Abstract
This cross-sectional study was done to identify and determine the socio-demographic and health-related factors associated with diabetic retinopathy and nephropathy screening in Korea. Participants included 2,660 adults, aged 40 or older, with diabetes. Of the 2,660 adults, 998 (37%) and 1,226 (46.1%) had received a diabetic retinopathy and a nephropathy screening within one year, respectively. Regarding retinopathy, subjects older than 65, living in urban areas, with high educational levels, and with self-reported "unhealthy" status were likely to receive annual screening. Subjects living in urban areas, with higher educational levels, with self-reported "fair" or "unhealthy" status, and with 1 to 2 co-morbidities were likely to receive annual nephropathy screening. The Korea Composite Stock Price Index (KOSPI) continued to rise until 2007 when it started to decline over the subsequent years, following the same curve as the diabetic retinopathy and nephropathy screening rates during that time. Together with the financial matter, lack of patient education proved to be a hindrance to diabetes-related screening. The relatively low screening rates in Korea compared to the Western countries are likely to be due to the difference in the health system, economic situations and national demographics.
Keywords: Diabetes Complications, Diabetic Nephropathy, Diabetic Retinopathy, Economic Crisis, Diabetes Care, KNHANES
INTRODUCTION
Diabetic retinopathy and nephropathy are two complications of diabetes that substantially affect patient quality of life. Diabetic retinopathy, a main complication of diabetes, often results in loss of vision and is also a leading cause of blindness in developed countries throughout the world (1). The Wisconsin Epidemiologic Study of Diabetic Retinopathy (WESDR) states that within five years after diagnosis, 14% of diabetes type I patients and 33% of diabetes type II patients develop diabetic retinopathy (2). Screening for diabetic retinopathy is intended to detect early sight-threatening lesions, diabetic retinopathy treatable with laser photocoagulation (3), and the clinical impact of screening for retinopathy has been well established (4, 5). Diabetic nephropathy is a frequent cause of chronic renal failure resulting from arteriolar disease or glomerulosclerosis. Diabetic retinopathy almost always precedes nephropathy, and therefore early detection of diabetic retinopathy can be crucial for treating both complications (6).
A health disparity is defined as a difference, between socioeconomic classes, in the chance of preventing certain health outcomes (7). Regarding diabetes, studies in the United States show that health disparities still exist to this day. Yet, similar sufficient data are not available in Asian countries, particularly data based on a nationally representative data.
In this study, we investigated how socio-demographic factors, health behavioral risk factors, and health status correlate with screening rates of diabetic retinopathy and nephropathy. We analyzed the trends of associated factors based on a national health survey in Korea, the Third and Fourth Korea National Health and Nutrition Examination Survey 2005 and 2007-2009 (KNHANES III and IV, respectively). Each is a nationally representative survey conducted by the Ministry of Health and Welfare that provides data on vision status, health care use, and other socio-demographic factors of more than 50,000 adults.
MATERIALS AND METHODS
Study design and population
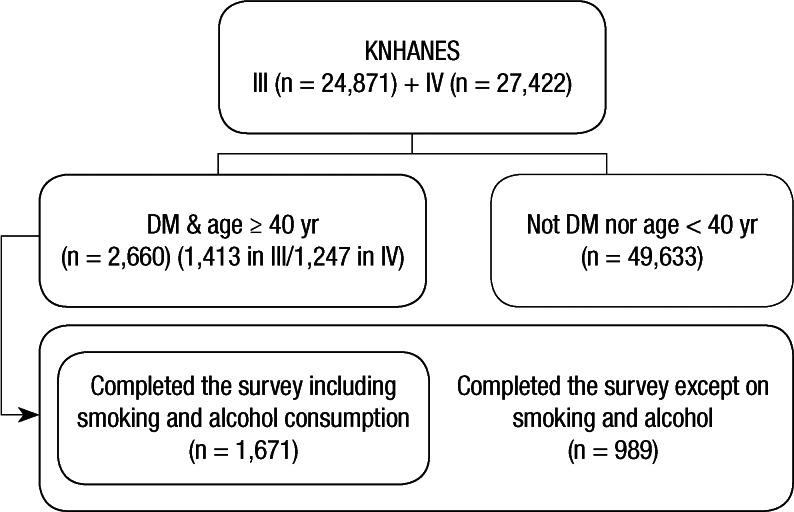
Our study evaluated data collected from KNHANES III and IV, a cross-sectional nationwide health survey in Korea, in order to identify various factors associated with diabetic retinopathy and nephropathy screening in Korea. A population-based random sampling covering 39,060 people across 600 national districts was selected. KNHANES IV used a population-based random sampling of 24,871 individuals in households across 500 national districts. KNHANES III was a compilation of data from 2005, but KNAHNES IV included data compiled from the years 2007 to 2009. Consequently, the third survey is named 2005 KNHANES, and the fourth, 2007-2009 KNHANES. KNHANES III and IV were each divided into three parts: the Health Interview Survey, the Health Examination Survey, and the Nutrition Survey. For the Health Interview Survey, a trained interviewer asked questions directly to individuals aged 12 yr or older. Of the 27,422 subjects aged 40 yr older in both national health surveys, 2,660 were diagnosed with diabetes (1,413 from KNHANES III and 1,247 from KNHANES IV). Our study includes 2,660 adults aged 40 or older who completed questionnaires about relevant independent factors and diabetic retinopathy and nephropathy screening. KNHANES III also included several health behavioral risk factors such as lifetime smoking and binge alcohol use in a separate health interview survey called Health Promotion Knowledge, Attitude, and Practice, but fewer people have completed this survey. Of the 2,660 subjects, 1,671 have completed the survey including health behavioral risk factors, and our study is based on these 1,671 subjects when analyzing the associations between screening and health behavioral risk factors (Fig. 1).
