Abstract
OBJECTIVE
Hospital readmissions are a current target of initiatives to reduce healthcare costs. This study quantified the association between having a clinical culture positive for 1 of 3 prevalent hospital-associated organisms and time to hospital readmission.
DESIGN
Retrospective cohort study.
PATIENTS AND SETTING
Adults admitted to an academic, tertiary care referral center from January 1, 2001, through December 31, 2008.
METHODS
The primary exposure of interest was a clinical culture positive for methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant enterococci (VRE), or Clostridium difficile obtained more than 48 hours after hospital admission during the index hospital stay. The primary outcome of interest was time to readmission to the index facility. Multivariable Cox proportional hazards models were used to model the adjusted association between positive clinical culture result and time to readmission and to calculate hazard ratios (HRs) and 95% confidence intervals (CIs).
RESULTS
Among 136,513 index admissions, the prevalence of hospital-associated positive clinical culture result for 1 of the 3 organisms of interest was 3%, and 35% of patients were readmitted to the index facility within 1 year after discharge. Patients with a positive clinical culture obtained more than 48 hours after hospital admission had an increased hazard of readmission (HR, 1.40; 95% CI, 1.33–1.46) after adjusting for age, sex, index admission length of stay, intensive care unit stay, Charlson comorbidity index, and year of hospital admission.
CONCLUSIONS
Patients with healthcare-associated infections may be at increased risk of hospital readmission. These findings may be used to impact health outcomes after discharge from the hospital and to encourage better infection prevention efforts.
Hospital readmission has been identified as a key quality indicator and target for reducing healthcare spending. For example, approximately 20% of Medicare beneficiaries in 2004 were readmitted within 30 days after hospital discharge at a cost of approximately $17.4 billion.1 Similarly, healthcare-associated infections are associated with higher healthcare costs and may act as a surrogate for hospital quality of care.2 Healthcare-associated infections are also associated with considerable morbidity and mortality among infected patients and continue to increase in incidence despite laborious and costly infection prevention efforts.3,4
Although much attention has been directed toward hospital readmissions and healthcare-associated infections as potentially preventable conditions and targets to reduce healthcare spending, to our knowledge, no studies have directly assessed the association between the two. In this study, we aimed to investigate the association between hospital-associated infection and time to hospital readmission. A positive association would provide additional incentives for infection prevention and could aid in targeting patients for more intensive hospital discharge planning. We hypothesized that a clinical culture positive for 1 of 3 prevalent healthcare-associated pathogens (methicillin-resistant Staphylococcus aureus [MRSA], vancomycin-resistant enterococci [VRE], or Clostridium difficile) that was obtained more than 48 hours after hospital admission would be associated with a shorter time to hospital readmission.
METHODS
Study Design and Population
This study was approved by the University of Maryland, Baltimore, institutional review board. We used a retrospective cohort of adult patients (>18 years of age) who were admitted to the University of Maryland Medical Center (UMMC) over an 8-year period from January 1, 2001, through December 31, 2008. During the study period, UMMC was a 656-bed tertiary care facility in Baltimore, Maryland, with an active infection prevention program that included MRSA and VRE surveillance culturing in all intensive care units (ICUs) and MRSA surveillance culturing of medical and surgical patients at high risk for infection at hospital admission.5
Each hospital admission was listed as an index admission. Hence, multiple admission and readmission events per patient were possible, and each admission to the hospital resulted in a new row of data. We excluded patients who were not at risk of readmission due to death during their index hospitalization as well as readmissions that occurred less than 24 hours after the initial admission. The second exclusion criterion was to account for transfers from one service to another within the hospital that may have been registered as separate admission events in the database. However, these patients were not completely excluded from the analysis. The admission that resulted in a readmission within 24 hours was excluded, but the readmission would be counted as a new index admission and was therefore not excluded. Finally, because our primary exposure was a positive clinical culture result obtained more than 48 hours after hospital admission, we excluded all patients with a length of stay of less than 48 hours, because these patients could not have this exposure.
