Abstract
It is well recognized that an interdisciplinary approach is essential in the development and implementation of solutions to address the current pediatric obesity epidemic. In two half‐day meetings that included workshops and focus groups, faculty from diverse fields identified critically important research challenges, and gaps to childhood obesity prevention. The purpose of this white paper is to describe the iterative, interdisciplinary process that unfolded in an academic health center setting with a specific focus on underrepresented minority groups of Black and Hispanic communities, and to summarize the research challenges and gaps related to pediatric obesity that were identified in the process. Although the research challenges and gaps were developed in the context of an urban setting including high‐risk populations (the northern Manhattan communities of Washington Heights, Inwood, and Harlem), many of the issues raised are broadly applicable. The processes by which the group identified research gaps and methodological challenges that impede a better understanding of how to prevent and treat obesity in children has resulted in an increase in research and community outreach collaborations and interdisciplinary pursuit of funding opportunities across units within the academic health center and overall university. Clin Trans Sci 2010; Volume 3: 172–177
Keywords: pediatric obesity prevention, interdisciplinary, research priorities
Introduction: Defining the Problem and Goal
The prevalence of obesity among children and adolescents has tripled over the past three decades, and it is projected that childhood obesity may shorten life expectancy by 2–5 years by midcentury in the United States. 1 In 2005–2006, 34% of U.S. children and adolescents between the ages of 2 and 19 were either at risk of overweight (body mass index [BMI]>85th percentile) or overweight (BMI>95th percentile), 2 with a disproportionate increase among minority populations. The disproportionate prevalence among minority populations is prominent in New York City (NYC) where NYC has the 37th highest rate of adult obesity in the nation, compared with other major cities. The rates of childhood overweight and obesity in NYC are about 25% higher than the national levels. 3 The obesity rates among minority populations in the K−8th grades are even higher, with 29% of Hispanic boys and 23% of Hispanic girls classified as obese. These rates are approximately 50% higher than NYC Caucasian, non‐Hispanic boys (20%) and girls (14%) of the same ages. 3
These unabating increases in childhood obesity rates, both nationally and locally, and the discouraging reality that few programs have succeeded in reversing these trends, 4 , 5 motivate researchers to take more multifaceted, multilevel approaches that incorporate both individual or “below the skin” (e.g., biology, physiology, behavior, and genetics) and systemic or “above the skin” (e.g., schools, community, and public policy) strategies. Academic settings offer an opportunity to mobilize multiple research efforts to impact this trend. To foster synergy across disciplines, the Columbia University community of basic and clinical scientists, clinicians, educators, service providers, and public health researchers with a specific interest in pediatric obesity formed an interdisciplinary working group in 2008. 6 This type of interdisciplinary approach has led to successful outcomes in other complex and challenging areas of public health such as tobacco cessation. 7 Although many interdisciplinary efforts involving childhood obesity have been initiated throughout the country, the process of development and formation of these interdisciplinary teams has not been described in detail in the medical or public health literature.
In this paper, we describe the process of forming an interdisciplinary research team, the short‐term outcomes of its efforts, and the long‐term goals set for reducing childhood obesity in our local communities. The process and its outcomes are not meant to imply that “one size fits all,” but rather that within a relatively short time frame our interdisciplinary approach has established research priorities and initiated new projects that incorporate the perspectives and efforts of researchers from multiple disciplines.
