Abstract
Physician racial bias and patient perceived discrimination have each been found to influence perceptions of and feelings about racially discordant medical interactions. However, to our knowledge, no studies have examined how they may simultaneously influence the dynamics of these interactions. This study examined how (a) non-Black primary care physicians’ explicit and implicit racial bias and (b) Black patients’ perceived past discrimination affected physician-patient talk time ratio (i.e., the ratio of physician to patient talk time) during medical interactions and the relationship between this ratio and patients’ subsequent adherence. We conducted a secondary analysis of self-report and video-recorded data from a prior study of clinical interactions between 112 low-income, Black patients and their 14 non-Black physicians at a primary care clinic in the Midwestern United States between June, 2006 and February, 2008. Overall, physicians talked more than patients; however, both physician bias and patient perceived past discrimination affected physician-patient talk time ratio. Non-Black physicians with higher levels of implicit, but not explicit, racial bias had larger physician-patient talk time ratios than did physicians with lower levels of implicit bias, indicating that physicians with more negative implicit racial attitudes talked more than physicians with less negative racial attitudes. Additionally, Black patients with higher levels of perceived discrimination had smaller physician-patient talk time ratios, indicating that patients with more negative racial attitudes talked more than patients with less negative racial attitudes. Finally, smaller physician-patient talk time ratios were associated with less patient subsequent adherence, indicating that patients who talked more during the racially discordant medical interactions were less likely to adhere subsequently. Theoretical and practical implications of these findings are discussed in the context of factors that affect the dynamics of racially discordant medical interactions.
Keywords: medical interactions, racial bias, perceived past discrimination, talk time, adherence, United States
Introduction
Even though Black patients generally prefer to see Black physicians (Garcia et al., 2003; Saha et al., 2000), approximately 75% of Black patients interact with non-Black physicians (Chen et al., 2005), including White physicians from North America and physicians of various ethnicities trained outside North America (American Medical Association, 2007). The high incidence of Black patients who engage in racially discordant medical interactions has substantial implications for racial healthcare disparities because whether medical interactions are racially concordant or discordant has a direct impact on the quality of healthcare patients receive. There is strong evidence that communication in racially discordant medical interactions is usually less productive and positive in content and tone than in racially concordant interactions. For example, compared to racially concordant medical interactions, racially discordant ones are characterized by less: positive affect (Johnson et al., 2004), relationship building (Siminoff et al., 2006), treatment planning (Oliver et al., 2001), and health information exchange (Eggly et al., 2011; Gordon et al., 2006).
The landmark volume of the Institute of Medicine, “Unequal Treatment” (Smedley et al., 2003), argued that both non-Black physicians’ and Black patients’ racial attitudes are major contributors to racial healthcare disparities. In health disparities literature, physicians’ racial attitudes are typically operationalized as racial bias, whereas patients’ racial attitudes are operationalized as perceptions of or reactions to the experience of racial prejudice and discrimination at both a societal and personal level. Prior research has shown that both physician racial bias and patient perceived past discrimination influence thoughts and feelings about racially discordant medical interactions (Benkert et al., 2006; Penner et al., 2009). For instance, Penner, Dovidio et al. (2010) reported that non-Black physicians’ explicit racial bias affected their reports of how much they involved their Black patients in treatment decisions as well as their perceived communality with their Black patients. Cooper and colleagues (2012) found that greater physician implicit racial bias was negatively associated with patient ratings of interpersonal care. Similarly, Benkert et al. (2006) found that Black patients’ perceptions of experience with racism was negatively associated with patients’ satisfaction with their healthcare provider; this relationship was mediated by trust in that provider. That is, Black patients who perceived racism in their lives trusted their physicians less, which, in turn, led to lower satisfaction.
Although previous studies have demonstrated that both physicians’ and patients’ racial attitudes affect each participant’s perceptions of racially discordant medical interactions, little work has examined how such attitudes simultaneously affect their behavior during such interactions. The present study addresses this issue by examining the impact of racial attitudes on the dynamics and outcomes of racially discordant medical interactions. The dynamics of medical interactions can be assessed in many different ways, but we focus on one specific aspect of physicians’ and patients’ behavior—the amount of talk time during medical interactions—because it has been shown to affect patient health-related attitudes and behaviors (e.g., Epstein & Street, 2007; Hahn, 2009; Roter & Hall, 1993) and health (Kaplan et al., 1989).
As far as we are aware, only one prior study (Cooper et al., 2012) has examined how racial attitudes affect the relative amount physicians and patients talk during medical interactions. In that study, Cooper et al. found that higher physician implicit bias was associated with greater physician verbal dominance, which they defined as a greater number of physician statements relative to patient statements. The present study, which was a secondary analysis of self-report data and video-recordings from a larger study of clinical interactions between low-income Black patients and their non-Black primary care physicians (see Penner et al., 2009), builds on this prior research by Cooper et al. Like Cooper et al., we examined verbal dominance during racially discordant medical interactions. In our study, however, we operationalized verbal dominance as the ratio of time the physician talked relative to time the patient talked (i.e., physician-patient talk time ratio). In research on social interactions, relative and/or absolute talk time is considered a valid measure of participants’ motivation to dominate an interaction (Dovidio et al., 1988; Mast, 2002). We extended Cooper and colleagues’ work in three ways. First, we examined the simultaneous effects of physicians’ implicit and explicit racial bias on physician-patient talk time ratio. Second, we examined the impact of patients’ perceived past discrimination on physician-patient talk time ratio. Third, we examined the association between physician-patient talk time ratio and patients’ subsequent adherence to physician treatment recommendations. The rationale for the study hypotheses follows.
Racial Attitudes, Interaction Goals, and Behaviors
Non-Black Physician Perspective
Racial attitudes can operate at both an explicit and implicit level (see Wilson et al., 2000). At the explicit, or conscious, level, non-Black physicians are more likely to perceive Black patients as less trustworthy, more contentious, and less likely to adhere to their recommendations than White patients (Moskowitz et al., 2011; van Ryn & Burke, 2000). At the implicit, often non-conscious level, physicians display a preference for White over Black patients and are more likely to associate White than Black patients with being compliant and cooperative (Sabin et al., 2008). Thus, biased physicians might be inclined to assume an authoritative role and exert more control during interactions with Black patients.
However, behaviors that might represent bias in healthcare are widely and vigorously condemned within the medical profession (Green et al., 2007). As a result, physicians are likely to attempt to self-regulate these potentially negative behaviors (Shelton et al., 2005; Vorauer & Turpie, 2004). Yet, there is substantial evidence showing that people’s ability to self-regulate the expression of bias in their behaviors depends on how aware they are of their racial bias and how easy or hard the behaviors are to self-regulate (Ferguson, 2007). Specifically, people are better at self-regulating explicit racial bias manifested in more planned behaviors, such as verbal behaviors, than they are at regulating implicit racial bias manifested in more spontaneous behaviors, such as nonverbal and paraverbal behaviors (Dovidio & Gaertner, 2004). Thus, even if non-Black physicians are able to successfully self-regulate negative explicit racial bias manifested in more planned behaviors, their implicit racial bias may still be manifested in spontaneous behaviors that are more difficult to self-regulate (Cooper et al., 2012; Penner, Dovidio et al., 2010).
