Abstract
Men and women differ in exposure to trauma and the development of posttraumatic stress disorder (PTSD); however, research regarding sex differences in recovery from PTSD has been sparse. This study evaluated the treatment response trajectory for 69 male and female interpersonal assault survivors, using a modified Cognitive Processing Therapy (CPT) protocol that allowed survivors to receive up to18 sessions of CPT, with treatment end determined by therapy progress. Few sex differences were observed in trauma history, baseline PTSD and depressive severity, Axis I comorbidity, anger, guilt and dissociation. Women did report more sexual assault in adulthood and elevated baseline guilt cognitions, whereas men reported more baseline anger directed inward. Attrition and total number of sessions did not differ by sex. Over the course of treatment and follow-up, men and women demonstrated similar rates of change in PTSD and depressive symptoms. However, medium effect sizes on both of these primary outcomes at the 3-month follow-up assessment favored women. Several differences in the slope of change emerged on secondary outcomes such that women evidenced more rapid gains on global guilt, guilt cognitions, anger/irritability, and dissociation. Results suggest that male survivors may warrant additional attention to address these important clinical correlates.
Keywords: trauma recovery, sex differences, PTSD
Epidemiologic study suggests that there are multiple sex differences in exposure to trauma as well as in the subsequent development of posttraumatic stress disorder (PTSD). In the general population, 60% of men experience a traumatic event during their lifetime compared to 50% of women (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). With the exception of rape and sexual assault, men are more likely than women to experience every type of trauma (Kessler et al., 1995). The development of psychopathology subsequent to traumatic exposure differs by sex as well (Tolin & Foa, 2006). For example, PTSD (the most common psychopathology developed in response to a traumatic event; Resick, 2001) occurs disproportionately across the sexes such that women are twice as likely as men to develop the disorder (Breslau, Peterson, Poisson, Schultz, & Lucia, 2004; Kessler et al., 1995), and may be more likely to suffer a more chronic course of the disorder (Norris, Foster, & Weisshass, 2002). Meta-analytic study contributes to our understanding of sex differences in exposure to trauma and the development of PTSD in concluding that although males report an overall higher frequency of exposure to traumatic events, females are exposed more frequently to sexual assault across their lifespan (Tolin and Foa, 2006). As sexual assault is the trauma associated with the highest rates of PTSD, the elevated exposure to this specific type of assault may, in part, explain the disproportionate prevalence rates of PTSD in women. However, meta-analytic study has also demonstrated that the increased risk for PTSD in women cannot solely be attributed to differences in exposure to sexual assault as these sex differences remain when the type of trauma is controlled. Tolin and Foa (2006) suggest additional variables of interest to help explain the sex differences in the development of PTSD, including specific aspects of the traumatic event itself and differences in important clinical correlates of PTSD.
We can conclude that women are at a higher risk than men for exposure to interpersonal violence and the development of PTSD. Far less is understood regarding potential sex differences in the recovery process once PTSD has developed. Interpersonal violence results in the highest rates of PTSD when compared to other types of trauma (Kessler, 2000); however, most of the interpersonal violence research specifically focuses on rape, including female samples almost exclusively (Blain, Galovski, & Robinson, 2010). As a result, there is very little information at all on the recovery of male survivors of sexual assault suffering from PTSD. So, although approximately 3% to 12% of men experience a sexual assault in their lifetime (Fiebert & Osburn, 2001; National Institute of Justice, 1996; Porche, 2005), there is little empirical research assessing the generalizability of interventions for PTSD developed with female samples to their male counterparts. In fact, the extant treatment outcomes literature has been largely dichotomized by sex with the majority of all trauma studies focusing on either combat-related trauma (including primarily male samples or lacking statistical control for amount of combat exposure), or interpersonal physical assault and rape consisting primarily of female samples. Relatively fewer randomized clinical trials have included survivors of both sexes, even fewer have chosen to examine sex differences in either primary or secondary outcomes, and, to date, no study has been designed to specifically examine sex differences in recovery from PTSD (Blain, Galovski, & Robinson, 2010).
Of those studies that have examined sex differences, the results have been mixed. While most studies show similar treatment outcomes with regards to PTSD symptomatology (e.g., Basoglu, Salcioglu, & Livanou, 2007; Basoglu, Salcioglu, Livanou, Kalender, & Acar, 2005; Blanchard et al., 2003), some mixed trauma type studies indicate that women may realize greater treatment gains (e.g., Karatzias et al., 2007; Tarrier, Sommerfield, Pilgrim, & Faragher, 2000). Similarly, when attrition was compared in these studies, drop-out rates were generally comparable across men and women (Basoglu et al., 2005; Blanchard et al., 2003; Konuk, et al., 2006; Litz et al., 2007; Taylor et al., 2001) with some exceptions suggesting that males may be at higher risk to drop out of treatment prematurely (Lange, Rietdijk, et al., 2003; Sijbrandt et al., 2007; van Minnen, et al., 2002). Further confounding this comparison, most studies that have found significant sex differences in improvement of PTSD symptomatology have used mixed trauma samples in which men and women may have experienced very different traumas. Therefore, it is difficult to determine whether the study results are due to true sex differences, or to the potential confounding effect of trauma type.
Several important sex differences have been documented in the clinical presentation of PTSD-positive individuals. Sex differences across a variety of comorbid disorders and clinical correlates of PTSD including depression, guilt, anger, and dissociation (Olff, Langeland, Draijer, & Gersons, 2007) have been identified. Upwards of 30–50% of individuals suffering with PTSD also exhibit clinically significant symptoms of depression (Blanchard, Buckley, Hickling, & Taylor, 1998; Nixon, Resick, & Nishith, 2004; Kessler et al., 1995), with women more likely to endorse depressive symptoms (Tolin & Foa, 2006). Elevated guilt is also associated with PTSD severity (Beck et al., 2011; Kletter, Weems, & Carrion, 2009) in trauma survivors. Galovski, Mott, Young-Xu, and Resick, (2011) reported that male and female interpersonal assault survivors with PTSD experience guilt similarly, but self-blame cognitions which typically lead to feelings of guilt are elevated in women as compared to men (Tolin & Foa, 2006). Anger has also been identified as an important clinical correlate in PTSD-positive individuals (Olatunji, Ciesielski, & Tolin, 2010) and predicts both initial PTSD development (Meffert et al., 2008), and less successful treatment outcomes (Forbes et al., 2008). Sex differences in anger have emerged with men endorsing higher levels of anger compared to women (Castillo, Fallon, C’de Baca, Conforti, & Qualls, 2002). It is unclear, however, how the type of trauma experienced may affect this outcome as the Castillo study compared men who survived combat and suffered from PTSD to female survivors with sexual trauma-related PTSD. Anger has been shown to be higher in survivors of combat-related trauma, compared to other trauma types (Orth & Wieland, 2006). Thus, anger elevations observed in male combat samples may be better attributed to the type of trauma experienced as opposed to a true sex difference.
