Abstract
This study examined the association between patient-reported anxiety and post-cardiac surgery mortality and major morbidity. Frailty ABC'S was a prospective multicenter cohort study of elderly patients undergoing cardiac surgery (coronary artery bypass surgery and/or valve repair or replacement) at 4 tertiary care hospitals between 2008 and 2009. Patients were evaluated a mean of 2 days preoperatively with the Hospital Anxiety and Depression Scale (HADS), a validated questionnaire assessing depression and anxiety in hospitalized patients. The primary predictor variable was high levels of anxiety, defined by HADS score ≥11. The main outcome measure was all-cause mortality or major morbidity (stroke, renal failure, prolonged ventilation, deep sternal wound infection, or reoperation) occurring during the index hospitalization. Multivariable logistic regression examined the association between high preoperative anxiety and all-cause mortality/major morbidity, adjusting for Society of Thoracic Surgeons (STS) predicted risk, age, gender, and depression symptoms. A total of 148 patients (mean age 75.8 ± 4.4 years; 34% women) completed the HADS-A. High levels of preoperative anxiety were present in 7% of patients. There were no differences in type of surgery and STS predicted risk across preoperative levels of anxiety. After adjusting for Society of Thoracic Surgeons predicted risk, age, gender, and symptoms of depression, preoperative anxiety remained independently predictive of postoperative mortality or major morbidity (OR 5.1; 95% CI 1.3, 20.2; p=0.02). In conclusion, although high levels of anxiety were present in a minority of patients anticipating cardiac surgery, this conferred a strong and independent heightened risk of mortality or major morbidity.
Keywords: geriatric, cardiac surgery, outcomes, anxiety
The importance of altered mood states in cardiovascular disease has been highlighted by several reports.1-6 With regards to surgical outcomes, depressive symptoms were evaluated in a cohort of patients undergoing coronary artery bypass graft surgery at between 1989 and 1991, with Blumenthal et al discovering a significantly higher mortality among patients with preoperative depression.7 Despite the interrelation between the affective states of anxiety and depression,8 preoperative anxiety was not assessed. Prospective and simultaneous assessment of both anxiety and depression using a measure such as the Hospital Anxiety and Depression Scale (HADS) is necessary to understand and distinguish the role of these two affective states in post-operative outcomes.3, 5 As such, we administered the Hospital Anxiety and Depression Scale (HADS) to measure anxiety and depression prospectively in hospitalized elderly patients awaiting coronary artery bypass grafting (CABG) and/or valve repair or replacement.
Methods
Consecutive patients were screened for study inclusion between 2008 and 2009 at 4 university-affiliated tertiary care centers in the United States and Canada as part of the Frailty ABC'S (Frailty and Anxiety Before Cardiac Surgery) study.9 Eligible patients were asked by study personnel to complete a structured questionnaire that included the HADS and a brief battery of physical performance tests. Mini-mental status examinations were also administered and patients were asked to grade their overall health status. Frailty criteria were determined according to the Cardiovascular Health Study (CHS) scale.10
Inclusion criteria were age ≥ 70 and scheduled to undergo coronary artery bypass grafting (CABG) and/or valve replacement or repair through a traditional midline sternotomy. Exclusion criteria included any of the following: emergent surgery defined as surgery for ongoing refractory cardiac compromise for which there should be no delay; clinical instability defined as active coronary ischemia, decompensated heart failure, or any acute process causing significant symptoms or abnormal vital signs; severe neuropsychiatric condition causing inability to cooperate with study procedures; or the patient's planned surgery was cancelled. Treating physicians were blinded to the results of the HADS in order to not influence perioperative care.
This manuscript was prepared in keeping with the standards set forth by the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) Statement.11 Institutional review board approval was obtained at each enrolling center prior to proceeding with patient enrollment or any data acquisition. All patients signed an informed consent to participate in the study.
