Abstract
Managing diabetes can be a daunting task for patients with cancer. Empowerment-based diabetes education and motivational interviewing are complementary approaches. Oncology nurses may feel unprepared to teach patients and their families about self-care for diabetes, but they provide individualized information on symptom management of cancer throughout hospitalization and at discharge. The essential self-care issues include food, exercise, medication, blood glucose monitoring, prevention, recognition and treatment of hypoglycemia and hyperglycemia, and when and how to get additional medical and educational support. This patient-centered model of diabetes education differs from the older “compliance” model that covers many universal rules for all patients, which are predetermined by the nurse. Informing nurses about their role in care of patients with cancer and diabetes is critical.
The incidence of diabetes in the United States continues to rise, with 23.6 million Americans (8% of the population) affected (Centers for Disease Control and Prevention [CDC], 2007). Healthy People 2010 (2000a) has two major goals: increase quality and years of healthy life and eliminate health disparities. The priority focus regarding diabetes is reducing the economic burden and improving quality of life for all people who have or are at risk for diabetes (Healthy People 2010, 2000b). The treatment of diabetes and its accompanying complications are costly, $100 billion annually in the United States and continuing to rise (Garber et al., 2004). Diabetes affects 8%–18% of patients with cancer and can negatively influence the outcomes of treatment (Psarakis, 2006; Singer, 2007). The American Cancer Society ([ACS], 2008) estimates that 1.4 million new cases of cancer will be diagnosed in 2008, and 112,000–252,000 also will have or develop diabetes, making it a significant comorbid condition. Peripheral neuropathies in people with diabetes coupled with chemotherapeutic agents can result in increased toxicities, morbidities, and the potential for treatment discontinuation (Visovsky, Meyer, Roller, & Poppas, 2008).
Many patients with cancer have diabetes, usually type 2 or pre-diabetes, at the time of diagnosis and require dual management of the two conditions (Psarakis, 2006). In addition, several chemotherapeutic regimens such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) and combinations of steroids can lead to hyperglycemia (Oyer, Shah, & Bettenhausen, 2006). Studies have indicated that 38% of all hospitalized patients have documented hyper glycemia, and patients with new hyperglycemia have increased length of hospital stays and higher mortality (Umpierrez et al., 2002). Therefore, healthcare providers often test patients’ hemoglobin A1c (HgA1c), which measures glucose control over the previous two or three months. The test shows whether blood glucose levels are being controlled by the current treatment plan for an existing diabetes. The American Diabetes Association ([ADA], 2007) recommends an HgA1c less than 7%, which reflects an average blood glucose of less than 170 mg/dl. The closer a patient is to that goal, the less he or she is at risk of developing microvascular complications (ADA). The target goal of less than 170 mg/dl may have to be assessed based on clinical presentation of the patient and existing health problems.
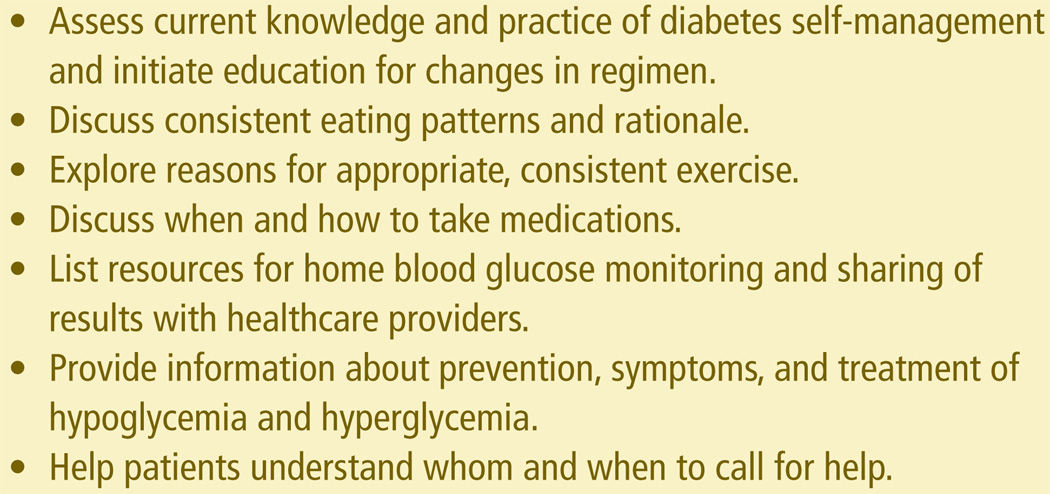