Finally, dissociation has also been identified as an associated feature of PTSD. Peritraumatic dissociation (dissociation that occurs during or immediately after the traumatic event) may be a risk factor for both the development of PTSD as well as for increased severity of PTSD symptomatology (e.g., Bremner & Brett, 1997; Dancu, Riggs, Hearst-Ikeda, Shoyer, & Foa, 1996). Women may be more likely than men to experience peritraumatic dissociation (Bryant & Harvey, 2003; Grieger, Fullerton, & Ursano, 2003) which may translate into increased risk for PTSD development and symptom severity (Bryant & Harvey, 2003; Fullerton et al., 2001). There is less information on sex differences in decreases in dissociation over the course of trauma-focused therapy.
Current Study
Men and women are clearly exposed to trauma differentially, develop psychopathology such as PTSD and depression at different rates, and present clinically with a host of PTSD concomitants such as guilt, anger and dissociation differentially. Far less is known about potential sex differences in treatment outcome, particularly in homogenous trauma samples of PTSD survivors. The current study was specifically designed to evaluate sex differences and, to our knowledge, represents the first study to implement an a priori design to test these differences in PTSD recovery. In an effort to reduce the possibility that sex differences may be attributable to multiple types of trauma found in mixed samples, the current study utilized a sample of treatment-seeking survivors of interpersonal violence (sexual and physical assault) only. First, the trauma histories of men and women were compared to assess similarities and differences across types of trauma (physical assault and sexual assault), onset of trauma (childhood and adulthood), and time since the traumatic event. It was hypothesized that men and women would describe similar overall trauma histories in this treatment-seeking sample. Next, in an effort to detect differences in initial clinical presentation, baseline PTSD severity, depressive severity, and the presence of comorbid Axis I disorders was compared across sexes. Finally, baseline differences across important clinical correlates such as guilt, anger, and dissociation were also compared. In accordance with the previous literature, we hypothesized that women would report elevated levels of depression and dissociation, while men would endorse more anger. We hypothesized that men and women would not differ significantly on overall PTSD severity and guilt.
This study then sought to assess differences in treatment retention, length of treatment necessary to reach study end state criteria, and rates of change across primary and secondary outcomes. Although findings regarding attrition rates have been mixed, we hypothesized that rates within our sample with a similar trauma history would be comparable. Considering the success of CPT in remediating PTSD and depressive symptoms in previous trials (Resick et al., 2002; Resick et al., 2008), it was hypothesized that CPT would be equally effective for male and female survivors of interpersonal trauma on these primary outcomes and that men and women would utilize a similar number of sessions to attain these outcomes. Finally, considering the scant literature suggesting that there may be sex differences in the experience of anger, guilt, and dissociation for men and women suffering from PTSD, we hypothesized that differences would emerge in the rate of change across these secondary outcomes.
Method
Participants and Procedure
Sixty-nine participants (22 men and 47 women) sought outpatient trauma-focused therapy following an interpersonal assault. All participants met full criteria for PTSD secondary to a sexual or physical assault as assessed by the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990). All participants were at least 3 months post-trauma at the time of the initial assessment, and there was no upper limit on time since trauma. Participants were required to be stable on medications for a period of 1-month, but were not excluded based on the use of psychiatric medication, and had to be out of any violent relationships for at least 3 months. Exclusion criteria included the presence of acute psychotic or manic symptoms, suicidal intent, or current substance dependence.
Participants were recruited from the greater St. Louis metropolitan via flyers, advertisements, referrals from local treatment providers and community agencies, and word-of-mouth. Interested participants completed a brief phone screen to determine eligibility, and those eligible were invited for an initial assessment during which they read and signed the informed consent. There were no adverse events and the single-site study was conducted with University of Missouri - St. Louis Institutional Review Board approval. Participants in the larger parent trail were randomized to a Modified CPT (MCPT) or to symptom monitoring, delayed treatment (SMDT). In the parent trial, participants who were initially randomized to SMDT were crossed over to MCPT following symptom monitoring, thus all participants eventually received the MCPT. For more detail regarding the larger trial see Galovski, Blain, Mott, Elwood, and Houle, (2012). The present study includes data from the full sample of individuals whom we intended to treat with MCPT (those initially randomized to MCPT and those who crossed over to MCPT following SMDT; N = 69). For those who crossed over from SMDT to MCPT, “pre-treatment” scores were taken from post-SMDT assessment (i.e., the assessment time point immediately prior to treatment).
During treatment, participant progress on PTSD and depressive symptoms was evaluated at each session using the Posttraumatic Stress Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997) and Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). One of the modifications to the original CPT protocol (Resick & Schnicke, 1993) was the ability to vary the length of therapy (dependent on client progress) versus the standard 12-session administration of the protocol. Specifically, participants could complete treatment as early as session 4, provided each of the following criteria was met: achievement of study end-state criterion (PDS ≤ 20 and BDI-II ≤ 18), agreement between the therapist and participant that treatment goals had been attained, and independent confirmation of participant’s negative PTSD status by a blind rater using the CAPS. Participants who did not meet the end-state criteria at the traditional end of the CPT protocol (session 12) could receive up to 6 additional sessions. Post-treatment assessments were completed 2 weeks after treatment (irrespective of number of sessions completed) and at a 3-month follow-up. Every effort was made to attain post-treatment data on treatment drop-outs. Blind raters conducted post-treatment and follow-up assessments. Participants were compensated for assessments ($50 for pre-treatment, $75 for post-treatment, and $100 for 3-month follow-up).
Measures
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1990) is clinician-administered diagnostic instrument which assesses the 17 symptoms of PTSD. Symptoms are rated on separate 5-point scales ranging from 0 (never) to 4 (daily or almost daily) for frequency and from 0 (none) to 4 (extreme) for intensity. Symptom items are summed to form a total score, such that higher scores indicate more severe PTSD symptoms (range 0 to 136). The CAPS has demonstrated excellent reliability and validity (Weathers, Keane, & Davidson, 2001). Internal consistency for the 17 PTSD symptoms in current study was high (α’s = .73 to .89) as was reliability among coders (κ [current diagnosis] = 1.00; r [total score] = .91).
Posttraumatic Stress Diagnostic Scale (PDS; Foa et al., 1997) is a self-report screening and diagnostic instrument which assesses the severity of PTSD symptoms. The 17 symptom items are rated on a 4-point scale from 0 (not at all/only one time) to 3 (5 or more times a week/almost always), with higher scores representing more frequent symptoms (range 0 to 51), and can be interpreted by the following clinical cutoffs: 0 = no rating, 1–10 = mild, 11–20 = moderate, 21–35 = moderate to severe, and >36 = severe. The PDS has demonstrated good sensitivity, specificity, and reliability (Foa et al., 1997). Internal consistency in the current study was high (α’s = .85 to .96).
Beck Depression Inventory-II (BDI-II; Beck et al., 1996) is a self-report measure of depressive symptoms. The 21 items are rated on a 4-point severity scale. Total scores are obtained by summing the items, with higher scores indicating increased depressive symptom severity (range 0 to 63), and can be interpreted by the following clinical cutoffs: 0–13 = minimal; 14–19 = mild; 20–28 = moderate; 29–63 = severe. The scale has well-established reliability and validity (Beck et al., 1996). Internal consistency was high in the current study (α’s = .90 to .96).
