Summary
The most common form of heart failure occurs with normal systolic function and often involves cardiac hypertrophy in the elderly. To clarify the biological mechanisms that drive cardiac hypertrophy in aging, we tested the influence of circulating factors using heterochronic parabiosis, a surgical technique in which joining of animals of different ages leads to a shared circulation. After 4 weeks of exposure to the circulation of young mice, cardiac hypertrophy in old mice dramatically regressed, accompanied by reduced cardiomyocyte size and molecular remodeling. Reversal of age-related hypertrophy was not attributable to hemodynamic or behavioral effects of parabiosis, implicating a blood-borne factor. Using modified aptamer-based proteomics, we identified the TGFβ superfamily member GDF11 as a circulating factor in young mice that declines with age. Treatment of old mice to restore GDF11 to youthful levels recapitulated the effects of parabiosis and reversed age-related hypertrophy, revealing a new therapeutic opportunity for cardiac aging.
INTRODUCTION
Among the diseases and disorders associated with advancing age, one of the most debilitating is the loss of normal cardiac function leading to heart failure. Heart failure affects approximately 1% of individuals over 50 and over 5% of individuals over 75. With the ongoing steep rise in the proportion of elderly individuals within our population (Schocken et al., 2008), age-related heart failure is becoming increasingly prevalent.
Most age-related heart failure occurs in the setting of normal systolic function and is called “diastolic heart failure”, in contrast to “systolic heart failure” (Aurigemma, 2006). Although progress has been made in the treatment of systolic heart failure, with substantial improvements in outcome over the past two decades, progress in treating diastolic heart failure has been much more elusive (Hunt et al., 2009). Indeed, one can argue that there are no specific therapies for patients who experience the ventricular “stiffening” associated with the diastolic dysfunction that accompanies aging (Kitzman and Daniel, 2007).
Emerging evidence indicates that systemic factors profoundly influence tissue aging. Some of these data have emerged from the experimental model of parabiosis, which was first developed in the 19th century (Finerty, 1952). In parabiosis, two mice are surgically joined, such that they develop a shared blood circulation with rapid and continuous exchange of cells and soluble factors at physiological levels through their common circulatory system (Wright et al., 2001). The pair of animals may be the same age (isochronic parabionts) or different ages (heterochronic parabionts). Because parabiotic mice are connected solely through their common circulation, parabiosis is a powerful model to determine whether circulating factors can alter tissue function (Balsam et al., 2004; Brack et al., 2007; Conboy et al., 2005; Eggan et al., 2006; Ruckh et al., 2012; Sherwood et al., 2004; Villeda et al., 2011; Wagers et al., 2002; Wright et al., 2001). Heterochronic parabiosis experiments suggest that blood-borne signals from a young circulation can significantly impact the function of aging tissues, as indicated by the restoration of appropriate activation and function of endogenous, “old” skeletal muscle satellite cells and successful muscle repair after injury following exposure to a “youthful” systemic milieu (Conboy et al., 2005). Conversely, exposing a young mouse to an old systemic environment can inhibit myogenesis (Brack et al., 2008) and neurogenesis (Villeda et al., 2011) in the young mouse.
Cardiac hypertrophy is a prominent pathological feature of age-related diastolic heart failure (Aurigemma, 2006). Here, using a parabiosis model, we demonstrate that age-related cardiac hypertrophy can be reversed by exposure to a young circulatory environment. These experiments reveal that the cardiac hypertrophy of aging is at least in part mediated by circulating factors, and led to the discovery that systemic GDF11, a TGFβ family member, can reverse age-related cardiac hypertrophy. These data suggest that at least one pathologic component of age-related diastolic heart failure is hormonal in nature and reversible.
RESULTS
Heterochronic parabiosis reverses age-related cardiac hypertrophy
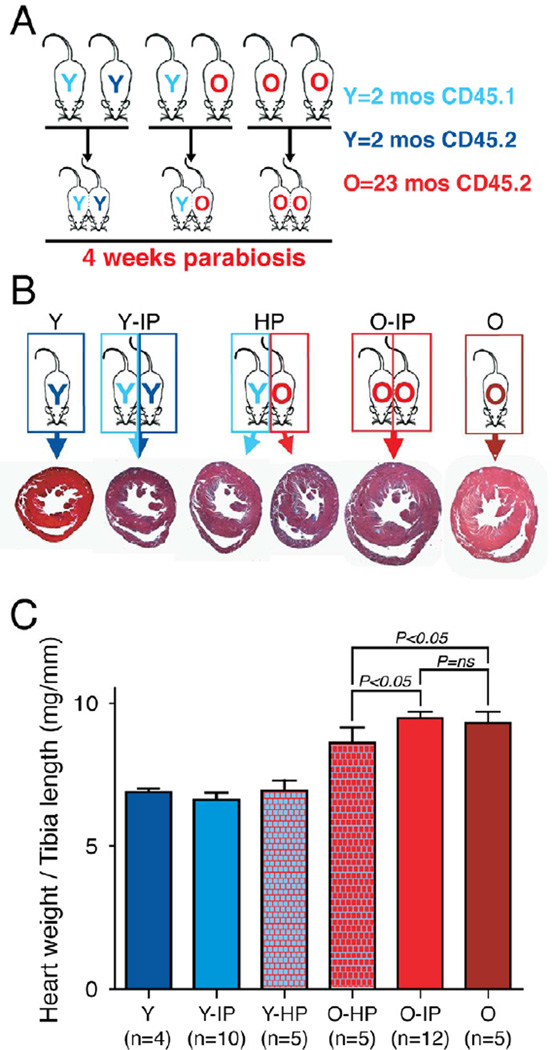
We hypothesized that circulating factors specific to a young mouse might reverse cardiac aging. To test this hypothesis, we generated heterochronic parabiotic (HP) pairs, in which young female C57BL/6 mice (Y-HP, 2 months) were surgically joined to old partners (O-HP, 23 months), and compared these to isochronic parabiotic (IP) pairs (young–young, Y-IP, or old–old, O-IP), joined at identical ages, and to age- and sex-matched unpaired mice as controls (young Y and old O) (Figure 1A). Cardiac aging in C57Bl/6 mice recapitulates human cardiac aging, including development of age-related cardiac hypertrophy (Dai et al., 2009) in a gender independent fashion. Parabiotic pairs were maintained for 4 weeks before analysis, and congenic markers were used to distinguish blood cells from aged (CD45.2+) versus young (CD45.1+) partners (Wright et al., 2001). This strategy allowed us to monitor blood chimerism in the pairs; however, because old CD45.1+ mice are not commercially available, we used only CD45.2+ mice to generate isochronic old pairs. Mice were euthanized 4 weeks after joining, and cross-circulation was confirmed in most of the pairs (>90%) by measuring the frequency of donor-derived blood cells from one partner (CD45.1+) in the blood or spleen of the other partner (CD45.2+) (Figure S1).
Figure 1. Heterochronic parabiosis reverses age-related cardiac hypertrophy.
(A) Experimental scheme. Pairs of young isochronic, heterochronic and old isochronic parabiotic mice were generated. 4 weeks after parabiosis surgery mice were euthanized and tissues harvested for analysis.
(B) Reduced heart size in old mice exposed to a young circulation for 4 weeks. Trichrome stained cross-sections at mid-ventricle.
(C). Graph representing the heart weight / tibia length ratio after 4 weeks of parabiosis. The heart weight to tibia length ratio was significantly lower in old mice exposed to a young circulation (O-HP) compared to old mice exposed to an old circulation (O-IP) for 4 weeks and to old unpaired mice (O). No significant difference was observed when comparing old isochronic to old unpaired mice or when comparing any of the young groups.
Data shown as mean ± s.e.m. See also Figure S1.
The striking effect of a young circulation on old hearts was immediately apparent on visual inspection. Hearts from old mice exposed to a young circulation (O-HP) for 4 wks were noticeably smaller than hearts from O-IP mice. This observation was confirmed by a blinded comparison of short-axis histological sections taken from the midventricle (Figure 1B). We also weighed the hearts at the time of sacrifice and normalized cardiac mass to tibia length, a standard method that corrects for differences in body frame size (Yoshioka et al., 2007) and that is more appropriate than normalization to body weight when using older mice (Jackson et al., 2012; Yin et al., 1982). The heart weight to tibia length ratio was significantly lower in old mice exposed to a young circulation (O-HP) compared to old mice exposed to an old circulation (O-IP), after 4 weeks of parabiosis (7.93+/− 0.19 vs.9.61+/−0.21 mg/mm, P<0.05, Figure 1C).
