Abstract
The goal of this study was to evaluate the association between gallbladder (GB) polyps and metabolic syndrome. A total of 5,685 healthy subjects were included, and 485 of these subjects had GB polyps and 744 had metabolic syndrome. In this study, metabolic syndrome was diagnosed according to standards suggested by the AHA/NHLBI ATP III 2005, and abdominal obesity (≥ 90 cm in men and ≥ 85 cm in women for Korean) was diagnosed according to standards set forth by the Korean Society for Study of Obesity. Biphasic logistic regression adjusted for age and gender was used to evaluate the association between metabolic syndrome and GB polyps. Subjects who were male (OR, 1.493; 95% CI, 1.11-2.00) and hepatitis B suface Ag (HBsAg) positive (OR, 1.591; 95% CI, 1.06-2.38) were significantly more likely to have GB polyps. The metabolic syndrome group had a higher risk of GB polyps (OR, 1.315; 95% CI, 1.01-1.69) than the group without metabolic syndrome. In conclusion, subjects who were HBsAg positive and male appear to be associated with the risk of GB polyps. The presence of metabolic syndrome also appears to be associated with the risk of GB polyps in Koreans.
Keywords: Metabolic Syndrome, GB Polyp, Risk Factors
INTRODUCTION
Metabolic syndrome is a disease with symptoms that include abdominal obesity, high triglyceride, low high density lipoprotein (HDL) cholesterol, high glucose, and hypertension. As the prevalence of obesity increases worldwide, the prevalence of metabolic syndrome has also increased (1). An analysis of data from a Korean nutrition survey showed a rapid increase in the prevalence of metabolic syndrome from 24.9% in 1998 to 31.3% in 2007 (2). Metabolic syndrome can increase the risk of cardiovascular disease and death, thus prevention and early treatment of metabolic syndrome is an important public health issue (3).
Gallbladder (GB) polyps are defined as any type of mass found in the gallbladder lumen, and they have become more common as ultrasonic examinations are more widely used in physical examinations. GB polyps are roughly classified into true polyps and pseudopolyps. True polyps include adenomas and adenocarcinomas, while pseudopolyps include cholesterol polyps, inflammatory polyps, and hyperplastic polyps (4). As with colorectal cancer, the adenoma-carcinoma sequence is associated with gallbladder cancer (5) and surgical removal is recommended for all true polyps because adenoma is considered a precancerous change. However, it is hard to obtain polyp tissue before surgery and to distinguish true polyps from pseudopolyps. Therefore, in order to increase survival rates it is necessary to find polyps as early as possible by using various clinical and image indices.
Recent studies have shown that obesity (6-10). and impaired glucose tolerance (7) are associated with GB polyps, which is believes so far to be the risk factor of gallbladder cancer (11,12). Thus, it seems likely that the prevalence of GB polyps is increasing. However, rare research has been conducted on the association between metabolic syndrome and GB polyps in Korea.
This study aimed to evaluate the association between elements of metabolic syndrome and GB polyps found by abdominal ultrasonography. The study also assessed the association between other possible risk factor that impact GB polyps in order to determine if there is an association between the metabolic indices and GB polyps, the risk factor of gallbladder cancer. Ultimately, this will help determine whether metabolic syndrome is related to GB polyps or not in Korean population, and we can make use of this result to our medical knowlege base.
MATERIALS AND METHODS
Research subjects
The primary subjects of this study were adult males and females over the age of 20 who received a physical examination in a health-screening center of a Seoul tertiary care hospital in 2008. Patients who received abdominal ultrasonography and whose medical records included age, height, BMI, waist circumference, and information about metabolic syndrome elements were included in the study. Patients who had a cholecystectomy or GB stones, or whose medical records did not include information about hepatitis B surface Ag (HBsAg) levels, body fat, or muscle mass were excluded. A total of 5,685 subjects were included in the study and 485 of them had GB polyps and 744 had metabolic syndrome.