Oncology nurses care for patients with chronic diseases, cancer, and diabetes, and educating and supporting patients with diabetes are critical. Most patients with diabetes self-manage the condition through lifestyle modifications of healthful eating and physical activity, as well as medication adherence and collaborative problem solving using results from home blood glucose monitoring (Weiss & Funnell, 2007). Collaborative patient plans are essential for optimal results (Funnell, Anderson, Austin, & Gillespie, 2007). Hospital-based oncology nurses face ongoing challenges in teaching patients about glycemic control through self-management. Hyperglycemia increases morbidity and mortality in hospitalized patients and increases length of stay by one to three days (Van den Berghe et al., 2001). Alterations in blood glucose levels for inpatients with cancer can impair their ability to interact with caregivers and family members, which can lead to difficulty understanding self-management of diabetes. The ADA delineated inpatient education in its 2004 position statement with specialized educators focusing on diabetes education (Clement et al., 2004; Mensing et al., 2004) (see Figure 1).
Figure 1. Predischarge Instructions.
Note. Based on information from Clement et al., 2004; Joint Commission, 2009; Mensing et al., 2004; Nettles, 2005.
Oncology nurses routinely provide patients and families with information about cancer (e.g., when to call a healthcare provider, signs and symptoms of a fever, ways to manage symptoms), but they also should educate them about prevention, recognition, and treatment of hypoglycemia and hyperglycemia. To provide oncology nurses with a foundation for inpatient diabetes education, this article reviews the pathophysiology of diabetes in patients with cancer and aspects of current diabetes self-management education (DSME): empowerment-based approaches and motivational interviewing.
Pathophysiology
Diabetes is a chronic metabolic disease in which the body does not produce or does not properly use insulin, a hormone required to convert sugar, starches, and other food into energy for the body. The cause of diabetes remains elusive; however, genetics, environment, and lifestyle are major factors in disease development. The two most common categorizations of diabetes are type 1 and type 2. Type 1 is an autoimmune disease in which the pancreatic beta cells are destroyed. Without sufficient beta cell mass, insulin production is either nonexistent or insufficient to sustain life. A person with type 1 diabetes must take insulin regularly to survive. Typically, type 1 diabetes develops in children or young adults, but it can occur at any age. Type 2 diabetes is more common, accounting for 90%–95% of patients with diabetes. In type 2 diabetes, the pancreas continues to produce insulin, but the body becomes resistant to it. Over time, the insulin resistance exceeds the pancreas’s ability to produce sufficient insulin, resulting in rising blood glucose. Factors increasing insulin resistance include obesity, aging, sedentary lifestyle, and steroids. The risk of developing type 2 diabetes also is related to a history of gestational diabetes, family history, and ethnicity (ADA, 2007). As with other acute illnesses, when a diabetic patient also has cancer, normoglycemic control becomes more difficult (Lilley & Levine, 1998). Other adverse consequences of diabetes occur in patients with cancer, including increased neurologic ischemia, a higher infection rate, volume and electrolyte abnormalities, and impaired leukocyte function (Lilley & Levine).
Steroid-Induced Hyperglycemia in Patients With Cancer
Glucocorticoids are a major component of therapy for many cancers, either as part of the treatment regimen or for management of symptoms such as nausea, cord compression, and cerebral edema. For example, CHOP is used in non-Hodgkin and Hodgkin lymphoma. Dexamethasone is used commonly in antiemetic regimens as part of premedication for chemotherapy regimens. The half-life of dexamethasone is more than 48 hours, and the drug can have extended effects on serum glucose levels (Schwab & Porter, 2007). The increase in blood glucose comes from stimulation of hepatic glucose production and inhibition of peripheral glucose uptake, factors that increase insulin resistance. Thus, steroid use can lead to new hyperglycemia or compound the management of existing diabetes.