Fig. 1.
Flow diagrams showing selection of the study population.
Outcome variables
Subjects were asked two questions: 1) "Within the past year, have you ever received an eye examination (fundus photography) to screen for diabetic retinopathy?" with possible responses of "yes" or "no"; 2) "Within the past year, have you ever received a urine examination (microalbuminuria) to screen for diabetic nephropathy?" with possible responses of "yes" or "no".
Independent variables
From the KNHANES III and IV dataset, we collected data regarding various socio-demographic factors, which were obtained through direct interviews using structured questionnaires The socio-demographic variables included: current age (40-49/50-64/65 yr or older), sex (male/female), residential area (urban/rural), monthly household income (lowest quintile/2nd-4th quintile/highest quintile), and highest educational level achieved (elementary school or lower/middle school/high school/university or higher). The health status questionnaire included self-reported health status (healthy/fair/unhealthy) and the number of co-morbidities (0/1-2/≥ 3). The health behavioral risk variables included obesity (no/yes), lifetime smoking (no/yes), binge alcohol use (no/yes), physical activity of moderate intensity (never/more than once in a week), sleep duration (< 6/6-8/> 8 hr), and stress (minimally stressful/moderately stressful/extremely stressful).
"Residence" was classified as living in an urban area or not (e.g., living in a town or in the countryside). The per capita income was calculated using the following formula: household income/square root of the number of people in the household (8). To determine co-morbidities, subjects were asked the question: "Have you ever been diagnosed with diseases by a doctor before?" with possible responses of "yes" or "no". The trained interviewer emphasized "by a doctor" to minimize potential bias in the results. Co-morbidities included hypertension, dyslipidemia, osteoarthritis, rheumatoid arthritis, osteoporosis, atopic dermatitis, asthma, thyroid disease, and liver cirrhosis. Body mass index (BMI) was calculated using the following equation: body weight in kg/height in meters squared. We used the World Health Organization's BMI-defined obesity standard (≥ 25 kg/m2) for adults (9). All respondents were asked if they had smoked a total of 100 cigarettes in their life (10). Those who answered "yes" and who still smoke were classified as lifetime smokers, and those who reported that they have not smoked 100 cigarettes or those who do not currently smoke were classified as "non-smokers." Binge alcohol users were defined as those who consume more than 7 drinks on a single occasion for men, and 5 drinks on a single occasion for women, on one or more occasions in a month (11). We defined moderate-intensity physical activities as those lasting at least 30 min in duration and which increased heart rate slightly. Examples include volleyball, table tennis, swimming, yoga, and badminton, but not walking (12). Regarding stress, the following question was asked: "How much stress do you feel on a daily basis?" The potential responses were "minimal, moderate, or an extreme amount".
Statistical analysis
The basic characteristics of the study population are included by descriptive statistics: population number and percentage are mentioned for each variable. A two-step, multi-dimensional approach was used to identify the predictive factors for diabetic retinopathy screening. First, to identify the predictive factors associated with screening, the odds ratios and 95% confidence interval (CI) were calculated by univariate logistic regression analysis. Second, multivariate logistic regression analysis was used to determine independent predictive factors. All of the predictive factors that were identified as affecting diabetic retinopathy and nephropathy screening by univariate analysis were included in the multivariate analysis. For the multivariate analysis, we used the data of 1,671 subjects who completed the health survey including health behavioral factors. Furthermore, to evaluate temporal trends of predictive factors of diabetic retinopathy and nephropathy screening, multivariate logistic analysis was performed using all the socio-demographic factors in KNHANES III and IV, separately. Since this does not include health behavioral risk factors, we used the data of 2,660 subjects to evaluate the temporal trends. All statistical tests were twosided at 95% CI and were performed using the Stata/SE software version 12.1 (StataCorp, College Station, TX, USA).
Ethics statement
This study was approved by the institutional review board of Severance Hospital, Yonsei University College of Medicine in Seoul, Korea (IRB number: 4-2013-0172). Informed consent was waived by the board.
RESULTS
Baseline characteristics of the study population
The participant characteristics at baseline are described in Table 1. The mean age of the 2,660 participants aged more than 40 yr was 62.6 yr (standard deviation; 10.4). Of the 2,660 adults, 225 (8.5%) had received a diabetic retinopathy screening only, 453 (17.0%) had received a diabetic nephropathy screening only, and 773 (29.1%) had received screening for both within the previous year.
Table 1.