State-Trait Anger Expression Inventory (STAXI; Spielberger, 1991) is a self-report measure which assesses the experience, expression, and control of anger. The 44 items tap six primary subscales including state anger, trait anger, anger-in, anger-out, anger control, and anger expression. The present study utilized the anger-in, anger-out, and anger control subscales, which have been of particular interest in the PTSD literature (Olatunji et al., 2010; Orth & Wieland, 2006). For anger in and anger out, higher scores indicate more anger. Specifically, anger-in represents the degree to which angry feelings are experienced and suppressed or held in, whereas, anger-out measures the frequency with which angry feelings are experienced and outwardly expressed (i.e., aggressive behavior). Anger control taps the frequency of attempts to control the experience and expression of anger. Thus lower scores indicate less control (or higher symptoms).
Trauma Related Guilt Inventory (TRGI; Kubany et al., 1996) is a self-report measure which assesses the strength of experiences of guilt related to traumatic events. The 32 items are rated on a 5-point rating scale ranging from 4 (extremely true) to 0 (not at all true). The TRGI has three main scales: global guilt, distress, and guilt cognitions. Intercorrelations between TRGI scales and subscales range between r = .29 and .68, suggesting related but separate constructs are measured. Internal consistency in the initial study was high for each of the subscales (α’s ranged from .73 to .91) and test-re-test correlations were also high (ranging from r = .74 to .86). Internal consistency of the three primary scales was moderate to high in the current study (α’s = .72 to .94).
Trauma Symptom Inventory (TSI; Briere, 1995)
The TSI is a self-report measure developed to assess both short-term and long-term sequelae of traumatic experiences. The 100 items are rated on a scale from 0 (never) to 3 (often). The measure contains nine clinical scales, including Anxious Arousal, Anger-Irritability, Depression, Defensive Avoidance, Dissociation, Dysfunctional Sexual Behavior, Intrusive Experiences, Impaired Self-Reference, and Sexual Concerns. These scales had a mean alpha coefficient of .84–.87 in general, clinical, university, and military samples. The TSI exhibits convergent, predictive, and incremental validity in both clinical and non-clinical samples. The Anger-Irritability and Dissociation scales were used in the present study. Internal consistency for these scales was high in the current study (α’s = .83 to .91).
Structured Clinical Interview for DSM–IV Axis I Disorders — Patient Edition (SCID; First, Gibbon, Spitzer, & Williams, 1996) is a widely used semi-structured interview designed to assess DSM–IV Axis I diagnoses. The current study utilized the Mood, Anxiety, and Substance Use modules of the SCID. The SCID has well-established psychometrics (First et al., 1996). Inter-rater reliability in the current study was good (κ [all lifetime diagnoses] = 0.85; κ [all current diagnoses] = 0.74).
Analytical Strategy
Prior to assessing differences in response to treatment, chi-square and t-tests were used to compare men and women across a number of study variables to assess pre-treatment differences on demographics, trauma history, Axis I comorbidity, and the full range of treatment outcome variables. Chi-square and t-tests were then used to examine sex differences in drop-out from treatment and number of sessions utilized, respectively. Multilevel modeling was then utilized to analyze differences between sexes in treatment outcomes in the intent to treat (ITT) sample (N = 69) on pre-treatment, post-treatment, and follow-up time points. Multilevel modeling is ideal for studies employing repeated measurements nested within individuals and handles missing data by assuming that data is missing at random and generating missing data points based on the model fit (Singer & Willet, 2003). Post-hoc sensitivity power analysis indicated the obtained ITT sample achieved 80% power to detect even a relatively small interaction effect (i.e., sex*time; Cohen’s f = .17) and small to medium main effect of sex (Cohen’s f = .27).
The primary analyses were defined as sex differences on the primary treatment targets (i.e., the slopes of the CAPS, PDS, and BDI-II). To hold the primary analyses to the nominal level of statistical significance, a Bonferroni correction was applied to the slope parameters of these three outcomes (i.e., α = 0.05/3 = 0.016). On completion of the primary analyses, secondary analyses were conducted to assess the influence of the intervention on additional clinical correlates using the STAXI (anger-in, anger-out, and anger control subscales), TRGI (global guilt, distress, and guilt cognition scales), and TSI (anger-irritability and dissociation scales).
Analysis of each DV was conducted using the following contingent steps (Singer & Willet, 2003): 1) analyze the variation in the DV to assess variance attributable to individuals versus change over time, 2) model change in the DV (i.e., linear versus quadratic), 3) determine if the slopes are random (i.e., individuals change differently), 4) determine if sex moderates individual change, and 5) replicate models using polynomial coding of time to reduce multicolinearity. Raw coding of the polynomials (Time, Time2) was used for increased interpretability (Biesanz, Deeb-Sossa, Papadakis, Bollen, & Curran, 2004), according to the following scheme: 0 (pre-treatment), 1 (post-treatment), and 2 (3-month follow-up). Several variants of this model were tested in a tear-down procedure (Cohen, Cohen, Aiken, & West, 2003) to determine whether growth was linear or quadratic (level 1). Models were then replicated using polynomial coding. Sex was dummy coded (with male as the reference group) and tested as a predictor of group differences in change across several important clinical outcomes (level 2). Randomization was effective as no demographic or primary outcome variable had different baseline values by sex (p > 0.25), thus no variables were controlled in the present analyses.
An ITT philosophy was used for creation of the primary outcome models. Although 69 participants were enrolled, 11 of these did not complete a follow-up assessment. All 11 participants who had follow-up data missing were treatment drop-outs. There was no difference in missing data between men and women (χ2 (1; N = 69) = .12, p = .728). As a final step, we replicated models using only the treatment completer sample (n = 50) to ensure that treatment dropouts did not unduly influence the model results. Modeling analyses were completed using the Linear and Nonlinear Mixed Effects Models package from R (Pinhero, Bates, DebRoy, & Sarkar, 2006). Effect sizes presented in Table 2 reflect sex differences in change over the full study period (pre-treatment to follow-up) and are based on Feingold’s (2009) computation for between group differences (equation 5, p. 6).
Table 2.