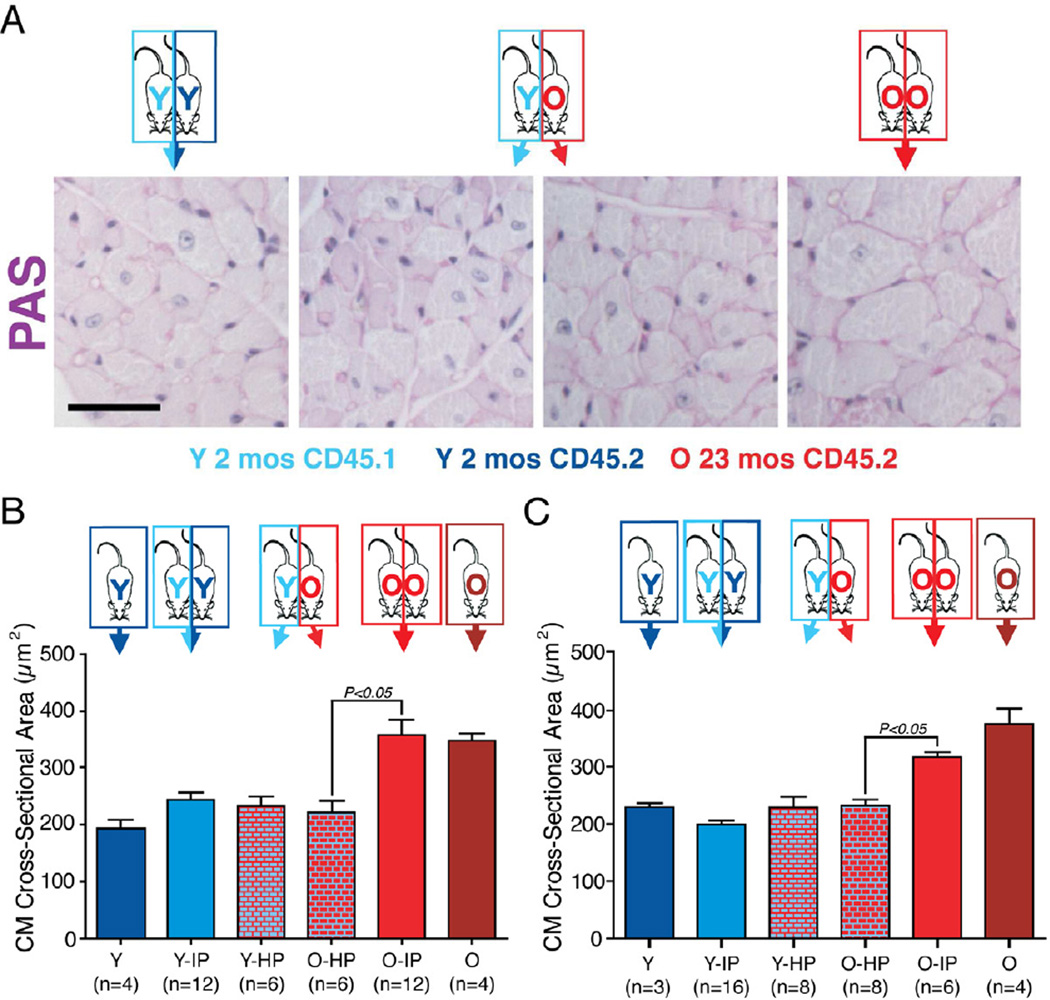
We next tested if the gross regression of cardiac hypertrophy was due to changes in cellular hypertrophy by performing blinded morphometric analysis of cardiac histologic sections (Figure 2A). We found no significant difference in LV cardiac myocyte cross sectional area in young mice from any of the three experimental conditions (186.7±4.9 µm2 in Y, 243.1±12.1 µm2 in Y-IP, 232.2±16.4 µm2 in Y-HP). As expected from published data (Dai et al., 2009), the average cardiac myocyte cross-sectional area was significantly greater in the hearts of the old isochronic (357.8±25.8 µm2) and old non-parabiotic controls (348.3±12.6 µm2) Figure 2B). However, aging hearts from mice exposed to a young circulation for 4 wks (O-HP) showed a significant reduction in myocyte size when compared to O-IP hearts (220.4±21.9 vs. 357.8±25.8 µm2, P<0.05). Thus, exposure to a young circulation reverses the hypertrophic cellular phenotype of aged hearts to the morphologic phenotype typical of a young adult mouse.
Figure 2. Reversal of age-related cardiomyocyte hypertrophy by exposure to a young circulation.
(A) Periodic acid Schiff (PAS) staining of left ventricles 4 wks after parabiosis surgery. Myocytes of aged mice exposed to a young circulation (old heterochronics) are smaller compared to old isochronic controls. Scale bar=20µm.
(B) Graph representing myocyte cross-sectional area measured after PAS staining in female mice. Myocyte size was determined from cross-sectional area (CSA) measurements of 100–200 myocytes per animal in 5 independent myocardial sections. Results are based on the average CSA from 4 to 12 animals per group.
(C) The same experiment as (B) was performed using male mice.
Data shown as mean ± s.e.m.
To evaluate possible sex-specific effects, we repeated these experiments using male mice, and observed a similar regression in age-related hypertrophy after exposure to a young circulation (Figure 2C). These data indicate that gender is not a factor in the reversal of age-related hypertrophy by a young circulation. Thus, age-dependent cardiac hypertrophy may be reversed in both males and females through the activity of systemic factors, and the striking impact of such youthful factors on this age-related pathology is apparent with only 4 weeks of parabiosis.
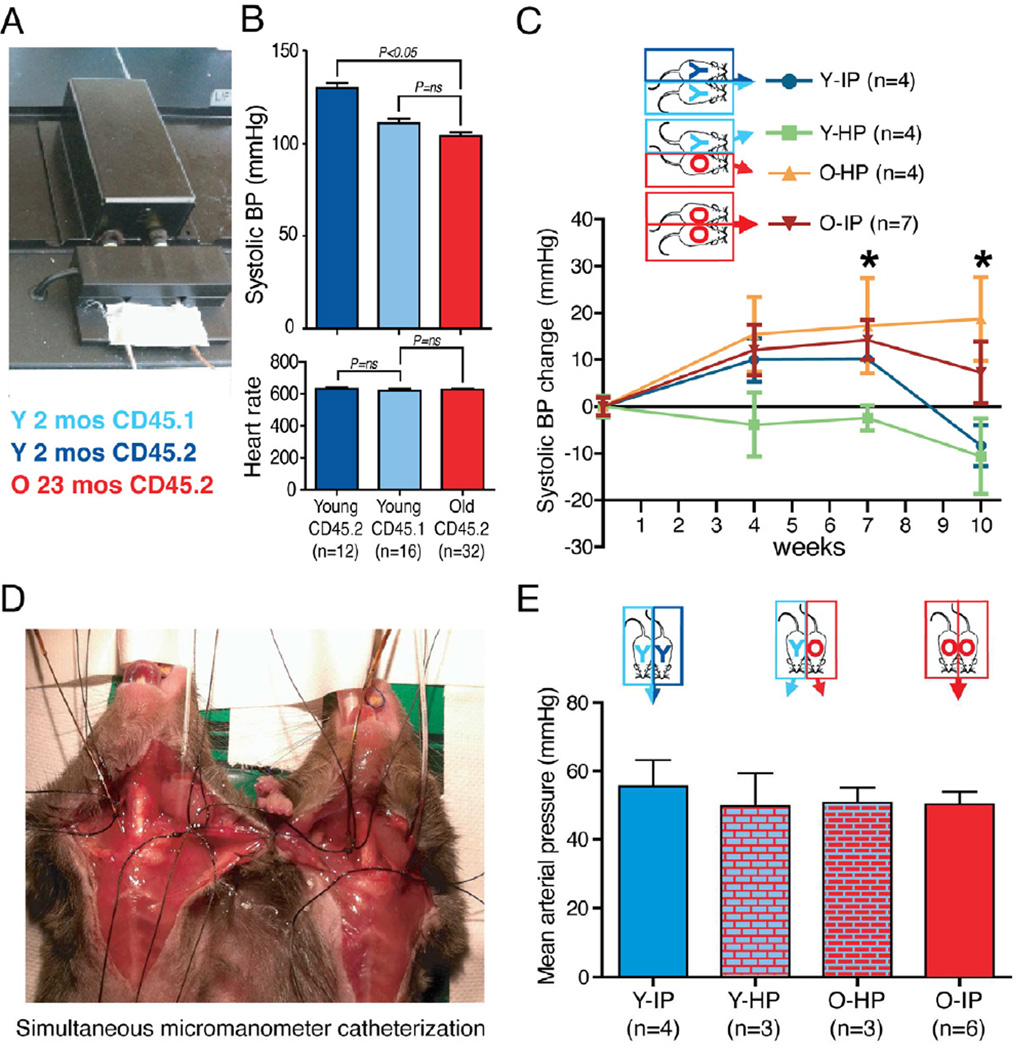
The reversal of cardiac hypertrophy in old mice exposed to a young circulation is not explained by a reduction in blood pressure
A crucial question raised by these data is whether a hemodynamic effect may mediate the reduced cardiac hypertrophy seen in aged mice following heterochronic parabiosis. To explore the hemodynamic issue in the setting of parabiosis, we generated female heterochronic parabiotic pairs (young, 2 months and old, 21 months) and compared them with equal numbers of young and old isochronic parabiotic pairs and with sex and age-matched non-parabiotic controls, using congenic markers to confirm development of cross-circulation (Figure S2A).