Oncology nurses have a central role in assessing the needs of patients with diabetes. Understanding that normal blood glucose is 70–100 mg/dl is key. The ADA recommends in the hospital setting targeting less than 110 mg/dl before meals and maximum two-hour postprandial blood glucose less than 180 mg/dl (Clement et al., 2004). If a blood glucose level is low or high, healthcare professionals must treat the patient and assess contributing factors (e.g., nothing by mouth for procedure, use of steroids, choice of foods and liquids). As noted earlier, steroids are a major component of oncology protocols and can increase activity and appetite, as well as affect sleep patterns. Extended use of steroids (for periods longer than two to three weeks) can affect the adrenal gland production of cortisol and possibly lead to adrenal atrophy and insufficiency (Schlaghecke, Kornely, Santen, & Ridderskamp, 1992). Extended use of steroids may lead to a blunted or no response from the hypothalamus-pituitary-adrenal axis. In a stressful event, the adrenal glands usually release epinephrine, cortisol, and growth hormone. Each hormone has a direct effect on glucose metabolism, in some way decreasing pancreatic insulin release and increasing hepatic glucose output. Thus, the patient on chronic steroids (usually longer than two weeks) would not have the usual counter-regulatory hormone response to a low blood glucose. He or she may have a particularly difficult time recovering from a low blood glucose and a sustained (about 24-hour) hyperglycemic response once recovered from the hypoglycemia.
Glucocorticoid administration is associated with increased blood glucose in many patients, and the increase often is proportional to the dose given (Gurwitz et al., 1994; Uzu et al., 2007). In the authors’ experience, prednisone, a commonly used glucocorticoid, often has significant impact on blood glucose control in doses higher than 20 mg given once daily in the morning. Very little information is available in the literature about the timing of prednisone administration and its effects on blood glucose throughout the day. If prednisone is given in the morning, the highest blood glucose level usually is postprandial and occurs between 2 pm and 8 pm. The effects typically clear by the early morning hours, before the next scheduled prednisone dose. This may leave a patient with the potential for hypoglycemia between 2 am and 5 am. Think of the consequences if a patient taking steroids is on sliding-scale insulin. If the patient eats an evening meal and has an elevated blood glucose level at bedtime, an inexperienced provider might order extra units of insulin in addition to the scheduled basal dose. If the blood glucose then drops at 3 am, questions would arise and interventions might be initiated to respond to this “unexpected” drop. This is not uncommon, but it can be prevented if the nurse and provider have an understanding of the action of insulin and the effects of steroids on blood glucose levels.
Patients with type 1 diabetes may be surprised by the increased insulin requirements associated with cancer treatment. Patient teaching about the effects of steroids is critical to ensure that patients are willing to make the necessary changes to their insulin regimens (type 1 patients do not take oral antiglycemic drugs), particularly because patients often feel that they know how to manage their diabetes more effectively than their healthcare providers. Poorly matched prandial or basal insulin can lead to hypoglycemia from excess insulin or hyper glycemia from insufficient insulin. Hyperglycemia then can lead to glycosuria (usually occurring with blood glucose of 180 mg/dl or higher). Once a patient reaches a glycosuric state, excess calories are neither used for metabolism nor stored but are excreted by the kidneys. Throughout cancer treatment, patients should be screened and monitored for hyperglycemia. Insulin regimens should be adjusted throughout treatment to compensate for increased insulin resistance related to steroids, stress, and decreased activity, as well as potentially decreased nutrition.