The HADS is a brief user-friendly self-report questionnaire developed by Zigmond and Snaith in 1983 to assess the levels of anxiety and depression among patients in non-psychiatric hospitals .12 This self-report scale can be administered to patients in approximately 5 minutes or less, and can be scored in approximately one minute. The HADS has been repeatedly validated and shown to perform well as a screening tool in assessing presence and symptom severity of both anxiety disorders and depression.13, 14 The HADS has been translated into many languages, with validation studies confirming the international applicability of the questionnaire.15 In the present study, HADS questionnaires were administered in English or French.
The HADS questionnaire consists of 14 items, 7 for each of two subscales: anxiety (HADS-A) and depression (HADS-D). Each item is rated 0 to 3 (3-point Likert scale), resulting in a potential range of scores from 0 to 21 for each subscale. A score of 11 or greater on either subscale is considered to indicate cases of ‘significant psychological morbidity’. Scores 8 to 10 represent ‘possible anxiety’ and 0 to 7 represent ‘no anxiety’. Designed for use in the inpatient setting, the individual HADS items are formulated as symptoms referring to the prior seven days and do not include physical indices of psychological distress which may be expected to result in false positives among hospitalized patients. Table 1 displays the key phrases from questions comprising the HADS-A subscale.
Table 1.
Questions from the Hospital Anxiety and Depression Scale – Anxiety (HADS-A)a
| Question | How often in the past week did you... ? |
|---|---|
| A1 | “feel tense or ‘wound up’” |
| A2 | “get a sort of frightened feeling as if something awful is about to happen” |
| A3 | “have worrying thoughts go through your mind” |
| A4 | “sit at ease and feel relaxed” |
| A5 | “get a sort of frightened feeling like ‘butterflies’ in the stomach” |
| A6 | “feel restless as if I have to be on the move” |
| A7 | “get sudden feelings of panic” |
Complete Hospital Anxiety and Depression Scale available in the original 1983 paper by Zigmond and Snaith12
The primary outcome measure was the incidence of mortality or major morbidity (stroke, renal failure, prolonged ventilation, deep sternal wound infection, and need for reoperation) occurring after cardiac surgery during the index hospitalization. STS database definitions were used for all outcomes: death was defined as mortality from any cause, stroke was central neurologic deficit persisting > 72 hours, renal failure was new dialysis requirement or rise in serum creatinine >2mg/dL and > 2 fold above the preoperative level, prolonged ventilation was need for mechanical ventilation > 24 hours, and reoperation was for any reason. The secondary outcome measures were discharge to a healthcare facility for ongoing medical care or rehabilitation, and prolonged postoperative length of stay defined by the STS standard of >14 days after surgery. The physicians ascertaining outcomes from medical records were blinded to results of the HADS questionnaire.
Demographic and operative characteristics were compared across categories of HADS-A scores: 0 to 7 (no anxiety), 8 to 10 (possible anxiety), and ≥11 (anxiety). Categorical variables were displayed as % and continuous variables were presented as medians with 25th and 75th percentiles. Comparisons of baseline variables were conducted using the nonparametric Wilcoxon rank-sum test.
Multivariable analyses were performed with logistic regression modeling and reported as odds ratios (ORs) with 95% confidence intervals (CIs). Because the number of risk factors in patients undergoing cardiac surgery is large,16, 17 entering all possible covariates in the model would have resulted in model instability and overfitting. Therefore, we used the STS predicted risk of mortality or major morbidity (STS-PROMM) as a risk score to adjust for the surgical risk associated with traditional medical factors.18-20 The STS-PROMM was selected among all available adult cardiac surgery risk scores because this score was specifically designed to predict in-hospital mortality or major morbidity, the precise primary endpoint of this study.
Sensitivity analysis using a non-parsimonious model adjusted for additional covariates was performed to ensure that significant confounding had not been overlooked. The performance of the model was assessed before and after addition of the HADS-A score to determine its incremental value. Model discrimination, reflecting the ability to assign a higher predicted risk to those who will have the observed outcome, was measured with the area under the ROC curve c-statistic.21 Sensitivity analyses with HADS-A score represented as a continuous variable were also performed. All analyses were performed with STATA version 11 (StataCorp, College Station, Texas).