Pre-, Post-treatment, and Follow-up Values by Gender across Measured Outcome Variables in the ITT MCPT Sample
| Pre-treatment | Post-treatment | Follow-up | ESa | ||||
|---|---|---|---|---|---|---|---|
| Men (n = 22) | Women (n = 47) | Men (n = 18) | Women (n = 40) | Men (n = 17) | Women (n = 40) | ||
| CAPS Total | 75.68 (16.85) | 70.96 (18.24) | 34.06 (31.02) | 23.40 (20.01) | 33.18 (30.65) | 19.70 (19.74) | −0.293 |
| PDS Total | 31.38 (7.90) | 31.13 (9.46) | 15.94 (15.19) | 11.03 (12.19) | 18.67 (16.00) | 10.51 (12.13) | −0.573 |
| BDI-II Total | 29.00 (12.14) | 30.34 (11.96) | 14.28 (14.11) | 10.26 (10.92) | 15.76 (15.19) | 10.41 (12.36) | −0.583 |
| STAXI | |||||||
| Anger-in | 22.00*p (5.03) | 19.05 (3.96) | 17.67 (5.49) | 16.14 (4.38) | 19.50 (5.97) | 15.64 (4.30) | −0.363 |
| Anger-out | 15.39 (4.34) | 15.14 (4.40) | 13.11 (3.29) | 13.41 (3.27) | 15.06 (4.23) | 12.81 (3.51) | −0.463 |
| Anger-control | 21.21 (5.60) | 21.75 (5.99) | 23.59 (6.17) | 23.26 (5.76) | 24.00 (4.57) | 23.34 (6.59) | −0.233 |
| TRGI | |||||||
| Global guilt | 1.92 (1.35) | 2.47 (1.21) | 1.15 (1.23) | 1.43 (1.12) | 1.66 (1.61) | .95*m (.88) | −1.073 |
| Distress | 2.87 (.77) | 3.16 (.71) | 2.01 (.97) | 2.25 (.96) | 2.25 (1.20) | 2.14 (.89) | −0.633 |
| Guilt cognitions | 1.26*p (.56) | 1.60 (.80) | .86 (.48) | 1.01 (.71) | 1.08 (.83) | .79*m (.43) | −0.693 |
| TSI | |||||||
| Anger/Irritability | 11.60 (5.83) | 12.63 (6.75) | 7.00 (6.53) | 6.25 (5.90) | 9.13 (7.27) | 5.22*m (5.08) | −0.673 |
| Dissociation | 12.20 (4.51) | 10.54 (5.45) | 9.24 (7.36) | 3.59 (3.51) | 9.47 (6.84) | 3.74*m (4.40) | −0.643 |
Note: CAPS = Clinician Administered PTSD Scale; BDI-II = Beck Depression Inventory-II; PDS = Posttraumatic Stress Diagnostic Scale; STAXI = State-Trait Anger Expression Inventory; TRGI = Trauma-Related Guilt Inventory; TSI = Trauma Symptom Inventory.
Effect sizes reflect differences by sex between pre-treatment and follow-up using Feingold’s (2009) computation for between group differences (equation 5, p. 6).
p < .05 (main effect of sex at pre-treatment);
p < .05 (moderation effect of sex over time)
This particular study design was complex with regard to power estimation. Change was expected to be non-linear (initial rate of change flattens from post to follow-up measurement). This rendered power estimation via the multilevel models difficult (see Feingold, 2009 and Raudenbush & Liu, 2001). Using a repeated measures ANOVA approach, we estimated that the given data (number of observations = 184) and study design (2 groups, 3 repeated measurements) in the ITT sample had power 99% to detect a medium effect. The power to detect a small effect was much less (27%), but the ITT sample size should detect an effect of modest size (between ‘small’ and ‘medium’, ES = .05) at 80% power. The completer only sample (n = 50), had 90% power to detect a medium effect size and the effect size detectable at 80% power was .051 (similar to the full sample). These analyses are thus limited in their power to detect gender differences at smaller effect sizes and should be considered conservative. The multilevel strategy used in this study produces more power than repeated measures ANOVA for a number of reasons (e.g., no need to eliminate partial data, better equipped to model nonlinearity). Therefore, given the data being analyzed, this study should have sufficient power to detect meaningful group differences effect on change should they exist.
Results
Participants demographic and trauma history comparisons by gender can be found in Table 1. Demographics did not differ by sex. Overall, participants reported a complex trauma history, with lifetime endorsements of child sexual abuse (64%), child physical abuse (57%), adult sexual assault (51%), and adult physical assault (65%). As can be seen in Table 1, lifetime trauma history did not differ by sex, except that women endorsed a higher incidence of adult sexual assault. All participants selected an index event, or worst traumatic event, for the focus of treatment. Similarly, there was no difference in time since the index event between men and women.
Table 1.
Pre-treatment Demographic and Trauma History Comparisons by Gender in the ITT MCPT Sample
| Men (n = 22) | Women (n = 47) | t or χ2 | p | |
|---|---|---|---|---|
| Age | 40.27 | 40.55 | −.10 | .9253 |
| Years of Education | 12.82 | 13.43 | −.84 | .4053 |
| Single | 14 (64%) | 24 (51%) | 2.52 | .2843 |
| Caucasian | 12 (55%) | 22 (47%) | .36 | .5493 |
| Household Income Under 20,000 | 14 (64%) | 29 (62%) | .004 | .9483 |
| Lifetime CSA | 12 (55%) | 28 (60%) | .16 | .693 |
| Lifetime CPA | 9 (41%) | 23 (49%) | .22 | .6433 |
| Lifetime ASA | 5 (23%) | 29 (62%) | 8.34 | .004**3 |
| Lifetime APA | 13 (59%) | 29 (62%) | .0001 | .9873 |
| Index Event CSA | 8 (36%) | 21 (45%) | .42 | .514 |
| Index Event CPA | 5 (23%) | 6 (13%) | 1.11 | .2923 |
| Index Event ASA | 2 (9%) | 12 (26%) | 2.51 | .1143 |
| Index Event APA | 7 (32%) | 8 (17%) | 1.93 | .1653 |
| Time Since Trauma (months) | 235.27 | 244.96 | −.20 | .842 |
Note:
p < .001
With respect to Axis I comorbidity, the SCID was used to assess the presence of comorbid Axis I disorders. The majority of participants (79.6%) met criteria for at least one current comorbid disorder at pre-treatment, with major depressive disorder (48%), generalized anxiety disorder (GAD; 25%), social phobia (22%), obsessive compulsive disorder (OCD; 16%), and panic disorder (16%) being the most commonly diagnosed disorders. No sex differences emerged on these diagnoses, (χ2= .40 – 1.51, ps < .43 – .73). Current alcohol and substance dependence were exclusion criteria for the study. No sex differences emerged on past alcohol dependence (χ2 (1; N = 69) = .23, p = .64) with 29.4% of the total sample meeting criteria for past alcohol dependence. Approximately one-third of the sample (28.1%) met criteria for past substance dependence with no differences between men and women (χ2 (1; N = 69) = .05, p = .82). Finally, a lifetime history of MDD was assessed and the majority (78%) of the participants had experienced past MDD, with women endorsing higher rates of past MDD (χ2 (1; N = 69) = .4.06, p = .04).
Treatment Outcomes
Of the 69 participants (22 men and 47 women) who began CPT, 19 dropped out (8 men, 11 women). Sex did not differ significantly across drop-outs (χ2 (1; N = 69) = 1.26, p = .261, Cramer’s V = .14). Of the 69 participants in ITT MCPT sample, 22 (6 men, 16 women) were crossovers, having completed SMDT prior to MCPT. Original treatment condition (SMDT vs MCPT) did not differ by gender (χ2 (1; N = 69) = .57, p = .782, Cramer’s V = .07). Completers utilized between 4 and 18 sessions with no sex differences in length of treatment necessary to achieve study end state criteria, averaging 11.43 sessions for men and 10.58 sessions for women (t = .60, p = .55). Of the 50 completers, 46 participants reached the a priori defined end state criteria by session 18 (the maximum allowable number of sessions). Two of the 4 remaining participants continued to improve over the three-month follow-up interval, leaving only 2 (4% of treatment completers) PTSD positive at the 3-month follow-up. Both of these treatment non-responders were males.