Nutritional Problems
Over the course of cancer treatment, many patients experience impaired nutritional intake. Indeed, a major side effect of chemotherapy and radiation is loss of appetite. Patients with cancer have unique eating patterns related to decreased appetite and chemotherapy-related nausea and vomiting. When eating is impaired, patients should be encouraged to eat foods and drink liquids that are high in calories. Assisting patients with creating individualized eating plans and administering antiemetics can decrease the risk of dehydration, hypoglycemia, and chemical imbalances. Patients with cancer also are at increased risk for depleted glucose stores, and blood glucose levels may not rise as expected with diabetic ketoacidosis or in response to treatment of a hypoglycemic event.
Diabetes Self-Management Education
In a survey of nurses’ perceptions about providing care to diabetic patients, 84% said that established guidelines in their facilities were extremely helpful in their decision making (McDonald, Tilley, & Havstad, 1999). However, they also indicated a need for more education and diabetes-management updates to improve patient care. Nurses should remain current in their knowledge and nursing practice (Nettles, 2005).
Oncology nurses may not be aware of the role of a diabetes educator or diabetes clinical nurse specialist (CNS) (Davis, 1990), but it involves patient education; development of online, computer-based learning modules; mentoring of staff nurse diabetes champions; updates for medical staff on current practices for glycemic control; and dissemination of diabetes patient education information within the institution through publications and presentations (Davis, 2000; Davis & Tornquist, 1995).
Interdisciplinary communication is critical to ensure open dialogue among nurses, physicians, pharmacists, social workers, case managers, and diabetes CNSs as they provide care. All patients discharged from the hospital should be referred to an outpatient diabetes education program (Davis, Midgett, & Gourley, 1994), so that they can follow up with healthcare providers who will answer questions about diabetes regimens.
For patient education about diabetes to be successful and meaningful, the plan of care must be individualized (Anderson & Funnell, 2000, 2008). Oncology nurses can assist their patients by encouraging them to address their greatest concerns and fears. For example, a nurse might ask, “What is your biggest worry about taking care of your diabetes at home?” (Davis, Vander Meer, Yarborough, & Roth, 1999). Oncology nurses also can assist patients by asking questions and listening supportively (Anderson & Rubin, 2002). Components of diabetes education should be integrated into patient-nurse communication from the time of admission; insulin doses can be added to discharge plans at a later date.
The American Association of Diabetes Educators (2007) listed seven self-care behaviors for patients to help them manage diabetes (Boren, 2007) (see Figure 2). Inpatient oncology nurses can interact with patients and work with them to discuss needed lifestyle changes at home, emphasizing parts of the seven self-care behaviors that are most critical for inpatients to incorporate into their post-hospital lives. A major part of self-care is monitoring blood glucose at home. Nurses should instruct patients to write down their blood glucose levels or use blood glucose meters with memory features and take them to their follow-up appointments. A log book accompanies all blood glucose meters. Such records allow providers to assess trends in blood glucose levels and collaborate with patients to make changes to regimens. If patients report that their healthcare providers do not look at their logs or tell patients, “There is no pattern, but keep on testing,” they will not be motivated to continue self-testing. Providers cannot collaborate with patients to make changes to a diabetes regimen without blood glucose numbers to direct individualized care.
Figure 2. AADE7™ Self-Care Behaviors.
Note. Based on information from American Association of Diabetes Educators, 2007; Boren, 2007.
The rationale for glycemic control during hospitalization is evident because higher blood glucose levels are associated with poorer outcomes, including longer lengths of stay, higher costs of care, and greater mortality (Psarakis, 2006; Singer, 2007). The Diabetes Control and Complications Trial Research Group (1993) confirmed that keeping HgA1c under 7% significantly reduced microvascular complications in people with type 1 diabetes. Also, the United Kingdom Prospective Diabetes Study (UKPDS) Group (1998) demonstrated improved outcomes (e.g., glycemic) and blood glucose control with type 2 diabetes. Both of the studies reinforce the importance of controlling elevated blood glucose levels.