Results
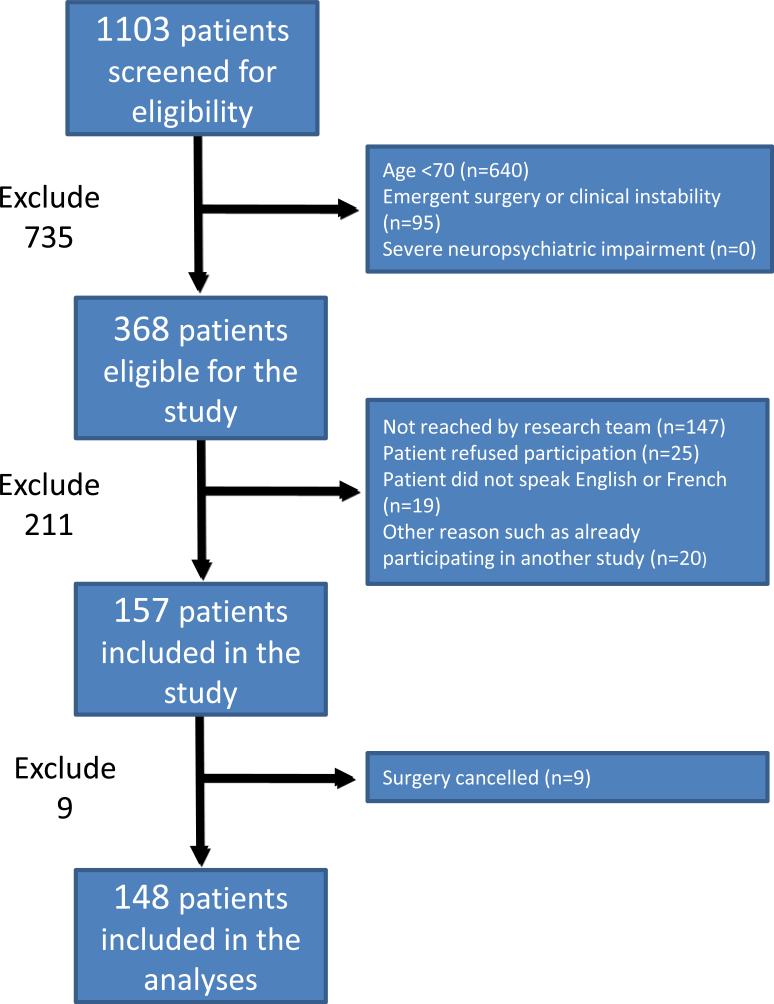
The cohort for these analyses consisted of 148 patients who completed the HADS questionnaire and underwent cardiac surgery within the Frailty ABC'S study. The median time from completion of the questionnaire to surgery was 2 days (IQR 1, 3). No patients were lost to follow-up. Figure 1 displays the flow of patients through the study. Table 2 displays baseline variables stratified by HADS-A score: 71% scored 0 to 7 (“no anxiety”); 22% scored 8 to 10 (“possible anxiety”); and 7% scored 11 to 21 (“anxiety” group). Age and gender were included individually along with STS risk score in the multivariable model presented below. Patients with anxiety were less likely to have a university level education. The three HADS groups were not markedly different in procedure type. Median STS-PROMM was 17%, 16%, and 15% respectively for the no anxiety, possible anxiety, and anxiety groups (Table 2).
Figure 1.
Flow diagram
Table 2.
