Abstract
Background
Referral to psychological therapies is recommended for people with common mental health problems (CMHP) however its impact on healthcare utilisation in people with long term conditions (LTCs) is not known.
Method
Routinely collected primary care, psychological therapy clinic and hospital data were extracted for the registered population of 20 practices (N = 121199). These data were linked using the SAPREL (Secure and Private Record Linkage) method. We linked the 1118 people referred to psychological therapies with 6711 controls, matched for age, gender and practice. We compared utilisation of healthcare resources by people with LTCs, 6 months before and after referral, and conducted a controlled before and after study to compare health utilisation with controls. We made the assumption that collection of a greater number of repeat prescriptions for antidepressants was associated with greater adherence.
Results
Overall 21.8% of people with an LTC had CMHP vs. 18.8% without (p < 0.001). People with LTCs before referral were more likely to use health care resources (2-tailed t-test p < 0.001). Cases with LTCs showed referral to the psychological therapies clinic was associated with increased antidepressant medication prescribing (mean differences 0.62, p < 0.001) and less use of emergency department than controls (mean difference −0.21, p = 0.003).
Conclusions
Referral to improved access to psychological therapies (IAPT) services appears of value to people with LTC. It is associated with the issue of a greater number of prescriptions for anti-depressant medicines and less use of emergency services. Further studies are needed to explore bed occupancy and outpatient attendance.
Keywords: Long term conditions/Chronic disease; Common mental health problems; Psychological therapies; Health service utilisation; Antidepressive agents; Medical record systems, computerized
Highlights
-
•
People with long term conditions (LTC) have more common mental health problems.
-
•
People with LTC make more use of health services including accident and emergency.
-
•
Improving access to psychological (IAPT) services reduces health consumption.
-
•
People with LTC referred to IAPT make fewer emergency department attendances.
-
•
People with LTC referred to IAPT may adhere better to antidepressant therapy.
Introduction
Long term conditions (LTCs) are common and an increasing proportion of the burden of disease (Lopez, Mathers, Ezzati, Jamison, Murray, 2006; Mathers, Boerma, & Ma Fat, 2009). People with LTCs have a higher prevalence of common mental health problems (CMHP), principally depression and anxiety (Patten, 2001; Patten et al., 2008; Shen, Sambamoorthi, & Rust, 2008). People with chronic physical conditions and mental illness are more likely to use emergency services and have higher total, outpatient, and pharmaceutical expenditures than those without mental illness (Shen et al., 2008).
A variety of case-management models are proposed for people with long term conditions (Drennan & Goodman, 2004); and managing both mental and physical health is important (Harkness et al., 2010; Lempp et al., 2009). The principles of care described within the “Chronic care model” (Bodenheimer, Wagner, & Grumbach, 2002a) appear to be associated with improved clinical outcomes in both physical and mental health (Bodenheimer, Wagner, & Grumbach, 2002b; Tsai, Morton, Mangione, & Keeler, 2005). In the UK the number of people with LTCs is increasing and these people make greater use of the health service (Wilson, Buck, & Ham, 2005). Recent policy developments propose the greater use of mental health services in the long term care of people with LTCs (Lau, 2005). However, the focus at health service level has been on improved case management by experienced nurses (“community matrons”) and the use of risk scores to attempt to identify those at highest risk of readmission (Hall, Kulendran, Sadek, Green, & de Lusignan, 2011).
Improving Access to Psychological Therapies (IAPT), principally the provision of brief interventions and access to cognitive behavioural therapy, has been provided by the NHS in England (Clark et al., 2009); and we have shown that referral to these services is associated with a reduction in health care utilisation; people referred to IAPT are issued fewer sick certificates, have fewer admissions to hospital, bed-days, and emergency department attendances (de Lusignan, Chan, Parry, Dent-Brown, & Kendrick, 2011).
We carried out this study to explore whether referral of people with LTCs to a psychological therapies service was associated with a change in health service utilisation or adherence to antidepressant therapy. The principal comparison in the paper is a controlled before and after comparison of those with LTCs exposed to IAPT compared with those with LTCs who are not.
Method
Overview
We carried out anonymous linkage of general practice, hospital and psychological therapy service data. We report the prevalence of LTCs; and the proportion of people with CMHP who have an LTC.
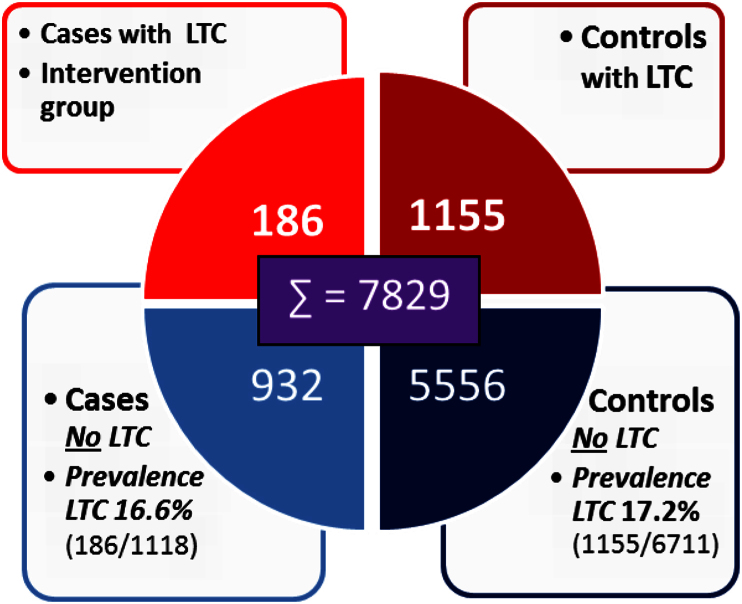
Our cases are people exposed to IAPT (n = 1118) of whom 118 had an LTC and 932 did not; our controls were age, gender, practice matched with an approximate ratio of 6:1. Of the controls (n = 6711) 1155 had an LTC and 5556 did not (Fig. 1). The controls were identified from the total number of people with LTCs (n = 23,1310) or from the wider practice population without LTCs (n = 98,068).
Fig. 1.
Cases and controls, with and without long term conditions (LTC). Cases have been exposed to psychological therapies (IAPT).
We report the utilisation of health care resources by those with and without LTCs; and healthcare consumption before and after referral to IAPT. Finally, we make a controlled before and after comparison of the people with LTC and CMP (n = 118) and the controls with LTCs (n = 1115).
