by others in the future with similar samples or in studies that have already been published in the literature. There are many clinical studies of alcohol biomarkers, and there is not yet uniform agreement as to how best to measure or report all these markers.
In Table 1, for both DUI offender and clinical populations, the values shown represent the biomarker status at the beginning of a behavior change intervention, whether interlock or treatment. There is heterogeneity in the data including methodological differences, laboratory differences, analytic differences, sample differences, and estimates of central tendency from small sample sizes mixed together with those of large sample sizes. Therefore, the tabled and charted values are just estimates and offer an initial framework for policymakers who will need to have some context for interpreting the meaning of a laboratory value. Currently, this knowledge resides primarily in the small community of forensic toxicologists, epidemiologists, and other researchers who read this literature. For these new biomarker tools to be made understandable to the larger group of administrators, judges, physicians, psychologists, and counselors who help to rehabilitate patients or who help to keep our roadways safe, efforts such as this are warranted if they can simplify without being too simplistic.
Acknowledgement
This research was supported by the National Institute on Alcohol Abuse and Alcoholism (grants R01 AA014206, R21 AA019696, and P20 AA017831).
Footnotes
An earlier version of this paper was presented at the European Workplace Drug Testing Society Meeting, Edinburgh, Scotland, June 20, 2011
The NESARC is a general population survey in which the subjects are a random, representative sample of adults in the USA. NESARC respondents were selected at random from household samples aged 18 or older; the sample—43,093 respondents – can be accurately generalized to the US adult population.
The Netherlands is close to or has recently implemented a nationwide interlock program. Other EU nations have regional or pilot interlock programs underway.
References
- [1].Grant BF, Dawson DA, Moss HB. Disaggregtating the burden of substance dependence in the United States. Alcoholism. 2011;35(3):387–388. doi: 10.1111/j.1530-0277.2011.01433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kreitman N. Alcohol consumption and the preventive paradox. Br J Addict. 1986;81:353–363. doi: 10.1111/j.1360-0443.1986.tb00342.x. [DOI] [PubMed] [Google Scholar]
- [3].Stockwell T, Hawks D, Lang E, Rydon P. Unravelling the preventive paradox for acute alcohol problems. Drug Alcohol Review. 1996 Mar;15(1):7–15. doi: 10.1080/09595239600185611. [DOI] [PubMed] [Google Scholar]
- [4].Voas RB, Hause JM. Deterring the drinking driver: The Stockton experience. Accid Anal Prev. 1987;19(2):81–90. doi: 10.1016/0001-4575(87)90027-3. [DOI] [PubMed] [Google Scholar]
- [5].Miller TR, Spicer RS, Levy DT. How intoxicated are drivers in the United States? Estimating the extent, risks, and costs per kilometer of driving by blood alcohol level. Accid Anal Prev. 1999;31:515–523. doi: 10.1016/s0001-4575(99)00008-1. [DOI] [PubMed] [Google Scholar]
- [6].Jakobsson L. The Swedish work with alcoholics. Trafikverket, Swedish Transportation Administration; [Google Scholar]
- [7].Marques PR, Voas RB, Tippetts AS, Beirness DJ. Behavioral monitoring of DUI offenders with the alcohol ignition interlock recorder. Addiction. 1999;94(12):1861–1870. doi: 10.1046/j.1360-0443.1999.9412186111.x. [DOI] [PubMed] [Google Scholar]