Black Patient Perspective
One widely held belief among Blacks is that when they interact with non-Blacks, they will be the target of prejudice and/or discrimination (Shelton, 2003; Shelton & Richeson, 2006). As a consequence, Blacks often avoid interracial interactions (Mendoza-Denton et al., 2002; Shelton & Richeson, 2005; 2006). However, some interracial interactions are unavoidable, such as medical interactions. In these situations, Blacks are likely to become more active with the aim of limiting their vulnerability associated with being the target of prejudice (Shelton et al., 2005). Moreover, prior research has shown that Black patients with higher levels of perceived past discrimination are less likely to trust physicians (Benkert et al., 2006; Schuster et al., 2005) and that less trusting patients, regardless of their racial background, tend to play a more active role during medical interactions and are less willing to give physicians treatment decisional control (Trachtenberg et al., 2005). This research thus suggests that Black patients who report higher perceived past discrimination may be more verbally active in their medical interactions with non-Black physicians and perhaps less likely to follow the physicians’ recommendations (see Penner et al., 2009).
Hypotheses
In the present study, we examined the simultaneous effects of physicians’ explicit and implicit racial bias and patients’ perceived past discrimination on the amount of time the physician talked relative to the patient (i.e., physician-patient talk time ratio). We also examined the association between physician-patient talk time ratio and patients’ subsequent adherence to physicians’ treatment recommendations. Our first hypothesis was that non-Black physicians’ implicit, but not explicit, racial bias would predict physician-patient talk time ratio. Specifically, we expected higher physician implicit bias to be associated with larger physician-patient talk time ratios. This is because talk time during an interaction can be considered as spontaneous paraverbal behavior, defined as how we say something, not what we say (Mast & Sczesny, 2010); thus it should be better predicted by implicit racial bias than explicit racial bias (see Dovidio et al., 2009).
Our second hypothesis was that higher perceived past discrimination among Black patients would be associated with smaller physician-patient talk time ratios during medical interactions. This is because we expected that Blacks would try to take a more active role during interactions when they expect to be the target of prejudice or when they do not trust the physicians.
As part of the examination of these hypotheses, we conducted ancillary analyses to better understand any significant relationships between physician and patient racial attitudes and physician-patient talk time ratio. Specifically, we examined whether the primary impact of physician and patient racial attitudes was on their own talk time, that of the other participant in the interaction, or a combination of both.
Finally, we hypothesized an association between physician-patient talk time ratio and patients’ subsequent adherence to treatment recommendations. We did not make a directional prediction because, as we describe below, two different bodies of research suggest different predictions. In the patient-centered care literature, it is generally believed that greater patient talk time is desirable and associated with positive health outcomes, including greater adherence (e.g., Hahn, 2009). This is because greater patient talk time is thought to represent more patient empowerment and more patient involvement in care. Therefore, according to the patient-centered care literature, larger physician-patient talk time ratios (driven by more physician talk time) should be associated with lower patient adherence. However, as discussed earlier, in the social psychology literature on interracial bias, greater talk time by Blacks in racially discordant social interactions is often found to be associated with greater concerns about being discriminated against (Shelton et al., 2005) and a consequent desire to exert personal control. In addition, Black patients’ negative racial attitudes are generally associated with lower adherence (Casagrande et al., 2007; Penner et al., 2009). Thus, according to this literature, smaller physician-patient talk time ratios (driven by more patient talk time) should be associated with lower patients’ subsequent adherence.
Method
Participants
Participants were 112 low-income, self-identified Black patients (76.8% women, Mage = 42.83, SD = 13.86) who participated in clinical interactions with 14 non-Black primary physicians [12 Asians (6 from India/Pakistan, 6 from other parts of Asia), 2 Whites, 50.0% women, Mage = 30.09, SD = 2.74] in an earlier larger study. The high percentage of Asian physicians is relatively common for primary clinics that serve low-income, residentially segregated minority patient populations in the United States (Hing & Lin, 2009; Mertz et al., 2007; Smedley et al., 2003). The patients and physicians included in this study did not differ from the patients or physicians in the parent study (Penner et al., 2009) on any of the demographic or self-report measures.
Procedure
The parent study protocol was approved by Karmanos Cancer Institute (KCI) Protocol Review and Monitoring Committee and Wayne State University (WSU) IRB. The present secondary analysis was approved by the WSU IRB. (The KCI Committee did not deem it necessary to approve a secondary analysis of a study it had already approved). The majority of the physicians approached (83%) agreed to be in the study and did not differ demographically from those who declined. Physicians received a gift card for their participation. Patients were approached by a Black female clinic staff member when they entered the clinic and, if interested in the study, signed an informed consent and HIPAA release form. About 75% of the patients approached agreed to be in the study. Patients received gift cards for participation on the day of the visit and completion of the follow-up questionnaires.
Physicians completed measures of explicit and implicit racial bias shortly after they were consented. Patients completed a baseline questionnaire that included measures of demographic characteristics, adherence to physicians’ recommendations over the past month, and perceived past discrimination. Next, they were video-recorded during their appointment with a physician. Four and 16 weeks later, participants were mailed a follow-up questionnaire about their adherence to the physicians’ treatment recommendations. Of the 112 patients who completed the baseline measure, 80 (71.4%) completed the 4-week follow-up questionnaire and 71 (63.4%) completed the 16-week follow-up questionnaire.
Measures
Physician explicit racial bias
Non-Black physicians’ explicit racial bias toward Blacks was assessed with 25 items taken from Brigham’s (1993) Attitudes toward Blacks Scale and McConahay’s (1986) Modern Racism Scale (α = .89). Higher numbers indicate higher explicit racial bias toward Blacks.
Physician implicit racial bias
The computer-based race Implicit Association Test (IAT; Greenwald et al., 1998) was used to assess non-Black physicians’ implicit racial bias toward Blacks. IAT responses were scored with procedures recommended by Greenwald, Nosek, and Banaji (2003), producing a D measure. Higher numbers indicate more implicit pro-White bias and thus greater negative bias toward Blacks.
Patient perceived past discrimination
Perceived past discrimination was assessed using Brown’s (2001) measure of “Self-perceived racial and ethnic discrimination.” Participants were first asked whether they had ever experienced unfair treatment in each of seven social domains: jobs, education, medical treatments, job applications, police encounters, housing, and dealing with neighbors. The majority of patients (56.4%) reported they had experienced discrimination in the past at least in one domain. The internal consistency for this seven item “yes/no” scale was relatively high (odd-even reliability with Spearman-Brown correction = .74); thus, we computed the sum of “yes (1)/no (0)” responses across the seven items. Higher numbers indicate higher perceived past discrimination.