Baseline variables stratified by HADS-A score
| Variable | No anxiety HADS-A 0-7 (n=105) | Possible anxiety HADS-A 8-10 (n=32) | Anxiety HADS-A 11-21 (n=11) |
|---|---|---|---|
| Age (years) (Q1, Q3) | 75 (72, 79) | 76 (73, 80) | 76 (71, 79) |
| Women | 29 (28%) | 17 (53%) | 4 (36%) |
| Living alone | 30 (29%) | 9 (28%) | 4 (36%) |
| University-level education | 34 (32%) | 8 (25%) | 1 (9%) |
| General perception of health | |||
| Very good | 29 (28%) | 4 (13%) | 0 (0%) |
| Good | 47 (45%) | 12 (38%) | 5 (45%) |
| Fair | 27 (26%) | 10 (31%) | 4 (36%) |
| Poor | 2 (2%) | 6 (19%) | 1 (18%) |
| Body mass index (kg/m2) (Q1, Q3) | 26 (24, 29) | 27 (23, 30) | 27 (26, 30) |
| Diabetes mellitus | 39 (37%) | 13 (41%) | 4 (36%) |
| Hypertension | 75 (71%) | 26 (81%) | 8 (73%) |
| Dyslipidemia | 67 (64%) | 22 (69%) | 9 (82%) |
| Current or past smoker | 59 (56%) | 20 (62%) | 5 (45%) |
| Chronic heart failure | 30 (29%) | 9 (28%) | 2 (18%) |
| LVEF, % (Q1, Q3) | 55 (45, 60) | 60 (54, 65) | 55 (35, 65) |
| Atrial fibrillation | 17 (16%) | 4 (13%) | 3 (27%) |
| Chronic renal failure | 19 (18%) | 6 (19%) | 2 (18%) |
| Stroke | 12 (11%) | 3 (9%) | 1 (9%) |
| History of anxiety | 6 (6%) | 2 (6%) | 0 (0%) |
| History of depression | 5 (5%) | 2 (6%) | 1 (9%) |
| HADS depression score /11 (Q1, Q3) | 2 (1, 4) | 4 (2, 7) | 8 (6, 10) |
| MMSE score /30 (Q1, Q3) | 27 (23, 29) | 28 (26, 29) | 27 (25, 29) |
| Frailty (CHS scale) | 16 (15) | 9 (28) | 5 (45) |
| Type of surgery | |||
| Isolated CABG | 64 (61%) | 18 (56%) | 8 (73%) |
| Valve procedure +/- CABG | 41 (39%) | 14 (44%) | 3 (27%) |
| Urgent surgery | 56 (53%) | 20 (63%) | 5 (45%) |
| STS-PROMM, % (Q1, Q3) | 17 (11, 26) | 16 (13, 21) | 15 (10, 23) |
| STS-PROM, % (Q1, Q3) | 3 (1, 4) | 2 (2, 3) | 2 (1, 4) |
| Logistic EuroSCORE (Q1, Q3) | 7 (4, 12) | 8 (5, 14) | 6 (4, 9) |
CABG = coronary artery bypass graft surgery; CHS = cardiovascular health survey;16 EuroSCORE = European System for Cardiac Operative Risk Evaluation; HADS = hospital anxiety and depression scale; LVEF = left ventricular ejection fraction; MI = myocardial infarction; STS = Society of Thoracic Surgeons; MMSE = mini-mental state examination; STS-PROMM = Society of Thoracic Surgeons predicted risk of mortality and morbidity; STS-PROM = Society of Thoracic Surgeons predicted risk of mortality
The median mini-mental status examination score was 27 out of 30 (normal range), without differences across the 3 HADS-A groups. An existing diagnosis of depression was more often present in patients with anxiety and median HADS-D (depression) scores were 2, 4, and 8 respectively for the no anxiety, possible anxiety, and anxiety groups (Table 2).
Table 3 displays clinical outcomes according to HADS-A score. The composite endpoint of mortality or major morbidity occurred in 22% of the no anxiety group, 25% of the possible anxiety group, and 55% of the anxiety group. In-hospital mortality across the three HADS-A score groups was 4%, 6%, and 9% respectively. Discharge to a healthcare facility (nursing home, convalescence or rehabilitation facility) was also increased with increasing anxiety.
Table 3.