Characteristics of study population (n=2,660)
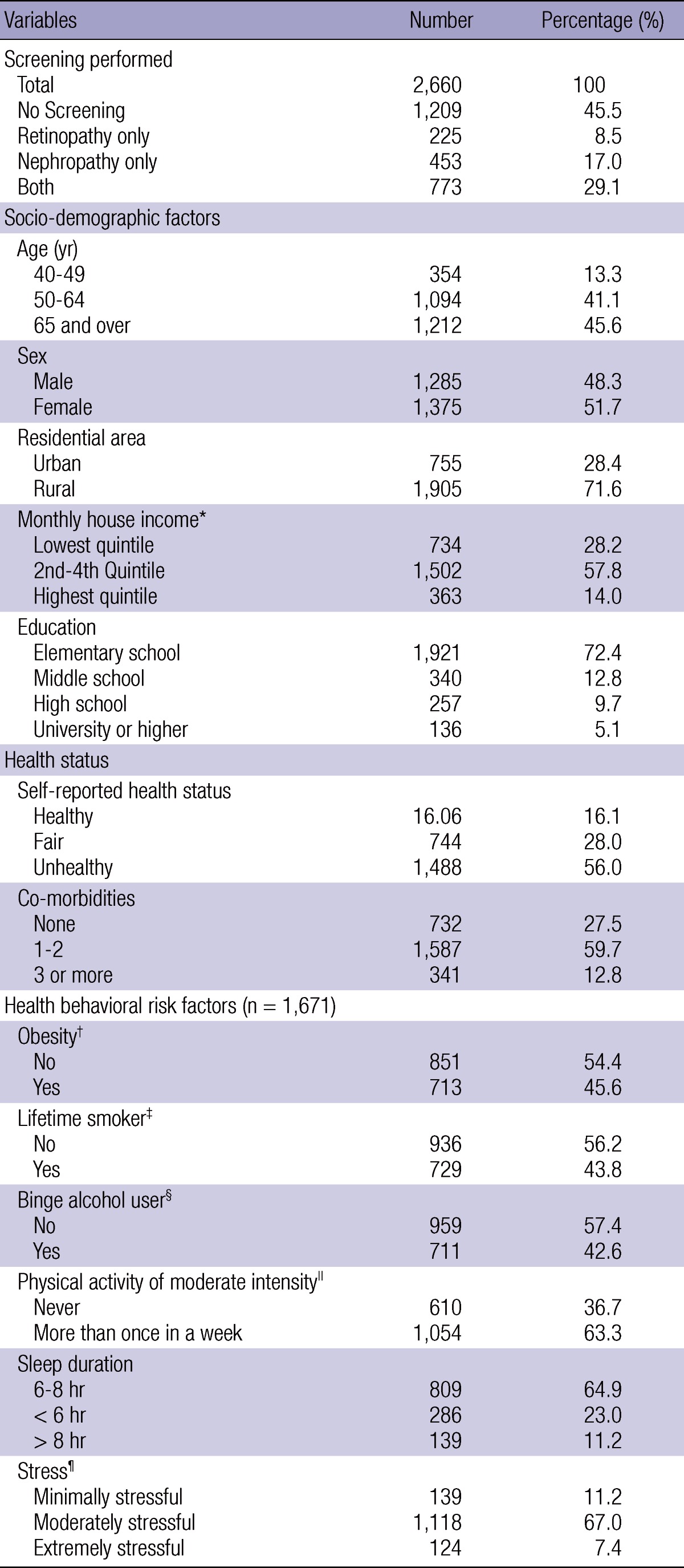
*To derive income per adult, we used the following formula: income/square root of the number of persons in the household; †We used the World Health Organization's BMI-defined obesity standard (≥ 25 kg/m2) for adults; ‡Lifetime smokers included subjects who reported that they have smoked at least 100 cigarettes in their lifetime and now smoke; §Binge alcohol users were defined as those who consume more than 7 drinks on a single occasion for men, and 5 drinks on a single occasion for women, on one or more occasions in a month; ∥Moderate-intensity activities were defined as lasting at least 30 min and increasing the heart rate slightly, as compared with sedentary activities; ¶Stress was assessed with the question: "How much stress do you feel on a daily basis?"