Physician-patient talk time ratio
Using video recordings of the interactions, one coder recorded how many seconds the physician and patient each talked during a given interaction using Noldus Observer® software. Then, physician-patient talk time ratio was computed by dividing physicians’ talk time by patients’ talk time. Because patients’ talk time was the denominator, values above 1 indicate that the physician talked more than the patient; the larger the ratio, the more the physician talked relative to the patient. The mean ratio score was 1.99 (SD = 1.24), indicating that overall physicians talked more than their patients, which is typical of most medical interactions. The ratio provides one way to normalize for total time of the interaction. Because physician-patient talk time ratio was positively skewed [skewness = 2.19, SE = .22; kurtosis = 6.27, SE = .44; Shapiro-Wilk(120) = .80, p < .001], a log-transformation was used to normalize the distribution [skewness = .08, SE = .22; kurtosis = .65, SE = .44; Shapiro-Wilk(120) = .99, p = .59]. Although the log-transformed physician-patient talk time ratio was used in our statistical analyses, in the interest of clarity, means and standard deviations are presented using the raw physician-patient talk time ratio.
Patient adherence to physicians’ treatment recommendations
(Baseline, four and 16 weeks after the interactions). Three positively worded items from the 5-item adherence subscale from the RAND Health’s Medical Outcomes Study (Hays et al., 1994) were used to assess Black participants’ past general adherence (i.e., baseline, α = .74) and adherence to the recommendations of the physicians whom they saw in this study (both four and 16 weeks α’s =.75). Higher numbers indicate higher adherence to medical recommendations.
Trust in one’s own physician
The parent study was divided into two phases of data collection. In the second phase of the study, a measure of patient trust was added, and patients were asked to complete it immediately after the interaction. Specifically, two items from Dugan, Trachtenberg, and Hall’s (2005) “Interpersonal Trust in a Physician” short form scale were used to assess patients’ trust in the physician they had just seen. The items were: “I completely trust this doctor’s decisions about which medical treatments are best,” and “All in all, I have complete trust in this doctor.” The correlation between the two items was .71, so they were combined into a single average score. The scale ranged from 1 (Strongly Disagree) to 6 (Strongly Agree). Trust data were available only for 58 of the patients in this study. As would be expected, patient trust was significantly negatively correlated with perceived past discrimination, r(57) =−.38, p = .004. As will be discussed shortly, the measure of trust was used to further explicate the relationship between their attitudes and talk time.
Analysis Overview
Racial Attitudes and Physician-Patient Talk Time Ratio
Main analyses
The preliminary set of analyses was product moment correlations among racial attitudes and the physician-patient talk time ratio. However, because patients were nested within physicians, the primary form of analysis was multiple regressions using General Estimating Equations (GEE). GEE is a form of multilevel modeling, which treats group-level variation (in this case, physicians) as a nuisance parameter and provides consistent and asymptotically normal estimates regardless of how strongly observations within groups are correlated with one another (Hardin & Hilbe, 2003). For the analysis predicting physician-patient talk time ratio, we conducted three separate GEE regressions with each of the three racial attitudes measures (i.e., physician explicit racial bias, physician implicit racial bias, and patient perceived past discrimination) as a predictor. In these and all other GEE regressions predictor variables were grand-mean-centered before being entered into the model.
The GEE regression of patient perceived past discrimination predicting physician-patient talk time ratio was further followed-up with two additional GEE regression analyses because a preliminary analysis revealed that Black patients’ perceived past discrimination had a zero-inflated Poisson distribution (ZIP), which consists of two parts: “binary” and “count” (Cameron & Trevedi, 1998). In this instance, the binary part indicates whether patients reported ever having experienced any discrimination in the past (yes versus no), whereas the count part indicates in how many different social domains they report experiencing discrimination. Currently, there are no statistical programs for the analysis of regression models with ZIP predictor variables. Therefore, we ran separate GEE regressions to decompose the binary and count parts of the ZIP distribution when examining the association between patient perceived past discrimination and physician-patient talk time ratio. For the binary part, patients’ perceived past discrimination was re-coded as any/no report of past discrimination (a presence effect), and for the count part, patients’ perceived past discrimination was re-coded as frequency of past discrimination excluding patients who reported no past discrimination (a magnitude effect). They were, then, entered into GEE regressions separately as a predictor of physician-patient talk time ratio.
Ancillary analyses
In addition to the primary analyses to test the main hypotheses, we also conducted three sets of ancillary analyses to further explore the nature of the effects of racial attitudes on physician-patient talk time ratio. The first set of analyses was intended to determine if the primary impact of each participant’s racial attitudes was on their own talk time, the talk time of the other person, or a combination of both. This required two additional GEE regressions. In one, physician raw talk time was regressed onto physician implicit bias and patient perceived past discrimination; in the other, patient raw talk time was regressed onto the same two measures.
The second set of ancillary analyses examined the relation between the two components of the talk time ratio (i.e., the physician talk time, which is the numerator in talk time ratio, and the patient talk time, which is the denominator of the talk time ratio). To do this, we conducted another GEE regression in which we regressed patient raw talk time on physician raw talk time, controlling for the amount of time patients and physicians were in a room together. This analysis not only clarifies the relation of the two variables that form physician-patient talk time ratio, but also provides insight into the dynamics of the interaction as assessed by talk time of the individuals.
Finally, we conducted a set of ancillary analyses to explore a potential mechanism through which patient perceived past discrimination affects the physician-patient talk time ratio. In the introduction, we speculated that if a relationship between patient perceived past discrimination and physician-patient talk time ratio was found, it would at least partially be explained by the impact of patient trust on this ratio. Using the trust data from patients in the second phase of the study, we conducted two GEE regressions. In the first GEE regression, we regressed patient trust on perceived past discrimination; in the second GEE regression, we regressed physician-patient talk time ratio on patient trust. We also conducted a follow-up mediation analysis to examine the indirect effects of patients’ perceived past discrimination on physician-patient talk time ratio through patient trust, using Hayes’ (2012) bootstrapping method with n = 5000 samples.
Physician Patient Talk-Time Ratio and Adherence
We used product moment correlations and GEE regressions to examine the relationship between physician-patient talk time ratio and patient adherence at the 4 and 16 week follow-ups. We then conducted two separate GEE regressions. In the first, we regressed adherence at the 4-week follow-up on physician-patient talk time ratio, controlling for the baseline general adherence, physician implicit racial bias, and patient perceived past discrimination. In the second, we used the same variables to predict adherence at the 16-week follow-up.
Results
Table 1 presents means, standard deviations, and correlations for all measured variables. Examinations of means indicate that, on average, physicians showed a slight preference for Blacks relative to Whites on their implicit racial attitudes, but size of this difference was not statistically different from 0, t(13) = −0.99, p = .34. Implicit racial bias was positively correlated with explicit racial bias, r(14) = .06, p = .02. Patient past adherence (measured at baseline) was significantly correlated with adherence at the 4- and 16-week follow-ups, r(78) = .58, p < .001 and r(68) = .46, p < .001, respectively. Thus, as already noted, baseline adherence was controlled in the analyses of follow-up adherence.
Table 1.