In-Hospital Outcomes by Anxiety Groups
| Outcomes | No anxiety HADS-A 0-7 (n=105) | Possible anxiety HADS-A 8-10 (n=32) | Anxiety HADS-A 11-21 (n=11) |
|---|---|---|---|
| Mortality or major morbidity | 23 (22%) | 8 (25%) | 6 (55%) |
| Mortality | 4 (4%) | 2 (6%) | 1 (9%) |
| Prolonged length of stay >14 days | 25 (24%) | 12 (38%) | 3 (28%) |
| Discharge to healthcare facility | 28 (28%) | 14 (47%) | 5 (50%) |
HADS-A = Hospital Anxiety and Depression Scale Anxiety subscale
The relationship between the measured HADS-A score and adverse events demonstrated a threshold effect rather than a graded linear response. ROC analysis was performed to identify the optimal threshold cutoff, and showed that a HADS-A score of 11 or higher was most predictive of mortality or major morbidity in our cohort of elderly patients undergoing cardiac surgery (76% of patients correctly classified). This cutoff is in keeping with established norms recommended for categorizing the HADS-A score (0-7 for no anxiety, 8-10 for possible anxiety, ≥11 for anxiety). In a univariable logistic regression with HADS-A score considered as a dichotomous variable (score ≥11 signifying anxiety vs. score <11 signifying possible or no anxiety), the unadjusted odds ratio (OR) for mortality or major morbidity was 4.1 (95% confidence interval [CI] 1.2, 14.4; p=0.027).
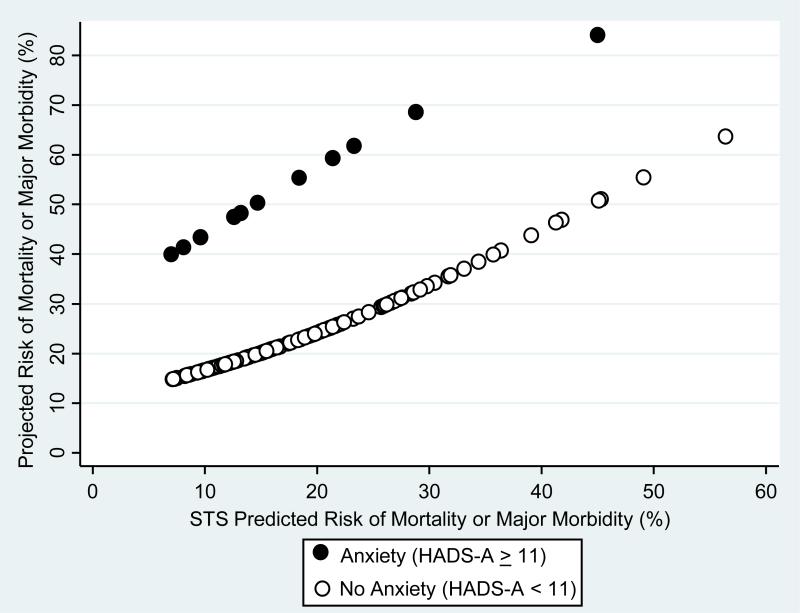
When adjusting for STS-PROMM, age, gender, and HADS-D score, the adjusted OR for mortality or major morbidity was 5.1 (95% CI 1.3, 20.2; p=0.02) (Table 4). Figure 2 demonstrates that for a given STS-PROMM (STS risk score), the predicted risk based on our regression model was higher for patients with anxiety (HADS-A ≥11) compared to patients with no anxiety or possible anxiety (HADS-A <11).
TABLE 4.
Multivariable model to predict mortality or major morbidity
| Odds Ratio (95% CI) | P value | |
|---|---|---|
| STS-PROMM | 1.06 (1.01, 1.10) | 0.01 |
| Age | 1.02 (0.93, 1.12) | 0.62 |
| Female gender | 3.49 (1.52, 7.99) | 0.003 |
| Depression (HADS-D score ≥11) | 1.28 (0.25, 6.59) | 0.77 |
| Anxiety (HADS-A score ≥11) | 5.1 (1.27, 20.2) | 0.02 |
CI = confidence interval; HADS-A = Hospital Anxiety and Depression Scale Anxiety subscale; HADS-D = Hospital Anxiety and Depression Scale Depression subscale; STS-PROMM = Society of Thoracic Surgeons predicted risk of mortality and morbidity.
Figure 2.