Methods: Interdisciplinary Process
The process, initiated with the support of the Clinical and Translational Science Award (CTSA) at Columbia University (NIH RR024156), launched a new collaboration among faculty from dentistry, education, medicine, nursing, nutrition, pediatrics, psychology, public health, and social work. The national CTSA consortium has as its mission the promotion of interdisciplinary research that brings together researchers who might not otherwise interact with the goal of facilitating interdisciplinary collaboration. Beginning in 2007, a campus‐wide survey of obesity experts was conducted to improve our understanding of organizational factors and collaborative patterns that characterize health sciences research in obesity. Social network analysis was used to identify “key players” with this research focus. 8 Combining Google and PubMed searches as well as the snowball sampling method, 9 , 10 a total of 113 obesity experts (defined as those who had published using keywords of obesity and/or fat, or those identified by published colleagues as researchers in this area) were contacted and then surveyed regarding their collaborators, research interests, and affiliations with academic departments and research centers. The primary research questions centered on how to effectively characterize and identify “obesity experts,” to describe existing collaboration patterns among obesity experts and to identify success factors leading to sustained interdisciplinary health science collaborations. From among these obesity experts, those indicating an interest in pediatric or childhood obesity were identified. This effort was combined with a more grassroots initiative to promote collaboration led by several faculty members doing childhood obesity prevention work in the clinical and community settings, and the list was expanded to include others with childhood obesity‐related expertise on campus (for a total of 79 researchers).
The first meeting was convened in June 2008. An e‐mail invitation was sent to all identified researchers with an interest in childhood obesity prevention on the faculties of dentistry, medicine, nursing, public health, education, and social work. The participants included basic and clinical scientists, clinicians, community and public health researchers, educators, and policy researchers. The major goal of this 3‐hour meeting was to provide an opportunity for faculty to introduce their interest areas to the larger group, and to list the major obstacles and frustrations they experience in their work related to childhood obesity, and are listed in Table 1 . The participants agreed that additional meetings were needed to develop specific collaborative projects. Participants also suggested that community be invited to the table once goals and priorities were set. A core planning group of five, which expanded to 10 individuals several months later (December 2008), met biweekly for approximately 4 months (December 2008 to March 2009) to discuss future workshops and other networking opportunities to facilitate the development of interdisciplinary research teams focused on pediatric obesity. This meeting also resulted in the formation of several working groups focusing on the following areas: community engagement, recommendations for treatment of pediatric obesity, and the establishment of a symposium to educate local health practitioners about childhood obesity. A second workshop was convened in April 2009 to allow for further faculty interaction and to work collaboratively to identify gaps in research targeting the prevention and treatment of pediatric obesity. Because of the demographics of our surrounding communities ( Figure 1 ) and the disproportionately high prevalence of obesity in these groups, a special emphasis was placed on those gaps that require an interdisciplinary approach and a focus on two traditionally underrepresented groups (Blacks and Hispanics), many of whom were recent immigrants. During the workshop, attendees were assigned to one of four focus groups, each led by a member of the core working group. Eight master’s and doctoral students in dentistry, nursing, nutrition, and public health, along with several faculty facilitators, were provided with detailed instructions on how to guide the group’s discussions toward research gaps and priority areas; facilitators also took extensive notes during each focus group. The focus groups then reconvened as a single group, notes were summarized into themes or areas of priority and reported back to all workshop participants for confirmation of content. After the workshop, the notes were transcribed, underwent a content analysis, and were thoroughly vetted by workgroup members for completeness and accuracy.
Table 1.
Major obstacles and frustrations experienced by faculty related to their work on childhood obesity.
| A. Isolation/duplication of efforts |
| Lack of coordinated approach to issue |
| Inexperience to form collaborations |
| Lack of time to make fruitful collaborations |
| B. Challenges of community engaged research |
| Lack of institutional support, resources, training for community based participatory research (CBPR) |
| Lack of institutional support and resources for CBPR |
| Labor intensive nature of CBPR is very challenging |
| C. Lack of evidence‐based research/clinical care |
| Lack of known solutions to (childhood obesity) problem |
| No evidence based advice and clinical standards |
| D. Special issues of junior faculty |
| Junior researchers lack collaborators |
| Collaborations can hurt junior faculty on tenure track |
| E. Need for different theoretical approaches to childhood obesity research |
| Family based and transgenerational approaches to obesity are seldom adopted or utilized |
| F. Lack of funding |
| No large based grant funding |
| Lack of resources and funding within institution |
| G. Research participant recruitment |
| How to target large groups of children and adolescents, especially those most vulnerable |
Figure 1.