Means, standard deviations, and Pearson correlations among all measured variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Physician Explicit Racial Bias | -- | |||||||
| 2. Physician Implicit Racial Bias | .60* (14) | -- | ||||||
| 3. Patient Perceived Past Discrimination | .12 (110) | .07 (110) | -- | |||||
| 4. Physician-Patient Talk Time Ratio | .05 (106) | .32** (106) | −.20* (105) | -- | ||||
| 5. Adherence at 4-Week Follow-Up | .04 (80) | .11 (80) | −.23* (80) | .29* (77) | -- | |||
| 6. Adherence at 16-Week Follow-Up | −.06 (71) | .12 (71) | −.23† (70) | .33** (69) | .64** (63) | -- | ||
| 7. Baseline Adherence | −.11 (106) | .03 (106) | −.32** (105) | .25* (101) | .58** (78) | .46** (68) | -- | |
| 8. Trust in One’s Own Physician | −.06 (58) | .03 (58) | −.38** (57) | .32* (56) | .20 (38) | .25 (32) | .58** (58) | -- |
|
| ||||||||
| M | 2.05 | −.10 | 1.29 | 1.99 | 4.55 | 4.58 | 4.55 | 5.51 |
| SD | .40 | .36 | 1.53 | 1.24 | 1.21 | 1.12 | 1.12 | .71 |
Note.
indicates p = .051,
indicates p < .05, and
indicates p < .01.
Values in parentheses are numbers of cases on which the correlations were based. As noted, the trust measure was introduced about halfway through the data collection.
Racial Attitudes and Physician-Patient Talk Time Ratio
Main analyses
Initially, we tested the first two hypotheses by computing product-moment correlations. As shown in Table 1, physician explicit racial bias did not predict the physician-patient talk time ratio. However, as we predicted, physician implicit racial bias was significantly and positively associated with physician-patient talk time ratio during the interactions. Turning to the second hypothesis, as also predicted, patients’ perceived past discrimination was significantly and negatively correlated with physician-patient talk time ratio.
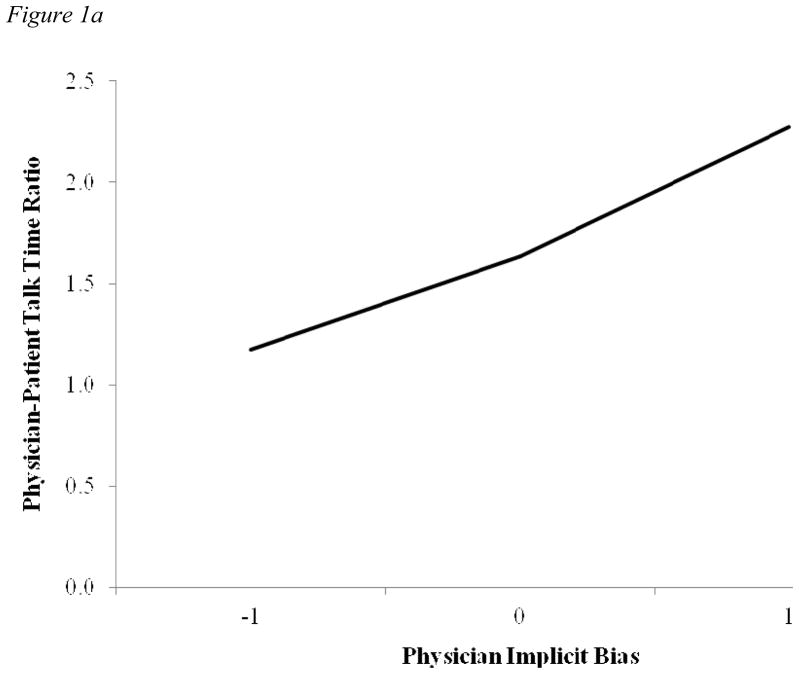
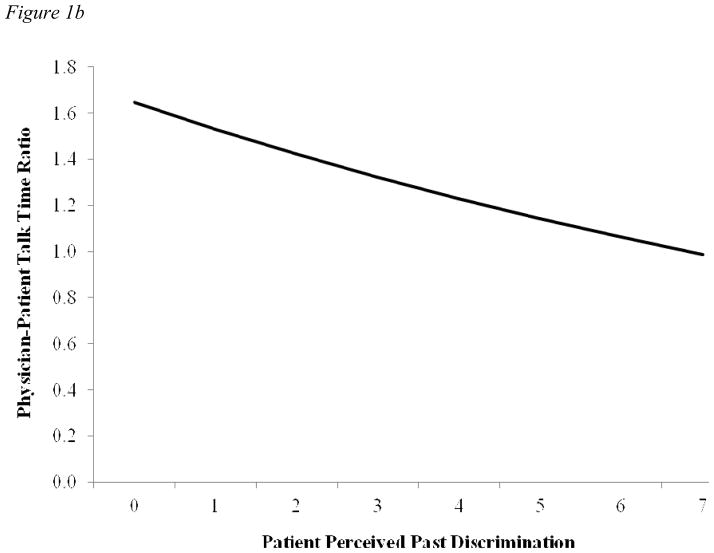
These product-moment correlations provide preliminary support for the first two hypotheses. These correlations do not, however, provide a strong test of the first two hypotheses because they do not take into account the nesting of patients within physicians and produce biased estimates. A stronger test of these hypotheses is given by the GEE regressions. Consistent with the correlation, the first GEE regression analysis revealed that there was no association between physician explicit racial bias and physician-patient talk time ratio, b = .04, SE = .14, Wald χ2(1) = .10,p = .78. The second analysis showed that there was a marginally significant, positive relationship between physician implicit racial bias and physician-patient talk time ratio, b = .33, SE = .19, Wald χ2(1) = 3.09,p = .08 (Figure 1a), which is consistent with the findings from the product-moment correlations. It should be noted that one possible reason why the GEE regression indicated a somewhat weaker association between physicians’ implicit racial bias and physician-patient talk time ratio than the correlation may have been the small number of the upper-level cases (i.e., physician sample size, n = 14). Finally, the third GEE regression showed that higher levels of patients’ perceived past discrimination were significantly associated with smaller physician-patient talk time ratios, b = −.07, SE = .03, Wald χ2(1) = 4.52,p = .03 (Figure 1b), which was consistent with the findings from the product-moment correlations.
Figure 1.
Figure 1a. Effects of physician implicit racial bias on physician-patient talk time ratio
Figure 1b. Effects of patient perceived past discrimination on physician-patient talk time ratio
However, as already noted, patients’ perceived past discrimination score had a ZIP distribution. Thus, we decomposed the effects of patients’ perceived past discrimination into the binary (i.e., the presence effect) and the count parts (i.e., the magnitude effect) and assessed the impacts of these effects on physician-patient talk time ratio. The presence effect on physician-patient talk time ratio was marginally significant, b = −.11, SE = .06, Wald Χ2(1) = 3.50, p = .06, whereas the magnitude effect on physician-patient talk time ratio was significant, b = −.09, SE = .04, Wald χ2(1) = 4.94, p = .03. Given the proximity to α = .05 cutoff for the binary model, we cannot completely rule out the presence effect. Thus, the effects of perceived past discrimination on physician-patient talk time ratio may have been driven by both the presence (i.e., whether or not patients reported experiencing discrimination in the past) and the magnitude effect (i.e., the amount of discrimination patients reported).