Mice were joined for 10 weeks, and during this period we performed noninvasive blood pressure measurements using a computerized tail-cuff system (BP-2000, Visitech Systems, Apex, NC) (Krege et al., 1995) that we modified to hold parabiotic mice (Figure 3A). In non-parabiosed controls (Figure 3B), we observed a significantly lower systolic blood pressure in aged female mice (23 months old and 21 months old, n=32) compared to young (8 wk-old) CD45.2 females (n=12) (98.3±1.8 vs. 129.9±2.0 mmHg, P<0.05), but we saw no difference when comparing aged CD45.2 to young CD45.1 female mice (n=16) (98.3±1.8 vs. 104.1±1.9 mmHg, P=ns). There were no differences in heart rate between the groups (Figure 3B). These data suggest that differences in blood pressure or heart rate at the time of study entry are unlikely to explain the ensuing changes in myocyte size and global ventricular mass seen in O-HP mice.
Figure 3. Reversal of cardiac hypertrophy in old mice exposed to a young circulation cannot be explained by a reduction in blood pressure.
(A). Systolic blood pressure was measured using a computerized tail-cuff system that we modified to allow simultaneous blood pressure measurement of both members of the parabiotic pair.
(B) Systolic blood pressure and heart rate were measured at baseline on unoperated young and old mice. Young (2 months) CD45.2 mice show a significantly higher systolic blood pressure when compared to young CD45.1 (2 months) mice and old (21 months) mice with no difference between young CD45.1 and old mice and no difference in heart rate among all groups.
(C). Using the system shown in (A), blood pressure was measured simultaneously in each member of the indicated parabiotic pair at 4, 7 and 10 weeks after mice were conjoined. O-HP mice showed a significant increase in systolic blood pressure at 7 and 10 weeks; O-IP mice had a significant increase in blood pressure at 7 weeks when compared to baseline values. *: P<0.05
(D) Mean arterial pressure was determined by performing terminal intra-arterial catheterizations obtained simultaneously on paired mice after they had been conjoined for 10 wks.
(E) No significant intergroup differences in blood pressure were detected with terminal intra-arterial catheter-based measurements.
Data shown as mean ± s.e.m. See also Figure S2.
To further address the possible impact of hemodynamic changes in the parabiotic mice, we also performed noninvasive blood pressure measurements at serial time points on heterochronic pairs and compared them to isochronic young and old pairs over 10 wks. We detected no change over time in the blood pressure of young mice from any of the groups (Figure 3C). In contrast, aged mice exposed to a young circulation (O-HP) showed a significant increase in systolic blood pressure at 7 and 10 weeks, and aged members of isochronic pairs exhibited significantly increased blood pressure at 7 weeks, relative to baseline measurements. Finally, we obtained terminal intra-arterial hemodynamic tracings using simultaneous micromanometer cathetherizations, performed after mice had been joined for 10 weeks (Figure 3D). In these studies, mean arterial pressure did not differ significantly among any of the groups (Figure 3E). Cross-circulation was confirmed after euthanasia by measuring the frequency of donor-derived blood cells from one partner (CD45.1+) in the spleen of the other partner (CD45.2+) (data not shown), and evaluation of cardiac mass confirmed that O-HP mice in this 10 week experiment also showed significant reduction in the heart weight-tibia length index when compared to the old controls (Figure S2B). In addition, cardiac size was unaltered in young mice joined for 10 weeks to an old partner, indicating that prolonged exposure to an aged circulation did not induce hypertrophy in young mice, as might be predicted if young mice were serving as a sink for a hypertrophic factor produced by the old mice (Figure S2B). Finally, consistent with these direct measurements of blood pressure in parabiotic mice, circulating levels of angiotensin II and aldosterone were not different in animals involved in heterochronic parabiosis as compared to their age-matched counterparts joined in isochronic parabiosis (data not shown). Thus, it is unlikely that changes in the renin-angiotensin-aldosterone (RAA) axis, well known for its ability to regulate blood pressure and volume, contribute to remodeling of the myocardium in aged heterochronic parabionts.
Taken together, these data clearly demonstrate that the observed reversal of cardiac hypertrophy in old mice exposed to a young circulation cannot be explained by a simple reduction in blood pressure or modulation of known effectors of blood pressure in the older mice. These data further implicate an anti-hypertrophic factor produced by young mice (rather than dilution of a prohypertrophy factor produced by old mice) in the cardiac remodeling induced by heterochronic parabiosis.
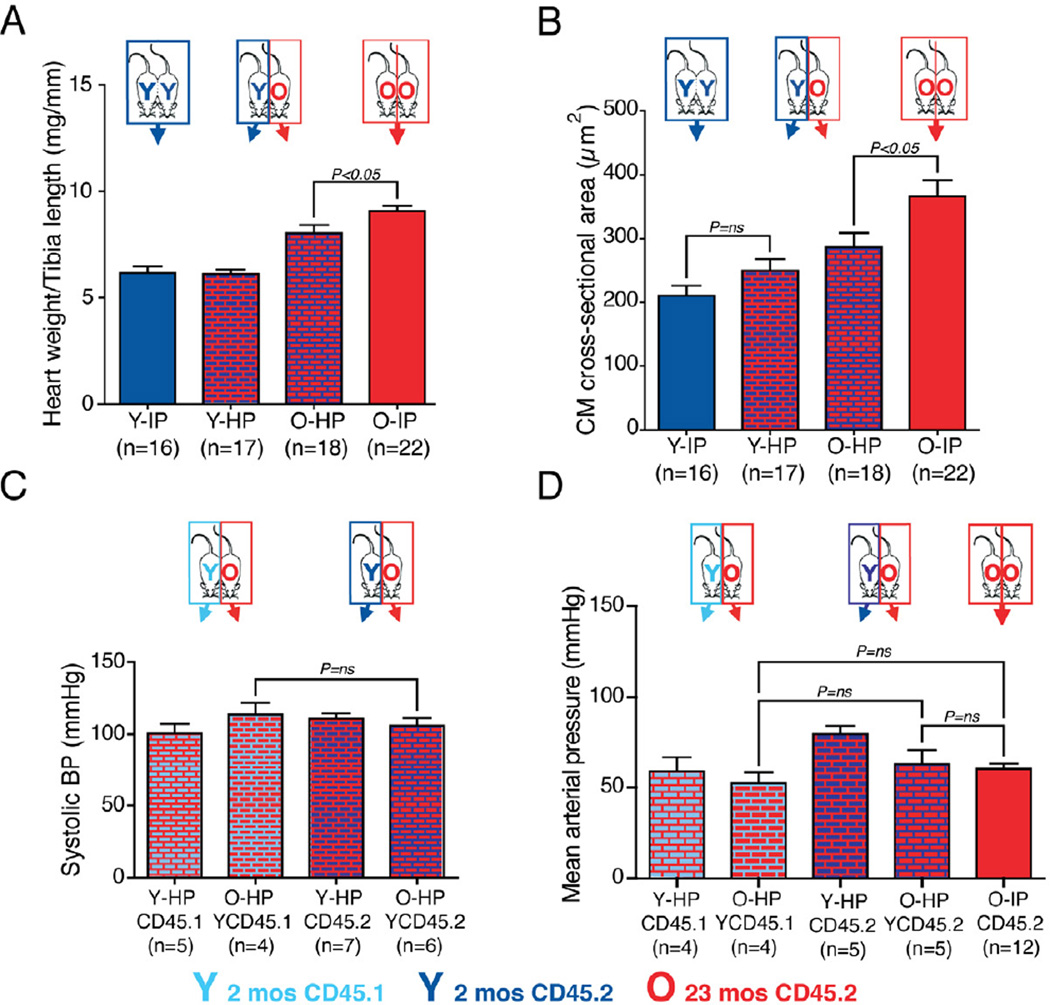
Differences in blood pressure between young CD45.1 and CD45.2 mice do not explain the reversal of cardiac hypertrophy
Because young CD45.1 mice have a significantly lower blood pressure at baseline when compared to young CD45.2 mice, we repeated our parabiosis experiments using exclusively CD45.2 mice to generate heterochronic pairs in which young CD45.2 female mice (Y-HP, 2 months) were joined to aged CD45.2 partners (O-HP, 23 months). We compared these heterochronic mice to isochronic pairs (Y-IP, 2 months, or O-IP, 23 months), after 4 weeks of parabiosis. As the mice in this experiment were genetically identical, we could not use flow cytometry to verify the establishment of chimerism in these pairs; however, extensive experience with this model strongly supports the conclusion that cross-circulation is effectively established in fully isogenic pairs (Pietramaggiori et al., 2009).
As in our prior studies, exposure to the circulation of young CD45.2 mice via parabiosis led to a reduction of heart weight to tibia length ratio in O-HP CD45.2 mice (n=18) when compared to O-IP animals (n=22) (8.03+/− 0.38 vs. 9.07+/−0.24 mg/mm, P<0.05, Figure 4A). Cardiomyocyte cross-sectional area was also significantly reduced in O-HP mice when compared to O-IP (286.3±22.7 vs. 366.4±25.4 µm2, P<0.05, Figure 4B). Aged partners of heterochronic pairings using only CD45.2 mice also showed a blood pressure profile after 4 weeks that was comparable to O-HP mice that had been joined to young CD45.1 partners (Figure 4C-D). Also, similar to results obtained using CD45.1 young partners, heterochronic parabiosis induced no changes in heart weight/tibia ratio (Figure 4A), cardiomyocyte size (Figure 4B), or blood pressure in young CD45.2 mice joined to aged partners (Figure 4C-D). These data demonstrate that the regression of cardiac hypertrophy observed in old mice exposed to a young circulation cannot be explained by the blood pressure differences we observed in young CD45.1 and CD45.2 C57Bl/6 mice.