Screening rates and trends by year
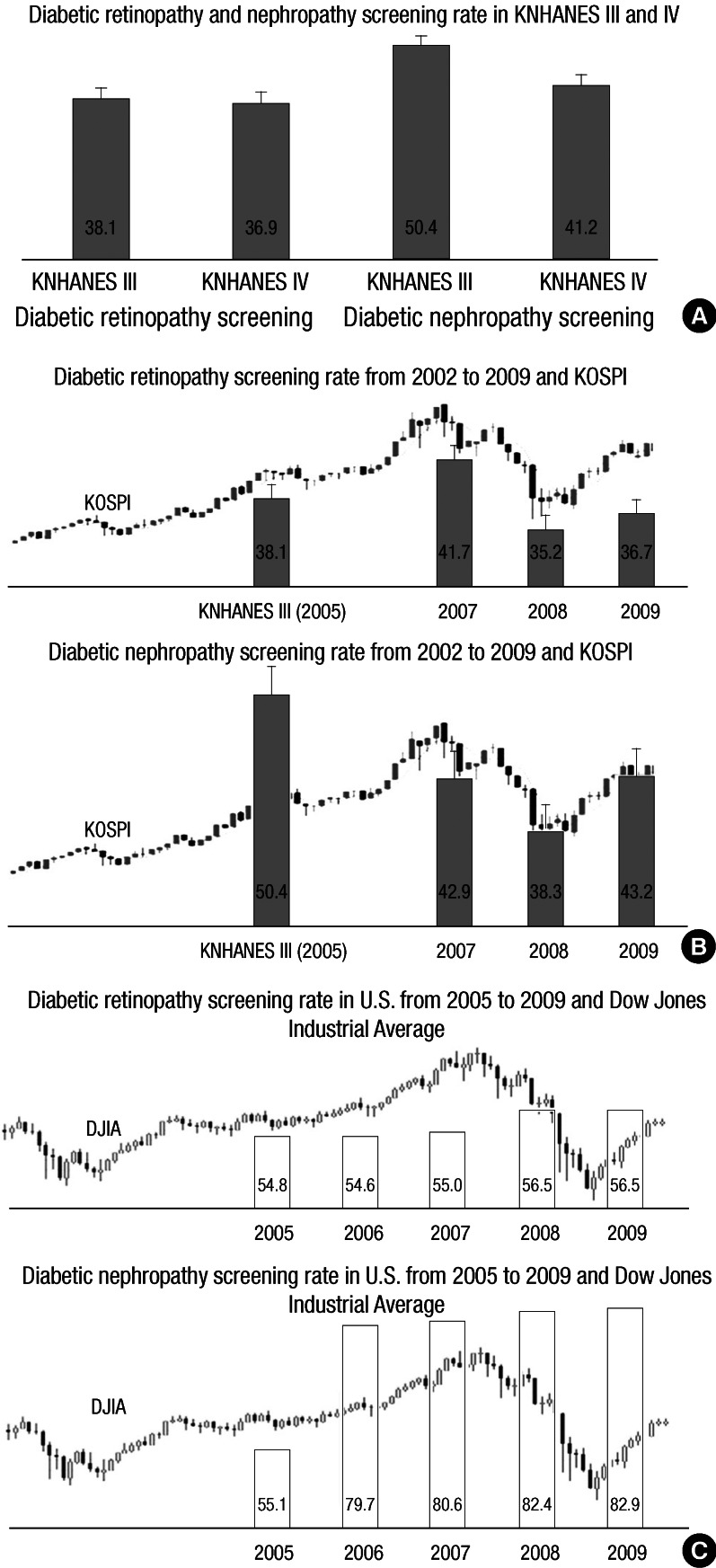
The screening rate for diabetic retinopathy was 38.1% in KNHANES III and 36.9% in KNHANES IV and the rate for diabetic nephropathy was 50.4% in KNHANES III and 41.2% in KNHANES IV (Fig. 2A). To evaluate the relationship between socio-economic status and screening rates, we compared the Korea Composite Stock Price Index (KOSPI) to the screening rates. The KOSPI slowly increased until 2007 and then decreased over the next few years (reflecting the global economic crisis), which is the exact same pattern seen in the diabetic retinopathy screening rates (Fig. 2B). In contrast, in the United States, the Dow Jones Industrial Average (DJIA) decreased after 2007 but both diabetic retinopathy and nephropathy screening rates gradually increased (Fig. 2C).
Fig. 2.
Screening rates of diabetic retinopathy and nephropathy. (A) Diabetic retinopathy screening rates are 38.1% (SE 5.5) in Korea National Health and Nutrition Examination Survey 2005 (KNHANES III) and 36.9% (SE 5.8) in KNHANES IV. Diabetic nephropathy screening rates are 50.4% (SE 5.3) in KNHANES III and 41.2% (SE 5.8) in KNHANES IV. (B) The averages of diabetic retinopathy screening rates were 38.1% (SE 5.5) in 2005, 41.7% (SE 14.2) in 2007, 35.2% (SE 9.4) in 2008, and 36.7% (SE 8.8) in 2009. In terms of diabetic nephropathy screening, the rates were 42.9% (SE 14.4) in 2007, 38.3% (SE 9.3), and 43.2% (SE 8.6) in 2009. The Korea Composite Stock Price Index (KOSPI) goes parallel with the diabetic retinopathy and nephropathy screening rates. (C) The averages of diabetic retinopathy screening rates in the United States were 54.8 in 2005, 54.6 in 2006, 55.0 in 2007, 56.5 in 2008, and 56.5 in 2009. The averages of diabetic nephropathy screening rates were 55.1 in 2005, 79.7 in 2006, 80.6 in 2007, 82.4 in 2008, and 82.9 in 2009. The Dow Jones Industrial Average (DJIA) decreased after 2007, but both diabetic retinopathy and nephropathy screening rates gradually increased.