Empowering Patients and Families for Home Care
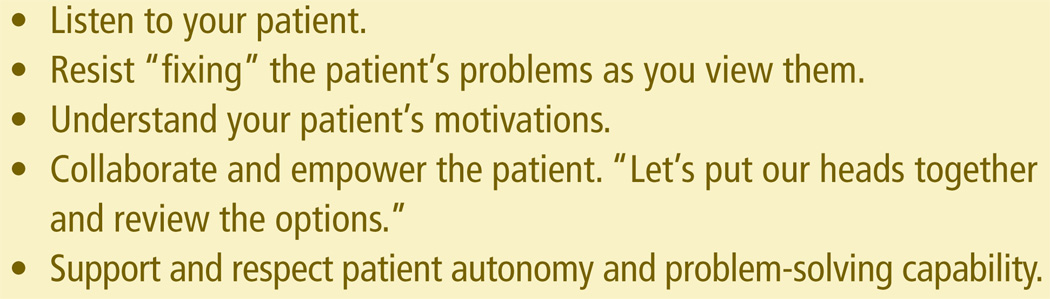
Individualized inpatient diabetes education is essential. About 99% of diabetes care is provided by patients themselves through dietary and physical lifestyle modifications and medication (Funnell & Anderson, 2008; Tuerk, Mueller, & Egede, 2008; Weiss & Funnell, 2007). Oncology nurses can target areas for instructing patients before discharge by asking patients questions (see Figure 3). With empowerment-based diabetes patient education, nurses listen to patients’ concerns and engage them in collaborative problem solving. For example, patients and families may be concerned about the cost of nutritious foods, so nurses can provide information about heart-healthy, portion-controlled, carbohydrate-consistent food choices.
Figure 3. Guiding Principles of Motivational Interviewing.
Note. Based on information from Rollnick et al., 2008; Welch et al., 2006.
Oncology nurses also can help patients understand that they should not drink soda, sweet tea, or fruit juice between meals because such sweetened liquids affect blood glucose levels. Healthful food choices are important in managing people’s diabetes. Patients with cancer may need special nutritional considerations, and nurses can help them make choices to maintain caloric intake and balance insulin dosing. As noted earlier, common side effects of chemotherapy and radiation treatment are loss of appetite, nausea, vomiting, diarrhea, and constipation. Oncology nurses can educate patients and families about the importance of nutrition and correct the misconception that if a patient cannot eat but is hyperglycemic, then he or she still needs insulin. The body must remain nourished during and after treatment. An individualized plan fits a diabetes regimen to a patient and his or her cancer treatment; it does not ft the patient to a universal regimen.
Self-monitoring of blood glucose is the modern way to manage diabetes. Blood glucose meters can be found at all drug stores and through mail-order pharmacies. Private insurance, Medicaid, and Medicare assist with the cost of the meters; however, meter strips are the major cost in diabetes self-care, which may result in decreased monitoring. The number of times a person should test per day varies depending on the clinical condition. Encouraging patients to wash their fingers with warm water and soap instead of alcohol prior to glucose testing will reduce irritation and drying of the skin.
Early recognition of hypoglycemia is critical for early intervention. Oncology nurses can teach patients and families about the value of 15 g of carbohydrates found in three glucose tablets, which can be found in grocery stores and pharmacies. Patients and family members can carry the tablets when they are away from home. Patients may be tempted to stop taking insulin after one low blood glucose episode, but they should be encouraged to keep a record of their blood glucose numbers and note any trends.
Motivational Interviewing
The goal of motivational interviewing (MI) is to increase patients’ internal motivation to change their behavior (Rollnick, Miller, & Butler, 2008). MI is a patient-centered approach that encourages discussion of targeted behavior changes. People learn to change behaviors when doing so seems personally important and achievable and has measurable benefits (Welch, Rose, & Ernst, 2006; West, DiLillo, Bursac, Gore, & Green, 2007). MI has been used to reduce psychiatric disorders, addictive behaviors, and risk of sexually transmitted infections.
Nurses can ask patients questions in a nonthreatening way.
Do you mind if I ask you a few questions related to your diabetes?
With your permission, I would like to propose a plan related to your diabetes.
If you are willing, may I share some information with you?