Figure 4. Differences in blood pressure between young CD45.1 and CD45.2 mice do not explain the reversal of cardiac hypertrophy.
(A) Graph representing the heart weight / tibia length ratio after 4 weeks of parabiosis, using only CD45.2 mice.
(B) Left ventricular myocyte cross-sectional area based on PAS staining in CD45.2 mice. Exposure of an old mouse to the circulation of a young CD45.2 mouse reverses cardiac hypertrophy.
(C) Old mice conjoined to young CD45.1 or CD45.2 mice show no difference in blood pressure measured by the tail-cuff system (Fig. 3A) after 4 weeks.
(D) No significant intergroup differences in blood pressure were detected with terminal intra-arterial catheter-based measurements. Data shown as mean ± s.e.m.
Heterochronic parabiosis is associated with molecular remodeling
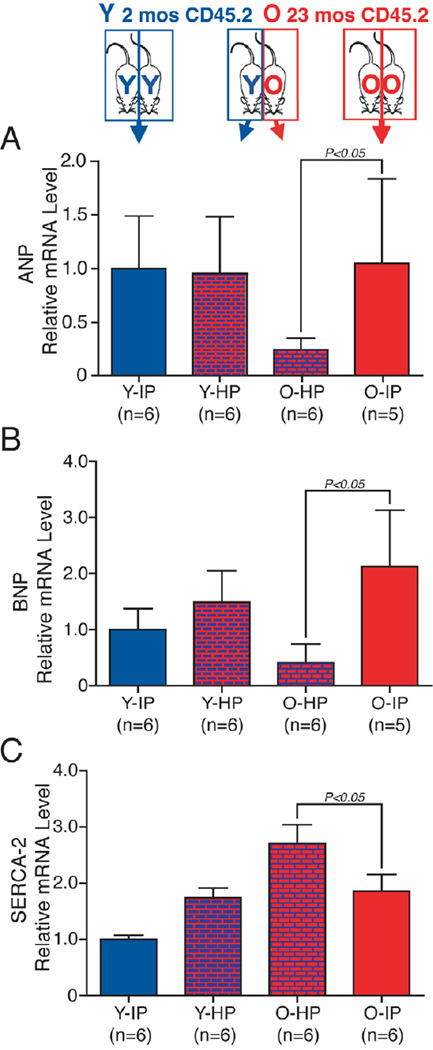
Cardiac hypertrophy is associated with altered expression of a number of cardiac markers. To evaluate the reversal of hypertrophy in O-HP mice on a molecular level, we quantified the cardiac transcriptional expression of atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP), molecular markers of myocyte hypertrophy (Figure 5A-B). We detected a significant reduction in ANP and BNP transcript levels in the hearts of old mice exposed to a young circulation, as compared to the isochronic age-matched controls. Interestingly, the ANP and BNP transcript levels were lower in the old heterochronic mice compared to young isochronic mice. We speculate that this may reflect a process of active regression of cellular hypertrophy, which may be different from nonhypertrophied myocytes in steady-state. We also quantified transcript levels of sarcoplasmic reticulum calcium ATPase (SERCA-2), expression of which may vary with age (Dai et al., 2009) and is functionally important for normal diastolic relaxation. SERCA-2 expression was significantly increased in hearts of aged mice exposed to a young circulation (O-HP) when compared to O-IP controls (Figure 5C). These data provide additional evidence that young circulating factors modify discrete molecular pathways associated with cardiac myocyte hypertrophy and diastolic function.
Figure 5. Molecular evidence for remodeling of aged myocardium by a young systemic circulation.
ANP and BNP transcript levels were significantly reduced in old mice exposed to a young circulation when compared to old isochronic mice. SERCA-2 transcript levels were significantly higher in old mice exposed to a young circulation when compared to old isochronic mice. Transcript levels measured with real-time PCR and normalized to the Y-IP group.
Data shown as mean ± s.e.m.
Behavioral changes associated with parabiosis do not explain reversal of cardiac hypertrophy in heterochronic mice
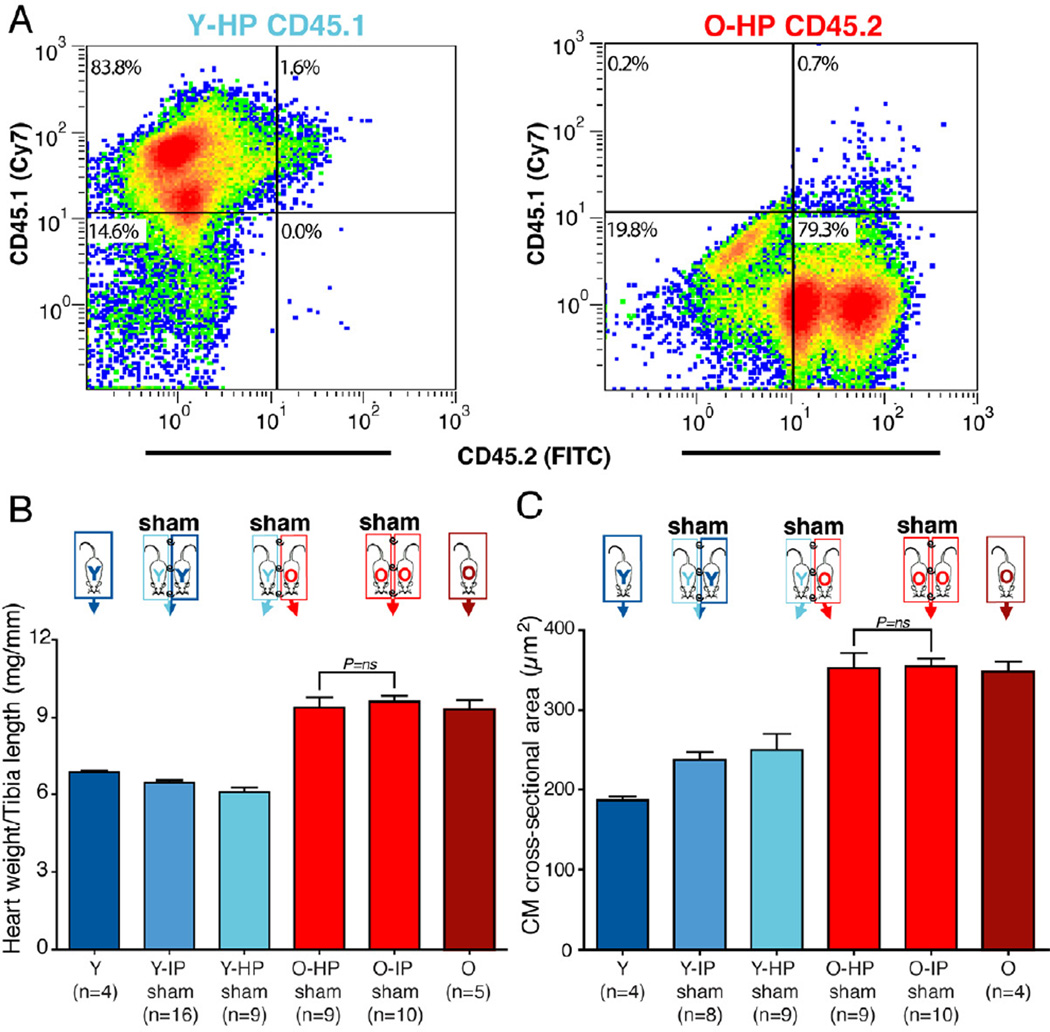
Although the parabiosis model has been used for physiological studies for over a century (Finerty, 1952), we considered the possibility that the physical constraints of parabiotic pairing introduced behavioral changes that contributed to the observed reversal of cardiac hypertrophy. Thus, we developed a surgical technique that we called “sham parabiosis”, whereby mice are surgically joined while leaving the skin intact, such that they do not develop a shared circulation (Figure 6A). We generated sham heterochronic parabiotic pairs, in which young female mice (2 months) were joined to aged partners (23 months), and compared these to sham isochronic parabiotic pairs (young–young or old–old) and to age-matched heterochronic and isochronic parabiotic pairs (Figure 6A-C). The hearts of sham pairs were analyzed after 4 wks, as in prior experiments. In contrast to conventional parabiotic joining, in which effective cross-circulation was established, we found no significant difference in heart weight to tibia length ratio in aged mice involved in sham heterochronic parabiosis, as compared to aged isochronic shams (9.38+/− 0.39 vs. 9.63+/−0.22 mg/mm, P=ns) (Figure 6B). These data indicate that cross-circulation and exchange of blood-borne factors is required for reversal of age-related cardiac hypertrophy. This finding was also confirmed at the cellular level, since cardiomyocyte size in aged heterochronic shams did not differ from myocyte size in aged isochronic shams (352.9±18.9 vs. 355.0±9.5 µm2, P=ns) (Figure 6C). Finally, we evaluated ANP, BNP and SERCA-2 transcript levels in sham operated pairs. Levels of these molecular markers of hypertrophy were either significantly increased (ANP) or unaltered (BNP and SERCA-2) in old heterochronic shams when compared to old isochronic shams (data not shown), indicating that the molecular remodeling associated with reduced cardiac hypertrophy does not occur in the absence of a shared circulation.