Factors associated with diabetic retinopathy and nephropathy screening
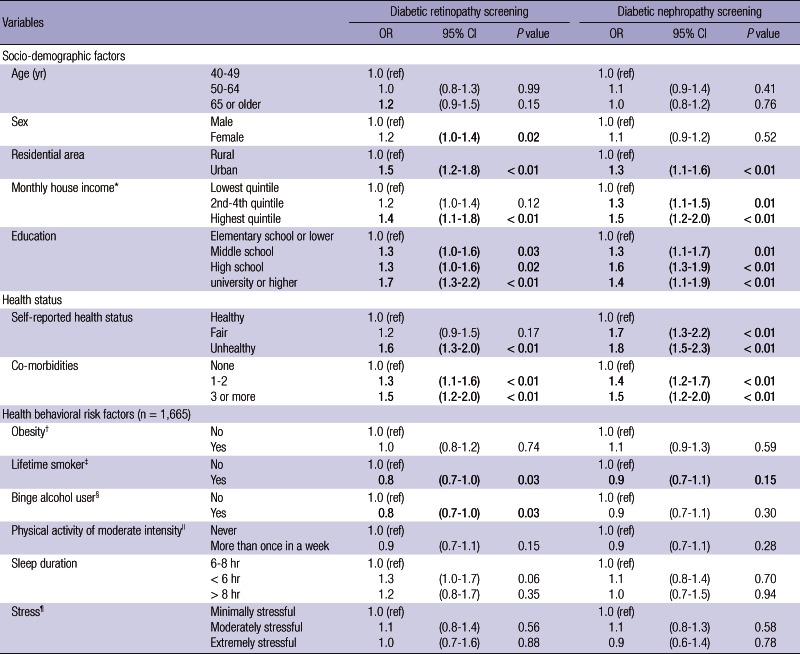
The statistically significant factors associated with diabetic retinopathy screening in the univariate analysis were all socio-demographic factors with the exception of age (Table 2). All other variables of health status, including lifetime smoking and binge alcohol use, were statistically significant. In terms of nephropathy screening, factors including residential area, monthly income, education, self-reported health status, co-morbidities, and lifetime smoker status were statistically significant in the univariate analysis.
Table 2.
Factors associated with screening for diabetes complications and trends-multivariate analysis
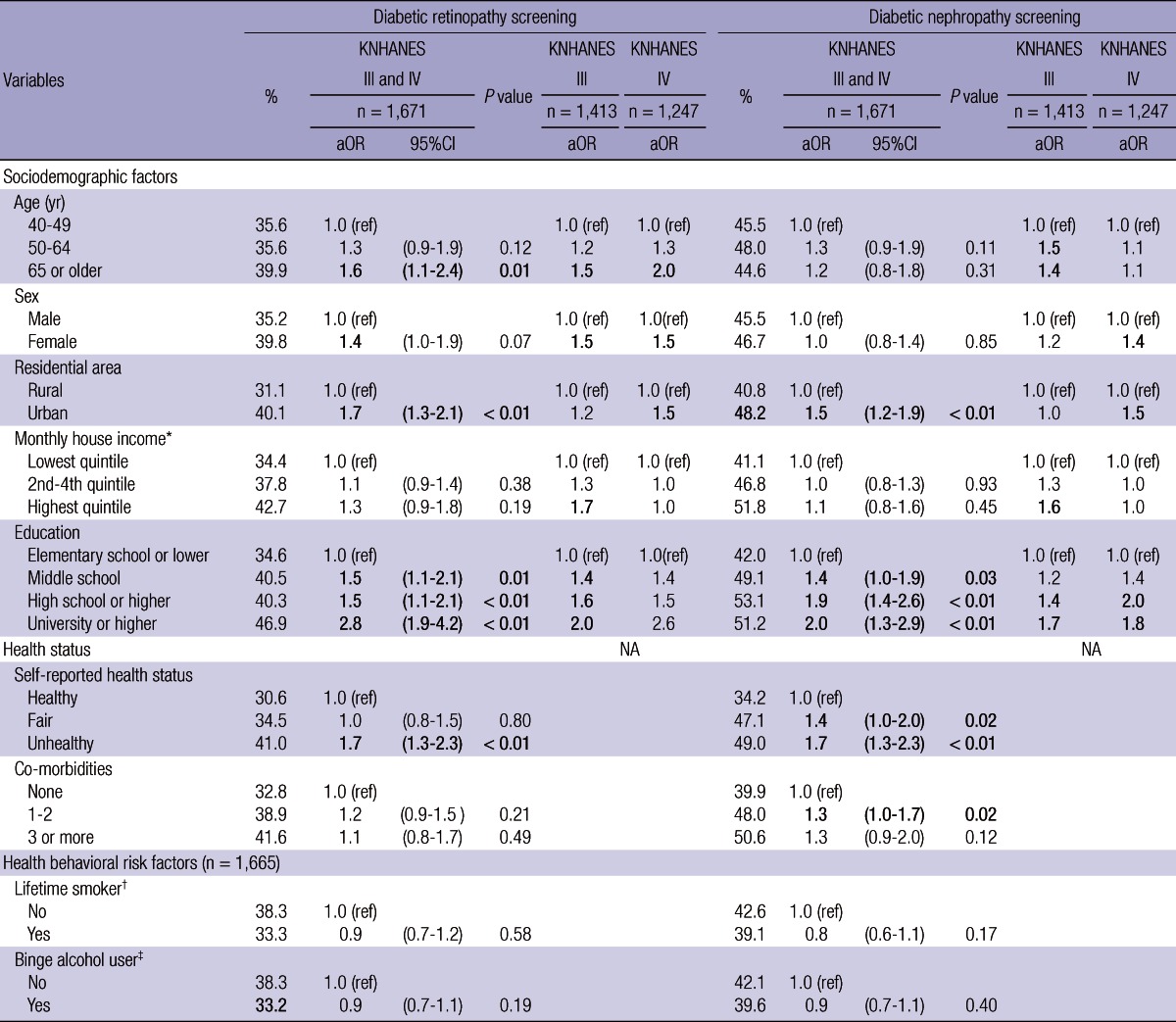
*To derive income per adult, we used the following formula: income/square root of the number of persons in the household; †Lifetime smokers included subjects who reported that they have smoked at least 100 cigarettes in their lifetime and now smoke; ‡Binge alcohol users were defined as those who consume more than 7 drinks on a single occasion for men, and 5 drinks on a single occasion for women, on one or more occasions in a month; Bold facerepresent P-values that are statistically significant.