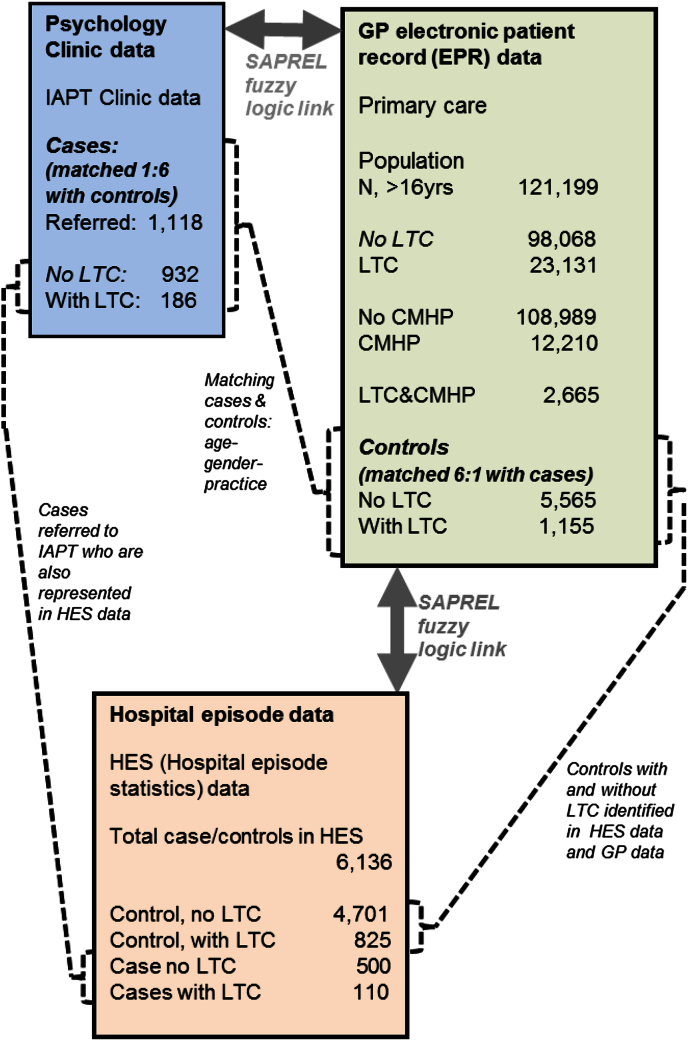
Sample
The study used linked primary care, psychological therapy and hospital datasets linked using our Secure and Private Record Linkage (SAPREL) method (de Lusignan, Navarro, et al., 2011). This novel method uses fuzzy-logic to link records without the researcher knowing the identity of the linked cases. Routinely collected primary care, psychological therapy clinic and hospital data were extracted for the registered population of 20 practices situated in two sites – one in East London, the other in a northern city (N = 121,199 registered patients) as part of a National Institute for Health Research evaluation of IAPT demonstration sites (Parry et al., 2011). We collected the following data from practices: basic demographic, mental health problems, sick-certificate issue, anti-depressant prescription and LTC data (Fig. 2). We extracted coded data for the study variables along with the related date, and where relevant the value field. The primary care data we extracted were coded using the Read Code system (de Lusignan, 2005); and extracted, aggregated and processed using our standard methods (Michalakidis et al., 2010).
Fig. 2.
People referred to psychology clinic (n = 1118), Population recorded on GP electronic patient record (EPR) system (N = 121,199), and control group (n = 6720), and number of cases and controls with Hospital episode data (n-6136).
Linked data collection
The three sources of data were recorded differently: Primary care data were generally recorded by the general practitioners at the point of care; the IAPT data were a Department of Health defined minimum dataset completed by administrative staff or therapists; and Hospital Episode Statistics (HES) data were entered by medical record data entry staff after the episode was completed based on their interpretation of written clinicians' notes. HES data comprises data about: in-patient (IP) data both number of episodes and length of stay – commonly described as occupied bed day (OBD), out-patient (OP) and accident and emergency (A&E) attendances.
People with long term conditions (LTC)
This analysis focuses on the impact of IAPT on people with long term conditions (LTC). This study collected information on the following long-term conditions: Diabetes mellitus, Chronic Kidney Diseases (CKD), Heart failure, Ischaemic Heart Diseases, Hypertensive disease and Chronic Obstructive Pulmonary Diseases (COPD). A derived variable called “LTC” was defined as a diagnosis of at least one of these conditions. We compared the disease prevalence recorded with that reported in the Pay for Performance (P4P) quality indicators for the areas from where the sample was selected (NHS Information Centre, Quality and Outcomes Framework).
Cases and controls
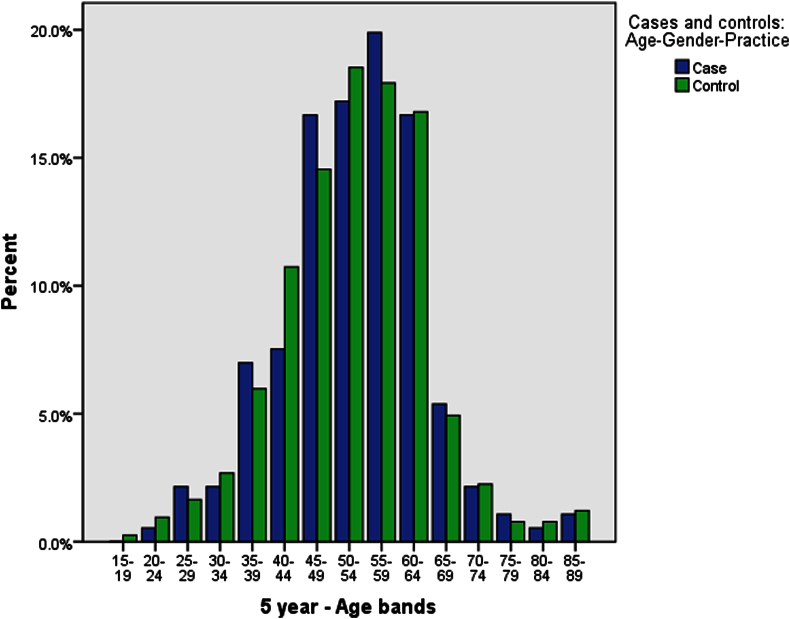
We defined our cases as the population referred to IAPT services (n = 1118, of whom 186 had LTCs) and the controls were people with LTC from within the group of people not referred to IAPT (n = 6711, of whom 1155 had LTCs). We used a computerised statistical programme to match controls to cases, following a standard process (Mounib & Satchi, 2000). We listed the variables we wished to match on: age, gender and practice. Our goal was to get the best possible match with between four and eight controls per case. The steps of this process are as follows. Firstly, our cases (people referred to psychological therapies) are identified and we set the desired ratio and age matching range. We used 10-year age bands, and initially a ratio of eight cases to controls. We then run this and end up with a subset of matching people. We then sequentially add other variables seeing if we can achieve the maximum number of age-gender-practice matched controls. Six was the optimum selection, maximising the number of matches with the boundaries set; the nearness of the age-band match is shown in Fig. 3.