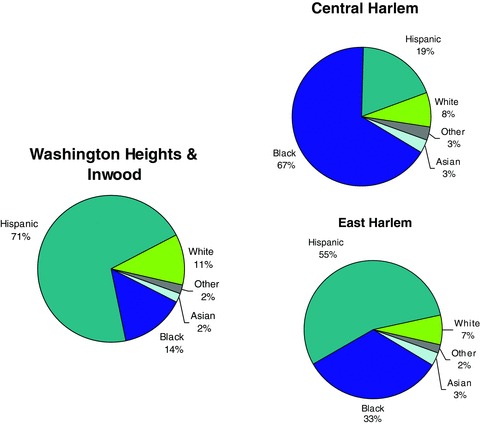
Ethnic/race breakdown of local communities.
The core planning group summarized this content from the workshop into 41 statements of priority, 23 related to interdisciplinary research priorities and 18 related to methodological priorities. The research priorities were organized into four subcategories based on their similarity in focus: epidemiology, behavioral, and social sciences; intervention trials and evaluation; basic biology; and informatics research to assist with childhood obesity prevention. Similarly, the 20 methodological priorities were organized into four categories: communications, networking, and coordination; education; developing or strengthening linkages; and policy. Using a web‐based survey tool (Survey Monkey, http://www.surveymonkey.com), the individuals previously identified as faculty with expertise or interest in pediatric obesity were then asked to rate the importance of each of the priority statements using a five‐point Likert scale (1 = not at all important, 2 = somewhat important, 3 = important, 4 = very important, 5 = extremely important).
Results: Challenges and Gaps Identified
Of the 79 persons invited to complete the survey, 55 responded (70%) to at least one question in the survey, 35 of whom attended the workshop. All were invited to vote on the importance of 41 research topics and strategies in the eight aforementioned general research and methodological domains. Of the 55 respondents, 40 voted on the importance of the 41 items. Among all respondents (those who attended the workshop and those who did not), the top 10 areas selected as most important to pursue (with average scores on the 1 to 5 scale given in parentheses) were
-
1
Integration of behavioral and cultural components into research (4.21).
-
2
Contribution of health disparities on rates of childhood obesity in our communities (4.10).
-
3
Social determinants of health and identification of previously unmeasured factors (4.00).
-
4
Effectiveness of behavioral approaches targeted toward families (3.97).
-
5
Translating current evidence into practice in the clinic and community (3.90).
-
6
Evaluation of approaches to promote sustained physical activity (3.90).
-
7
Developing community advocates and advocacy materials (3.89).
-
8
Developing linkages to other Columbia University schools and academic programs (3.89).
-
9
Developing linkages to governmental agencies such as the Department of Health and the Department of Education (3.86).
-
10
Developing linkages to Washington Heights community organizations and community leaders (3.81).
When the rankings of individuals who attended the workshop and those who did not were evaluated separately, importance scores awarded by attendees tended to be higher than scores awarded by nonattendees. Although the ranking of priority areas also differed somewhat between attendees and nonattendees, it was clear that the integration of behavioral and cultural components into research efforts was viewed as very important by everyone, regardless of attendance. In addition, attendees and nonattendees endorsed research into the contribution of health disparities on rates of childhood obesity in our communities.
Figures 2 and 3 depict the combined percent of respondents who rated each item as extremely important or very important. As noted in Figure 2 , the top ranking research priorities were to examine the contribution of health disparities on rates of childhood obesity and to integrate behavioral and cultural components into research designs. The highest ranking methodological issues ( Figure 3 ) included making linkages within and beyond the institution and translating evidence into practice.
Figure 2.