The DCCT (1993) and UKPDS (1998) found that education by nurses and dietitians promoted glycemic control, and outcomes were achieved through individualized coaching. The two least productive statements used by providers are “watch what you eat” and “get more exercise.” The statements are not helpful and do not involve patients in decision making. Motivational messages that remain positive are more effective and result in better-controlled blood glucose (Anderson & Rubin, 2002; Davis et al., 1999).
Can you think of ways you might work daily exercise into your schedule, like you did so well yesterday?
You told me about the change you made in your bedtime snack. How did you know that eating peanut butter and crackers would help your morning blood sugar so much?
I think you’re onto something about not going grocery shopping when you’re hungry, or on the way home from work.
Great job of keeping records of your blood sugars and remembering to bring them to this appointment.
A potential challenge faced by nurses is lack of time, which does not allow full assessment of a patient’s story. However, it takes less than five minutes for patients to share a concern about a targeted behavior (Levinson, Gorawara-Bhat, & Lamb, 2000; Welch et al., 2006). Also, oncology nurses can educate patients and families throughout hospitalization and not wait until the day of discharge.
Another challenge is delivering clear, concise, and relevant information to answer a patient’s questions and needs. Other challenges to inpatient diabetes education using the MI approach include low literacy and lack of understanding of diabetes management. Nurses must be cognizant that some patients have low literacy or are illiterate but may not be willing to share that information (Cotugna, Vickery, & Carpenter-Haefele, 2005). Supportive coaching, which does require some re-education by healthcare providers, can take less time with patients than older methods of lecturing.
Together, the empowerment-based model and MI have demonstrated improvements in patient glycemic control (Funnell & Anderson, 2008; West et al., 2007). The techniques differ from older models in which nurses taught patients universal rules that often were difficult or impossible to follow. The collaborative MI approach helps patients to communicate their concerns about their behaviors. With the approach, oncology nurses can assist patients to feel empowered and in control of their diabetes (Welch et al., 2006). When oncology nurses have up-to-date knowledge of diabetes self-care, they are able to help patients with cancer self-manage their diabetes.
Individualized self-care plans with an emphasis on patient involvement can help patients with cancer cope better with their diabetes after hospitalization. The unique eating habits and insulin requirements of patients with cancer remain a challenge, but the issues can be managed properly. When empowerment-based education is integrated at all levels of the disease process, oncology nurses can be major influences in guiding, educating, and empowering patients in self-management of their diabetes.
At a Glance
Empowerment-based education and motivational interviewing are complementary approaches to diabetes patient education that have affected glycemic control.
Knowledge about cancer and diabetes is essential in the delivery of individualized plans of care.
Oncology nurses provide patients and families with skills and resources necessary to manage their cancer symptoms and to perform self-care of diabetes.
Acknowledgments
The authors gratefully acknowledge Joey Misuraca, RN, BSN, OCN®, nurse manager for hematology/oncology services at Duke University Medical Center, and Elizabeth Tornquist, MA, FAAN, editorial consultant in the School of Nursing at the University of North Carolina at Chapel Hill, for their review and editorial assistance.
References
- American Association of Diabetes Educators. 2007 AADE7™ self–care behaviors. 2007. Retrieved July 1, 2008, from http://www.diabeteseducator.org/ProfessionalResources/AADE7/
- American Cancer Society. Cancer facts and fgures 2008. 2008. Retrieved May 27, 2008, http://www.cancer.org/downloads/STT/2008CAFFfnalsecured.pdf".