Fig. 3.
Distribution by age of LTC in the intervention and control groups.
Outcome variables and comparisons made
We first explored the utilisation of health care resources by people with LTCs in the total practice population (N = 121,199). We then compared healthcare utilisation in the 6 months before and after referral to IAPT services, as well as the mean difference between the intervention group (people with LTCs referred to IATP, n = 186) and controls (n = 1155) in the 6 months before and after (Figs. 1 and 2). Analysis of the outcomes of the IAPT intervention was based on “intention to treat,” that is, all those referred to IAPT whether or not they engaged with the service or completed their course of therapy (CONSORT 2010; Hollis & Campbell, 1999).
Prescription issue as a proxy for adherence
We used issue of prescriptions as a marker of adherence with antidepressant therapy. We counted the number of prescriptions issued in the last year, as a proxy measure of adherence. We accept that a proportion of people won't fill their prescription, though this has been estimated as <5%. A much bigger problem with antidepressant consumption is that nearly a quarter of people only collect a single script and do not then attend for further follow-up (van Geffen et al., 2009); we would expect that interventions that engaged people in their therapy might be associated with a higher mean number of antidepressant scripts.
Statistical methods
We analysed the data in SPSS (PASW/IBM Statistics) version 18. We used descriptive data to compare the samples as well as inferential statistical procedures to compare differences in the outcomes. We used Pearson Chi-square to compare proportions, and we report odds ratios (OR) and 95% confidence intervals to report any association between the presence and absence of binary conditions (e.g. having an LTC and a CMHP). We used an independent samples t-test to compare differences in health care consumption.
We identified the 6711 controls from the practice population. We identified approximately 6 controls for each case. The date of the first therapeutic session was used to define the cut off between “before” and “after”. If the date was missing we used the date of the initial assessment. We report the mean differences between groups to describe differences in the utilisation of health care services by the four groups:
-
(1)
The intervention group: Cases, people referred to IAPT (with CMHP) who have LTCs;
-
(2)
Cases, people referred to IAPT (with CMHP) without LTCs;
-
(3)
Controls, people with CMHP and LTCs; and
-
(4)
People with CMHP but without LTCs. We compared mean levels of health care utilisation between these groups (Fig. 1) before and after the intervention.
Ethical considerations
An NHS national research ethics committee (reference No: 08/H0715/101) provided ethical review, and the research office of the local health care organisations involved provided local site approvals. In addition, specific approval was obtained from the Patient Information Advisory Group (PIAG) (now the National Information Governance Board and Section 158 exemption). The SAPREL process complied with the approved use and protection of patient information and was commended by PIAG as an example of best practice (de Lusignan, Chan, et al., 2011).
Results
Population
he prevalence of LTC in the total practice population was 15.2% (23200/152302) and 18.8% (n = 23131/121,199) among people 16 years and over. The LTC cases comprised the following proportions of the practice population: Diabetes 5.7%; chronic kidney disease 4.6%; heart failure 0.8%; Hypertensive disease 14.5%; Chronic Obstructive Pulmonary Disease (COPD) 0.7%. These conditions were not mutually exclusive and co-morbidity was common. The prevalence of LTCs was similar but higher than that reported for P4P targets for the relevant NHS localities, Table 1 (NHS Information Centre, Prevalence data tables).
Table 1.
Prevalence of long term conditions identified in the study compared with best matching prevalence from P4P indicators.
| Prevalence |
||
|---|---|---|
| GP data | P4P data | |
| Diabetes | 5.7% | 5.0% |
| CKD | 4.6% | 2.9% |
| Heart failure | 0.8% | 0.4% |
| IHD/CHD | 3.8% | 3.2% |
| Hypertension | 14.5% | 12.4% |
| COPD | 0.7% | 1.6% |
In the adult population (>16 years, N = 121199) we found an association between CMPH and LTC, the OR of an association of was 1.21 (95% CI 1.15–1.26; p < 0.001, Table 2). Each of the LTCs were associated with CMHP, (chi-square p < 0.001), except heart failure where the proportion with CMHP was not significantly different and the 95% confidence intervals for the OR crossed parity (OR 1.09, 95% CI 1.07–1.27; Chi-square p = 0.43 n.s.). CMHP were almost twice as common in people with COPD; with one of the strongest associations (OR 1.75, 95% CI 1.46–2.11).
Table 2.
Recorded prevalence of long-term conditions, for population age 16 and over.
| Common mental health problem (CMHP) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Present |
Absent |
All |
Odds ratio (OR) |
Chi-square |
||||
| n | % | n | % | n | (95% CI) | p | ||
| Population | >16 yr | 12210 | 10.1% | 108,989 | 89.9% | 121,199 | ||
| Any LTC | Y | 2665 | 21.8% | 20,466 | 18.8% | 23,131 | 1.21 | p < 0.001 |
| N | 9545 | 78.2% | 88,523 | 81.2% | 98,068 | (1.15–1.26) | ||
| Diabetes | Y | 775 | 6.3% | 6081 | 5.6% | 6856 | 1.15 | p < 0.001 |
| N | 11435 | 93.7% | 102,908 | 94.4% | 114,343 | (1.01–1.24) | ||
| CKD | Y | 644 | 5.3% | 4974 | 4.6% | 5618 | 1.16 | p < 0.001 |
| N | 11566 | 94.7% | 104,015 | 95.4% | 115,581 | (1.07–1.27) | ||
| CHF | Y | 105 | 0.9% | 860 | 0.8% | 965 | 1.09 | p = 0.403 |
| N | 12105 | 99.1% | 108,129 | 99.2% | 120,234 | (0,89–1.34) | ||
| IHD | Y | 574 | 4.7% | 4012 | 3.7% | 4586 | 1.29 | p < 0.001 |
| N | 11636 | 95.3% | 104,977 | 96.3% | 116,613 | (1.18–1.41) | ||
| HT | Y | 1901 | 15.6% | 15,631 | 14.3% | 17,532 | 1.10 | p < 0.001 |
| N | 10309 | 84.4% | 93,358 | 85.7% | 103,667 | (1.05–1.56) | ||
| COPD | Y | 133 | 1.1% | 680 | 0.6% | 813 | 1.75 | p < 0.001 |
| N | 12077 | 98.9% | 108,309 | 99.4% | 120,386 | (1.46–2.11) | ||
Key: LTC = Long term conditions, CKD = Chronic kidney disease, CHF = Chronic Heart Failure, IHD = Ischaemic Heart Disease, HT = Hypertension, COPD = Chronic Obstructive Pulmonary Disease 95%, CI = 95% Confidence Intervals. Bold represents total population.