Figure 6. Heterochronic sham parabiosis does not reverse cardiac hypertrophy in aged mice.
(A). Flow cytometry plots depicting CD45.1 (y-axis) or CD45.2 expression (x-axis) by splenocytes isolated from young or old mice joined by sham heterochronic parabiosis. Sham parabiotic pairs showed no cross-circulation of partner-derived blood cells as is observed in experimental parabiosis (see Fig S1).
(B). Graph representing the heart weight / tibia length ratio after 4 weeks of sham parabiosis.
(C) Left ventricular myocyte cross-sectional area based on PAS staining after 4 weeks of sham parabiosis.
Data shown as mean ± s.e.m.
Growth differentiation factor 11 is reduced in the circulation of aged mice and “youthful” levels are restored by heterochronic parabiosis
The studies described above strongly suggest that differences in blood-borne factors in young versus old mice underlie the induced cardiac remodeling observed in old mice after heterochronic parabiosis. To identify candidates that might account for the regression of cardiac hypertrophy in old mice exposed to a youthful circulation, we performed a series of screens on serum and plasma collected from young or old mice involved in isochronic or heterochronic parabiosis (4 weeks duration). With plasma from old parabionts exposed to a young circulation or from isochronic controls, we performed metabolomic profiling of 69 amino acids and amines; and lipidomics analysis, assessing 142 lipids from 9 lipid classes: lyso-phosphatidylcholines, lysophosphatidylethanolamines, sphingomyelins, phosphatidyl-cholines, diacylglycerols, cholesterol esters, phosphatidylethanolamines, phosphatidyl-inositols and triacylglycerols. However, we failed to detect significant differences between heterochronic and isochronic parabiotic mice in either the metabolomic or the lipidomic screen (data not shown). We next performed a broad scale proteomics analysis (SomaLogic, Inc. Boulder, CO), using aptamer-based technology to quantitatively evaluate plasma samples from 10 young (2 month) and 10 old (23 month) mice. This approach revealed 13 analytes that reliably distinguished young mice from old mice (Table S1). Of these candidates, one (Growth differentiation factor 11, GDF11, a member of the activin/TGFβ superfamily of growth and differentiation factors) was confirmed in analyses of isochronic and heterochronic parabiotic mice to show differential abundance in the blood plasma of isochronic-old vs. isochronicyoung pairs and a more “youthful” expression profile in old-heterochronic animals (Figure 7A).
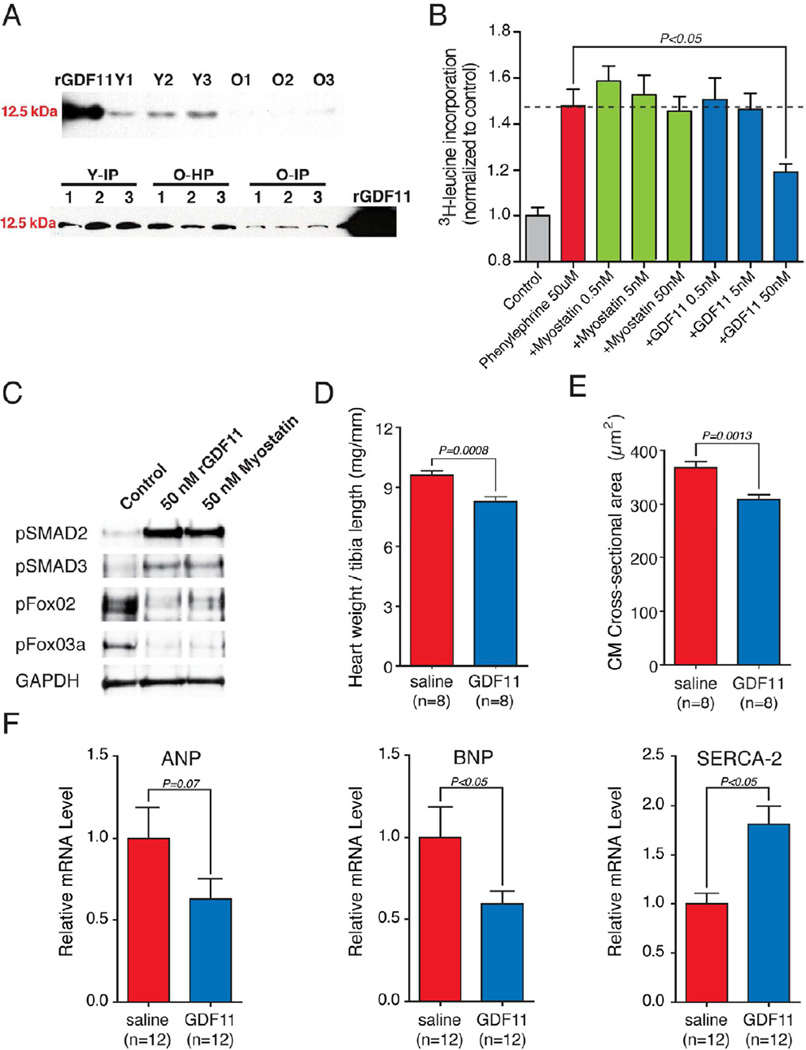
Figure 7. Circulating levels of GDF11 are reduced in aged mice and restoring GDF11 to “youthful” levels promotes reversal of cardiac hypertrophy and molecular remodeling.
(A) Western Blot analysis shows reduced levels of GDF11 in the plasma of old mice compared to young mice (n=3 per group). Similarly GDF11 is reduced in the plasma of old isochronic (O-IP) compared to young isochronic (Y-IP) mice and is restored to “youthful” levels in old mice after exposure to a young circulation (O-HP) (n=3 per group).
(B) Phenylephrine-induced cardiac hypertrophy measured by 3H-leucine incorporation in cardiac myocytes exposed to rGDF11 or myostatin. rGDF11 (50nM) prevented phenylephrine-induced 3H-leucine incorporation.
(C) GDF11 signals through a TGFβ pathway and suppresses Forkhead transcription factor phosphorylation in human cardiomyocytes. Western blots of human induced pluripotent stem cell-derived cardiomyocytes stimulated for 15min with serum free media (Control) or with the same media containing the indicated proteins.
(D) Randomized, vehicle controlled study of rGDF11 therapy in aged (23 mos) mice. rGDF11 (0.1mg/kg) or saline (vehicle control) administered by daily intraperitoneal injection for 30d. Graph representing heart weight / tibia length ratio.
(E) Left ventricular myocyte cross-sectional area measured after PAS staining. rGDF11 therapy leads to a reduction in myocyte cross sectional area.
(F) Expression of ANP, BNP or SERCA-2 in hearts harvested from old mice treated with rGDF11 or saline. Real-time PCR transcript measurements are normalized to levels in the saline group.
Data shown as mean ± s.e.m.
See also Figures S3-S6.
To elucidate possible mechanisms for age dependent reduction in circulating GDF11, we analyzed its expression in a range of tissues and cell populations. Our data suggest wide-spread expression, as previously reported (McPherron, 2010), with the spleen showing the highest levels of GDF11 mRNA (Figure S3A). We next examined GDF11 expression as a function of age, comparing the tissues of old (24 months) and young (3 months) C57Bl/6 mice (Figures S3B-C). We detected a significant decline in both GDF11 gene expression and GDF11 protein levels in the spleens of old mice. These data suggest that a reduction in splenic GDF11 could contribute to the decline of circulating GDF11 in aging mice, although as GDF11 is produced in many organs (McPherron, 2010), changes in expression in other tissues and organs may also contribute.
GDF11 prevents cardiac hypertrophy in vitro and suppresses Forkhead transcription factor phosphorylation
We next tested whether GDF11 displayed anti-hypertrophic properties in cultured neonatal cardiomyocytes using a leucine incorporation assay. After serum starvation, neonatal rat cardiomyocytes were treated for 24h with recombinant GDF11 (rGDF11) or the closely related TGFβ superfamily protein myostatin at three different concentrations, followed by 24h exposure to 3Hleucine and phenylephrine (50µM). We observed a significant and reproducible inhibition of phenylephrine-induced 3H-leucine incorporation in myocytes treated with 50nM rGDF11, an effect that was not observed after treatment with myostatin at the same concentration (Figure 7B). We also tested the ability of rGDF11 or myostatin to activate TGFβ pathways in human induced pluripotent stem cell-derived cardiomyocytes, as previously shown in non-cardiac tissues (Tsuchida et al., 2008). Cells were stimulated for 15min with serum free media (Control) or with the same media containing rGDF11 (50 nM) or Myostatin (50 nM). Cells stimulated with rGDF11 or with myostatin exhibited a significant increase in pSMAD2 and pSMAD3, consistent with activation of TGFβ pathway, and suppression of Forkhead transcription factor phosphorylation (Figure 7C). Taken together, these data suggest that GDF11 has a direct anti-hypertrophic effect at the level of the cardiac myocyte.