- American Diabetes Association. Standards of medical care in diabetes—2007. Diabetes Care. 2007;30(Suppl. 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- Anderson B, Funnell MM. The art of empowerment: Stories and strategies for diabetes educators. Alexandria, VA: American Diabetes Association; 2000. [Google Scholar]
- Anderson B, Rubin R. Practical psychology for diabetes clinicians. 2nd ed. Alexandria, VA: American Diabetes Association; 2002. [Google Scholar]
- Anderson RM, Funnell MM. The art and science of diabetes education: A culture out of balance. Diabetes Educator. 2008;34(1):109–117. doi: 10.1177/0145721707312398. [DOI] [PubMed] [Google Scholar]
- Boren S. AADE7™ self-care behaviors: Systematic reviews. Diabetes Educator. 2007;33(6):866–871. doi: 10.1177/0145721707309662. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National diabetes fact sheet, 2007. 2007 Retrieved July 2, 2008, from http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schaefer RG, et al. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27(2):553–591. doi: 10.2337/diacare.27.2.553. [DOI] [PubMed] [Google Scholar]
- Cotugna N, Vickery CE, Carpenter-Haefele KM. Evaluation of literacy level of patient education pages in health-related journals. Journal of Community Health. 2005;30(3):213–219. doi: 10.1007/s10900-004-1959-x. [DOI] [PubMed] [Google Scholar]
- Davis ED. Role of the diabetes nurse educator in improving patient education. Diabetes Educator. 1990;16(1):36–38. doi: 10.1177/014572179001600109. [DOI] [PubMed] [Google Scholar]
- Davis ED. A quality improvement project in diabetes patient education during hospitalization. Diabetes Spectrum. 2000;13(4):228–231. [Google Scholar]
- Davis ED, Midgett L, Gourley CS. Teach less, teach better at every opportunity. Diabetes Educator. 1994;20(3):236–238. doi: 10.1177/014572179402000310. [DOI] [PubMed] [Google Scholar]
- Davis ED, Tornquist EM. Writing partnerships: A CNS and staff nurses write for publication. Clinical Nurse Specialist. 1995;9(4):215–220. [PubMed] [Google Scholar]
- Davis ED, Vander Meer JM, Yarborough PC, Roth SB. Using solution-focused therapy strategies in empowerment-based education. Diabetes Educator. 1999;25(2):249–252. 255–257. doi: 10.1177/014572179902500210. [DOI] [PubMed] [Google Scholar]
- Diabetes Control and Complications Trial Research Group. The effect of intensive diabetes treatment on the development and progression of long-term complications in insulin-dependent diabetes mellitus: The Diabetes Control and Complication Trial. New England Journal of Medicine. 1993;329(14):978–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- Funnell M, Anderson R. Influencing self-management: From compliance to collaboration. In: Feinglos MN, Bethel MA, editors. Type 2 diabetes mellitus: An evidence-based approach to practical management. Totowa, NJ: Humana Press; 2008. pp. 455–466. [Google Scholar]
- Funnell M, Anderson R, Austin A, Gillespie S. AADE position statement: Individualization of diabetes self-management education. Diabetes Educator. 2007;33(1):45–49. doi: 10.1177/0145721706298308. [DOI] [PubMed] [Google Scholar]
- Garber AJ, Moghissi ES, Bransome ED, Jr, Clark NG, Clement S, Cobin RH, et al. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocrine Practice. 2004;10(1):77–82. doi: 10.4158/EP.10.1.77. [DOI] [PubMed] [Google Scholar]
- Gurwitz JH, Bohn RL, Glynn RJ, Monane M, Mogun M, Avorn J. Glucocorticoids and the risk of initiation of hypoglycemic therapy. Archives of Internal Medicine. 1994;154(1):97–101. [PubMed] [Google Scholar]
- Healthy People 2010. Diabetes. 2000a doi: 10.2337/diacare.23.6.853. Retrieved June 1, 2008, from http://www.healthypeople.gov/document/HTML/Volume1/05Diabetes.htm. [DOI] [PubMed]
- Healthy People 2010. What are its goals? 2000b Retrieved June 1, 2008, from http://www.healthypeople.gov/About/goals.htm.