Primary outcomes: PTSD and depressive symptoms
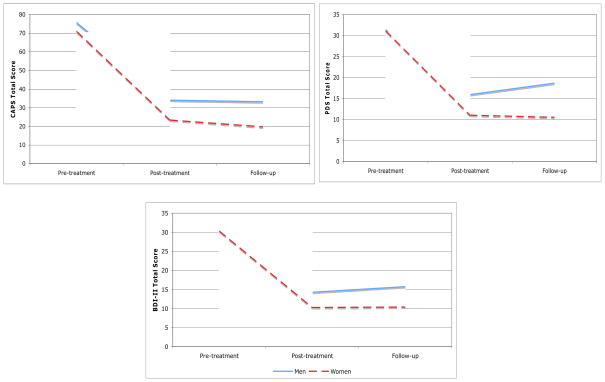
Participants in the MCPT treatment sample evidenced significant reductions on primary outcome measures (CAPS, PDS, and BDI-II; ts = −8.38 to −8.63, ps < .0001) of PTSD and depression. All tested outcomes followed a quadratic pattern of change, with more rapid initial gains being followed by a slowing of change (or maintenance of gains; ts = 7.51 to 7.60, ps < .0001). As can be seen in Figure 1, both male and female participants entered treatment reporting similar levels of distress (ts = −.08 to −1.57, ps = .12 to .42) and demonstrated similar trajectories in change over the course of the study (ts = −.84 −1.75, ps = .08 to .40 [linear] and ts = −.45 to .73; ps = .47 to .69 [quadratic]) on the primary outcome variables. Table 2 displays changes in actual scores and effect sizes across sexes in the ITT MCPT sample. Although sex did not significantly moderate treatment outcomes, effect sizes (ESs) ranged from −.29 to −.58, such that women reported non-significantly better outcomes than men between pre-treatment and the 3-month follow-up.
Figure 1.
Means of primary outcomes by sex in the ITT sample.
Secondary outcomes: Anger, guilt, and dissociation
Overall, the study participants evidenced statistically significant reductions on secondary outcome measures. Anger (anger in, anger out, anger control: STAXI & anger/irritability: TSI), guilt (global guilt, guilt-related distress, guilt cognitions: TRGI), and dissociation (TSI) demonstrated a quadratic pattern of change, with more rapid initial gains (linear function) being followed by a slowing of change (quadratic function) over the follow-up interval (or maintenance of gains; (STAXI, TRGI, and TSI; ts = −2.88 to −6.42, ps < .0001 [linear], ts = 2.12 to 4.36, ps = .036 to .0001 [quadratic]). Anger control marked an exception to the quadratic pattern of change observed on all other outcomes such that it demonstrated a linear pattern of change over the entire study period during which participants steadily increased on their anger control (t = 2.78, p = .011).
Multilevel modeling was used to assess response efficiency across sexes. The pattern of response varied greatly among tested clinical correlates (see Table 2). Two pre-treatment differences were noted. Specifically, guilt cognitions demonstrated a difference by sex at pre-treatment, such that women endorsed more guilt cognitions than men at pretreatment (t = −2.00, p = .049), whereas anger-in was significantly higher among men (t = 2.30, p = .028). Several clinical correlates demonstrated differential change over time by sex. Specifically, women evidenced more rapid gains than men on global guilt (t = −4.41, p < .001, ES −1.07), guilt cognitions (t = −2.76, p = .007, ES = −.69), anger irritability (t = −3.13, p = .002, ES = −.67), and dissociation (t = −2.43, p = .017, ES = −.64). The remaining tested outcomes did not differ by gender (anger-in, anger-out, anger control, and guilt distress; ts = −.75 to −1.64, ps = .10 to .45, ESs = −.23 to −.63). Of note, secondary outcomes followed a quadratic pattern of change, with more rapid initial gains being followed by a slowing of change (or maintenance of gains) with the exception of anger control (described above). No sex differences were observed in the quadratic function for any variable that demonstrated an overall pattern of quadratic change (ts = −1.45 to .18, ps = .15 to .87). Thus, although men and women differed in their initial rate of change over the study period, their maintenance of gains was similar across those measures.
Completer analyses (n = 50) overall revealed a largely consistent pattern of results with significant differences across sexes emerging on change in global guilt and anger/irritability. However, two previously significant interaction effects remained only marginally significant in the completer sample: guilt cognitions (t = −1.87, p = .066, ES = −.50) and dissociation (t = −1.87, p = .065, ES = −.70). Although not meeting criteria for statistical significance (t = −1.93, p = .056), guilt distress emerged with a large effect size in the completer sample (ES = −1.02). It is noteworthy that the effect sizes for these results were in the medium to large range, indicating that loss of power may have affected the statistical significance of these analyses.
Discussion
Although sex differences have been detected in exposure to trauma and in the subsequent development of PTSD, the paucity of research on potential differences in the recovery from this debilitating disorder is apparent in a review of the treatment outcomes literature (Blain, Galovski, & Robinson, 2010). The handful of existing studies examining sex differences are confounded by mixed trauma type, rendering interpretation of sex disparities in outcomes difficult to attribute to sex versus trauma experience. In addition to the lack of direct comparison across sexes, there is an overall dearth of information on the recovery process of male interpersonal assault survivors in totality. Thus, the generalizability of PTSD interventions assessed primarily within female interpersonal assault samples to their male counterparts has been largely untested. The preponderance of PTSD research examining the effectiveness of psychosocial interventions with male samples primarily consists of survivors of combat trauma. As combat and interpersonal violence are qualitatively different experiences, the generalizability of treatment results from male combat survivors to treatment outcomes with male survivors of sexual and physical violence is also difficult to estimate. Thus little information is currently available regarding the recovery of male assault survivors who suffer from PTSD.
This study sought to address this substantial hole in the larger PTSD treatment outcomes literature by identifying similarities and differences in change in PTSD and depressive symptoms and related clinical correlates between men and women through a course of Cognitive Processing Therapy (CPT). These results should be interpreted with caution due to the low male sample size and the potential for Type II error. Power analyses revealed 80% power to detect a medium effect size in the ITT sample (.050) and in the completer sample (.051). Therefore, Type II error is elevated for small effects in the current analyses. Descriptive statistics and effect size estimates will also be considered in the interpretation of the limited power in the present data.