Ancillary analyses
The physician-patient talk time ratio, per se, does not tell us how physician and patient racial attitudes affected the individuals’ talk time. For example, the positive association between physician implicit bias and physician-patient talk time ratio may be due to one of three processes: (1) physicians with higher implicit racial bias talked more than physicians with lower implicit bias; (2) patients who interacted with physicians with higher implicit racial bias talked less than patients who interacted with physicians with lower implicit racial bias; or (3) a combination of both increased physician talk time and decreased patient talk time. In the same vein, the negative association between patient perceived discrimination and physician-patient talk time ratio may be due to one of three parallel processes: (1) patients with higher perceived past discrimination talked more than patients with lower perceived past discrimination; (2) physicians who interacted with patients with higher perceived past discrimination talked less than physicians who interacted with patients with lower perceived past discrimination; or (3) a combination of both increased patient talk time and decreased physician talk time.
The ancillary analyses were intended to further explicate the impact of racial attitudes on patients’ and physicians’ talk time. In the first analysis, we assessed whether the primary impact of each participant’s racial attitudes was on their own talk time, that of the other person, or a combination of both. The first GEE regression analysis revealed that physician implicit bias was significantly associated with their own raw talk time, b = 163.97, SE = 76.39, Wald χ2(1) = 4.61, p = .03, but not with patient raw talk time, b = 11.90, SE = 70.20, Wald χ2(1) = .03, p = .87. In the second GEE regression analysis, there was also a marginally significant association between patient perceived past discrimination and their own raw talk time, b = 17.72, SE = 9.37, Wald χ2 (1) = 3.58, p = .06, but not physician raw talk time, b = −6.51, SE = 12.69, Wald χ2 (1) = .26, p = .61. These ancillary analyses tentatively suggest the impact of each participant’s racial attitudes may have primarily been on their own talk time. Specifically, these results suggest that the positive association between physician implicit bias and physician-patient talk time ratio reflects greater talk time among physicians with higher implicit racial bias than physicians with lower implicit racial bias. Likewise, the negative association between patient perceived past discrimination and the physician-patient talk time ratio reflects greater talk time among patients with higher perceived past discrimination than patients with lower perceived past discrimination.
The second ancillary analysis addressed the relationship between physician talk time and patient talk time—did patients actually talk more as physicians talked less, or were changes in physician and patient talk time basically independent of one another? The GEE regression revealed a significant negative association between the two raw talk times, b = −.34, SE = .11, Wald χ2(1) = 9.26, p = .002. These findings suggest that changes in physician-patient talk time ratio reflect changes in both physician talk time and patient talk time and that the dynamics of these racially discordant medical interactions were jointly determined by both the physicians and patients.
Finally, we explored whether the association between patient perceived past discrimination and physician-patient talk time ratio would at least partially be explained by the impact of patient trust on physician-patient talk time ratio. As already noted there was a significant negative correlation between perceived past discrimination and trust (see Table 1). A GEE regression produced the same significant negative relationship, b = −.16, SE = .07, Wald χ2(1) = 5.83, p = .02. More germane to the present issue, the more Black patients trusted their physicians, the larger the physician-patient talk time ratios, b =.18, SE = .07, Wald χ2(1) = 5.83, p = .02. That is, in interactions where Black patients expressed more trust in physicians, physicians talked more relative to their patients. The follow-up mediation analysis revealed that the full model, in which trust in physicians mediates the effects of patient perceived past discrimination on physician-patient talk time ratio, was significant, R2 = .14, F (2, 52) = 4.28, p = .02. Specifically, when trust was included in the model in addition to perceived past discrimination, the previously significant direct effect of perceived past discrimination on physician-patient talk time ratio became non-significant (p = .47), but the indirect effect of trust was significant, b = .22, SE =.09, p = .02., 95% CI = −.116 ~ −.001. Thus, trust significantly mediated the effects of patients’ perceived past discrimination on physician-patient talk time ratio.
Physician Patient Talk-Time Ratio and Adherence
The product-moment correlations between physician-patient talk time ratio and adherence to treatment recommendations at 4-weeks and between talk time ratio and adherence at 16-weeks were both significant and positive (see Table 1). Since larger physician-patient talk time ratios reflect more physician talk time relative to patient talk time, the positive relationship means that the more physicians talked, the more patients adhered. As a stronger test of these relationships, we conducted GEE regressions (with the baseline adherence, physician implicit racial bias, and patient perceived discrimination as covariates). The first GEE regression analysis failed to find a significant association between physician-patient talk time ratio and patient adherence at 4-weeks., b = 20, SE = .19, Wald χ2(1) = 1.08, p = .30. However, the second GEE regression found a significant positive association between physician-patient talk time ratio and patients’ adherence at 16-weeks follow-up (Table 2).
Table 2.
Effects of physician-patient talk time ratio during the interactions on patients’ adherence 16 weeks after the interaction
| b | SE | χ2 | df | |
|---|---|---|---|---|
| Intercept | 4.45 | .05 | ||
| Baseline Adherence | .41 | .13 | 10.53*** | 1 |
| Physician Implicit Racial Bias | −.18 | .26 | .47 | 1 |
| Patient Perceived Past Discrimination | −.10 | .09 | 1.17 | 1 |
| Physician-Patient Talk Time Ratio | .50 | .20 | 5.99* | 1 |
Note. Patients’ baseline adherence, physicians’ implicit racial bias, and patients’ perceived past discrimination were entered as covariates.
indicates p < .05, and
indicates p < .01.
Discussion
The IOM report, “Unequal Treatment” (Smedley et al., 2003), argued that racial attitudes can affect the dynamics of racially discordant medical interactions and these dynamics play a critical role in racial healthcare disparities. The present study investigated how both physicians’ and patients’ racial attitudes can jointly shape the dynamics of racially discordant medical interactions, and in turn, affect patients’ subsequent health behaviors.
Among non-Black physicians, more negative implicit, but not explicit, racial bias was associated with larger physician-patient talk time ratios. The ancillary analysis further showed that physician implicit racial bias significantly affected their own talk time, but not patient talk time. These findings indicate that physicians with more negative implicit racial attitudes talked more during racially discordant medical interactions, as compared to physicians with less negative implicit racial attitudes. Thus, we replicated the Cooper et al.’s (2012) findings about the role of physician implicit bias in racially discordant medical interactions, even though we used a somewhat different operationalization of verbal dominance (i.e., the amount of talk time as opposed to the number of utterances) and our sample of physicians was demographically rather different from Cooper et al.’s (for example, their sample of non-Black physicians was 52% White, 48% Asian, and 13.4 years post residency, on average; our sample was primarily Asian physicians in their residency).
The current findings provide further insights into the nature of the effects of racial attitudes on the dynamics of racially discordant medical interactions. Specifically, our findings suggest that more subtle, but important aspects of the dynamics of racially discordant medical interactions may not be affected by physicians’ explicit or conscious racial attitudes, but may be affected by physicians’ implicit racial attitudes. This suggests programs that address physicians’ explicit racial attitudes may not be effective in reducing healthcare disparities in racially discordant medical interactions; rather, the programs also need to employ innovative strategies (e.g., Devine et al., 2002) that target implicit or automatic reactions to Black patients.