Projected risk of mortality or major morbidity according to anxiety or no anxiety by HADS-A score for any Society of Thoracic Surgeons predicted risk
Sensitivity analyses with HADS-A score represented as a continuous variable confirmed similar results to those presented in Table 4. Further sensitivity analysis was performed using a non-parsimonious model adjusted for additional covariates frailty and education level. This did not suggest any evidence of residual confounding, with the OR for anxiety unchanged after the additional variables were added to the model.
Discussion
In this prospective multi-center study, significant levels of patient-reported preoperative anxiety independently predicted a greater risk of in-hospital mortality or major morbidity in elderly patients undergoing cardiac surgery. This increased hazard persisted even after adjustment for surgical risk (STS risk score) related to traditional risk factors as well as depressive symptoms. This study also demonstrates that patients with high levels of anxiety are unlikely to carry a clinical diagnosis of general anxiety disorder. Importantly, as high levels of anxiety are potentially modifiable, identifying these patients may provide an opportunity to increase psychological comfort and improve clinical outcomes in this high risk group.
The relationship between preexisting anxiety and outcomes after cardiac surgery has not been clearly defined. This is likely due in part to the small size of prior studies, variations in anxiety definitions (anxiety disorder, symptoms, or trait anxiety), and failure to consider depression and anxiety simultaneously. 22, 23 We found anxiety in the days preceding surgery among hospitalized elderly patients to be associated with a greater risk for mortality or major morbidity after adjusting for not only the STS risk score but also symptoms of preoperative depression measured by the HADS-D questionnaire. This is particularly relevant given that most prior studies did not explicitly test for coexisting anxiety.7
Depression, and to a lesser extent anxiety, are known risk factors for progressive cardiovascular disease among medically managed outpatients.2, 24 In a study of 1054 patients with stable coronary artery disease completing the HADS questionnaire, Rothenbacher et al simultaneously considered anxiety and depressive symptom scores in relation to adverse cardiovascular events during 3-year follow-up.25 Similar to our study, anxiety was associated with an increased risk for cardiovascular events [HR 3.3 (95% CI 1.3-8.3)], whereas depressive symptoms were associated with a nonsignificant risk [HR 0.62; (95% CI 0.20-1.87)] among these patients not undergoing surgical treatment.25
Several pathophysiological processes have been proposed to explain the negative relationship between anxiety and adverse events, including hypercortisolemia with insulin resistance, sympathetic vagal disturbance with deregulation of blood pressure, and lifestyle risk factors including cigarette smoking.26,27Increased anxiety could stem from low health literacy or lower educational status, which results in unfamiliarity with the health care environment. In this case, patients who feel anxious or ill-at-ease are more likely to be unable to adhere to the post-procedural plan of care, resulting in adverse events. This explanation would represent a potentially modifiable process.
The results of the present study have relevance for clinical care. Administration of the simple HADS questionnaire may warrant further study for use in rapid bedside diagnostic orientation. A quick evaluation of anxiety symptoms as part of the preoperative workup may allow identification of high-risk patients for whom pharmacological or psychotherapeutic interventions may be instituted. Moreover, stress management and education intervention services are offered at many hospitals and these resources could be utilized for appropriately identified cardiac surgical inpatients.
Recent literature has suggested that cardiovascular procedures following myocardial infarction may be underutilized in patients with mental health disorders,28 and we caution readers not to interpret these findings as a barrier to delivery of evidence-based care. Instead, our observations should encourage recognition of preoperative anxiety among elderly patients before cardiac surgery and promote collaboration among cardiovascular physicians with psychiatric services to reduce emotional tension and perhaps improve post-cardiac surgery outcomes.
This study has several important limitations. First, this was an observational study for which causality cannot be inferred and effects of unknown confounders on the observed associations cannot be excluded. Second, patients with high levels of anxiety reported slightly lower overall health status, suggesting something about their health may not be captured in the clinical variables (including the STS risk score). In other words, anxiety symptoms may act as a surrogate for more sick or vulnerable patients not captured by the STS risk score. Third, although we adjusted for depression symptoms as a comorbid state using the HADS-D, the severity of depression was not considered. Fourth, prior or current use of antidepressants, anxiolytics, or psychiatric services was not assessed. Finally, while this was a multi-institutional and multinational study, the findings of our study remain to be validated in a larger external dataset, particularly for younger patients.