Utilisation of health resources by people with LTCs compared with those without
Unsurprisingly, people with LTC were more likely to have higher health consumption that those without (Table 3). They received just over three times as many antidepressant prescriptions in the previous year, and had nearly three times as many sick notes. They also had nearly three times as many hospital admissions, and their total number of occupied bed days was roughly six times that of people without LTCs, suggesting a mean length of admission twice that of those without LTCs. People with LTCs had nearly 2.5 times as many outpatient attendances and 1.5 times as many visits to A&E.
Table 3.
Utilisation of healthcare resources of people with long term conditions (LTC). A negative mean difference implies that something is more common in people with LTC.
| Type of health consumption/Sick certification | LTC | n | Mean | Mean difference | SE difference | 95% CI of difference | t-test sig. (2 tailed) |
|---|---|---|---|---|---|---|---|
| Psychotropic Medication (Prescribed <1 year) |
Y | 23,131 | 2.7 | −1.84 | 0.04 | −1.92 to −1.76 | p < 0.001 |
| N | 98,068 | 0.87 | |||||
| Sick notes issued (<1 year) | Y | 23,131 | 2.17 | −1.39 | 0.03 | −1.45 to −1.32 | p < 0.001 |
| N | 98,068 | 0.78 | |||||
| Inpatient admissions | Y | 23,131 | 0.8 | −0.52 | 0.02 | −0.55 to −0.49 | p < 0.001 |
| N | 98,068 | 0.28 | |||||
| Total days admitted (OBD) | Y | 23,131 | 3.58 | −2.99 | 0.14 | −3.26 to −2.72 | p < 0.001 |
| N | 98,068 | 0.59 | |||||
| Outpatient attendances | Y | 23,131 | 3.9 | −2.43 | 0.05 | −2.52 to −2.33 | p < 0.001 |
| N | 98,068 | 1.47 | |||||
| A&E attendances | Y | 23,131 | 0.48 | −0.17 | 0.01 | −0.19 to −0.15 | p < 0.001 |
| N | 98,068 | 0.3 |
Changes before and after referral
People with LTC referred to IAPT were more likely to be prescribed antidepressant medications after referral (p < 0.001), and less likely to attend A&E (p = 0.009; Table 4). Other differences between the groups before and after referral to IAPT were not significantly different.
Table 4.
Utilisation of healthcare resources by people with LTC and CMHP 6 months before and after referral to IAPT. A negative mean difference implies greater consumption in a group, a positive mean difference a lower consumption.
| Group |
Mean differences |
Significance |
|||||
|---|---|---|---|---|---|---|---|
| Name | n | SD | SE | 95% CI | p | ||
| Numbers of Anti-depressant Px – prescribed in previous year | Case with LTC | 186 | −0.94 | 2.51 | 0.18 | −1.3 to −0.58 | p < 0.001** |
| Case without LTC | 932 | −0.27 | 2.03 | 0.07 | −0.4 to −0.14 | ||
| Control with LTC | 1155 | −0.32 | 1.43 | 0.04 | −0.4 to −0.24 | ||
| Control without LTC | 5556 | −0.11 | 1.03 | 0.01 | −0.14 to −0.09 | ||
| Total | 7829 | −0.18 | 1.31 | 0.01 | −0.21 to −0.15 | ||
| Number of recent sick notes issued | Case with LTC | 186 | 0.01 | 1.08 | 0.08 | −0.15 to 0.16 | p = 0.001** |
| Case without LTC | 932 | 0.11 | 1.09 | 0.04 | 0.04 to 0.18 | ||
| Control with LTC | 1155 | 0.04 | 0.86 | 0.03 | −0.01 to 0.09 | ||
| Control without LTC | 5556 | 0.00 | 0.75 | 0.01 | −0.02 to 0.02 | ||
| Total | 7829 | 0.02 | 0.83 | 0.01 | 0.00 to 0.03 | ||
| Number of in-patient admissions | Case with LTC | 110 | −0.02 | 0.54 | 0.05 | −0.12 to 0.08 | p = 0.901 |
| Case without LTC | 500 | 0.02 | 0.75 | 0.03 | −0.04 to 0.09 | ||
| Control with LTC | 825 | −0.02 | 1.50 | 0.04 | −0.11 to 0.07 | ||
| Control without LTC | 4701 | −0.02 | 1.18 | 0.02 | −0.05 to 0.01 | ||
| Total | 6136 | −0.02 | 1.20 | 0.01 | −0.05 to 0.01 | ||
| Total days admitted (Occupied bed days - OBD) | Case with LTC | 110 | 0.96 | 9.06 | 0.86 | −0.75 to 2.68 | p = 0.302 |
| Case without LTC | 500 | 0.15 | 3.11 | 0.14 | −0.12 to 0.43 | ||
| Control with LTC | 825 | −0.16 | 7.22 | 0.21 | −0.58 to 0.25 | ||
| Control without LTC | 4701 | 0.03 | 6.30 | 0.08 | −0.13 to 0.2 | ||
| Total | 6136 | 0.02 | 6.34 | 0.07 | −0.12 to 0.17 | ||
| Number out-patient attendances | Case with LTC | 110 | −0.5 | 1.71 | 0.16 | −0.82 to −0.18 | p = 0.636 |
| Case without LTC | 500 | −0.12 | 1.97 | 0.09 | −0.3 to 0.05 | ||
| Control with LTC | 825 | −0.21 | 3.37 | 0.1 | −0.41 to −0.02 | ||
| Control without LTC | 4701 | −0.20 | 2.70 | 0.04 | −0.27 to −0.13 | ||
| Total | 6136 | −0.2 | 2.76 | 0.03 | −0.26 to -0.14 | ||
| Number of A&E attendances | Case with LTC | 110 | 0.11 | 0.67 | 0.06 | −0.02 to 0.24 | p = 0.009** |
| Case without LTC | 500 | 0.03 | 0.70 | 0.03 | −0.03 to 0.09 | ||
| Control with LTC | 825 | −0.10 | 1.00 | 0.03 | −0.16 to −0.05 | ||
| Control without LTC | 4701 | −0.08 | 0.98 | 0.01 | −0.11 to −0.06 | ||
| Total | 6136 | 0.06 | 1.03 | 0.05 | −0.1 to -0.05 | ||
Cases = people with CMHP referred to IAPT; Controls = people with CMHP not referred to IAPT. Bold represents statistical significance.