When the statistically significant variables in the univariate analysis were combined in a multivariate analysis, four factors continued to be statistically significant in each screening (Table 2). Subjects who were 65 or older (adjusted Odds Ratio [aOR], 1.6; 95% CI, 1.1-2.4) were more likely to receive diabetic retinopathy screening than those who were 40 to 49. Also, subjects living in urban areas (aOR, 1.7; 95% CI, 1.3-2.2) were more likely to receive diabetic retinopathy screening than those living in rural areas. Subjects who graduated from middle school (aOR, 1.6; 95% CI, 1.1-2.2), high school (aOR, 1.5; 95% CI, 1.1-2.1), or from a higher education institute (aOR, 2.7; 95% CI, 1.8-4.2) were more likely to receive diabetic retinopathy screening compared to subjects who graduated from elementary school or lower. In terms of health status, subjects with a self-reported "unhealthy" health status (aOR, 1.7; 95% CI, 1.3-2.3) were more likely to receive diabetic retinopathy screening than those who did not self-report this status.
Subjects living in urban areas (aOR, 1.5; 95% CI, 1.2-1.9) were more likely to have received diabetic nephropathy screening than those living in rural areas. Subjects who graduated from middle school (aOR, 1.5; 95% CI, 1.1-2.0), high school (aOR, 1.9; 95% CI, 1.4-2.5), or a higher education institute (aOR, 1.8; 95% CI, 1.2-2.7) were more likely to receive diabetic nephropathy screening compared to subjects who graduated from elementary school or lower. In terms of health status, subjects with a self-reported "fair" health status (aOR, 1.4, 95% CI, 1.0-1.9) or "unhealthy" health status (aOR, 1.8; 95% CI, 1.2-2.7) were more likely to receive diabetic nephropathy screening than those who did not self-report this status. Subjects with one or two co-morbidities were more likely to receive diabetic nephropathy screening than those with no co-morbidities (aOR, 1.4; 95% CI, 1.1-1.8).
DISCUSSION
In this study, we analyzed various factors associated with the screening rates of diabetic retinopathy and nephropathy using nationally representative datasets. Many interesting results appeared, including various risk factors as well as a trend of diabetic retinopathy and nephropathy screening rates from 2005 to recent years. Our study presents two possibilities: the relatively low screening rates of Korea compared to Western countries may be due to the differences of economic development of those countries, or they may be due to the unique health care system of Korea and the people's specific situations such as income and education.
In the United States, The State of Health Care Quality published by The National Committee for Quality Assurance in 2009 states that diabetic retinopathy screening rates were 56.5% for a commercial group with a Health Maintenance Organization. In a study in London published in 1980, the screening rate was reported to be 59% (13). For diabetic nephropathy screening, the Committee reported screening rates of 82.9% for the commercial group, 88.6% for the Medicare group, and 76.9% for the Medicaid group in 2009. We could see that the diabetic retinopathy and nephropathy screening rates in Korea are still lower than those reported in other advanced countries.
Several barriers to screening have been suggested. First, a short supply of ophthalmologists and primary physicians could negatively affect screening rates, especially in low-income and rural regions (14). Second, even with easy access to eye care, patients are reluctant to undergo re-examination the following year after an examination ranging from 16% to 49% (15-17). To solve the shortage of ophthalmologists, teleophthalmology could be a cost-effective method of decreasing disparities between higher-educated, urban patients and under-educated, rural patients (18, 19). The lack of patient education, rather than financial shortage, led to low compliance with screening recommendations and lack of follow up re-examinations among patients (14). Therefore, while decreasing cost is important, it should be combined with multi-dimensional patient education using a booklet or video (20). Ultimately, the establishment of a diabetic registry would be the best way to offer comprehensive diabetic care, because it would enable identification of highrisk groups and patient-targeted programs.