Additionally, patients’ racial attitudes also seem to affect the dynamics of racially discordant medical interactions. Among Black patients in this study, higher perceived past discrimination was associated with smaller physician-patient talk time ratios. Furthermore, the ancillary analysis showed that the effects of patient perceived past discrimination was primarily on their own talk time and not on physician talk time. Thus, these findings suggest that patients with more negative racial attitudes talked more during racially discordant medical interactions than patients with less negative racial attitudes. It is important to note that physicians usually talk more in medical interactions than patients, and this was true in this study as well. This may be possibly due to the power differential between physicians and patients in medical interactions. However, our findings suggest that patients’ and physicians’ racial attitudes can (and do) jointly affect the physician-patient talk time ratio. More specifically, the first set of ancillary analyses suggests that physicians’ implicit racial bias affected how much they talked and that patients’ perceived past discrimination affected how much they talked. The second ancillary analysis suggests that physician and patient racial attitudes jointly determine the relative amount of time each party talks.
The study also investigated whether the dynamics of racially discordant medical interactions were associated with patients’ subsequent adherence to the physicians’ treatment recommendations. At four weeks after the interactions, we found somewhat weak evidence that the smaller physician-patient talk time ratio, the less patients adhered to the physicians’ medical recommendations. However, there was much stronger evidence of this relationship at 16 weeks after the interactions. That is, Black patients who talked more during racially discordant medical interactions were less likely to adhere to their physicians’ recommendations subsequently than Black patients who talked less.
The null findings at four weeks were not expected. We can offer two post hoc explanations. First, the 4-week follow-up analysis was based on a somewhat larger sample and thus had somewhat more power. However, the baseline adherence measure, which was used as a covariate in the GEE regressions, was much closer in time to the 4-week follow-up measure of adherence than to that of the 16-week follow-up. It is thus possible that inclusion of the baseline adherence as a covariate in the GEE regressions might have resulted in much more variance in the adherence assessed four weeks after the interactions being explained by this variable than in the adherence assessed 16 weeks after the interactions. This could have served to reduce the variance in 4-week follow-up adherence that could be explained by other predictors in the equation, including the physician-patient talk time ratio. A second, more theoretical, explanation is that perhaps the psychological impact of the racially discordant medical interactions on patient adherence may be a delayed rather than an immediate one. For example, because of norms and social pressure, patients may initially try to adhere to physicians’ recommendations, regardless of the quality of the medical interactions the patients experienced. However, as the explicit pressure to adhere decreases over time, experiencing more negative medical interactions may erode patients’ motivations to adhere to the physician’s recommendations, resulting in a wider difference in the levels of adherence as a function of the original dynamics of the medical interaction.
These post hoc explanations can be more directly tested in future research. However, neither of them negates the finding of a significant association between physician-patient talk time ratio and patient adherence 16 weeks after the interactions, even when baseline adherence was controlled. This finding seems to indicate that greater patient talk time may not reflect positive patient reactions to patient-centered interactions, as the literature on patient-centered care would suggest (Hahn, 2009). Rather, greater patient talk time was associated with both high levels of perceived past discrimination and low levels of trust. This pattern of relationships suggests that Black patients may talk more in racially discordant medical interactions not necessarily because they feel respected or empowered by physicians, but because they fear they may be the victims of discrimination and have less trust of their physicians. Therefore, how much Black patients talk in racially discordant medical interactions may, at least in part, represent their own attempts to actively control interactions in order to avoid being the target of prejudice and poor medical care. We speculate that Black patients who reported more perceived past discrimination (or less trust) might have had stronger expectations that they would be mistreated by non-Black physicians in general. This mistrust in non-Black physicians, in turn, might have led them to talk more in an attempt to prevent such treatment, and also to less subsequent adherence to physician recommendations.
At first glance, these findings seem inconsistent with a patient-centered perspective on the meaning of patient talk time (Epstein & Street, 2007). Patient-centeredness is a valid and desired goal for all medical interactions, but the behaviors associated with patient-centeredness may differ between racially concordant and racially discordant medical interactions. As West, Shelton, and Trail (2009) have shown, sometimes exactly the same behaviors may be viewed in different, frequently opposite, ways in same-race interactions and different-race interactions. Thus, our research further highlights the importance of recognizing and understanding how the distinctive dynamics of racially concordant and discordant interactions can affect medical encounters and outcomes.
Limitations and Future Research
This study was a secondary data analysis, and we were limited by the information available in data already collected. Thus, we were unable to directly measure the actual interaction goals of either the physicians or the patients or other motives that might explain why racial attitudes predicted the physician-patient talk time ratio. Future studies should directly examine actual interaction goals of non-Black physicians and Black patients and their association with their race-related perceptions and feelings.
Next, this study focused only on how racial attitudes affected physician-patient talk time ratio, but of course racial attitudes were not the sole determinants of how much physicians and patients talked during the interactions or how much patients adhered to physicians’ recommendations. For example, one other likely determinant is the reason for patients’ visit to the doctor. Patients who present complex health problems during the visit may have to provide more explanation, which may affect how much their physicians talk. Complicated health problems may also lead to complicated treatment recommendations, which will affect patients’ ability or willingness to adhere to them. Likewise, patients’ prior relationship with physicians may also influence both parties’ talk time and patients’ adherence to treatment recommendations. It was not possible to systematically measure any of these other potential factors on the primary outcomes, but it seems quite reasonable to posit that talk time and adherence are determined by multiple factors in addition to racial attitudes. Although we expect these factors to be randomly distributed with respect to physicians and patients, future research should use both quantitative and qualitative approaches to explore other potential influences on talk time and adherence and attempt to determine the relative portions of variance in patients’ behaviors that are explained by racial attitudes and by other variables.
In addition, the sample size of the current study was small (physician n = 14, patient n = 112), which did not allow us to model any effects of physician characteristics (e.g., the impact of physician race/ethnicity). Also, some of the significant associations we found for the correlations were not statistically significant for the GEE regressions, which correct for biased error estimates by taking into account non-independence of patients within each physician. Future research would benefit from a larger sample of physicians and patients, as well as from examining these processes in a range of different kinds of healthcare settings. However, it should be noted that the results of the present study are consistent with Cooper et al.’s (2012) findings, suggesting that the effects of racial attitudes on physician-patient talk time ratio we found in this study are stable and replicable findings. Further, the different findings for the impact of physician explicit racial attitudes and physician implicit racial attitudes on physician talk time are also consistent with a large literature on how these two kinds of bias affect controlled versus spontaneous behaviors (Dovidio et al., 2009). Finally, the impact of patient racial attitudes on patient talk time was significant for both through perceived past discrimination and trust, which is consistent with the prior literature on how these attitudes affect Black patients’ reactions to racially discordant medical interactions (Benkert et al., 2006; Penner et al., 2009).