Acknowledgements
Dr. Williams was supported in part by training grant T32-HL069749 from the National Institutes of Health and Drs. Williams, Smith, and Perrault are supported in part by grant U01-HL088953 from the National Institutes of Health Cardiothoracic Surgical Trials Network.
References
- 1.Frasure-Smith N, Lesperance F, Talajic M. Depression following myocardial infarction. Impact on 6-month survival. JAMA. 1993;270:1819–1825. [PubMed] [Google Scholar]
- 2.Gullette EC, Blumenthal JA, Babyak M, Jiang W, Waugh RA, Frid DJ, O'Connor CM, Morris JJ, Krantz DS. Effects of mental stress on myocardial ischemia during daily life. JAMA. 1997;277:1521–1526. [PubMed] [Google Scholar]
- 3.Arnold SV, Spertus JA, Ciechanowski PS, Soine LA, Jordan-Keith K, Caldwell JH, Sullivan MD. Psychosocial modulators of angina response to myocardial ischemia. Circulation. 2009;120:126–133. doi: 10.1161/CIRCULATIONAHA.108.806034. [DOI] [PubMed] [Google Scholar]
- 4.Martens EJ, de Jonge P, Na B, Cohen BE, Lett H, Whooley MA. Whooley, Scared to death? Generalized anxiety disorder and cardiovascular events in patients with stable coronary heart disease:The Heart and Soul Study. Arch Gen Psychiatry. 2010;67:750–758. doi: 10.1001/archgenpsychiatry.2010.74. [DOI] [PubMed] [Google Scholar]
- 5.Roest AM, Martens EJ, Denollet J, de Jonge P. Prognostic association of anxiety post myocardial infarction with mortality and new cardiac events: a meta-analysis. Psychosom Med. 2010;72:563–569. doi: 10.1097/PSY.0b013e3181dbff97. [DOI] [PubMed] [Google Scholar]
- 6.Dao TK, Chu D, Springer J, Gopaldas RR, Menefee DS, Anderson T, Hiatt E, Nguyen Q. Clinical depression, posttraumatic stress disorder, and comorbid depression and posttraumatic stress disorder as risk factors for in-hospital mortality after coronary artery bypass grafting surgery. J Thorac Cardiovasc Surg. 2010;140:606–610. doi: 10.1016/j.jtcvs.2009.10.046. [DOI] [PubMed] [Google Scholar]
- 7.Blumenthal JA, Lett HS, Babyak MA, White W, Smith PK, Mark DB, Jones R, Mathew JP, Newman MF, NORG Investigators Depression as a risk factor for mortality after coronary artery bypass surgery. Lancet. 2003;362:604–609. doi: 10.1016/S0140-6736(03)14190-6. [DOI] [PubMed] [Google Scholar]
- 8.Bankier B, Januzzi JL, Littman AB. The high prevalence of multiple psychiatric disorders in stable outpatients with coronary heart disease. Psychosom Med. 2004;66:645–650. doi: 10.1097/01.psy.0000138126.90551.62. [DOI] [PubMed] [Google Scholar]
- 9.Afilalo J, Eisenberg MJ, Morin JF, Bergman H, Monette J, Noiseux N, Perrault LP, Alexander KP, Langlois Y, Dendukuri N, Chamoun P, Kasparian G, Robichaud S, Gharacholou SM, Boivin JF. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56:1668–1676. doi: 10.1016/j.jacc.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research Group Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 11.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 12.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiat Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 13.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 14.Osborne RH, Elsworth GR, Sprangers MA, Oort FJ, Hopper JL. The value of the Hospital Anxiety and Depression Scale (HADS) for comparing women with early onset breast cancer with population-based reference women. Qual Life Res. 2004;13:191–206. doi: 10.1023/B:QURE.0000015292.56268.e7. [DOI] [PubMed] [Google Scholar]