Comparison of intervention and control groups for people with LTCs
Between the intervention (n = 186) and control group (n = 1155) with LTCs there were no significant differences in the proportion of the individual LTCs, or in their demographics including the ethnicity of the two groups (Table 5). The mean age in the intervention group was 53.0years (SD 10.99) and the same in the controls 52.6years (SD 11.24); psychological therapies were targeted at people of working age at the time of this study, Fig. 3. Most of the people with LTCs and CMHPs in the study population who were referred to IAPT were in the age bands between 45 and 60 years old, female, of white ethnicity, and less likely to be of Asian ethnicity. There was also no statistically significant difference in the prevalence of LTCs between the intervention and the control group: 16.6% (186/1118) compared with 17.2% (1155/6711), respectively (Pearson chi square p = 0.64 n.s, Fig. 1).
Table 5.
Demographic and clinical characteristics of people with LTC in the cases and control groups.
| Population |
Cases LTC |
Controls LTC |
Population |
Significance |
|||
|---|---|---|---|---|---|---|---|
| Characteristic |
N = 186 |
N = 1155 |
N = 1341 |
Chi square | |||
| n | % | n | % | n | % | ||
| Gender | p = 0.836 | ||||||
| Female | 119 | 64 | 748 | 64.8 | 867 | 64.7 | |
| Male | 67 | 36 | 407 | 35.2 | 474 | 35.3 | |
| Ethnicity | |||||||
| White | 99 | 53.2 | 498 | 43.1 | 597 | 44.5 | |
| Black | 20 | 10.8 | 138 | 11.9 | 158 | 11.8 | |
| Asian | 14 | 7.5 | 129 | 11.2 | 143 | 10.7 | |
| Chinese & other | 2 | 1.1 | 23 | 2 | 25 | 1.9 | |
| Mixed | 2 | 1.1 | 10 | 0.9 | 12 | 0.9 | |
| LTCs | |||||||
| Diabetes | 55 | 29.6 | 370 | 32 | 425 | 31.7 | p = 0.503 |
| CKD | 26 | 14 | 175 | 15.2 | 201 | 15 | p = 0.677 |
| Heart failure | 5 | 2.7 | 38 | 3.3 | 43 | 3.2 | p = 0.665 |
| IHD | 25 | 13.4 | 186 | 16.1 | 211 | 15.7 | p = 0.355 |
| Hypertension | 133 | 71.5 | 799 | 69.2 | 932 | 69.5 | p = 0.522 |
| COPD | 2 | 1.1 | 28 | 2.4 | 30 | 2.2 | p = 0.248 |
A six-month before and after comparison of people with LTC referred to IAPT revealed that they also received more prescriptions of anti-depressants (p < 0.001) and had more out-patient appointments after referral (p = 0.003, Table 6). The number of admissions was unchanged, and although bed days fell from 1.33 to 0.36, this change was not statistically significant (p = 0.267). There was also a slight reduction in A&E attendance, also not statistically significant (p = 0.090).
Table 6.
Utilisation of healthcare resources of people with LTC and CMHP (cases) before and after 6 months IAPT intervention.
| Referral to IAPT | n= | Mean | Mean difference | SE difference | 95% CI of the difference | t-test sig. (2 tailed) | |
|---|---|---|---|---|---|---|---|
| Numbers of Anti-depressant Px | Before | 186 | 1.25 | −0.94 | 0.18 | −1.30 to −0.58 | p < 0.001 |
| After | 186 | 2.19 | |||||
| Number of recent sick notes issued | Before | 186 | 0.41 | 0.01 | 0.08 | −0.15 to 0.16 | p = 0.946 |
| After | 186 | 0.40 | |||||
| Number of in-pt admissions | Before | 110 | 0.25 | −0.02 | 0.05 | −0.12 to 0.08 | p = 0.725 |
| After | 110 | 0.26 | |||||
| Total days admitted (OBD) | Before | 110 | 1.33 | 0.96 | 0.86 | −0.75 to 2.68 | p = 0.267 |
| After | 110 | 0.36 | |||||
| Number out-pt attendances | Before | 110 | 1.40 | −0.50 | 0.16 | −0.82 to −1.76 | p = 0.003 |
| After | 110 | 1.90 | |||||
| Number of A&E attendances | Before | 110 | 0.33 | 0.11 | 0.06 | −0.02 to 0.24 | p = 0.090 |
| After | 110 | 0.22 |
Finally, we made a six-month before and after comparison with age, sex, practice matched controls of the intervention group with the control group with LTCs. Consistent with our earlier findings there was a statistically significant increase in prescription of antidepressants, over and above those prescribed to the control group (mean difference −0.94 vs. −0.32 respectively; p = 0.001). There was also a fall in A&E attendances, compared with an increase in the control group (0.11 vs. −0.10, respectively; p = 0.003). There was also an increase in out-patients attendances, a fall in bed days, and no change in admissions, but these differences were not significant (Table 7).
Table 7.
Healthcare consumption in the six months before and after IAPT intervention - comparing cases and controls with LTC (controlled for age, gender and practice).
| People with LTC | n= | Mean changes | Mean difference between intervention and control | SE difference | 95% CI of the difference | t-test sig. (2 tailed) | |
|---|---|---|---|---|---|---|---|
| Numbers of antidepressant Px | Intervention | 186 | −0.94 | −0.62 | 0.19 | −0.99 to −0.25 | p = 0.001 |
| Control | 1155 | −0.32 | |||||
| Number of recent sick notes issued | Intervention | 186 | 0.01 | −0.03 | 0.08 | −0.20 to 0.13 | p = 0.649 |
| Control | 1155 | 0.04 | |||||
| Number of admissions | Intervention | 110 | −0.02 | 0.00 | 0.07 | −0.13 to 0.13 | p = 0.990 |
| Control | 1155 | −0.02 | |||||
| Total bed-days admitted (OBD) | Intervention | 110 | 0.96 | 1.13 | 0.89 | −0.63 to 2.89 | p = 0.207 |
| Control | 1155 | −0.16 | |||||
| No of out-patients attendances (OPD) | Intervention | 110 | −0.50 | −0.29 | 0.19 | −0.66 to 0.09 | p = 0.134 |
| Control | 1155 | −0.21 | |||||
| Number of A&E attendances | Intervention | 110 | 0.11 | 0.21 | 0.07 | 0.07–0.35 | p = 0.003 |
| Control | 1155 | −0.10 |
Discussion
Principal findings
People with LTC had more admissions and much longer bed occupancy once admitted to hospital. With the exception of heart failure, people with CMHP are a little more likely to have co-morbid long term conditions (i.e. Diabetes, CKD, IHD, Hypertensive disease and COPD).