In addition to these limitations, there are also several caveats. First, while our findings highlight the important role of physician-patient talk time ratio in the dynamics of racially discordant medical interactions, it is still unclear why physicians and patients talked more when they harbored negative racial attitudes. For example, were physicians with more negative implicit racial bias talking more because they are trying to be more authoritative and giving instructions to patients on what to do? Were patients with higher perceived discrimination talking more because they were telling physicians what they want for their treatment? In order to address these important conceptual questions, future studies should utilize theory-generating qualitative methods, such as content analysis and conversation analysis, to explore aspects of the interactions that exhibit larger or smaller physician-patient talk time ratios.
The second caveat is that physician-patient talk time ratio represents only one aspect of the richness of racially discordant medical interactions. There are a number of other measures of the dynamics of medical interactions that might be employed (see Mead & Bower, 2000; Roter & Larson, 2002). Future research might thus consider assessing other physicians’ and patients’ verbal, nonverbal, and paraverbal behaviors using audio and video-recordings of racially discordant medical interactions.
Finally, the racial/ethnic distribution of the physicians in our sample—12 out of 14 physicians were Asian--was highly skewed. As already discussed, this is not unusual for clinics in low-income, residentially segregated communities in the United States (Hing & Lin, 2009; Mertz et al., 2007; Smedley et al., 2003). However, Black patients are also quite likely to interact with White physicians (Strumpf, 2011; Traylor et al., 2010). Thus, it is important to empirically examine whether the dynamics of medical interactions between Black patients and Asian physicians would be same as or different from those between Black patients and White physicians. The present study could not address this issue due to the limited physician sample size. Cooper et al. (2012) examined the potential moderating effects of physician race on the physician implicit racial bias-communication link and found that the associations of implicit bias with most communication measures were similar regardless of physician race. However, their physician sample was also relatively small (19 White physicians and 12 Asian physicians); therefore, it is still unclear whether the null findings reflects the actual effects of physician race/ethnicity or are simply due to low statistical power. To our knowledge, no study to date has been conducted to primarily investigate the difference in the quality of these two types of racially discordant interactions. Future studies should investigate this important question by directly comparing the quality of Black patient-Asian physician interactions to Black patient-White physician interactions.
These limitations and caveats not withstanding, we believe that the current findings have several important implications for health disparity research. First and foremost, this study provides more support for the importance of physician and patient racial attitudes in the outcomes of racially discordant medical interactions, as has been argued by the IOM panel (Smedley et al., 2003) and others (e.g., Penner, Albrecht, et al., 2010).
Second, our findings suggest that future studies of patient-physician interactions in racially discordant dyads have to go beyond simply documenting how they differ from racially concordant ones. Using both qualitative and quantitative methodologies, researchers need to study the attitudes and motives of each of the participants and how they affect communication between them. Understanding such feelings and cognitions should lead to interventions that could meaningfully address healthcare disparities. Obviously, we are not suggesting that such interventions focus on getting minority patients to speak less during racially discordant medical interactions. However, we do believe that researchers must give strong considerations to the role of racial attitudes when designing effective interventions to reduce healthcare disparities.
Acknowledgments
We thank Amy Peterson for her thoughtful comments on an earlier draft. This research was supported in part by an NINR grant (1R03NR013249-01) to the first author, an NICHD grant (1R21HD050445001A1) to the second author, and an NCI grant (U54CA153606) to the last author and services conducted by the Behavioral and Field Research Core, supported in part by NCI center grant (P30CA22453) to the Karmanos Cancer Institute, Wayne State University School of Medicine.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Medical Association. IMGs by country of origin. 2007 Retrieved from http://www.ama-assn.org/ama/pub/about-ama/our-people/member-groups-sections/international-medical-graduates/imgs-in-united-states/imgs-country-origin.page.
- Benkert R, Peters RM, Clark R, Keves-Foster K. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. Journal of the National Medical Association. 2006;98(9):1532–1540. [PMC free article] [PubMed] [Google Scholar]
- Brigham JC. College students’ racial attitudes. Journal of Applied Social Psychology. 1993;23(23):1933–1967. [Google Scholar]
- Brown TS. Measuring self-perceived racial and ethnic discrimination in social surveys. Sociological Spectrum. 2001;21(3):377–391. [Google Scholar]
- Cameron AC, Trevedi PK. Regression Analysis of Count Data. New York, NY: Cambridge University Press; 1998. [Google Scholar]
- Casagrande SS, Gary TL, LaVeist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. Journal of General Internal Medicine. 2007;22(3):389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen FM, Fryer GE, Jr, Phillips RL, Jr, Wilson E, Pathman DE. Patients’ beliefs about racism, preferences for physician race, and satisfaction with care. Annals of Family Medicine. 2005;3(2):138–143. doi: 10.1370/afm.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper LA, Roter DL, Carson KA, Beach MC, Sabin JA, Greenwald AG, Inui TS. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. American Journal of Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine PG, Plant EA, Amodio DM, Harmon-Jones E, Vance SL. The regulation of explicit and implicit race bias: The role of motivations to respond without prejudice. Journal of Personality and Social Psychology. 2002;82(5):835–848. [PubMed] [Google Scholar]
- Dovidio JF, Brown CE, Heltman K, Ellyson SL, Keating CF. Power displays between women and men in discussions of gender-linked tasks: A multichannel study. Journal of Personality and Social Psychology. 1988;55(4):580–587. doi: 10.1037//0022-3514.54.2.233. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Gaertner SL. Aversive racism. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 36. San Diego, CA: Academic Press; 2004. pp. 1–51. [Google Scholar]
- Dovidio JF, Kawakami K, Smoak N, Gaertner SL. The roles of implicit and explicit processes in contemporary prejudice. In: Petty RE, Fazio RH, Brinol P, editors. Attitudes: Insights from the new implicit measures. New York: Psychology Press; 2009. pp. 165–192. [Google Scholar]
- Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Services Research. 2005;5(64) doi: 10.1186/1472-6963-5-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eggly S, Harper FW, Penner LA, Gleason MJ, Foster T, Albrecht TL. Variation in question asking during cancer clinical interactions: A potential source of disparities in access to information. Patient Education and Counseling. 2011;82(1):63–68. doi: 10.1016/j.pec.2010.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein RM, Street RL., Jr . NIH Publication No 07-6225. National Cancer Institute; Bethesda, MD: U.S. Government Printing Office; 2007. Patient-centered communication in cancer care: Promoting healing and reducing suffering. [Google Scholar]
- Ferguson MJ. On the automatic evaluation of end-states. Journal of Personality and Social Psychology. 2007;92(4):596–611. doi: 10.1037/0022-3514.92.4.596. [DOI] [PubMed] [Google Scholar]
- Garcia JA, Paterniti DA, Romano PS, Kravitz RL. Patient preferences for physician characteristics in university-based primary care clinics. Ethnicity & Disease. 2003;13(2):259–267. [PubMed] [Google Scholar]
- Gordon HS, Street RL, Jr, Sharf BF, Kelly PA, Souchek J. Racial differences in trust and kung cancer patients’ perceptions of physician communication. Journal of Clinical Oncology. 2006;24(6):904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. The presence of implicit bias in physicians and its predictions of thrombolysis for Black and White patients. Journal of General Internal Medicine. 2008;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The implicit association test. Journal of Personality and Social Psychology. 1998;74(6):1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85(2):197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Hahn S. Patient-centered communication to assess and enhance patient adherence to glaucoma medication. Opthalmology. 2009;116(11 Suppl):S37–S42. doi: 10.1016/j.ophtha.2009.06.023. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized estimating equations. Boca Raton, FL: Chapman & Hall/CRC; 2003. [Google Scholar]
- Hayes AF. PROCESS [computer software] 2012 Available from http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html.