Data Collection
All data were extracted from the UMMC Clinical Data Repository, a relational database maintained by the University of Maryland Medical System Information Technology Group, which contains patient administrative, pharmacy, and laboratory data. These data have been used extensively in published epidemiologic studies.6–8 The validity of the clinical culture indicators in these data was assessed by comparing a random sample of 50 admissions with the patients’ paper medical records. This validity assessment suggested a sensitivity of 99% and a specificity of 92%. Comorbid illnesses were defined using International Classification of Diseases, Ninth Revision(ICD-9),9 codes and the Charlson comorbidity index was used to measure aggregate comorbidity.10
Our primary exposure of interest was clinical culture positive for MRSA, VRE, or C. difficile obtained more than 48 hours after hospital admission. The 48-hour cutoff point has been used previously as a proxy for hospital-associated infection.11–13 Clinical culture specimens could have been from any site and were collected when patients exhibited signs or symptoms of an infection. Patients who had a positive clinical culture result 48 hours or less after admission, patients who did not have a clinical culture specimen collected, or patients whose clinical cultures were negative for the organisms of interest were considered to not have the exposure of interest. Our primary outcome of interest was time to readmission to the index facility (ie, UMMC) after discharge from the hospital after the index admission. If a patient was readmitted to the hospital with a positive clinical culture result at admission (regardless of the infecting organism), that patient would not be considered to have our exposure of interest for the (new) index admission unless they had a new hospital-associated (ie, occurring >48 hours after hospital admission) positive clinical culture result at that admission. This assured that each incident positive clinical culture was considered only once.
Statistical Methods
We performed univariable and bivariable analyses on demographic and clinical variables. Discrete covariates were examined for association with both our exposure and our outcome using χ2 analysis. Continuous variables were examined using Student t tests for normally distributed variables and Wilcoxon rank-sum tests for non–normally distributed variables. A 2-sided P value of <.05 was considered statistically significant. We examined age as both a continuous and a categorical variable. Age categories used were <20 years, 20–29 years, 30–39 years, 40–49 years, 50–59 years, 60–69 years, and 70 years or older. Because age was a significant predictor of hospital readmission in our multivariable model as both a continuous and a categorical variable, we chose to dichotomize it at 65 years of age for ease of interpretation. The distribution of length of initial hospital stay was highly skewed and was therefore dichotomized about the median. We used the Cochran-Armitage trend test to determine whether the predominant organism in positive clinical cultures obtained 48 hours or more after hospital admission changed over time. We examined survival curves for patients with hospital readmission occurring within 365 days after hospital discharge, stratified by clinical culture status, using the Kaplan-Meier method. Survival curves were compared using the log-rank test statistic.
We modeled time-to-rehospitalization using a Cox proportional hazards model that accounted for repeated hospitalization events following Anderson-Gill’s counting process method.14 The sandwich estimator was used to produce robust standard error estimates. Our unadjusted model examined days to readmission as a function of positive clinical culture obtained more than 48 hours after hospital admission. Covariates that were found to be significantly associated with both our exposure and our outcome were added one at a time to the basic model. Covariates were retained in the model if their parameter estimates had P values <.05 or if they resulted in a 10% or greater change in the parameter estimate of positive clinical culture result. Statistical analyses were performed using SAS, version 9.2 (SAS Institute).
RESULTS
There were 244,852 adult patients admitted during the study period. Of these, 7,402 were excluded because the patient died during the initial hospital stay, 4,658 were excluded because the patient was readmitted less than 24 hours after the initial discharge, and 96,279 were excluded because they had a length of hospital stay of less than 48 hours. The remaining 136,513 admissions formed our study population (Table 1). The mean age of the sample (± standard deviation) was 51 ± 18 years, and 53% of the patients were male. The median (interquartile range [IQR]) length of stay of the initial hospitalization was 6 days (IQR, 3–13 days).
TABLE 1.