Referral of people with LTC and CMHP to an IAPT service was associated with increased antidepressant medication and less use of the emergency department than controls. There was a numeric decrease in the number of bed days and increase in out-patient use but these changes were not significant.
There appeared to be unrepresentativeness in terms of the gender and ethnicity of referrals to IAPT. More women and more people of white ethnicity were referred, and fewer of Asian ethnicity than would be expected if referral were evenly spread between ethnic groups.
Implications of the findings
LTCs are associated with CMHP, though we have no insight from these data as to the causal relationship.
Referral to IAPT seems to be appropriate for people with LTC and CMHP. It is plausible that the act of referral, which requires acknowledgement that there may be health benefit from treating a psychological component of their illness, may help provide insight and be therapeutic.
The over-representation of women, and people of with long term conditions and the ethnic disparity between groups warrants further exploration.
These results provide support for IAPT services. IAPT appears to add something to usual practice and may be more effective in dealing with the combination of LTC and CMHP by reducing their healthcare utilization. IAPT may have a role in helping to reduce attendances at A&E departments. It is possible that improving psychological health either directly improves physical health or patients ability to cope with symptoms from their LTC.
The disparity in referral between gender and ethnicity needs further exploration, but current service models may not be accessible to all ethnic groups and genders.
Comparison with the literature
Other studies have shown that people with LTC are known to use health services and resources to a greater extent than those without them, and comorbid CMHP further increases utilisation (Shen et al., 2008).
We found people with COPD approximately twice as likely to have mental health problems as those without it; an increased prevalence of anxiety and depression in COPD patients has also been found in other studies (Janssen et al., 2010).
These results are consistent with a study which found that helping people recognize the link between their physical symptoms and their stress or emotions resulted in a drop in number of visits to emergency departments (Abbass, Campbell, Magee, & Tarzwell, 2009). Also, antidepressant medications may have an additive effect further increasing the effect of psychological interventions and further reduce the use of services in patients with CMHP and LTCs (Clarke & Currie, 2009).
The findings about gender and ethnic disparities are compatible with other studies: Asian ethnicity is associated with a lower uptake of services (Commander, Odell, Surtees, & Sashidharan, 2004; Hussain & Cochrane, 2004); and females have higher consultation and prescribing rates in primary care and for depression (Moore et al., 2009; Shah, McNiece, & Majeed, 2001).
Limitations of the method
A longer period of data observation would be able to confirm these outcomes more strongly. It is possible with long lead times between referral and review in outpatients and subsequent inpatients that the effect of the intervention (referral to IAPT) had not had sufficient chance to percolate through the system and have an impact. In theory the English NHS has a target that treatment should take place within 18 weeks of referral, approximately five months (Godden & Pollock, 2009). However, patients referred to IAPT are not treated instantly so any impact might not be picked up in a six month period of observation.
There are well known limitations to collecting and working with routinely collected data (de Lusignan & van Weel, 2006) there are some possible limitations such as missing or incomplete data. We anticipated that the disease prevalence identified from the GP data would be higher because the P4P used a limited list of codes, defined within business rules (NHS Primary Care Commissioning), whilst there were a much wider range of codes that might be used to identify people with each of these conditions. We had experience of many of the coding pitfalls in diabetes (de Lusignan, Sadak, et al., 2011), CKD (Anandarajah et al., 2005), heart failure (Majeed, Williams, de Lusignan, & Chan, 2005), and hypertension (Stevens, Farmer, & de Lusignan, 2011). This was also not strictly a like-for-like comparison; the coding system used the term “Ischaemic Heart Disease (IHD)” whereas P4P used a narrower definition of “coronary heart disease (CHD); ” the coding system also used the broader term “heart failure” whereas P4P was limited to left ventricular dysfunction. The only exception expected was COPD where the P4P prevalence could exceed that extracted from GP data. This was likely to be an artefact of the coding system which had similar rubrics for acute and chronic bronchitis (using the latter as a synonym for COPD) and where COPD (code H3), was a parent code of asthma, code H33 (Faulconer & de Lusignan, 2004).
Issue of prescriptions does not prove adherence (van Geffen et al., 2009; Hunot, Horne, Leese, & Churchill, 2007). Whilst it would have been useful to have had a direct measure of adherence we cannot identify any reasons for a systematic bias between arms.
There are known weaknesses of the controlled before and after design (Grimshaw, Campbell, Eccles, & Steen, 2000). Due to the non-randomised design it is difficult to draw causal inference; and there is potential for there to be unknown confounders a known problem with primary care databases (Smeeth, Donnan, & Cook, 2006), even though we attempted to select a control group comparable to the intervention group. Other potential limitations include the absence of patient level details about the severity of the condition and variability in the quality of the IAPT service. Notwithstanding these limitations the study meets the criteria set by the Cochrane Effective Practice and Organisation of Care (EPOC) Review Group data collection checklist criteria for being included in EPOC reviews (McAuley & Ramsay, 2002).
Call for further research
The causal path is not explored from this analysis. Further research, possibly a cohort study, might explore whether LTC preceded CMHP, or do more people with CMHP go on to suffer from LTC.
We need to explore reasons for apparent bias in referral of more women than men – seen in both people with and without LTCs. The data from this study would allow us to conduct a power calculation for a more definitive study, possibly a cluster randomised trial. Such an investigation could be used to explore any health economic benefit of the IAPT service.
Conclusion
Referral to psychological therapies is associated with better adherence to antidepressant medicines and less A&E attendance, in people with LTCs and CMHPs. Larger studies are needed to explore the relationship with bed occupancy and attendance at out-patients as well as a longer period of observation to confirm these outcomes. The IAPT service reduces A&E attendances whilst simultaneously treating CMHP more effectively in people with long term physical illness.
Contributions
All authors read and approved the final manuscript
SdeL: Principal investigator for the nested DH funded data linkage project within the larger NHIR SDO programme funded this study (Ref: 08/1610/154); overall design and responsibility for the project. Developed the analysis plan with TC, drafted the paper outline and made major contributions to subsequent drafts and wrote the final draft.