- 15.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale--a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/s0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 16.Jones RH, Hannan EL, Hammermeister KE, Delong ER, O'Connor GT, Luepker RV, Parsonnet V, Pryor DB. Identification of preoperative variables needed for risk adjustment of short-term mortality after coronary artery bypass graft surgery. The Working Group Panel on the Cooperative CABG Database Project. J Am Coll Cardiol. 1996;28:1478–1487. doi: 10.1016/s0735-1097(96)00359-2. [DOI] [PubMed] [Google Scholar]
- 17.Tu JV, Sykora K, Naylor CD. Assessing the outcomes of coronary artery bypass graft surgery: how many risk factors are enough? Steering Committee of the Cardiac Care Network of Ontario. J Am Coll Cardiol. 1997;30:1317–1323. doi: 10.1016/s0735-1097(97)00295-7. [DOI] [PubMed] [Google Scholar]
- 18.Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3--valve plus coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:S43–62. doi: 10.1016/j.athoracsur.2009.05.055. [DOI] [PubMed] [Google Scholar]
- 19.O'Brien SM, Shahian DM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force Ann Thorac Surg. 2009;88:S23–42. doi: 10.1016/j.athoracsur.2009.05.056. [DOI] [PubMed] [Google Scholar]
- 20.Shahian DM, O'Brien SM, Filardo G, Ferraris VA, Haan CK, Rich JB, Normand SL, DeLong ER, Shewan CM, Dokholyan RS, Peterson ED, Edwards FH, Anderson RP, Society of Thoracic Surgeons Quality Measurement Task Force The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88:S2–22. doi: 10.1016/j.athoracsur.2009.05.053. [DOI] [PubMed] [Google Scholar]
- 21.Hosmer D, Lemeshow S. Applied Logistic Regression. 2nd ed: 2nd edition Wiley Inter-Science; 2000. [Google Scholar]
- 22.Hoen PW, Whooley MA, Martens EJ, Na B, van Melle JP, de Jonge P. Differential associations between specific depressive symptoms and cardiovascular prognosis in patients with stable coronary heart disease. J Am Coll Cardiol. 2010;56:838–844. doi: 10.1016/j.jacc.2010.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rothenbacher D, Hahmann H, Wusten B, Koenig W, Brenner H. Symptoms of anxiety and depression in patients with stable coronary heart disease: prognostic value and consideration of pathogenetic links. Eur J Cardiov Prev R. 2007;14:547–554. doi: 10.1097/HJR.0b013e3280142a02. [DOI] [PubMed] [Google Scholar]
- 24.Greillier L, Thomas P, Loundou A, Doddoli C, Badier M, Auquier P, Barlési F. The prediction of cardiac surgery outcome based upon preoperative psychological factors. Psychology & Health. 1996;11:471–477. [Google Scholar]
- 25.Tully PJ, Baker RA, Knight JL. Knight, Anxiety and depression as risk factors for mortality after coronary artery bypass surgery. Journal of Psychosomatic Research. 2008;64:285–290. doi: 10.1016/j.jpsychores.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Carney RM, Freedland KE, Miller GE, Jaffe AS. Depression as a risk factor for cardiac mortality and morbidity - A review of potential mechanisms. Journal of Psychosomatic Research. 2002;53:897–902. doi: 10.1016/s0022-3999(02)00311-2. [DOI] [PubMed] [Google Scholar]
- 27.Cohen BE, Marmar C, Ren L, Bertenthal D, Seal KH. Association of cardiovascular risk factors with mental health diagnoses in Iraq and Afghanistan war veterans using VA health care. JAMA. 2009;302:489–92. doi: 10.1001/jama.2009.1084. [DOI] [PubMed] [Google Scholar]
- 28.Druss BG, Bradford DW, Rosenheck RA, Radford MJ, Krumholz HM. Mental disorders and use of cardiovascular procedures after myocardial infarction. JAMA. 2000;283:506–511. doi: 10.1001/jama.283.4.506. [DOI] [PubMed] [Google Scholar]