Demographic and Clinical Characteristics of Adult Patients Admitted to University of Maryland Medical Center during the Period 2001–2008, by Culture Result
| Characteristic | Clinical culture result positive for MRSA, VRE, or Clostridium difficile >48 h after hospital admission
|
P | ||
|---|---|---|---|---|
| Yes (n = 4,737) | No (n = 131,776) | Overall (n = 136,513) | ||
| Age, mean ± SD | 52.5 ± 16.8 | 51.0 ± 17.9 | 51.1 ± 17.9 | <.0001 |
| Male sex, no. (%) of patients | 2,847 (60) | 69,413 (53) | 72,260 (53) | <.0001 |
| Charlson comorbidity index, mean ± SD | 2.0 ± 2.1 | 1.6 ± 2.0 | 1.6 ± 2.1 | <.0001 |
| Index length of stay, median days (IQR) | 24 (3–54) | 6 (3–13) | 6 (3–13) | <.0001 |
| ICU stay, no. (%) of patients | 2,174 (46) | 29,588 (22) | 31,762 (23) | <.0001 |
| Year of hospital admission, no. (%) of patients | <.0001 | |||
| 2001 | 445 (3.2) | 13,980 (96.8) | 13,925 (100) | |
| 2002 | 512 (3.3) | 14,762 (96.7) | 15,274 (100) | |
| 2003 | 602 (3.6) | 16,199 (96.4) | 16,801 (100) | |
| 2004 | 546 (3.6) | 16,811 (96.4) | 17,357 (100) | |
| 2005 | 615 (3.4) | 17,606 (96.6) | 18,221 (100) | |
| 2006 | 780 (4.2) | 17,957 (95.8) | 18,737 (100) | |
| 2007 | 726 (3.9) | 18,098 (96.1) | 18,824 (100) | |
| 2008 | 511 (2.9) | 16,863 (97.1) | 17,374 (100) | |
NOTE. ICU, intensive care unit; IQR, interquartile range; MRSA, methicillin-resistant Staphylococcus aureus; SD: standard deviation; VRE: vancomycin-resistant enterococci.
During the study period, 7,898 (6%) of the patients admitted to the hospital had a clinical culture positive for one of the organisms of interest, and 4,737 (3%) had a positive clinical culture obtained more than 48 hours after admission. Of these, 2,318 (49%) of the patients had cultures positive for MRSA, 1,174 (25%) had cultures positive for VRE, and 1,643 (35%) had cultures positive for C. difficile. Three hundred and eighty-three had cultures that were positive for more than 1 organism obtained 48 hours or more after hospital admission. In addition, trend analysis suggested a significant increasing trend in the proportion of clinical cultures obtained 48 hours or more after hospital admission that were positive for MRSA during the period 2001–2008 (P = .02) as well as slight decreasing trends for VRE-positive (P = .06) and C. difficile–positive cultures (P = .05).
Patients with hospitalizations during which a positive clinical culture was obtained more than 48 hours after admission differed significantly from other patients in a number of respects. Patients with a positive clinical culture were significantly older, were more likely to be male and to have an ICU stay, and had a higher mean Charlson comorbidity index. Furthermore, these patients had significantly longer median length of stay (P < .01 for all).