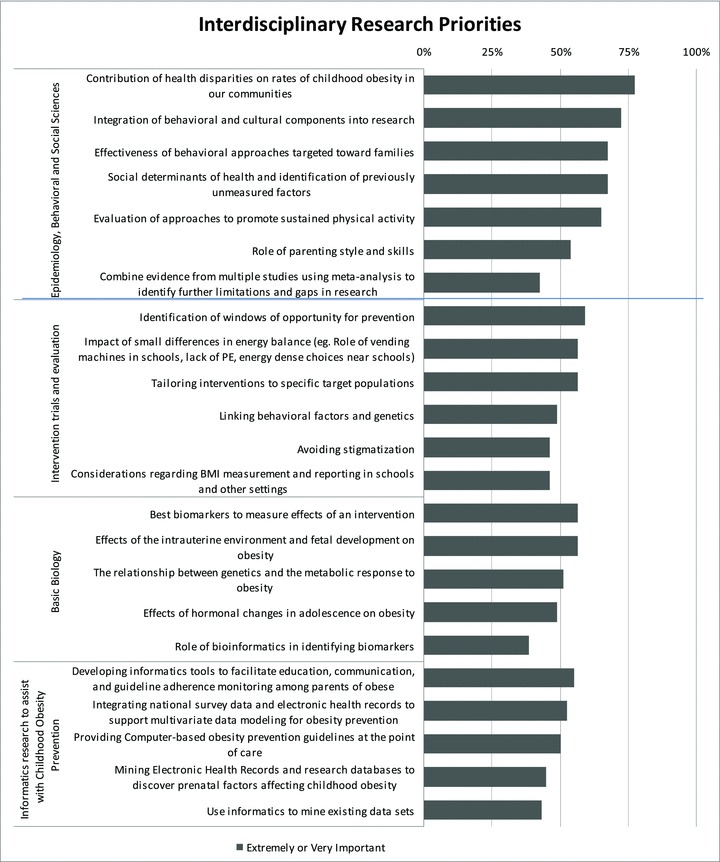
Summary of research priorities identified as very important and extremely important by an interdisciplinary pediatric obesity focus group (N= 40).
Figure 3.
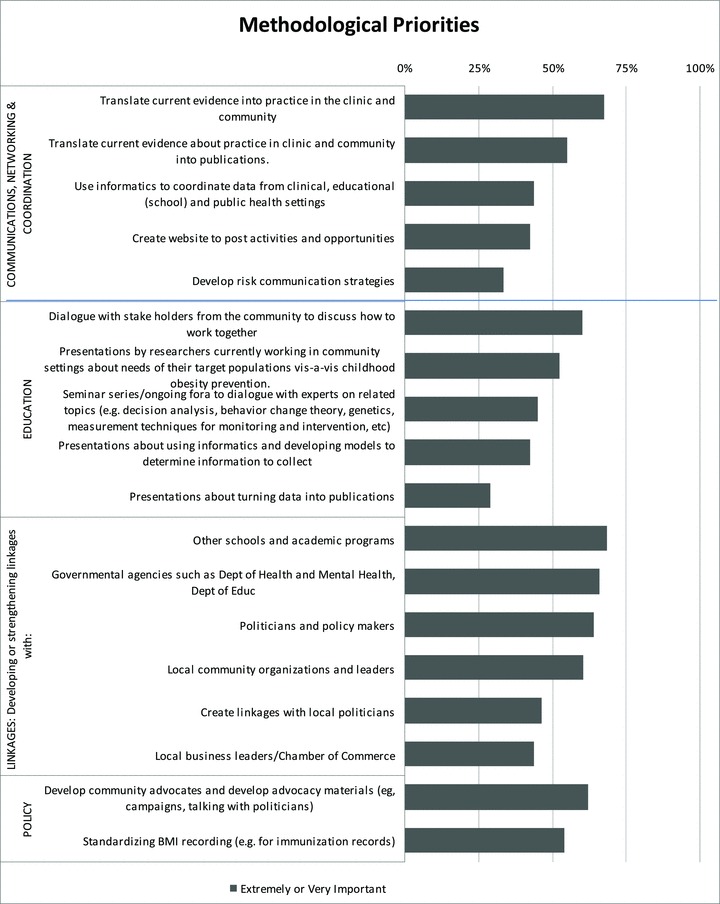
Summary of methodological priorities identified as very important and extremely important by an interdisciplinary pediatric obesity focus group (N= 40).