TC: Developed the detailed protocol, managed the ethics and PIAG (Patient Information Advisory Group) application (the forerunner of the NIGB – National Information Governance Board), and made major contributions to preparing the analysis and data tables for the paper.
MT: Enabled this paper to be completed by making a major contribution between first and final versions.
GP: PI of NIHR SDO evaluation of IAPT demonstration sites, input into protocol and contributed to the paper.
KD-B: Input into the detailed organisation and running of all stages of the project and contributed to the paper.
TK: Led the write up of the GP data within the NIHR SDO final report and contributed to the paper with a major contribution to the final draft.
Conflict of interest
The authors have stated that there are none.
Acknowledgements
Patients and practices who allowed routine data to be used in this study. The NIHR SDO programme funded this study (Project 08/1610/154) with additional funding for data linkage from the Department of Health IPT team. Rob Navarro for privately linking these data, and Jeremy van Vlymen for the selecting the matched cases.
Contributor Information
Simon de Lusignan, Email: s.Lusignan@surrey.ac.uk, sdelusignan@gmail.com.
Tom Chan, Email: t.chan@surrey.ac.uk.
Maria C. Tejerina Arreal, Email: tejerina@um.es.
Glenys Parry, Email: G.D.Parry@sheffield.ac.uk.
Kim Dent-Brown, Email: K.Dent-Brown@sheffield.ac.uk.
Tony Kendrick, Email: tony.kendrick@hyms.ac.uk.
References
- Abbass A., Campbell S., Magee K., Tarzwell R. Intensive short-term dynamic psychotherapy to reduce rates of emergency department return visits for patients with medically unexplained symptoms: preliminary evidence from a pre-post intervention study. Canadian Journal of Emergency Medicine. 2009;11(6):529–534. doi: 10.1017/s1481803500011799. [DOI] [PubMed] [Google Scholar]
- Anandarajah S., Tai T., de Lusignan S., Stevens P., O'Donoghue D., Walker M. The validity of searching routinely collected general practice computer data to identify patients with chronic kidney disease (CKD): a manual review of 500 medical records. Nephrology Dialysis Transplantation. 2005;20(10):2089–2096. doi: 10.1093/ndt/gfi006. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T., Wagner E.H., Grumbach K. Improving primary care for patients with chronic illness. The Journal of the American Medical Association. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T., Wagner E.H., Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. The Journal of the American Medical Association. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Clarke D.M., Currie K.C. Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence. Medical Journal of Australia. 2009;190(7 Suppl.):S54–S60. doi: 10.5694/j.1326-5377.2009.tb02471.x. [DOI] [PubMed] [Google Scholar]
- Clark D.M., Layard R., Smithies R., Richards D.A., Suckling R., Wright B. Improving access to psychological therapy: initial evaluation of two UK demonstration sites. Behaviour Research and Therapy. 2009;47(11):910–920. doi: 10.1016/j.brat.2009.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commander M.J., Odell S.M., Surtees P.G., Sashidharan S.P. Care pathways for south Asian and white people with depressive and anxiety disorders in the community. Social Psychiatry and Psychiatric Epidemiology. 2004;39(4):259–264. doi: 10.1007/s00127-004-0736-6. [DOI] [PubMed] [Google Scholar]
- CONSORT . 2010. Transparent reporting of trials. Box 6-intention to treat analysis.http://www.consort-statement.org/consort-statement/further-explanations/box6_intention-to-treat-analysis/ [Google Scholar]
- Drennan V., Goodman C. Nurse-led case management for older people with long-term conditions. British Journal of Community Nursing. 2004;9(12):527–533. doi: 10.12968/bjcn.2004.9.12.17241. [DOI] [PubMed] [Google Scholar]
- Faulconer E.R., de Lusignan S. An eight-step method for assessing diagnostic data quality in practice: chronic obstructive pulmonary disease as an exemplar. Inform Prim Care. 2004;12(4):243–254. [PubMed] [Google Scholar]
- van Geffen E.C., Gardarsdotti r H., van Hulten R., van Dijk L., Egberts A.C., Heerdink E.R. Initiation of antidepressant therapy: do patients follow the GP's prescription? British Journal of General Practice. 2009;59(559):81–87. doi: 10.3399/bjgp09X395067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godden S., Pollock A.M. Waiting list and waiting time statistics in Britain: a critical review. Public Health. 2009;123(1):47–51. doi: 10.1016/j.puhe.2008.06.005. [DOI] [PubMed] [Google Scholar]
- Grimshaw J., Campbell M., Eccles M., Steen N. Experimental and quasi-experimental designs for evaluating guideline implementation strategies. Family Practice. 2000;17(Suppl. 1):S11–S16. doi: 10.1093/fampra/17.suppl_1.s11. [DOI] [PubMed] [Google Scholar]
- Hall S., Kulendran M., Sadek A.R., Green S., de Lusignan S. Variability in selecting patients to manage in the community: a service evaluation of community matron's case-finding strategies. Family Practice. 2011;28(4):414–421. doi: 10.1093/fampra/cmq095. [DOI] [PubMed] [Google Scholar]
- Harkness E., Macdonald W., Valderas J., Coventry P., Gask L., Bower P. Identifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(4):926–930. doi: 10.2337/dc09-1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollis S., Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. British Medical Journal. 1999;319:670. doi: 10.1136/bmj.319.7211.670. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunot V.M., Horne R., Leese M.N., Churchill R.C. A cohort study of adherence to antidepressants in primary care: the influence of antidepressant concerns and treatment preferences. Journal of Clinical Psychiatry, the Primary Care Companion. 2007;9(2):91–99. doi: 10.4088/pcc.v09n0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain F., Cochrane R. Depression in South Asian women living in the UK: a review of the literature with implications for service provision. Transcultural Psychiatry. 2004;41(2):253–270. doi: 10.1177/1363461504043567. [DOI] [PubMed] [Google Scholar]
- Janssen D.J., Spruit M.A., Leue C., Gijsen C., Hameleers H., Schols J.M., Ciro network Symptoms of anxiety and depression in COPD patients entering pulmonary rehabilitation. Chronic Respiratory Disease. 2010;7(3):147–157. doi: 10.1177/1479972310369285. [DOI] [PubMed] [Google Scholar]
- Lau A. The case for inclusion: mental health and the NSF for long-term conditions. Advances in Psychiatric Treatment. 2005;11:385–387. [Google Scholar]