GDF11 reverses age related cardiac hypertrophy in vivo
Immunohistochemical staining of mouse cardiac sections with antibodies specific for GDF11 demonstrated evidence for GDF11 at the intercalated discs (Figure S4) between adjacent cardiomyocytes, a region on the plasma membrane where other ligand/receptor interactions have been shown to affect hypertrophic signaling pathways (Gustafson-Wagner et al., 2007; Johnston et al., 2009). These data, together with in vitro evidence (Figure 7B-C) showing GDF11-dependent signaling in cardiomyocytes, provided the rationale to test whether restoring “youthful” levels of circulating GDF11 in aged mice might reverse age-related cardiac hypertrophy. To determine the optimal dosage, route and interval of administration of rGDF11, we first performed a dose-response study, administering the protein to mice by bolus intraperitoneal (i.p.) injection at doses ranging from 0.005 to 0.1 mg/kg (data not shown). Only at the highest dose (0.1 mg/kg) did we observe a reproducible increase in the plasma level of GDF11 1h after injection (Figure S5). Furthermore, analysis of plasma samples collected serially over 48h after a single i.p. administration of 0.1 mg/kg rGDF11, indicated that GDF11 levels were persistently elevated for approximately 24h after this single injection (Figure S5).
Based on these results, we designed a randomized, blinded, vehicle-controlled study to test the effects of rGDF11 on gross and histologic parameters of cardiac hypertrophy. Old (23 month-old) female mice (C57Bl/6) received a daily intraperitoneal injection of rGDF11 (0.1mg/kg) or saline for 30 days (n=16 per group). The heart weight to tibia length ratio was significantly lower in old mice injected with rGDF11 compared to the saline injected control group (Figure 7D). Morphometric analysis further demonstrated that rGDF11 treatment resulted in significantly smaller cardiomyocytes compared to saline-injected controls (Figure 7E).
We also investigated molecular changes in the hearts of rGDF11-treated aged mice. We detected a significant reduction in BNP and a similar trend in ANP, both molecular markers associated with cardiac hypertrophy (Figure 7F). Conversely, SERCA-2 transcript levels, which correlate with diastolic function (Dai et al., 2009), were increased in rGDF11 treated hearts relative to saline-treated age-matched controls. This pattern of rGDF11-induced decrease in molecular markers of hypertrophy and increase in SERCA-2 expression resembles the pattern observed in old mice exposed to a young circulation by parabiosis. We also performed echocardiographic evaluation of 24 month old male C56Bl/6 mice that were randomized to receive a daily intraperitoneal injection of rGDF11 (0.1mg/Kg) or vehicle for 30 days. None of the functional parameters we evaluated was significantly different between the two groups (Table S2).
GDF11 does not prevent cardiac hypertrophy after pressure overload in vivo
To determine if the effect of GDF11 on cardiomyocytes is specific for age-related cardiac hypertrophy, 2 month old female C56Bl/6 mice were subjected to transverse aortic constriction and then randomized to receive a daily IP injection of rGDF11 (0.1mg/Kg) or vehicle for 30 days. We performed an echocardiographic evaluation at 15 days and then prior to sacrifice (Figure S6C). After 30 days, mice were euthanized and hearts were collected for histological and molecular evaluation. We evaluated cardiac morphometry by measuring the heart weight/tibia length ratio: there was no significant reduction in hypertrophy in mice subjected to aortic banding and treated for 30 days with rGDF11 (n=10) as compared with hearts of mice that received only vehicle (n=9) (P=0.4, Figure S6A). Furthermore, cardiomyocyte cross sectional area was not significantly different (Figure S6B). We also evaluated development of cardiac fibrosis and did not detect any difference between the two groups (data not shown). These data suggest that GDF11 does not prevent all forms of cardiac hypertrophy.
DISCUSSION
Left ventricular hypertrophy is an important feature of cardiac aging, contributing to diastolic dysfunction and heart failure with preserved systolic function (Lakatta and Levy, 2003). An autopsy study of elderly subjects without hypertension or clinically evident cardiovascular disease performed by Anversa and colleagues describes cardiomyocyte enlargement and decreased cardiomyocyte number, without a change in total myocardial mass, a pattern that was more pronounced in males (Olivetti et al., 1995). A cross-sectional study of a similar patient population, however, suggests an increase in left ventricular wall thickness in both sexes (Lakatta and Levy, 2003). Patients with diastolic dysfunction tend to be older and are more likely to be obese, diabetic, hypertensive and female, compared to patients with systolic dysfunction (Owan and Redfield, 2005), suggesting distinct underlying pathological mechanisms.
The central hypothesis of this study is that the aging cardiac phenotype is reversible upon exposure to factors in a young circulation. We tested this hypothesis using surgically anastomosed parabiotic mice. We chose to use C56Bl/6 mice for these experiments because they develop an age-related cardiac phenotype that resembles humans. In addition, because gender can play a role in physiologic cardiac hypertrophy (Foryst-Ludwig et al., 2011), we performed experiments in both males and females. We found that exposure of old mice to a young circulation via parabiosis reproducibly led to a reversal of cardiac myocyte hypertrophy in a gender-independent fashion, and that this reduced cardiomyocyte size translated into a reduction in global cardiac mass. This structural transformation was accompanied by a reduction in myocardial gene expression of natriuretic peptides known to promote maladaptive cardiac remodeling and an increase in Ca2+ ATPase (SERCA-2), the expression of which is integral to myocardial relaxation and hence normal diastolic function. Together, these data are consistent with the concept that factors present in a young circulation can reverse critical structural and molecular aspects of cardiac aging.
With circulatory transfer of a soluble substance emerging as a likely mechanism of cardiac hypertrophy regression in old parabiotic mice, we performed a systematic search to identify candidate factors present at higher levels in the blood of young mice that might underlie the anti-hypertrophic effect. Our proteomic analysis identified several factors with levels that change with age, and we cannot exclude the possibility that other factors also participate in the effect observed in heterochronic parabiosis; however, GDF11 emerged as a strong candidate from a series of screening analyses comparing the lipid profiles, metabolites, and signaling proteins present in young versus old plasma. While GDF11 expression is detectable in a range of tissues, the spleen shows the highest concentration, and exhibits an age dependent decline in GDF11 levels. Thus, the spleen may contribute to circulating GDF11 and an age-related production or secretory defect in the spleen could participate in the reduction in circulating GDF11 in old mice.
A recent study shows that the treatment of cachexic mice with soluble ActRIIB protein (sActRIIB), which antagonizes signaling by GDF11 (as well as myostatin, activin, and other TGFβ family members, given the promiscuity of the receptors (Tsuchida et al., 2008) reverses cardiac atrophy in tumor-bearing animals (Zhou et al., 2010). Together with our proteomic data, this study further supported the notion that GDF11 acts as a mediator of the systemic anti-hypertrophic activity found in young mice. Moreover, our histological data (Figure S4) suggested binding of GDF11 to cardiomyocytes in vivo. We therefore performed a randomized, vehicle-controlled study, administering rGDF11 to old mice for 30d. This rGDF11 therapy led to a significant regression of cardiac hypertrophy in old mice, as indicated by both heart weight measurements and morphometric analyses.
Moreover, the demonstration that rGDF11, but not myostatin, induced a dose-dependent inhibition of phenylephrine-mediated hypertrophy in neonatal cardiac myocytes, in vitro, suggests that GDF11 has specific and direct effects at the level of the cardiac myocyte. However, both rGDF11 and myostatin stimulated TGFβ signaling pathways including anti-hypertrophic FoxO factors. While it is plausible that the anti-hypertrophic effect of rGDF11 is mediated by FoxO-dependent proteasome-mediated protein degradation (Sandri et al., 2004), our data do not explain the differential effects of rGDF11 and myostatin. We speculate that the differential effect may be due to differences in the activity of endogenous inhibitors and/or subtle differences in receptor affinity (Mueller and Nickel, 2012).
The observation that myostatin negatively regulates skeletal muscle mass led to the development of therapeutic strategies for age- and cancer-related muscle atrophy by blocking myostatin signaling. Interestingly, although myostatin null mice have not consistently demonstrated important changes in cardiac mass during aging (Cohn et al., 2007; Jackson et al., 2012), treatment with a soluble ActRIIB antagonist leads to increased skeletal and cardiac muscle mass, suggesting that the cardiac effects of this antagonist may arise from inhibition of a ligand other than myostatin. Indeed, despite signaling through similar activin receptor combinations, GDF11 and myostatin exhibit many non-overlapping functions. Myostatin null mice demonstrate substantially increased skeletal muscle mass, whereas GDF11 null mice exhibit skeletal and renal abnormalities and die within 24h of birth (McPherron et al., 1999). Thus, we speculate that the reported ActRIIB antagonist effects on myocardium (Zhou et al., 2010) may be due to inhibition of GDF11 signaling and independent of effects on myostatin. Our data demonstrate that GDF11 and myostatin share some in vitro properties; apparent in vivo differences are not yet fully understood.
GDF11 was ineffective in preventing cardiac hypertrophy in the context of pressure overload, suggesting that the antihypertrophic properties of GDF11 may not be generalizable to all forms of cardiac hypertrophy. Interestingly, our preliminary studies suggest that GDF11 treatment may influence aging phenotypes in other tissues, such as skeletal muscle, and further investigations will be important for determining the role of GDF11 in aging beyond the heart.