Discussion
Other academic health centers have active interdisciplinary teams that have worked in varying capacities to tackle the issue of obesity. 11 Despite the considerable effort and resources devoted to this issue, the rate of childhood obesity continues to rise in most parts of the country, and there is currently no standardized or universally agreed upon prevention or treatment approach; most recent guidelines are largely based on consensus or expert opinion. 12 Solutions to seemingly intractable public health problems (e.g., smoking cessation, HIV/AIDS prevention, workplace safety) have required interdisciplinary approaches to gain traction and achieve success, but the nuts and bolts of developing such a process are rarely documented for others to follow. This paper has described such a process and demonstrated that in two relatively brief but broadly inclusive meetings, a forum with a focus on childhood obesity prevention has been created for faculty. The forum allowed faculty to identify potential collaborators, catalog primary obstacles, and increase intrainstitutional, interdepartmental research collaboration. These continuing collaborations, and the second meeting/workshop, led to the identification of research gaps and a group approach to ranking and prioritizing the importance of the identified gaps. The process led to the engagement of faculty and students across multiple disciplines resulting in the development to date of one large, collaborative grant proposal, and many coordinated efforts designed to address some of the obstacles identified at the first meeting.
The next stage will include additional collaborative efforts to secure funding, interdisciplinary curricular activities, the development of clinical practice guidelines throughout the academic health center, and the development of a logic model for the entire initiative. The process occurred in the context of the Columbia University community with a catchment area containing a large proportion of underserved children who are especially vulnerable to the development of obesity and its associated comorbidities. Consistent with our commitment and proximity to racially and ethnically diverse neighborhoods, it is not surprising that the most important research priorities identified related to disparities and cultural and behavioral components.
Sociocultural attitudes toward appearance may play an important role in self‐perception as it relates to body size. 13 , 14 Hence, acquiring an understanding of how sociocultural factors influence eating, physical activity, and degree overweight and/or obese would be important to help better understand the factors that promote or protect against obesity, and to assist in formulating culturally appropriate approaches to promoting healthy lifestyles and body size, especially in cultural groups with a high prevalence of obesity. Since the local neighborhoods of Washington Heights, Central Harlem, and East Harlem differ with regard to their ethnic/racial mix ( Figure 1 ) and cultural identities, self‐perception of body weight may be an important factor to consider in developing interventions to reduce obesity. 15 The gaps identified and the engagement by faculty to address these gaps must be viewed as unique to the demographic composition of the populations under study, as well as the expertise of the faculty involved. To that extent, the outcomes of this process are not necessarily directly relevant to other academic health communities. The process, however, can be studied and adapted by other academic settings to address their unique obstacles and gaps, thereby increasing the likelihood of adopting interdisciplinary approaches to resolve the daunting challenge of childhood obesity.
In summary, to accomplish the goals set for reducing childhood obesity, we propose that a number of approaches could be used within the university setting including (1) the formation of an interdisciplinary research team where each team member brings a unique set of skills/experiences to the group; (2) the workshop(s) described in the manuscript brought faculty from different disciplines together, who otherwise might not have an opportunity to interact or to know what other disciplines are engaged in with regard to pediatric obesity; (3) both of the aforementioned points increase the visibility of the “problem” across the university; (4) continuing dialogue on best approaches to overcome challenges and barriers to work effectively with the community, schools, and appropriate agencies/groups on the problem, including how to coordinate across programs.
“What’s Next?”