Men and women entered the study with remarkably similar demographic and clinical presentations. Interestingly, both sexes reported quite similar trauma histories particularly in childhood. Once study participants reached adulthood, the majority of them (65%) reported adult physical assaults at similar rates; however, the women reported significantly more adult sexual traumas. Participants were asked to choose the worst event (index trauma) as the focus of treatment, and men and women did not differ with respect to choice of index trauma. The majority of survivors chose a childhood event as their index event, particularly a sexual assault, suggesting similarities in the perception of severity of childhood events over those that occur in adulthood. In addition to relatively complex and chronic trauma histories, both men and women described significant psychiatric distress such that the majority of the sample met criteria for at least one Axis I comorbid disorder. Specifically, and in addition to PTSD, men and women similarly endorsed current comorbid MDD and a range of comorbid anxiety disorders including GAD, PD, OCD, and social phobia. In summary, men and women in this study looked remarkably similar psychiatrically, demographically, and with respect to trauma history.
These similarities continued in our evaluation of sex differences in primary treatment outcomes. There were no differences in attrition or in the efficiency of response to treatment, suggesting that CPT was equally amenable to both men and women and that, overall, sex did not influence the duration of the treatment required to reach study end state criteria. The rate of change on PTSD and depression also did not differ statistically, suggesting excellent generalizability on these primary outcomes to male survivors of interpersonal violence. Despite the lack of statistically significant differences in rates of change on these indices, we did see small to medium effect size differences favoring women on PTSD and depression respectively. Inspection of individual scores may help in the interpretation of these effects. As described above, participants’ conclusion of treatment in this trial was determined by individual progress in therapy such that individuals were considered successful completers when they achieved the specific end state criteria defined above. If those criteria were not yet met at session 12 (the end of the original CPT protocol), participants could receive up to an additional 50% more therapy (six additional sessions for a possible maximum of 18 sessions). Of the 50 completers, only 4 individuals did not achieve that end state criteria by session 18 and were still PTSD positive at the end of treatment. Two of those 4 individuals continued to improve over the follow-up interval and were PTSD negative at the 3-month assessment resulting in a total of 2 out of 50 treatment completers remaining PTSD positive at the end of the study. These two individuals are both males. Given the relatively small study sample, these two males’ scores may be contributing to the effect size favoring women in overall PTSD and depression outcomes at the 3-month follow-up. Overall, the rates of change across sexes were similar and suggest that CPT is a viable treatment option for male survivors of interpersonal assault suffering from PTSD.
Differences in initial presentation of our secondary outcomes were a bit more variable. Men and women were compared across a number of variables with observed baseline sex differences in previous research. In our sample, men and women reported similar initial levels of symptomatology on guilt, anger, and dissociation with two exceptions. Specifically, women endorsed more guilt cognitions than men and the reverse was true for anger directed inward. Previous study (Galovski et al., 2011) had shown equivalent reports of baseline guilt between men and women and these results were replicated here on the measure of guilt distress and global guilt. The current study’s finding that women may engage in more guilt cognitions was not found in our previous study, but a similar finding was reported in Tolin & Foa (2006) as women described more self-blame cognitions. Taken together, these two studies may suggest that women are engaging in a qualitatively different cognitive process in interpreting their traumatic event, perhaps resulting in more self-blame with subsequent feelings of guilt. CPT, with its primary emphasis on identifying and resolving trauma-related, self-blame cognitions early in therapy, is well-poised to target this particular clinical correlate of PTSD. Future research may try to identify variations across sexes in cognitive processes and schemas that result in guilt-related cognitions. Identifying sex differences in these areas may guide clinicians in querying trauma-related topics that may be more salient for men than women and vice versa.
Interestingly anger directed inward was more pronounced in men than in women prior to treatment. Meta-analytic study has revealed that anger-out, anger-in and anger control are specifically and uniquely associated with PTSD such that the relationship is stronger between these types of anger and PTSD than with any other type of anxiety disorder (Olatunji, Ciesielski, & Tolin, 2010). Chemtob, Novaco, Hamada, Gross, & Smith (1997) suggest that the chronic psychophysiological arousal in PTSD primes the individual to experience and display anger readily. Supporting this hypothesis, research in veteran samples has found that elevated anger is related to the presence of PTSD as opposed to exposure to combat alone and/or military training or predisposing personality factors (McFall, Wright, Donovan, & Raskind, 1999). If elevated anger is more a universal correlate of PTSD (it is a symptom of PTSD), then men and women diagnosed with PTSD should experience anger similarly. Contradicting the notion that elevated anger may be characteristic of PTSD irrespective of the type of trauma experienced, Castillo et al. (2002) reported sex differences such that male survivors of combat trauma endorsed heightened anger as compared to female sexual assault survivors. Results from this study are incongruent with the Castillo et al. study given that men and women in the current study endorsed anger directed outward and anger control similarly. Men in our study did report more baseline anger directed inward than did the women. Locating our results in the larger PTSD literature, it appears that the type of trauma experienced by the participant may play a role in the development and manifestation of anger, such that the experience of combat trauma as well as military training, etc. may explain the sex difference in anger observed in the Castillo et al. study (at least in part) as opposed to solely a sex difference.
The intent to treat analyses revealed differences in the rate of change on global guilt, guilt cognitions, anger/irritability, and dissociation, with all differences suggesting that women improve more rapidly on these outcomes. A possible explanation for these differences may be subtle variations in the presentation of these clinical correlates such that the manifestation and/or reporting of feelings of guilt and dissociation may be more apparent in women. Additional queries and probing might be helpful in detecting manifestations of these symptoms in male survivors of interpersonal violence. Consistent results emerged on global guilt and dissociation when the same analyses were conducted with the treatment completer sample. The sex differences observed in guilt cognitions and dissociation remained marginally significant when assessed in the completer sample. However, effect sizes calculated in the completer sample did not show similar reductions, with women evidencing greater treatment gains than men at a medium effect size on multiple secondary outcomes, leaving us to consider the possibility of compromised statistical power as the reason for the reduced statistical significance. These results must be interpreted cautiously in light of the limited statistical power. However, they provide initial evidence that men may need additional treatment to facilitate the reduction of secondary emotions. Further, previous study has suggested that emotional dysregulation may be particularly problematic in survivors of interpersonal violence and, perhaps specifically, in the aftermath of childhood abuse. Although not specifically assessed in this study, future research may consider potential sex differences in emotional regulation strategies given the observed differences in secondary emotions detected in this study.
Overall, our results indicated that men and women improved similarly, consistently showing decreases in symptoms across treatment with good maintenance of treatment gains over the long-term, follow-up interval. An exception to this pattern of change was observed on the measure of anger control. It appeared that, for men and women alike, control over one’s anger continued to improve steadily even after the conclusion of treatment. This continued improvement may suggest that control over one’s anger may be influenced immediately by the intervention (as indicated by the increase in anger control over the course of treatment), but also continue to improve, perhaps as a function of improvements in other symptom domains. The resolution of PTSD, depression, guilt, dissociation and other types of anger by treatment’s end may influence the continued improvement on the ability to control one’s anger observed across the follow-up interval.