In summary, our analysis of reverse remodeling in the hearts of heterochronic parabiotic mice led to the identification of GDF11 as an age-regulated circulating factor with potent anti-hypertrophic properties. Our studies implicate GDF11 in age-related cardiac hypertrophy but do not exclude participation of other factors (Table S1) nor do we have direct evidence indicating a role for GDF11 in the development of age-related cardiac hypertrophy in humans, although GDF11 does stimulate phosphorylation of target protein (SMAD2/3) in human pluripotent cell-derived cardiomyocytes (Figure 7C). Recently identified in the circulation of humans (Souza et al., 2008), GDF11 like other TGFβ family members circulates at significantly lower concentrations in humans compared to mice (Souza et al., 2008). Using a proteomic approach, Ganz and colleagues have reported preliminary data that low levels of GDF11 identify a cohort among humans with stable coronary artery disease with a higher risk of composite end-point of all-cause mortality, MI, heart failure, stroke (presented at the 2012 American Heart Association Scientific Sessions). Future studies will be necessary to evaluate the role of GDF11 in human cardiac hypertrophy. We recognize that cardiac hypertrophy of aging is a multifactorial process and that the observed regression of cardiac hypertrophy in old mice exposed to a young circulation is unlikely to be attributable entirely to the replenishment of a single factor. Nonetheless, our results suggest exciting therapeutic possibilities for targeting cardiac hypertrophy of aging by restoring youthful levels of circulating GDF11.
Experimental procedures
Animals
Aged (21–23 months) C57Bl/6 mice were obtained from the National Institute on Aging (NIA); young (2 months) C57Bl/6 (CD45.1−CD45.2+) or young B6.SJL (CD45.1+CD45.2−) mice were obtained from JAX. Maintenance of mouse colonies and all experiments were conducted in accordance with the Guide for the Use and Care of Laboratory Animals and approved by relevant institutional Committees.
Parabiosis
Parabiosis was performed as described previously (Bunster and Meyer, 1933; Ruckh et al., 2012). Blood chimerism was confirmed in a subset of parabiotic pairs by flow cytometry measuring the frequency of donor-derived blood cells from one partner (CD45.1+) in the spleen of the other partner (CD45.2+). Partner-derived cells typically represented 40–50% of splenocytes, consistent with establishment of parabiotic cross-circulation. Because old CD45.1+ mice are not commercially available we could not use this method to verify the establishment of chimerism in isochronic-old parabiotic pairs.
Sham parabiosis
Sham parabiosis was performed as a modification of the parabiosis procedure (Bunster and Meyer, 1933;Ruckh et al., 2012) to achieve surgical joining without development of a shared circulation. Mice were anesthetized to full muscle relaxation and joined by a modification of the technique of Bunster and Meyer. After shaving the corresponding lateral aspects of each mouse, matching skin incisions were made from the olecranon to the knee joint of each mouse, and the subcutaneous fascia was bluntly dissected to create about 1/2 cm of free skin. The olecranon and knee joints were attached with a single 2-0 prolene suture. The suture was sequentially passed through the skin and joint of the first mouse, through a silicon disk to separate the skin of the two mice, and then through the skin and joint of the second mouse. The suture was tied, such that the silicon disk separated the skin of each mouse at the joint and without any contact between the cutaneous flaps of each mouse. The skin incisions were closed with staples. The prolene sutures connecting the mice were reinforced with meshed staples.
Western Blot, flow cytometry, gene expression, metabolomic and lipidomic profiling analysis
Please refer to Supplemental Experimental Procedures.
Morphometric assessment of cardiomyocyte size
Mouse hearts were fixed with 4% paraformaldehyde, paraffin-embedded, sectioned, and stained with periodic acid Schiff (PAS). Staining, scanning, and quantification were carried out in a blinded manner using 5 randomly selected sections from the heart.
Noninvasive blood pressure
We used a computerized tail-cuff system (BP-2000, Visitech Systems, Apex, NC) that we modified to allow simultaneous blood pressure measurement of both members of the parabiotic pair. Unoperated mice or pairs of mice were trained for 5 consecutive days in the pre-warmed tail-cuff device to accustom them to the procedure, followed by measurements of heart rate and systolic blood pressure.
Neurohormonal measurements
Circulating levels of angiotensin II and aldosterone in serum samples were measured by ELISA (Enzo Life Sciences International, INC., USA)
Proteomic analysis
EDTA plasma samples (20 µl) from 20 mice were analyzed on the SomaLogic proteomics discovery platform (SOMAscan), which uses SOMAmers to measure 1001 proteins simultaneously. SOMAmers (Slow Off-rate Modified Aptamers) are nucleic acid-based protein binding reagents evolved through SELEX (Tuerk and Gold, 1990) to bind protein targets. SOMAscan transforms the concentration of proteins in the matrix into a relative quantity of SOMAmers, through equilibration binding and removal of unbound SOMAmers and proteins. The SOMAmer quantity is measured by hybridization to microarrays (for a full description, see(Gold et al., 2010))
In vitro cardiac myocyte hypertrophy assay
Neonatal cardiac myocytes were isolated from post-natal day 1 CD1 rats (Charles River) (Seki et al., 2009). Approximately 36h after plating, cardiac myocytes were serum starved for 24h in low-glucose DMEM supplemented with ITS (PAA Laboratories). Cardiac myocytes were pretreated with myostatin (R&D Systems) or rGDF11 (Peprotech) for 24h, prior to treating with phenylephrine (50µM, Sigma) and assaying protein synthesis/hypertrophy with 3H-leucine (1µCi/ml, Moravek). rGDF11 and myostatin treatments were continued during the period of exposure to phenylephrine and 3H-leucine. 24h after labeling with 3Hleucine, cells were washed with ice-cold PBS and fixed with ice-cold 10% trichloroacetic acid for 45 min at 4C. Cells were lysed with 0.05M NaOH and analyzed by liquid scintillation.
Induced pluripotent stem cell-derived human cardiomyocytes
Please refer to Supplemental Experimental Procedures for induced pluripotent stem cell-derived human cardiomyocytes.
Transverse Aortic Constriction and Echocardiography
Please refer to Supplemental Experimental Procedures for the Transverse Aortic Constriction and Echocardiography procedures.
Statistical analyses
Data comparison subjected to one-way ANOVA and post-hoc Bonferonni correction orStudent’s t-test assuming two-tailed distribution and unequal variances. Statistical significance was assigned for p<0.05; results are shown as standard error of the mean.
Supplementary Material
Highlights.