- Joint Commission. Inpatient diabetes certification. 2009. Retrieved February 12, 2009, from http://www.jointcommission.org/CertificationPrograms/Inpatient+Diabetes/
- Levinson W, Gorawara-Bhat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021–1027. doi: 10.1001/jama.284.8.1021. [DOI] [PubMed] [Google Scholar]
- Lilley SH, Levine GI. Management of hospitalized patients with type 2 diabetes mellitus. American Family Physician. 1998;57(5):1079–1088. [PubMed] [Google Scholar]
- McDonald PE, Tilley BC, Havstad SL. Nurses’ perceptions: Issues that arise in caring for patients with diabetes. Journal of Advanced Nursing. 1999;30(2):425–430. doi: 10.1046/j.1365-2648.1999.01096.x. [DOI] [PubMed] [Google Scholar]
- Mensing C, Boucher J, Cypress M, Weinger K, Mulcachy K, Barta P, et al. National standards for diabetes self-management education. Diabetes Care. 2004;27(Suppl. 1):S143–S150. doi: 10.2337/diacare.27.2007.s143. [DOI] [PubMed] [Google Scholar]
- Nettles AT. Patient education in the hospital. Diabetes Spectrum. 2005;18(1):44–48. [Google Scholar]
- Oyer D, Shah A, Bettenhausen S. How to manage steroid diabetes in the patient with cancer. Journal of Supportive Oncology. 2006;4(9):479–483. [PubMed] [Google Scholar]
- Psarakis HM. Clinical challenges in caring for patients with diabetes and cancer. Diabetes Spectrum. 2006;19(3):157–162. [Google Scholar]
- Rollnick S, Miller WR, Butler CC. Motivational interviewing in health care: Helping patients change behavior. New York: Guilford Press; 2008. [Google Scholar]
- Schlaghecke R, Kornely E, Santen RT, Ridderskamp P. The effect of long-term glucocorticoid therapy on pituitary-adrenal responses to exogenous corticotropin-releasing hormone. New England Journal of Medicine. 1992;326(4):226–230. doi: 10.1056/NEJM199201233260403. [DOI] [PubMed] [Google Scholar]
- Schwab N, Porter M. Inpatient diabetes mellitus in the oncology setting. Clinical Journal of Oncology Nursing. 2007;11(4):489–492. doi: 10.1188/07.CJON.489-492. [DOI] [PubMed] [Google Scholar]
- Singer M. Management of comorbid diabetes and cancer. Oncology. 2007;21(8, Suppl.):26–39. [PubMed] [Google Scholar]
- Tuerk P, Mueller M, Egede L. Estimating physician effects on glycemic control in the treatment of diabetes: Methods, effects sizes, and implications for treatment policy. Diabetes Care. 2008;31(5):869–873. doi: 10.2337/dc07-1662. [DOI] [PubMed] [Google Scholar]
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: An independent marker of in-hospital mortality in patients with undiagnosed diabetes. Journal of Clinical Endocrinology and Metabolism. 2002;87(3):978–982. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- United Kingdom Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes. Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- Uzu T, Harada T, Sakaguchi M, Kanasaki M, Isshiki K, Araki S, et al. Glucocorticoid-induced diabetes mellitus: Prevalence and risk factors in primary renal disease. Nephron Clinical Practice. 2007;105(2):c54–c57. doi: 10.1159/000097598. [DOI] [PubMed] [Google Scholar]
- Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, et al. Intensive insulin therapy in critically ill patients. New England Journal of Medicine. 2001;345(19):1359–1367. doi: 10.1056/NEJMoa011300. [DOI] [PubMed] [Google Scholar]
- Visovsky C, Meyer R, Roller J, Poppas M. Evaluation and management of peripheral neuropathy in diabetic patients with cancer. Clinical Journal of Oncology Nursing. 2008;12(2):243–247. doi: 10.1188/08.CJON.243-247. [DOI] [PubMed] [Google Scholar]
- Weiss MA, Funnell MM. The little diabetes book you need to read. Philadelphia: Running Press; 2007. [Google Scholar]
- Welch G, Rose G, Ernst D. Motivational interviewing and diabetes: What is it, how is it used, and does it work? Diabetes Spectrum. 2006;19(1):5–11. [Google Scholar]
- West SD, DiLillo V, Bursac Z, Gore SA, Green PG. Motivational interviewing improves weight loss in women with type 2 diabetes. Diabetes Care. 2007;30(5):1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]