- Hays RD, Kravitz RL, Mazel RM, Sherbourne CD, DiMatteo MR, Rogers WH, Greenfield S. The impact of patient adherence on health outcomes for patients with chronic disease in the Medical Outcomes Study. Journal of Behavioral Medicine. 1994;17(4):347–360. doi: 10.1007/BF01858007. [DOI] [PubMed] [Google Scholar]
- Hing E, Lin S. Role of international medical graduates providing office-based medical care: United States, 2005–2006. NCHS Data Brief. 2009;13:1–8. [PubMed] [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient–physician communication during medical visits. American Journal of Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Medical Care. 1989;27(3 Suppl):S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- Mast MS. Dominance as expressed and inferred through speaking time. Human Communication Research. 2002;28:420–450. [Google Scholar]
- Mast MS, Sczesny S. Gender, power, and nonverbal behavior. In: Chrisler JC, McCreary DR, editors. Handbook of gender research in psychology. New York, NY: Springer; 2010. pp. 411–425. [Google Scholar]
- McConahay JB. Modern racism, ambivalence, and the Modern Racism Scale. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. Orlando, FL: Academic Press; 1986. pp. 99–125. [Google Scholar]
- Mead N, Bower P. Measuring patient-centeredness: A comparison of three observation-based instruments. Patient Education and Counseling. 2000;39(1):71–80. doi: 10.1016/s0738-3991(99)00092-0. [DOI] [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: Implications for African American students’ college experience. Journal of Personality and Social Psychology. 2002;83(4):896–918. doi: 10.1037//0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Mertz E, Jain R, Breckler J, Chen E, Grumback K. Foreign versus domestic education of physicians for the United States: A case study of physicians of south Asian ethnicity in California. Journal of Health Care for the Poor and Underserved. 2007;18(4):984–993. doi: 10.1353/hpu.2007.0100. [DOI] [PubMed] [Google Scholar]
- Moskowitz D, Thom DH, Guzman D, Penko J, Miaskowski C, Kushel M. Is primary care providers’ trust in socially marginalized patients affected by race? Journal of General Internal Medicine. 2011;26(8):846–851. doi: 10.1007/s11606-011-1672-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliver MN, Goodwin MA, Gotler RS, Gregory PM, Stange KC. Time use in clinical encounters: are African-American patients treated differently? Journal of the National Medicical Association. 2001;93(10):380–385. [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Albrecht TL, Orom H, Coleman DK, Underwood W., III . Health and health care disparities. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The sage handbook of prejudice, stereotyping and discrimination. Thousand Oaks, CA: Sage Publication Inc; 2010. pp. 472–490. [Google Scholar]
- Penner LA, Dovidio JF, Edmondson D, Dailey RK, Markova T, Albrecht TL, Gaertner SL. The experience of discrimination and Black-White health disparities in medical care. Journal of Black Psychology. 2009;35(2):180–203. doi: 10.1177/0095798409333585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penner LA, Dovidio JF, West TV, Gaertner SL, Albrecht TL, Dailey RK, Markova T. Aversive racism and medical interactions with Black patients: A field study. Journal of Experimental Social Psychology. 2010;46(2):436–440. doi: 10.1016/j.jesp.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roter DL, Hall JA. Doctors talking to patients/patients talking to doctors. Westport, CT: Auburn; 1993. [Google Scholar]
- Roter D, Larson S. The Roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46(4):243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about trace and quality of medical care. Medical Care. 2008;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- Saha S, Taggart SH, Komaromy M, Bindman AB. Do patients choose physicians of their own race? Health Affair. 2000;19(4):76–83. doi: 10.1377/hlthaff.19.4.76. [DOI] [PubMed] [Google Scholar]
- Schuster MA, Collins R, Cunningham WE, Morton SC, Zierler S, Wong M, Tu W, Kanouse DE. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. Journal of General Internal Medicine. 2005;20(9):807–813. doi: 10.1111/j.1525-1497.2005.05049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shelton JN. Interpersonal concerns in social encounters between majority and minority group members. Group Processes and Intergroup Relations. 2003;6(2):171–185. [Google Scholar]
- Shelton JN, Richeson JA. Intergroup contact and pluralistic ignorance. Journal of Personality and Social Psychology. 2005;88(1):91–107. doi: 10.1037/0022-3514.88.1.91. [DOI] [PubMed] [Google Scholar]
- Shelton JN, Richeson JA. Ethnic minorities’ racial attitudes and contact experiences with White people. Cultural Diversity and Ethnic Minority Psychology. 2006;12(1):149–164. doi: 10.1037/1099-9809.12.1.149. [DOI] [PubMed] [Google Scholar]
- Shelton JN, Richeson JA, Salvatore J. Expecting to be the target of prejudice: Implications for interethnic interactions. Personality and Social Psychology Bulletin. 2005;31(9):1189–1202. doi: 10.1177/0146167205274894. [DOI] [PubMed] [Google Scholar]
- Shelton JN, Richeson JA, Salvatore J, Trawalter S. Ironic effects of racial bias during interracial interactions. Psychological Science. 2005;16(5):397–402. doi: 10.1111/j.0956-7976.2005.01547.x. [DOI] [PubMed] [Google Scholar]
- Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Education and Counseling. 2006;62(3):355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- Strumpf EC. Race/ethnic disparities in primary care: The role of physician-patient concordance. Medical Care. 2011;49(5):496–503. doi: 10.1097/MLR.0b013e31820fbee4. [DOI] [PubMed] [Google Scholar]
- Trachtenberg F, Dugan E, Hall MA. How patients’ trust relates to their involvement in medical care. Journal of Family Practice. 2005;54(4):344–352. [PubMed] [Google Scholar]
- Traylor AH, Schmittdiel JA, Uratsu CS, Mangione CM, Subramanian U. The perdictors of patient-physician race and ethnic concordance: A medical facility fixed-effects approach. Health Services Research. 2010;45(3):792–805. doi: 10.1111/j.1475-6773.2010.01086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science & Medicine. 2000;50(6):813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- Vorauer JD, Turpie CA. Disruptive effects of vigilance on dominant group members’ treatment of outgroup members: Choking versus shining under pressure. Journal of Personality and Social Psychology. 2004;87(3):384–399. doi: 10.1037/0022-3514.87.3.384. [DOI] [PubMed] [Google Scholar]
- West VT, Shelton JN, Traio TE. Relational anxiety in interracial interactions. Psychological Science. 2009;20(3):289–292. doi: 10.1111/j.1467-9280.2009.02289.x. [DOI] [PubMed] [Google Scholar]
- Wilson TD, Lindesy S, Schooler TY. A model of dual attitudes. Psychological Review. 2000;107(1):101–126. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]