Heterochronic parabiosis reverses age-related cardiac hypertrophy
The antihypertrophic effect is not due to hemodynamic or behavioral factors
GDF11 is a circulating TGFβ family member that declines with age
Restoration of youthful GDF11 levels reverses age-related cardiac hypertrophy
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the HSCI and DRC (NIH Award Number P30DK036836) Flow Cytometry Cores for excellent cytometry support. This work was funded in part by grants from the American Heart Association to FSL (postdoctoral fellowship) and MLS (AHA FTF), Glenn Foundation and NIH (1RO1 AG033053, 1DP2 OD004345, and 5U01 HL100402) to AJW, NIH (R01 AG032977 1R01 AG040019) to RTL and NIH (KO8 DK090147) to MLS. MLS is supported by the Watkins Cardiovascular Leadership Award. AJW is an Early Career Scientist of the Howard Hughes Medical Institute. Content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funding agencies. SOMAscan and SOMAmers are trademarks of SomaLogic, Inc.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aurigemma GP. Diastolic heart failure--a common and lethal condition by any name. N Engl J Med. 2006;355:308–310. doi: 10.1056/NEJMe068128. [DOI] [PubMed] [Google Scholar]
- Balsam LB, Wagers AJ, Christensen JL, Kofidis T, Weissman IL, Robbins RC. Haematopoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature. 2004;428:668–673. doi: 10.1038/nature02460. [DOI] [PubMed] [Google Scholar]
- Brack AS, Conboy MJ, Roy S, Lee M, Kuo CJ, Keller C, Rando TA. Increased Wnt signaling during aging alters muscle stem cell fate and increases fibrosis. Science. 2007;317:807–810. doi: 10.1126/science.1144090. [DOI] [PubMed] [Google Scholar]
- Bunster E, Meyer RK. An improved method of parabiosis. The Anatomical Record. 1933;57:339–343. [Google Scholar]
- Cohn RD, Liang HY, Shetty R, Abraham T, Wagner KR. Myostatin does not regulate cardiac hypertrophy or fibrosis. Neuromuscul Disord. 2007;17:290–296. doi: 10.1016/j.nmd.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conboy IM, Conboy MJ, Wagers AJ, Girma ER, Weissman IL, Rando TA. Rejuvenation of aged progenitor cells by exposure to a young systemic environment. Nature. 2005;433:760–764. doi: 10.1038/nature03260. [DOI] [PubMed] [Google Scholar]
- Dai DF, Santana LF, Vermulst M, Tomazela DM, Emond MJ, MacCoss MJ, Gollahon K, Martin GM, Loeb LA, Ladiges WC, et al. Overexpression of catalase targeted to mitochondria attenuates murine cardiac aging. Circulation. 2009;119:2789–2797. doi: 10.1161/CIRCULATIONAHA.108.822403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggan K, Jurga S, Gosden R, Min IM, Wagers AJ. Ovulated oocytes in adult mice derive from non-circulating germ cells. Nature. 2006;441:1109–1114. doi: 10.1038/nature04929. [DOI] [PubMed] [Google Scholar]
- Finerty JC. Parabiosis in physiological studies. Physiol Rev. 1952;32:277–302. doi: 10.1152/physrev.1952.32.3.277. [DOI] [PubMed] [Google Scholar]
- Foryst-Ludwig A, Kreissl MC, Sprang C, Thalke B, Bohm C, Benz V, Gurgen D, Dragun D, Schubert C, Mai K, et al. Sex differences in physiological cardiac hypertrophy are associated with exercise-mediated changes in energy substrate availability. Am J Physiol Heart Circ Physiol. 2011;301:H115–H122. doi: 10.1152/ajpheart.01222.2010. [DOI] [PubMed] [Google Scholar]
- Gold L, Ayers D, Bertino J, Bock C, Bock A, Brody EN, Carter J, Dalby AB, Eaton BE, Fitzwater T, et al. Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS One. 2010;5:e15004. doi: 10.1371/journal.pone.0015004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson-Wagner EA, Sinn HW, Chen YL, Wang DZ, Reiter RS, Lin JL, Yang B, Williamson RA, Chen J, Lin CI, et al. Loss of mXinalpha, an intercalated disk protein, results in cardiac hypertrophy and cardiomyopathy with conduction defects. Am J Physiol Heart Circ Physiol. 2007;293:H2680–H2692. doi: 10.1152/ajpheart.00806.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation. 2009;119:e391–e479. doi: 10.1161/CIRCULATIONAHA.109.192065. [DOI] [PubMed] [Google Scholar]
- Jackson MF, Luong D, Vang DD, Garikipati DK, Stanton JB, Nelson OL, Rodgers BD. The aging myostatin null phenotype: reduced adiposity, cardiac hypertrophy, enhanced cardiac stress response, and sexual dimorphism. J Endocrinol. 2012;213:263–275. doi: 10.1530/JOE-11-0455. [DOI] [PubMed] [Google Scholar]
- Johnston RK, Balasubramanian S, Kasiganesan H, Baicu CF, Zile MR, Kuppuswamy D. Beta3 integrin-mediated ubiquitination activates survival signaling during myocardial hypertrophy. FASEB J. 2009;23:2759–2771. doi: 10.1096/fj.08-127480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzman DW, Daniel KR. Diastolic heart failure in the elderly. Clin Geriatr Med. 2007;23:83–106. doi: 10.1016/j.cger.2006.09.002. [DOI] [PubMed] [Google Scholar]
- Krege JH, Hodgin JB, Hagaman JR, Smithies O. A noninvasive computerized tail-cuff system for measuring blood pressure in mice. Hypertension. 1995;25:1111–1115. doi: 10.1161/01.hyp.25.5.1111. [DOI] [PubMed] [Google Scholar]
- Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation. 2003;107:346–354. doi: 10.1161/01.cir.0000048893.62841.f7. [DOI] [PubMed] [Google Scholar]
- McPherron AC. Metabolic Functions of Myostatin and Gdf11. Immunol Endocr Metab Agents Med Chem. 2010;10:217–231. doi: 10.2174/187152210793663810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McPherron AC, Lawler AM, Lee SJ. Regulation of anterior/posterior patterning of the axial skeleton by growth/differentiation factor 11. Nat Genet. 1999;22:260–264. doi: 10.1038/10320. [DOI] [PubMed] [Google Scholar]
- Mueller TD, Nickel J. Promiscuity and specificity in BMP receptor activation. FEBS Lett. 2012;586:1846–1859. doi: 10.1016/j.febslet.2012.02.043. [DOI] [PubMed] [Google Scholar]
- Olivetti G, Giordano G, Corradi D, Melissari M, Lagrasta C, Gambert SR, Anversa P. Gender differences and aging: effects on the human heart. J Am Coll Cardiol. 1995;26:1068–1079. doi: 10.1016/0735-1097(95)00282-8. [DOI] [PubMed] [Google Scholar]
- Owan TE, Redfield MM. Epidemiology of diastolic heart failure. Prog Cardiovasc Dis. 2005;47:320–332. doi: 10.1016/j.pcad.2005.02.010. [DOI] [PubMed] [Google Scholar]
- Pietramaggiori G, Scherer SS, Alperovich M, Chen B, Orgill DP, Wagers AJ. Improved cutaneous healing in diabetic mice exposed to healthy peripheral circulation. J Invest Dermatol. 2009;129:2265–2274. doi: 10.1038/jid.2009.60. [DOI] [PubMed] [Google Scholar]
- Ruckh JM, Zhao JW, Shadrach JL, van Wijngaarden P, Rao TN, Wagers AJ, Franklin RJ. Rejuvenation of regeneration in the aging central nervous system. Cell Stem Cell. 2012;10:96–103. doi: 10.1016/j.stem.2011.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandri M, Sandri C, Gilbert A, Skurk C, Calabria E, Picard A, Walsh K, Schiaffino S, Lecker SH, Goldberg AL. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117:399–412. doi: 10.1016/s0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schocken DD, Benjamin EJ, Fonarow GC, Krumholz HM, Levy D, Mensah GA, Narula J, Shor ES, Young JB, Hong Y. Prevention of heart failure: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation. 2008;117:2544–2565. doi: 10.1161/CIRCULATIONAHA.107.188965. [DOI] [PubMed] [Google Scholar]
- Seki K, Sanada S, Kudinova AY, Steinhauser ML, Handa V, Gannon J, Lee RT. Interleukin-33 prevents apoptosis and improves survival after experimental myocardial infarction through ST2 signaling. Circ Heart Fail. 2009;2:684–691. doi: 10.1161/CIRCHEARTFAILURE.109.873240. [DOI] [PubMed] [Google Scholar]
- Sherwood RI, Christensen JL, Conboy IM, Conboy MJ, Rando TA, Weissman IL, Wagers AJ. Isolation of Adult Mouse Myogenic Progenitors; Functional Heterogeneity of Cells within and Engrafting Skeletal Muscle. Cell. 2004;119:543–554. doi: 10.1016/j.cell.2004.10.021. [DOI] [PubMed] [Google Scholar]
- Souza TA, Chen X, Guo Y, Sava P, Zhang J, Hill JJ, Yaworsky PJ, Qiu Y. Proteomic identification and functional validation of activins and bone morphogenetic protein 11 as candidate novel muscle mass regulators. Mol Endocrinol. 2008;22:2689–2702. doi: 10.1210/me.2008-0290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuchida K, Nakatani M, Uezumi A, Murakami T, Cui X. Signal transduction pathway through activin receptors as a therapeutic target of musculoskeletal diseases and cancer. Endocr J. 2008;55:11–21. doi: 10.1507/endocrj.kr-110. [DOI] [PubMed] [Google Scholar]
- Tuerk C, Gold L. Systematic evolution of ligands by exponential enrichment: RNA ligands to bacteriophage T4 DNA polymerase. Science. 1990;249:505–510. doi: 10.1126/science.2200121. [DOI] [PubMed] [Google Scholar]
- Villeda SA, Luo J, Mosher KI, Zou B, Britschgi M, Bieri G, Stan TM, Fainberg N, Ding Z, Eggel A, et al. The ageing systemic milieu negatively regulates neurogenesis and cognitive function. Nature. 2011;477:90–94. doi: 10.1038/nature10357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagers AJ, Sherwood RI, Christensen JL, Weissman IL. Little evidence for developmental plasticity of adult hematopoietic stem cells. Science. 2002;297:2256–2259. doi: 10.1126/science.1074807. [DOI] [PubMed] [Google Scholar]
- Wright DE, Wagers AJ, Gulati AP, Johnson FL, Weissman IL. Physiological migration of hematopoietic stem and progenitor cells. Science. 2001;294:1933–1936. doi: 10.1126/science.1064081. [DOI] [PubMed] [Google Scholar]
- Yin FC, Spurgeon HA, Rakusan K, Weisfeldt ML, Lakatta EG. Use of tibial length to quantify cardiac hypertrophy: application in the aging rat. Am J Physiol. 1982;243:H941–H947. doi: 10.1152/ajpheart.1982.243.6.H941. [DOI] [PubMed] [Google Scholar]
- Yoshioka J, Imahashi K, Gabel SA, Chutkow WA, Burds AA, Gannon J, Schulze PC, MacGillivray C, London RE, Murphy E, et al. Targeted deletion of thioredoxin-interacting protein regulates cardiac dysfunction in response to pressure overload. Circ Res. 2007;101:1328–1338. doi: 10.1161/CIRCRESAHA.106.160515. [DOI] [PubMed] [Google Scholar]
- Zhou X, Wang JL, Lu J, Song Y, Kwak KS, Jiao Q, Rosenfeld R, Chen Q, Boone T, Simonet WS, et al. Reversal of cancer cachexia and muscle wasting by ActRIIB antagonism leads to prolonged survival. Cell. 2010;142:531–543. doi: 10.1016/j.cell.2010.07.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.