- Lempp H., Thornicroft G., Leese M., Fearns N., Graves H., Khoshaba B. Implications of long-term conditions for both mental and physical health: comparison of rheumatoid arthritis and schizophrenia. Quality of Life Research. 2009;18(6):699–707. doi: 10.1007/s11136-009-9486-y. [DOI] [PubMed] [Google Scholar]
- Lopez A.D., Mathers C.D., Ezzati M., Jamison D.T., Murray C.J. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367(9524):1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- de Lusignan S. Codes, classifications, terminologies and nomenclatures: definition, development and application in practice. Inform Prim Care. 2005;13(1):65–70. doi: 10.14236/jhi.v13i1.580. [DOI] [PubMed] [Google Scholar]
- de Lusignan S., Chan T., Parry G., Dent-Brown K., Kendrick T. Referral to a new psychological therapy service is associated with reduced utilisation of healthcare and sickness absence by people with common mental health problems: a before and after comparison. Journal of Epidemiology and Community Health. 2011 doi: 10.1136/jech.2011.139873. [DOI] [PubMed] [Google Scholar]
- de Lusignan S., Navarro R., Chan T., Parry G., Dent-Brown K., Kendrick T. Detecting referral and selection bias by the anonymous linkage of practice, hospital and clinic data using Secure and Private Record Linkage (SAPREL): case study from the evaluation of the Improved Access to Psychological Therapy (IAPT) service. BMC Medical Informatics and Decision Making. 2011;11:61. doi: 10.1186/1472-6947-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lusignan S., Sadek N., Mulnier H., Tahir A., Russell-Jones D., Khunti K. Miscoding, misclassification and misdiagnosis of diabetes in primary care. Diabetic Medicine. 2011 doi: 10.1111/j.1464-5491.2011.03419.x. [DOI] [PubMed] [Google Scholar]
- de Lusignan S., van Weel C. The use of routinely collected computer data for research in primary care: opportunities and challenges. Family Practice. 2006;23(2):253–263. doi: 10.1093/fampra/cmi106. [DOI] [PubMed] [Google Scholar]
- McAuley L., Ramsay S. 2002. Cochrane effective practice and organisation of care review group data collection checklist.http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/datacollectionchecklist.pdf [Google Scholar]
- Majeed A., Williams J., de Lusignan S., Chan T. Management of heart failure in primary care after implementation of the National Service Framework for Coronary Heart Disease: a cross-sectional study. Public Health. 2005;119(2):105–111. doi: 10.1016/j.puhe.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Mathers C.D., Boerma T., Ma Fat D. Global and regional causes of death. British Medical Bulletin. 2009;92:7–32. doi: 10.1093/bmb/ldp028. [DOI] [PubMed] [Google Scholar]
- Michalakidis G., Kumarapeli P., Ring A., van Vlymen J., Krause P., de Lusignan S. A system for solution-orientated reporting of errors associated with the extraction of routinely collected clinical data for research and quality improvement. Studies in Health Technology and Informatics. 2010;160(Pt 1):724–728. [PubMed] [Google Scholar]
- Moore M., Yuen H.M., Dunn N., Mullee M.A., Maskell J., Kendrick T. Explaining the rise in antidepressant prescribing: a descriptive study using the general practice research database. British Medical Journal. 2009;339:b3999. doi: 10.1136/bmj.b3999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mounib, E., Satchi, T. (2000). Automating the selection of controls in case-control studies. In: Proceedings of the 25th SAS users' group international conference. Paper 230-25.
- NHS Information Centre. Prevalence data tables: PCT. Level QOF tables 2008/09 – Prevalence. URL: http://www.ic.nhs.uk/statistics-and-data-collections/supporting-information/audits-and-performance/the-quality-and-outcomes-framework/qof-2008/09/data-tables/prevalence-data-tables.
- NHS Information Centre. Quality and Outcomes Framework. URL: http://www.ic.nhs.uk/statistics-and-data-collections/audits-and-performance/the-quality-and-outcomes-framework.
- NHS Primary Care Commissioning. QOF implementation: Business rules. URL: http://www.pcc.nhs.uk/145.php.
- Parry G., Barkham M., Brazier J., Dent-Brown K., Hardy G., Kendrick T. NIHR Service Delivery and Organisation Programme; 2011. An evaluation of a new service model: improving Access to Psychological Therapies demonstration sites 2006–2009.http://www.sdo.nihr.ac.uk/files/project/SDO_FR_08-1610-154_V01.pdf Final report. URL: [Google Scholar]
- Patten S.B. Long-term medical conditions and major depression in a Canadian population study at waves 1 and 2. Journal of Affective Disorders. 2001;63(1–3):35–41. doi: 10.1016/s0165-0327(00)00186-5. Mar. [DOI] [PubMed] [Google Scholar]
- Patten S.B., Williams J.V., Lavorato D.H., Modgill G., Jetté N., Eliasziw M. Major depression as a risk factor for chronic disease incidence: longitudinal analyses in a general population cohort. General Hospital Psychiatry. 2008;30(5):407–413. doi: 10.1016/j.genhosppsych.2008.05.001. Sep–Oct. [DOI] [PubMed] [Google Scholar]
- Shah R., McNiece R., Majeed A. General practice consultation rates for psychiatric disorders in patients aged 65 and over: prospective cohort study. International Journal of Geriatric Psychiatry. 2001;16(1):57–63. doi: 10.1002/1099-1166(200101)16:1<57::aid-gps273>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Shen C., Sambamoorthi U., Rust G. Co-occurring mental illness and health care utilization and expenditures in adults with obesity and chronic physical illness. Disease Management. 2008;11(3):153–160. doi: 10.1089/dis.2007.0012. [DOI] [PubMed] [Google Scholar]
- Smeeth L., Donnan P.T., Cook D.G. The use of primary care databases: case-control and case-only designs. Family Practice. 2006;23(5):597–604. doi: 10.1093/fampra/cml025. [DOI] [PubMed] [Google Scholar]
- Stevens P.E., Farmer C.K., de Lusignan S. Effect of pay for performance on hypertension in the United Kingdom. American Journal of Kidney Disease. 2011;58(4):508–511. doi: 10.1053/j.ajkd.2011.06.010. [DOI] [PubMed] [Google Scholar]
- Tsai A.C., Morton S.C., Mangione C.M., Keeler E.B. A meta-analysis of interventions to improve care for chronic illnesses. American Journal of Managed Care. 2005;11(8):478–488. [PMC free article] [PubMed] [Google Scholar]
- Wilson T., Buck D., Ham C. Rising to the challenge: will the NHS support people with long term conditions? British Medical Journal. 2005;330(7492):657–661. doi: 10.1136/bmj.330.7492.657. [DOI] [PMC free article] [PubMed] [Google Scholar]