These results are very encouraging, suggesting good generalizability of treatment efficacy to male survivors of interpersonal violence. This study is not without its limitations. Our sample was small, particularly with respect to males. Recruitment of male survivors of interpersonal violence remains difficult, potentially due to the many barriers to reporting the crimes and seeking treatment that may be somewhat unique to male survivors. Such barriers include expectations for males to be more self-reliant and dominant, societal belief that early sexual experiences for males are normal and even desired, and the fear of being labeled as homosexual in the case of a male perpetrator (Nasjleti, 1980, Finkelhor, 1981; Rew & Esparza, 1990). Also, this study specifically assessed sex differences in interpersonal assault survivors. Future research should consider including different types of traumas in a larger study such that differential symptom elevations and rates of change may be attributed appropriately to sex differences or to trauma type. Such information would be invaluable in continuing to hone our successful interventions to capture the nuances of the individual seeking treatment.
Acknowledgments
This work was supported by a National Institute of Mental Health (NIMH) 1R34MH074937 grant awarded to Tara E. Galovski at the University of Missouri- St. Louis. We thank the clinicians and research assistants whose work to make this research possible and the generous individuals who participated in these trials.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tara E. Galovski, Email: galovskit@msx.umsl.edu, University of Missouri-St. Louis.
Leah M. Blain, Email: leahblain@umsl.edu, University of Missouri-St. Louis.
Courtney Chappuis, Email: ckchappuis@mail.umsl.edu, University of Missouri-St. Louis.
Thomas Fletcher, Email: t.d.fletcher@comcast.net.
References
- Basoglu M, Salcioglu E, Livanou M. A randomized controlled study of single-session behavioural treatment of earthquake-related post-traumatic stress disorder using an earthquake simulator. Psychological Medicine. 2007;37:203–213. doi: 10.1017/S0033291706009123. [DOI] [PubMed] [Google Scholar]
- Basoglu M, Salcioglu E, Livanou M, Kalender D, Acar Gnl. Single-session behavioral treatment of earthquake-related posttraumatic stress disorder: A randomized waiting list controlled trial. Journal of Traumatic Stress. 2005;18:1–11. doi: 10.1002/jts.20011. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beck JG, McNiff J, Clapp JD, Olsen SA, Avery ML, Hagewood JH. Exploring negative emotion in women experiencing intimate partner violence: Shame, guilt, and PTSD. Behavior Therapy. 2011;42:740–750. doi: 10.1016/j.beth.2011.04.001. [DOI] [PubMed] [Google Scholar]
- Biesanz JC, Deeb-Sossa N, Papadakis AA, Bollen KA, Curran PJ. The role of coding time in estimating and interpreting growth curve models. Psychological Methods. 2004;9:30–52. doi: 10.1037/1082-989X.9.1.30. [DOI] [PubMed] [Google Scholar]
- Blain LM, Galovski TE, Robinson T. Gender differences in recovery from posttraumatic stress disorder: A critical review. Aggression and Violent Behavior. 2010;15:463–474. doi: 10.1016/j.avb.2010.09.001. [DOI] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, et al. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. The Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Blanchard EB, Buckley TC, Hickling EJ, Taylor AE. Posttraumatic stress disorder and comorbid major depression: Is the correlation an illusion? Journal of Anxiety Disorders. 1998;12:21–37. doi: 10.1016/S0887-6185(97)00047-9. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Hickling EJ, Devineni T, Veazey CH, Galovski TE, Mundy E, et al. A controlled evaluation of cognitive behavioral therapy for posttraumatic stress in motor vehicle accident survivors. Behaviour Research and Therapy. 2003;41:79–96. doi: 10.1016/S0005-7967(01)00131-0. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Brett E. Trauma-related dissociative states and long-term psychopathology in posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10:37–49. doi: 10.1002/jts.2490100105. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating posttraumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychological Medicine. 2004;34:889–898. doi: 10.3109/00048670903393597. [DOI] [PubMed] [Google Scholar]
- Briere J. Trauma Symptom Inventory Professional Manual. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Bryant RA, Harvey AG. Gender differences in the relationship between acute stress disorder and posttraumatic stress disorder following motor vehicle accidents. Australian and New Zealand Journal of Psychiatry. 2003;37:226–229. doi: 10.1046/j.1440-1614.2003.01130.x. [DOI] [PubMed] [Google Scholar]
- Castillo DT, Fallon SK, C’de Baca J, Conforti K, Qualls C. Anger in PTSD: General psychiatric and gender differences on the BDHI. Journal of Loss & Trauma. 2002;7:119–128. doi: 10.1080/153250202753472282. [DOI] [Google Scholar]
- Chemtob CM, Novaco RW, Hamada RS, Gross DM, Smith G. Anger regulation deficits in combat-related posttraumatic stress disorder. Journal of Traumatic Stress. 1997;10(1):17–36. doi: 10.1023/a:1024852228908. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation Analysis for the behavioral Sciences. 3. Hillsdale, NJ: Erlbaum Press; 2003. [Google Scholar]
- Dancu CV, Riggs DS, Hearst-Ikeda D, Shoyer BG, Foa EB. Dissociative experiences and posttraumatic stress disorder among female victims of criminal assault and rape. Journal of Traumatic Stress. 1996;9:253–267. doi: 10.1002/jts.2490090208. [DOI] [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiebert MS, Osburn K. Effects of gender and ethnicity on self reports of mild, moderate, and severe sexual coercion. Sexuality & Culture. 2001;5:3–11. doi: 10.1007/s12119-001-1015-2. [DOI] [Google Scholar]
- Finkelhor D. The sexual abuse of boys. Victimology: An International Journal. 1981;6:76–84. [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM–IV (SCID) New York: New York State Psychiatric Institute, Biometrics Research Department; 1996. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. doi: 10.1037//1040-3590.9.4.445. [DOI] [Google Scholar]
- Forbes D, Parslow R, Creamer M, Allen N, McHugh T, Hopwood M. Mechanisms of anger and treatment outcome in combat veterans with posttraumatic stress disorder. Journal of Traumatic Stress. 2008;212:142–149. doi: 10.1002/jts.20315. [DOI] [PubMed] [Google Scholar]
- Fullerton CS, Ursano RJ, Epstein RS, Crowley B, Vance K, Kao T-C, et al. Gender differences in posttraumatic stress disorder after motor vehicle accidents. American Journal of Psychiatry. 2001;158:1486–1491. doi: 10.1176/appi.ajp.158.9.1486. [DOI] [PubMed] [Google Scholar]
- Galovski TE, Blain LM, Mott JM, Elwood L, Houle T. Manualized Therapy for PTSD: Flexing the Structure of Cognitive Processing Therapy. Journal of Consulting and Clinical Psychology. 2012 doi: 10.1037/a0030600. (Pagination pending, online first) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galovski TE, Mott J, Young-Xu Y, Resick PA. Gender differences in the clinical presentation of PTSD and its concomitants in survivors of interpersonal assault. Journal of Interpersonal Violence. 2011;26(4):789–806. doi: 10.1177/0886260510365865. [DOI] [PubMed] [Google Scholar]