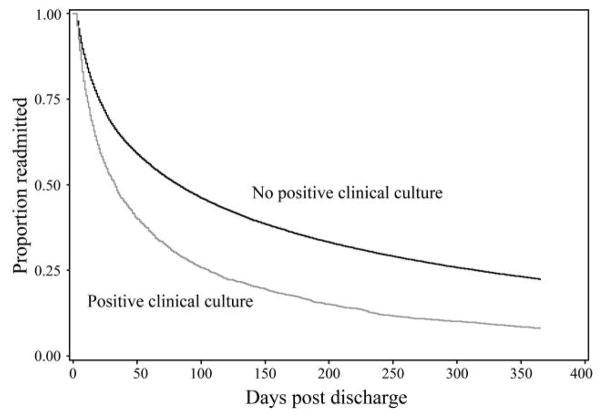
Thirty-five percent of patients were readmitted to the index hospital within 365 days. An examination of survival curves of time to readmission, stratified by clinical culture status, suggests a shorter time to readmission among those patients with a positive clinical culture obtained more than 48 hours after admission (log-rank χ2 value of <.0001; Figure 1) Median time to readmission among those with a positive clinical culture was 27 days (95% confidence interval [CI], 25–30 days), compared with 59 days (95% CI, 57–60 days) for patients without a positive clinical culture result. A 30-day period to readmission was also examined. The incidence of 30-day readmission among patients with a positive clinical culture result was 25%, compared with 15% for patients with a negative result or no clinical culture (P < .01). Our final Cox proportional hazards model contained terms for positive clinical culture, sex, age greater than 65 years, length of stay greater than 3 days, Charlson comorbidity index, ICU admission, and year of hospital admission. The results of this model are displayed in Table 2. Patients with a positive clinical culture obtained 48 hours or more after admission during their initial hospital stay had a significantly increased hazard of hospital readmission (hazard ratio [HR], 1.40; 95% CI, 1.38–1.51). Additional analysis suggested a greater hazard of readmission for patients with a clinical culture positive for VRE (HR, 1.67; 95% CI, 1.53–1.81), compared with patients with cultures positive for MRSA (HR, 1.30; 95% CI, 1.22–1.38) or C. difficile (HR, 1.35; 95% CI, 1.26–1.45). Furthermore, the inclusion of all 3 organisms in the model resulted in slightly reduced but significant hazards of readmission, which suggests that the presence of a clinical culture positive for each organism is an independent predictor of hospital readmission. Patients aged less than 65 years (HR, 1.45; 95% CI, 1.41–1.49) or who had a length of stay greater than 3 days (HR, 1.14; 95% CI, 1.12–1.17) also had a significantly increased hazard of hospital readmission. Patients with an ICU stay had a decreased hazard of readmission (HR, 0.87; 95% CI, 0.85–0.89). Sex was not a significant predictor of hospital readmission. Additional analyses were performed to determine whether the increased hazard of readmission among those aged less than 65 years was attributable to the inclusion of patients admitted to obstetric or pediatric services (n = 5,886). However, excluding these patients resulted in no change to the HR point estimates. Each unit increase in Charlson comorbidity index score was associated with an increased hazard of readmission (HR, 1.11; 95% CI, 1.10–1.11), whereas each unit increase in year of admission was associated with a decrease in the hazard of readmission (HR, 0.93; 95% CI, 0.93–0.94).
FIGURE 1.
Survival curves of time to hospital readmission within 1 year after hospital discharge for those with a clinical culture positive for methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci, or Clostridium difficile occurring more than 48 hours after hospitalization (n =58,857).
TABLE 2.
Adjusted Hazard Ratio of Readmission within 1 Year after Hospital Discharge for Patients with a Clinical Culture Positive for MRSA, VRE, or Clostridium difficile Occurring More than 48 Hours after Hospitalization
| Characteristic | Hazard ratio (95% confidence interval) (n = 136,513) |
|---|---|
| Unadjusted, positive clinical culture | 1.45 (1.38–1.51) |
| Adjusted | |
| Clinical culture positive for MRSA, VRE, or C. difficile | 1.40 (1.33–1.51) |
| Female sex | 0.98 (0.95–1.00) |
| Age <65 years | 1.45 (1.41–1.49) |
| Length of initial hospital stay >3 days | 1.14 (1.12–1.17) |
| ICU stay | 0.87 (0.85–0.89) |
| Charlson comorbidity index | 1.11 (1.10–1.11) |
| Year of hospital admissiona | 0.93 (0.93–0.94) |
NOTE. ICU, intensive care unit; MRSA, methicillin-resistant Staphylococcus aureus; VRE: vancomycin-resistant enterococci.
Decrease in hazard of readmission per increase in year of hospital admission.