- [8].Marques PR, Tippetts AS, Voas RB, Beirness DJ. Predicting repeat DUI offenses with the alcohol interlock recorder. Accid Anal Prev. 2001;33(5):609–619. doi: 10.1016/s0001-4575(00)00074-9. [DOI] [PubMed] [Google Scholar]
- [9].Marques PR, Tippetts AS, Voas RB. Comparative and joint prediction of DUI recidivism from alcohol ignition interlock and driver records. J Stud Alcohol. 2003;64(1):83–92. doi: 10.15288/jsa.2003.64.83. [DOI] [PubMed] [Google Scholar]
- [10].Marques PR, Voas RB, Tippetts AS. Behavioral measures of drinking: Patterns in the interlock record. Addiction. 2003;98(Suppl 2):13–19. doi: 10.1046/j.1359-6357.2003.00584.x. [DOI] [PubMed] [Google Scholar]
- [11].Marques PR, Voas RB, Roth R, Tippetts AS. Evaluation of the New Mexico Ignition Interlock Program. National Highway Traffic Safety Administration; Washington, DC: 2010. (DOT HS 811 410) [Google Scholar]
- [12].Marques P, Tippetts S, Allen J, Javors M, Alling C, Yegles M, Pragst F, Wurst F. Estimating driver risk using alcohol biomarkers, interlock BAC tests, and psychometric assessments: Initial descriptives. Addiction. 2010;105(2):226–239. doi: 10.1111/j.1360-0443.2009.02738.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Litten RZ, Bradley AM, Moss HB. Alcohol biomarkers in applied settings: Recent advances in future research opportunities. Alcoholism. 2010;34(6):955–967. doi: 10.1111/j.1530-0277.2010.01170.x. [DOI] [PubMed] [Google Scholar]
- [14].Aradottir S, Asanovska G, Gjerss S, Hansson P, Alling C. Phosphatidylethanol (PEth) concentrations in blood are correlated to reported alcohol intake in alcohol-dependent patients. Alcohol Alcohol. 2006;41(4):431–437. doi: 10.1093/alcalc/agl027. [DOI] [PubMed] [Google Scholar]
- [15].Høiseth G, Morini L, Christophersen A, Mørland J. Ethyl glucuronide in hair campared with traditional alcohol biomarkers – A pilot of heavy drinkers referred to an Alcohol Detoification Unit. Alcoholism. 2009 May;33(5):812–816. doi: 10.1111/j.1530-0277.2009.00900.x. [DOI] [PubMed] [Google Scholar]
- [16].Wurst FM, Thon N, Aradottir S, Hartmann S, Wiesbeck G, Lesch O, Skala K, Wolfersdorf M, Weinmann W, Alling C. Phosphatidylethanol: Normalisation during detoxification, gender aspects and correlation with other biomarkers and self-reports. Addict Biol. 2010;15(1):88–95. doi: 10.1111/j.1369-1600.2009.00185.x. [DOI] [PubMed] [Google Scholar]
- [17].Pragst F, Yegles M. Chapter 14: Alcohol markers in hair. In: Kintz P, editor. Analytical and Practical Aspects of Drug Testing in Hair. CRC Press, Taylor and Francis Group; Boca Raton, FL: 2007. pp. 287–323. [Google Scholar]
- [18].Agius R, Nadulski T, Kahl HG, Schräder J, Dufaux B, Yegles M, Pragst F. Validation of a headspace solid-phase microextraction-GC-MS/MS for the determination of ethyl glucuronide in hair according to forensic guidelines. Forensic Sci Int. 2010 Mar 20;196(1-3):3–9. doi: 10.1016/j.forsciint.2009.07.023. [DOI] [PubMed] [Google Scholar]
- [19].Liniger B, Nguyen A, Friedrich-Koch A. Abstinence monitoring of suspected drinking drivers: Ethyl glucuronide in hair versus CDT. Traffic Inj Prev. 2010 Apr;11(2):123–126. doi: 10.1080/15389580903518280. [DOI] [PubMed] [Google Scholar]
- [20].Dufaux B. A two years experience with lowered cut-off values for drugs of abuse in urine and hair. 7th Symposium on Workplace Drug Testing; Musselburgh, Edinburgh, Scotland. Queen Margaret University; European Workplace Drug Testing Society; [Google Scholar]