- Grieger TA, Fullerton CS, Ursano RJ. Posttraumatic stress disorder, alcohol use, and perceived safety after the terrorist attack on the Pentagon. Psychiatric Services. 2003;54:1380–1382. doi: 10.1176/appi.ps.54.10.1380. [DOI] [PubMed] [Google Scholar]
- Karatzias A, Power K, McGoldrick T, Brown K, Buchanan R, Sharp D, et al. Predicting treatment outcome on three measures of post-traumatic stress disorder. European Archives of Psychiatry and Clinical Neuroscience. 2007;257:40–46. doi: 10.1007/s00406-006-0682-2. [DOI] [PubMed] [Google Scholar]
- Kessler R. Posttraumatic stress disorder: The burden to the individual and to society. Journal of Clinical Psychiatry. 2000;61:4–12. [PubMed] [Google Scholar]
- Kessler R, Sonnega A, Bromet E, Hughes M, Nelson C. Posttraumatic stress disorder in the National Comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kletter H, Weems CF, Carrion VG. Guilt and posttraumatic stress symptoms in child victims of interpersonal violence. Clinical Child Psychology and Psychiatry. 2009;14:71–83. doi: 10.1177/1359104508100137. [DOI] [PubMed] [Google Scholar]
- Konuk E, Knipe J, Eke I, Yuksek H, Yurtsever A, Ostep S. The effects of Eye Movement Desensitization and Reprocessing (EMDR) therapy on posttraumatic stress disorder in survivors of the 1999 Marmara, Turkey, earthquake. International Journal of Stress Management. 2006;13(3):291–308. doi: 10.1037/1072-5245.13.3.291. [DOI] [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI) Psychological Assessment. 1996;8(4):428–444. doi: 10.1037//1040-3590.8.4.428. [DOI] [Google Scholar]
- Lange A, Rietdijk D, Hudcovicova M, van de Ven JP, Schrieken B, Emmelkamp PMG. Interapy: A controlled randomized trial of the standardized treatment of posttraumatic stress through the internet. Journal of Consulting and Clinical Psychology. 2003;71:901–909. doi: 10.1037/0022-006X.71.5.901. [DOI] [PubMed] [Google Scholar]
- Litz BT, Engel CC, Bryant RA, Papa A. A randomized, controlled proof-of-concept trial of an internet-based, therapist-assisted self-management treatment for posttraumatic stress disorder. American Journal of Psychiatry. 2007;164(11):1676–1683. doi: 10.1176/appi.ajp.2007.06122057. [DOI] [PubMed] [Google Scholar]
- McFall ME, Wright PW, Donovan DM, Raskind M. Multidimensional assessment of anger in Vietnam veterans with posttraumatic stress disorder. Comprehensive Psychiatry. 1999;40(3):216–220. doi: 10.1016/s0010-440x(99)90006-8. [DOI] [PubMed] [Google Scholar]
- Meffert SM, Metzler TJ, Henn-Haase C, McCaslin S, Inslicht S, Chemtob C, et al. A prospective study of trait anger and PTSD symptoms in police. Journal of Traumatic Stress. 2008;21:410–416. doi: 10.1002/jts.20350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nasjleti M. Suffering in silence: The male incest victim. Child Welfare. 1980;59:269–275. [PubMed] [Google Scholar]
- National Institute of Justice. Victim costs and consequences: A new look. Washington, D.C: U.S. Department of Justice; 1996. [Google Scholar]
- Nixon RD, Resick PA, Nishith P. An exploration of comorbid depression among female victims of intimate partner violence with posttraumatic stress disorder. Journal of Affective Disorders. 2004;82:315–320. doi: 10.1016/j.jad.2004.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, Foster JD, Weisshass DL. The epidemiology of sex differences in PTSD across developmental, societal, and research contexts. In: Kimmerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York: Guilford Press; 2002. pp. 3–42. [Google Scholar]
- Olatunji BO, Ciesielski BG, Tolin DF. Fear and loathing: A meta-analytic review of the specificity of anger in PTSD. Behavior Therapy. 2010;41:93–105. doi: 10.1016/j.beth.2009.01.004. [DOI] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, Gersons BPR. Gender differences in posttraumatic stress disorder. Psychological Bulletin. 2007;133:183–204. doi: 10.1037/0033-2909.133.2.183. [DOI] [PubMed] [Google Scholar]
- Orth U, Wieland E. Anger, hostility and posttraumatic stress disorder in trauma- exposed adults: A meta-analysis. Journal of Consulting and Clinical Psychology. 2006;74:698–706. doi: 10.1037/0022-006X.74.4.698. [DOI] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, DebRoy S, Sarkar D. NLME: Linear and nonlinear mixed effects models [Computer software and manual] 2006 Retrieved from www.cran.r-project.org/
- Porche DJ. Male sexual assault: History, description, epidemiology, and clinical presentation. The Journal for Nurse Practitioners. 2005;1:196–197. doi: 10.1016/j.nurpra.2005.10.012. [DOI] [Google Scholar]
- Raudenbush SW, Liu XF. Effects of study duration, frequency of observation, and sample size on power in studies of group differences in polynomial change. Psychological Methods. 2001;6(3):387–401. [PubMed] [Google Scholar]
- Resick PA. Stress and trauma. Clinical psychology, a modular course. New York, NY, US: Psychology Press; 2001. p. 205. [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Newbur Park, CA: Sage; 1993. [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive processing therapy, prolonged exposure, and a waiting condition for the treatment of posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006X.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resick PA, Galovski TE, Uhlmansiek M, Scher CD, Clum G, Young-Xu Y. A randomized clinical trial to dismantle components of Cognitive Processing Therapy for Posttraumatic Stress Disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology. 2008;76(2):243–258. doi: 10.1037/0022-006X.76.2.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rew L, Esparza D. Barriers to disclosure among sexually abused male children. Journal of Child and Adolescent Psychiatric and Mental Health Nursing. 1990;3:120–127. doi: 10.1111/j.1744-6171.1990.tb00458.x. [DOI] [PubMed] [Google Scholar]
- Sijbrandij M, Olff M, Reitsma JB, Carlier IVE, de Vries MH, Gersons BPR. Treatment of acute posttraumatic stress disorder with brief cognitive behavioral therapy: A randomized controlled trial. The American Journal of Psychiatry. 2007;164:82–90. doi: 10.1176/ajp.2007.164.1.82. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willet JB. Applied longitudinal data analysis: Modeling change and event occurrence. NY: Oxford University Press; 2003. [Google Scholar]
- Spielberger CD. State-Trait Anger Expression Inventory: Revised Research Edition. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Tarrier N, Sommerfield C, Pilgrim H, Faragher B. Factors associated with outcome of cognitive-behavioural treatment of chronic post-traumatic stress disorder. Behaviour Research and Therapy. 2000;38:191–202. doi: 10.1016/S0005-7967(99)00030-3. [DOI] [PubMed] [Google Scholar]
- Taylor S, Fedoroff IC, Koch WJ, Thordarson DS, Fecteau G, Nicki RM. Posttraumatic stress disorder arising after road traffic collisions: Patterns of response to cognitive-behavior therapy. Journal of Consulting and Clinical Psychology. 2001;69(3):541–551. doi: 10.1037//0022-006x.69.3.541. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132:959–992. doi: 10.1016/S0005-7967(99)00030-3. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]