DISCUSSION
Hospital readmission and healthcare-associated infections are common healthcare problems with important clinical and financial implications for both patients and hospitals. Our analysis of 8 years of hospital admissions data at a large urban tertiary care facility suggests that there is a significant association between the two; specifically, we found that patients with a clinical culture positive for 1 of 3 prevalent nosocomial pathogens obtained more than 48 hours after hospital admission had a shorter time to hospital readmission. Furthermore, the median time to readmission for such patients was almost half that for other patients. This study is novel in its investigation of the relationship between the presence of a positive clinical culture obtained more than 48 hours after hospital admission and time to rehospitalization among admitted patients.
To our knowledge, only one earlier study has examined the association between positive clinical culture result and hospital readmission. In that study, patients with MRSA surgical site infections were more likely than other patients to be readmitted to the hospital within 30 days.15 These results are consistent with our findings. In addition, our observations that longer lengths of stay and greater Charlson comorbidity index score are associated with shorter time to readmission is consistent with previous studies.1,16–19 In contrast with previous research, we observed age less than 65 years to be associated with shorter time to hospital readmission.1,20 Furthermore, we observed that having an ICU stay was protective in our statistical model. This may be attributable to the fact that patients who are admitted to ICUs are likely to be more severely ill and, as such, are more likely to be discharged to another healthcare facility, thereby reducing their risk of readmission to the hospital.
There are a number of limitations to this study that require comment. First, by excluding patients who died during their index hospitalization, a large proportion of patients with positive clinical culture results were also excluded. These patients constituted 16% of the total number of patients with a positive clinical culture result obtained more than 48 hours after hospital admission (including those who died). In addition, we used positive clinical culture result obtained more than 48 hours after admission as a proxy for hospital-associated infection. However, a study at the same institution that assessed the incidence of MRSA infection observed that approximately 82% of MRSA-positive clinical cultures were attributable to true infections, defined using National Hospital Safety Network criteria.5 Furthermore, this study used administrative data, and therefore, we did not have data on where patients originated from (eg, home or nursing home) and were unable to differentiate between patients who were readmitted within less than 24 hours after discharge from the hospital and those who were transferred between services within the hospital. Lastly, we only had data on readmissions to the index facility and may have potentially misclassified those patients who were readmitted to other hospitals as not having a readmission. However, this exclusion would have resulted in nondifferential misclassification and biased our results towards a null effect.
Despite these limitations, this study has several strengths, including a large sample size and data that were collected over an extended period. The authors believe that using data collected over a period of 8 years will help to account for fluctuations in the prevalence of specific antibiotic-resistant bacteria and changes in hospital policy or procedures related to quality of care over time.
In conclusion, our results suggest that healthcare-associated positive clinical culture results may be associated with a significantly shorter time to hospital readmission. Efforts to reduce healthcare-associated infections may have the additional benefit of reducing the incidence of hospital readmission and associated poor patient outcomes and increased healthcare costs. Furthermore, patients with a positive clinical culture result obtained more than 48 hours after hospital admission could be targeted to receive additional discharge planning resources designed to reduce the likelihood of hospital readmission.
Acknowledgments
We thank Colleen Reilly and Jingkun Zhu for data management and extraction.
Financial support. Agency for Healthcare Research and Quality grant R36HS021068–01 (to J.S.A) and National Institutes of Health grants 5K24AI079040–02 (to A.D.H.) and K01AI071015–04 (to J.P.F.).
Footnotes
Potential conflicts of interest. All authors report no conflicts of interest relevant to this article. All authors submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest, and the conflicts that the editors consider relevant to this article are disclosed here.