Regarding age, diabetes patients aged 65 or older had a significantly higher rate of diabetic retinopathy screening. These figures could be explained by the fact that patients who are younger may have less time to visit a doctor and be screened. Regarding sex, females had a higher screening rate than males with a marginal statistical significance, which may be due to the fact that in Korea fewer women have occupations compared to men and therefore have more spare time in which to be screened. In terms of nephropathy screening, no definite difference was found in relation to age or sex. Regarding co-morbidities, however, patients with one or more co-morbidities were more likely to receive screening for microalbuminuria. This could be explained by the fact that internists often run tests for nephropathy along with tests for diabetes screening, but tests for retinopathy require additional consultations with ophthalmologists.
In our multivariate analysis, subjects with higher educational levels had significantly higher diabetic retinopathy and nephropathy screening rates than those with lower educational levels, in both time periods of KNHANES III and IV. Regarding monthly income, however, there was a significant disparity in the KNHANES III survey period, but such difference disappeared in the KNHANES IV survey period in both diabetic retinopathy and nephropathy screening. We presume that the decreased screening rates in years 2008 and 2009 are influenced mostly by education levels rather than monthly incomes. In Korea, the cost of fundus photography is about U$6 equivalent, which is significantly inexpensive compared to a cost of about U$30-60 in the United States. The cost of the test for microalbuminuria is similarly low in Korea, about U$13 equivalent, in comparison to a cost of about U$59-79 in the United States.
There are several earlier studies on the relationship between economic conditions and health care status, and interestingly, the theories behind these studies can be applied to our study of Korea's diabetic screening rates. The global financial crisis a few years ago has had a profound impact on the healthcare spending plans of national governments as well as individuals (21). The global economic trend over the last several years has been very similar to that of the KOSPI and this trend has a deep association with diabetic retinopathy and nephropathy screening rates. In Fig. 2B, KOSPI slowly increased until 2007 and then decreased over the next few years, which is exactly the same pattern seen in diabetic retinopathy and nephropathy screening rates. Fig. 2C shows the diabetic retinopathy and nephropathy screening rates of commercial groups in the United States from 2005 to 2009 and DJIA. The screening rate gradually increased while the DJIA decreased after 2008. In the United States there was no association between diabetic retinopathy and nephropathy screening rates and the DJIA. Whereas healthcare utilization has decreased in developing countries such as Korea and Indonesia, healthcare in some countries, such as Germany, appeared to improve during the economic crisis because of an increase in unemployment and the resulting additional time to receive medical care (22). Recently in the United States, an overall reduction in usage of non-emergency medical care after the economic crisis was reported, and the reductions were more noticeable among the unemployed, people with lower incomes, and younger people (23). This is consistent with previous reports in Korea that people with higher incomes were only slightly affected, while the poor were highly influenced by the economic crisis in 1998 (24).
Our study has several limitations. Since this is a cross-section study, a temporal cause and effect relationship cannot be established, as with all cross-section studies. Secondly, this study only involves Asians, so circumstances may be different in Western countries, leading to different results. But this limitation can also be a strength because not many studies involve Asian population. Regarding subjects, some bias may exist because there are more subjects living in rural areas than urban areas. Similarly, there are more subjects of low educational levels than higher levels in this study. Finally, this study does not include the relationship between subjects' specific glucose levels and the frequency of receiving examinations. It is possible that patients with higher glucose levels may receive more frequent tests, and further study should be done about this matter in the future.
Despite the limitations, our study is significant as an analysis of predictive factors associated with diabetic retinopathy and nephropathy screening rates on a nationally representative basis. As an economically developing nation, Korea has a low screening rate, and this has close ties to the economic conditions and socio-economic discrepancies among the population. Education especially, rather than monthly income, proved to be a critical factor that affects both diabetic retinopathy and nephropathy screening rates. This conclusion may be correct for other nations throughout the world and, consequently, give doctors a new focus on education when treating diabetes patients. We therefore conclude that doctors of ophthalmology, internal medicine, family medicine, and any other field that involves diabetes patients should keep this fact in mind and educate diabetes patients who have lower educational levels about the importance of retinopathy and nephropathy screening. These efforts should be supported on a national scale as well.
Appendix 1
The factors associated with screening for diabetes complications-univariate analysis (n = 2,660)
*To derive income per adult, we used the following formula: income/square root of the number of persons in the household; †We used the World Health Organization's BMI-defined obesity standard (≥25 kg/m2) for adults; ‡Lifetime smokers included subjects who reported that they have smoked at least 100 cigarettes in their lifetime and now smoke; §Binge alcohol users were defined as those who consume more than 7 drinks on a single occasion for men, and 5 drinks on a single occasion for women, on one or more occasions in a month; ∥Moderate-intensity activities were defined as lasting at least 10 min and increasing the heart rate slightly, as compared with sedentary activities; ¶Stress was assessed with the question, "How much stress do you feel on a daily basis?".