The purpose of this paper was not to describe how to overcome barriers but rather how to identify them and develop a plan for next steps. Each discipline or group would have different responses to overcoming the obstacles identified. In terms of productivity resulting from the process described, the following are relevant: (1) a grant application entitled “Increasing Physical Activity in School and Community to Prevent Obesity in Minority Children” (in response to NIH RFA‐HL‐10‐004: Childhood Obesity Prevention and Treatment Research Consortium: UO1) was submitted; (2) interdisciplinary curricular activities including workshops and ongoing targeted seminars are planned through the CTSA to continue to convene faculty with a shared interest in pediatric obesity across departments; (3) the problem of obesity is the focus of several CTSA sponsored projects in the community; (4) the development of clinical practice guidelines throughout the academic health center is planned, and (5) the development of a logic model for the entire initiative is being worked on. We anticipate that some of these efforts will result in curricular innovation and others in future grant submissions.
Conflict of Interest
Each author declared that she or he has no conflict of financial or personal interests in any company or organization sponsoring this study.
Acknowledgments
Supported in part by National Institutes of Health Grants RR 024156, P30‐DK 26687, RO1 HD042187.
References
- 1. Ludwig DS. Childhood obesity—the shape of things to come. N Engl J Med. 2007; 357: 2325–2327. [DOI] [PubMed] [Google Scholar]
- 2. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006; 29: 1549–1555. [DOI] [PubMed] [Google Scholar]
- 3. Egger JR, Bartley KF, Benson L, Bellino D, Kerker B. Childhood obesity is a serious concern in New York City: higher levels of fitness associated with better academic performance. NYC Vital Signs. 2009; 8: 1–4. [Google Scholar]
- 4. Koplan J, Liverman CT, Kraak VI, eds. Preventing Childhood Obesity: health in the Balance. Washington , DC : National Academies Press; 2005. [PubMed] [Google Scholar]
- 5. F as in fat: how obesity policies are failing in America 2009. Available at: http://healthyamericans.org/reports/obesity2009/. Accessed October 19, 2009.
- 6. Aboelela SW, Larson E, Bakken S, Carrasquillo O, Formicola A, Glied SA, Haas J, Gebbie KM. Defining interdisciplinary research: conclusions from a critical review of the literature. Health Serv Res. 2007; 42: 329–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Provan KG, Clark PI, Huerta T. Transdisciplinarity among tobacco harm‐reduction researchers: a network analytic approach. Am J Prev Med. 2008; 35: 173–181. [DOI] [PubMed] [Google Scholar]
- 8. Weng C, Gallagher D, Bales ME, Bakken S, Ginsberg H. Understanding interdisciplinary health sciences collaborations: a campus‐wide survey of obesity experts. AMIA Annu Symp Proc . 2008; 798–802. [PMC free article] [PubMed]
- 9. Goodman LA. Snowball sampling. Ann Math Stat. 1961; 32: 148–70. [Google Scholar]
- 10. Salganik, M , Heckathorn DD. Sampling and estimation in hidden populations using respondent‐driven sampling. Sociol Methodol 2004; 34: 193–239. [Google Scholar]
- 11. Baillargeon JP, Carpentier A, Donovan D, Fortin M, Grant A, Simoneau‐Roy J, St‐Cyr‐Tribble D, Xhignesse M, Langlois MF. Integrated obesity care management system‐implementation and research protocol. BMC Health Serv Res. 2007; 7: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mackey ER, La Greca, AM . Adolescents’ eating, exercise, and weight control behaviors: does peer crowd affiliation play a role J Pediatr Psychol Spec Issue Pediatr Overweight. 2007; 32: 13–23. [DOI] [PubMed] [Google Scholar]
- 13. Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: a meta‐analysis. Psychol Bull. 2006; 132: 622–40. [DOI] [PubMed] [Google Scholar]
- 14. Barlow S; Expert Committee . Expert committee recommendations regarding the prevention, assessment and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007; 120; S164–S192. [DOI] [PubMed] [Google Scholar]
- 15. Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity. 2009; 17: 790–795. [DOI] [PubMed] [Google Scholar]