Presented in part: 49th Annual Interscience Conference on Antimicrobial Agents and Chemotherapy; San Francisco, California; September 2009.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Kang C, Kim S, Park W, et al. Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother. 2005;49:760–766. doi: 10.1128/AAC.49.2.760-766.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Emori TG, Culver DH, Horan TC, et al. National nosocomial infections surveillance system (NNIS): description of surveillance methods. Am J Infect Control. 1991;19:19–35. doi: 10.1016/0196-6553(91)90157-8. [DOI] [PubMed] [Google Scholar]
- 4.Toubes E, Singh K, Yin D, et al. Risk factors for antibiotic-resistant infection and treatment outcomes among hospitalized patients transferred from long-term care facilities: does antimicrobial choice make a difference? Clin Infect Dis. 2003;36:724–730. doi: 10.1086/368081. [DOI] [PubMed] [Google Scholar]
- 5.Harris A, Furuno J, Roghmann M, et al. Targeted surveillance of methicillin-resistant Staphylococcus aureus and its potential use to guide empiric antibiotic therapy. Antimicrob Agents Chemother. 2010;54:3143–3148. doi: 10.1128/AAC.01590-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furuno JP, McGregor JC, Harris AD, et al. Identifying groups at high risk for carriage of antibiotic-resistant bacteria. Arch Intern Med. 2006;166:580–585. doi: 10.1001/archinte.166.5.580. [DOI] [PubMed] [Google Scholar]
- 7.Furuno JP, Harris AD, Wright MO, et al. Value of performing active surveillance cultures on intensive care unit discharge for detection of methicillin-resistant Staphylococcus aureus. Infect Control Hosp Epidemiol. 2007;28:666–670. doi: 10.1086/518348. [DOI] [PubMed] [Google Scholar]
- 8.Schweizer ML, Furuno JP, Harris AD, et al. Empiric antibiotic therapy for Staphylococcus aureus bacteremia may not reduce in-hospital mortality: a retrospective cohort study. PLoS ONE. 2010;5:e11432. doi: 10.1371/journal.pone.0011432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.ICD-9-CM: International Classification of Diseases, 9th Revision; Clinical Modification, 6th Edition. 9. 1–3. Los Angeles, CA: Practice Management Information; 2006. [Google Scholar]
- 10.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–1251. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 11.Cosgrove SE, Qi Y, Kaye KS, Harbarth S, Karchmer AW, Carmeli Y. The impact of methicillin resistance in Staphylococcus aureus bacteremia on patient outcomes: mortality, length of stay, and hospital charges. Infect Control Hosp Epidemiol. 2005;26:166–174. doi: 10.1086/502522. [DOI] [PubMed] [Google Scholar]
- 12.Cowie SE, Ma I, Lee SK, Smith RM, Hsiang YN. Nosocomial MRSA infection in vascular surgery patients: impact on patient outcome. Vasc Endovascular Surg. 2005;39:327–334. doi: 10.1177/153857440503900404. [DOI] [PubMed] [Google Scholar]
- 13.McDonald LC, Coignard B, Dubberke E, Song X, Horan T, Kutty P. Recommendations for surveillance of Clostridium difficile–associated disease. Infect Control Hosp Epidem. 2007;28:140–145. doi: 10.1086/511798. [DOI] [PubMed] [Google Scholar]
- 14.Anderson PK, Gill RD. Cox’s regression model for counting processes: a large sample study. Ann Stat. 1982;10:1100. [Google Scholar]
- 15.Anderson D, Kaye K, Chen L, et al. Clinical and financial outcomes due to methicillin resistant Staphylococcus aureus surgical site infection: a multi-center matched outcomes study. PLoS ONE. 2009;4:e8305. doi: 10.1371/journal.pone.0008305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu LW, Pei CK. Risk factors for early emergency hospital readmission in elderly medical patients. Gerontol. 1999;45:220–226. doi: 10.1159/000022091. [DOI] [PubMed] [Google Scholar]
- 17.Williams S, Bottle A, Aylin P. Length of hospital stay and subsequent emergency readmission. BMJ. 2005;331:371. doi: 10.1136/bmj.331.7513.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hasan O, Meltzer DO, Shaykevich SA, et al. Hospital readmission in general medicine patients: a prediction model. J Gen Intern Med. 2010;25:211–219. doi: 10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marcantonio ER, Goldfinger M, Brennan TA, McKean S. Risk factors for unplanned readmission in members of a Medicare HMO. Am J Med. 1997;45:P142. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]
- 20.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. J Am Geriatr Soc. 1999;107:13–17. doi: 10.1016/s0002-9343(99)00159-x. [DOI] [PubMed] [Google Scholar]