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Congdon NG, Friedman DS, Lietman T. Important causes of visual impairment in the world today. JAMA. 2003;290:2057–2060. doi: 10.1001/jama.290.15.2057. [DOI] [PubMed] [Google Scholar]
- 2.Varma R. From a population to patients: the Wisconsin epidemiologic study of diabetic retinopathy. Ophthalmology. 2008;115:1857–1858. doi: 10.1016/j.ophtha.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 3.Photocoagulation for diabetic macular edema: Early Treatment Diabetic Retinopathy Study report number 1: Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol. 1985;103:1796–1806. [PubMed] [Google Scholar]
- 4.Javitt JC, Aiello LP, Chiang Y, Ferris FL, 3rd, Canner JK, Greenfield S. Preventive eye care in people with diabetes is cost-saving to the federal government: implications for health-care reform. Diabetes Care. 1994;17:909–917. doi: 10.2337/diacare.17.8.909. [DOI] [PubMed] [Google Scholar]
- 5.Javitt JC, Canner JK, Frank RG, Steinwachs DM, Sommer A. Detecting and treating retinopathy in patients with type I diabetes mellitus: a health policy model. Ophthalmology. 1990;97:483–494. doi: 10.1016/s0161-6420(90)32573-3. [DOI] [PubMed] [Google Scholar]
- 6.Talley NJ, O'Connor S. Examination medicine: a guide to physician training. 6th ed. Sydney: Churchill Livingston, Elsevier; 2010. [Google Scholar]
- 7.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- 8.Deaton A, Lubotsky D. Mortality, inequality and race in American cities and states. Soc Sci Med. 2003;56:1139–1153. doi: 10.1016/s0277-9536(02)00115-6. [DOI] [PubMed] [Google Scholar]
- 9.Defining an international standard for overweight and obesity in childhood. BMJ. 2000;320:0. [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults: United States, 1992, and changes in the definition of current cigarette smoking. MMWR Morb Mortal Wkly Rep. 1994;43:342–346. [PubMed] [Google Scholar]
- 11.World Health Organization, Department of Mental Health Substance Dependence, Noncommunicable Diseases Mental Health Cluster. International guide for monitoring alcohol consumption and related harm. Geneva: World Health Organization; 2000. [Google Scholar]
- 12.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O'Brien WL, Bassett DR, Jr, Schmitz KH, Emplaincourt PO, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 13.Yudkin JS, Boucher BJ, Schopflin KE, Harris BT, Claff HR, Whyte NJ, Taylor B, Mellins DH, Wootliff AB, Safir JG, et al. The quality of diabetic care in a London health district. J Epidemiol Community Health. 1980;34:277–280. doi: 10.1136/jech.34.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartnett ME, Key IJ, Loyacano NM, Horswell RL, Desalvo KB. Perceived barriers to diabetic eye care: qualitative study of patients and physicians. Arch Ophthalmol. 2005;123:387–391. doi: 10.1001/archopht.123.3.387. [DOI] [PubMed] [Google Scholar]
- 15.Brechner RJ, Cowie CC, Howie LJ, Herman WH, Will JC, Harris MI. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993;270:1714–1718. [PubMed] [Google Scholar]
- 16.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–574. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 17.Mukamel DB, Bresnick GH, Wang Q, Dickey CF. Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthalmic Epidemiol. 1999;6:61–72. doi: 10.1076/opep.6.1.61.1563. [DOI] [PubMed] [Google Scholar]
- 18.Aoki N, Dunn K, Fukui T, Beck JR, Schull WJ, Li HK. Cost-effectiveness analysis of telemedicine to evaluate diabetic retinopathy in a prison population. Diabetes Care. 2004;27:1095–1101. doi: 10.2337/diacare.27.5.1095. [DOI] [PubMed] [Google Scholar]
- 19.Whited JD, Datta SK, Aiello LM, Aiello LP, Cavallerano JD, Conlin PR, Horton MB, Vigersky RA, Poropatich RK, Challa P, et al. A modeled economic analysis of a digital tele-ophthalmology system as used by three federal health care agencies for detecting proliferative diabetic retinopathy. Telemed J E Health. 2005;11:641–651. doi: 10.1089/tmj.2005.11.641. [DOI] [PubMed] [Google Scholar]
- 20.Legorreta AP, Hasan MM, Peters AL, Pelletier KR, Leung KM. An intervention for enhancing compliance with screening recommendations for diabetic retinopathy: a bicoastal experience. Diabetes Care. 1997;20:520–523. doi: 10.2337/diacare.20.4.520. [DOI] [PubMed] [Google Scholar]
- 21.Parry J, Humphreys G. Health amid a financial crisis: a complex diagnosis. Bull World Health Organ. 2009;87:4–5. doi: 10.2471/BLT.09.010109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neumayer E. Recessions lower (some) mortality rates: evidence from Germany. Soc Sci Med. 2004;58:1037–1047. doi: 10.1016/s0277-9536(03)00276-4. [DOI] [PubMed] [Google Scholar]
- 23.Lusard A, Schneider DJ, Tufano P. The economic crisis and medical care usage: NBER Working Paper. No. 15843. Cambridge: National Bureau of Economic Research; 2010. pp. 1–24. [Google Scholar]
- 24.Yang BM, Prescott N, Bae EY. The impact of economic crisis on healthcare consumption in Korea. Health Policy Plan. 2001;16:372–385. doi: 10.1093/heapol/16.4.372. [DOI] [PubMed] [Google Scholar]