- [21].Jeppsson JO, Arndt T, Schellenberg F, Wielders JP, Anton RF, Whitfield JB, Helander A. International Federation of Clinical Chemistry and Laboratory Medicine Working Group on Standardization of Carbohydrate-deficient Transferin (IFCC-WG-CDT), Toward standardization of carbohydrate-deficient transferrin (CDT) measurements: I. Analyte definition and proposal of a candidate reference method. Clin Chem Lab Med. 2007;45(4):558–562. doi: 10.1515/CCLM.2007.107. [DOI] [PubMed] [Google Scholar]
- [22].Jones AW. Biomarkers of acute and chronic alcohol ingestion. In: Garriott JC, editor. Garriott’s Medicolegal Aspects of Alcohol. Fifth Edition Lawyers & Judges Publishing Company; Tucson, AZ: 2008. [Google Scholar]
- [23].Sillanaukee P, Olsson U. Improved diagnostic classification of alcohol abusers by combining carbohydrate-deficient transferrin and gamma-glutamyltransferase. Clin Chem. 2001;47(4):681–685. [PubMed] [Google Scholar]
- [24].Antilla P, Järvi K, Latvala J, Blake JE, Niemelä O. A new modified γ-%CDT method improves the detection of problem drinking: studies in alcoholics with or without liver disease. Clinica Chimica Acta. 2003;338(1):45–51. doi: 10.1016/j.cccn.2003.07.016. [DOI] [PubMed] [Google Scholar]
- [25].Berner M, Bentele M, Kriston L, Mänz C, Hans-Willi C, Härter M, Mundle G. DOVER and QUVER — New marker conbinations to detect and monitor at-risk drinking. Alcoholism. 2006 Aug;30(8):1372–1380. doi: 10.1111/j.1530-0277.2006.00163.x. [DOI] [PubMed] [Google Scholar]
- [26].Marques P, Hansson T, Isaksson A, Walther L, Jones J, Lewis D, Jones M. Detection of phosphatidylethanol (PEth) in the blood of drivers in an alcohol ignition interlock program. Traffic Inj Prev. 2011;12(2):136–141. doi: 10.1080/15389588.2010.544048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Morini L, Politi L, Groppi A, Stramesi C, Polettini AJ. Determination of ethyl glucuronide in hair samples by liquid chromatography/electrospray tandem mass spectrometry. Mass Spectrometry. 2006 Jan;41(1):34–42. doi: 10.1002/jms.943. [DOI] [PubMed] [Google Scholar]
- [28].Kronstrand R, Brinkhage L, Nyström FM. Ethyl glucuronide in human hair after daily consumption of 16 or 32g of ethanol for 3 months. Forensic Sci Int. 2011 doi: 10.1016/j.forsciint.2011.01.044. [DOI] [PubMed] [Google Scholar]
- [29].National Center for Statistics and Analysis . Traffic Safety Facts: 2009 Data; Alcohol-Impaired Driving. U.S. Department of Transportation, National Highway Traffic Safety Administration; Washington, DC: 2010. DOT HS 811 385. [Google Scholar]
- [30].Agius R, Kintz P. Guidelines for European workplace drug and alcohol testing in hair. Drug Test Anal. 2010;2:367–376. doi: 10.1002/dta.147. [DOI] [PubMed] [Google Scholar]
- [31].Rehm J, Mather C, Popova S, Thavorncharoensas M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. The Lancet. 2009;373(9682):2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- [32].Pragst F, Rothe M, Moench B, Hastedt M, Herre S, Simmert D. Combined use of fatty acid ethyl esters and ethyl glucuronide in hair for diagnosis of alcohol abuse: Interpretation and advantages. Forensic Sci Int. 2010;196(1-3):101–110. doi: 10.1016/j.forsciint.2009.12.028. [DOI] [PubMed] [Google Scholar]
- [33].Albermann ME, Musshoff F, Madea B. Comparison of ethyl glucuronide (EtG) and fatty acid ethyl esters (FAEEs) concentrations in hair for testing abstinence. Analytical and Bioanalytical Chemistry. 2010 Dec 3;400(1):175–181. doi: 10.1007/s00216-010-4443-8. Epub. Epub. [DOI] [PubMed] [Google Scholar]
- [34].Gareri J, Appenzeller B, Walasek P, Koren G. Impact of hair-care products on FAEE hair concentrations in substance abuse monitoring. Analytical and Bioanalytical Chemistry. 2011;400(1):183–188. doi: 10.1007/s00216-011-4685-0. [DOI] [PubMed] [Google Scholar]