Physical measurements and blood tests
Height and weight were measured by automatic measuring equipment, and body mass index (BMI) was determined by dividing weight (kg) by height squared (m2). Waist circumference was measured at the middle of the lowest part of rib and the highest part of iliac spine while the subject was in an erect posture and exhaling. Body fat and muscle mass of fasting subjects were measured with body composition analysis equipment (InBody 720, Biospace, Seoul, Korea) using the bioelectric impedance analysis method.
Brachial artery blood pressure was measured using an electronic hemodynamometer when the subject was seated and had been stable for at least ten minutes. If blood pressure measurements were not normal, blood pressure was measured again after resting for ten additional minutes. Average blood pressure was calculated as (systolic blood presseure + 2 × diastolic blood pressure)/3. Venous blood was collected after the subject had fasted for at least eight hours, and an auto analyzer measured fasting glucose, triglyceride, HDL cholesterol, gamma-GTP (γ-GTP), total bilirubin, and HBsAg.
Diagnosis of metabolic syndrome
In this study, metabolic syndrome was defined according to standards suggested by the American Heart Association (AHA)/National Heart, Lung and Blood Institute (NHLBI) ATP III 2005, which is using the standard suggested by International Diabetes Federation (IDF) (13) in 2005 and the standards by National Cholesterol Education Program, Adult Treatment Panel III (NCEP ATP III) in 2005 (14). And abdominal obesity was defined according to standards set forth (≥ 90 cm in men and ≥ 85 cm in women for Korean) by the Korean Society for Study of Obesity (15).
According to the guidelines suggested by AHA/NHLBI ATP III 2005, metabolic syndrome was diagnosed when three of following conditions were met:
Waist circumference ≥ 90 cm (male) or ≥ 85 cm (female) (15)
Trigyceride ≥ 150 mg/dL or medicated to treat this condition
HDL-C < 40 mg/dL (male), < 50 mg/dL (female) or medicated to treat this condition
Systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg or medicated to treat hypertension
Fasting glucose ≥ 100 mg/dL or medicated to treat diabetes
Diagnosis of GB polyps
One radiology specialist determined that a GB polyp is present by radiologic definition if ultrasonography reveals any size hyperechoic mass projecting from the gallbladder wall, without acoustic shadowing and without any movement following a change in posture (16-19). There is a study showing that metabolic syndrome was related to the increase of GB stone (20). Thus subjects with coexisting pancreatobiliary tract disease and GB stones were excluded, as were subjects who did not have a gallbladder due to a cholecystectomy.
Statistical analysis
All statistical analysis was performed using SPSS for Windows, version 18.0 (SPSS Inc., Chicago, IL, USA). The GB polyp group and the non-GB polyp group were compared using an independent t-test for continuous variable comparison and a chisquare test for non-continuous variable comparison. In multivariate analysis, the association between elements of metabolic syndrome, various risk factors and GB polyps were evaluated using biphasic logistic regression with a 95% confidence interval where P < 0.05 was considered statistically significant.
Ethics statement
The study protocol was approved by the institutional review board of Ewha Womens University Mokdong Hospital (IRB No. ECT 11-35-27). Informed consent was confirmed by the board.
RESULTS
General characteristics of research subjects
There were a total of 5,685 research subjects, with 485 in the GB polyp group and 5,200 in the non-GB polyp group. The effect of each component of metabolic syndrome and possible risk factor on GB polyps were evaluated by comparing the characteristics of the GB polyp group and the non-GB polyp group (Table 1). Average age of the 485 polyp patients was 44.9 ± 9.8 yr and average age of control group was 43.9 ± 10.4 yr. The frequency of GB polyps was higher in males (5.5%) than in females (3.1%). When the GB polyp group and the non-GB polyp group were compared, age (P = 0.036), BMI (P < 0.001), muscle mass (P < 0.001), waist circumference (P < 0.001), systolic blood pressure (P = 0.023), diastolic blood pressure (P = 0.021), fasting glucose (P = 0.039), and HDL cholesterol (P = 0.001) of the GB polyp group were significantly higher than the control group in an univariate analysis of continuous variables. In a univariate analysis of non-continuous variables, both male and female members of the GB polyp group were significantly more likely to be HBsAg positive (P = 0.017).
Table 1.
Univariate comparison between gallbladder polyp group and control group*
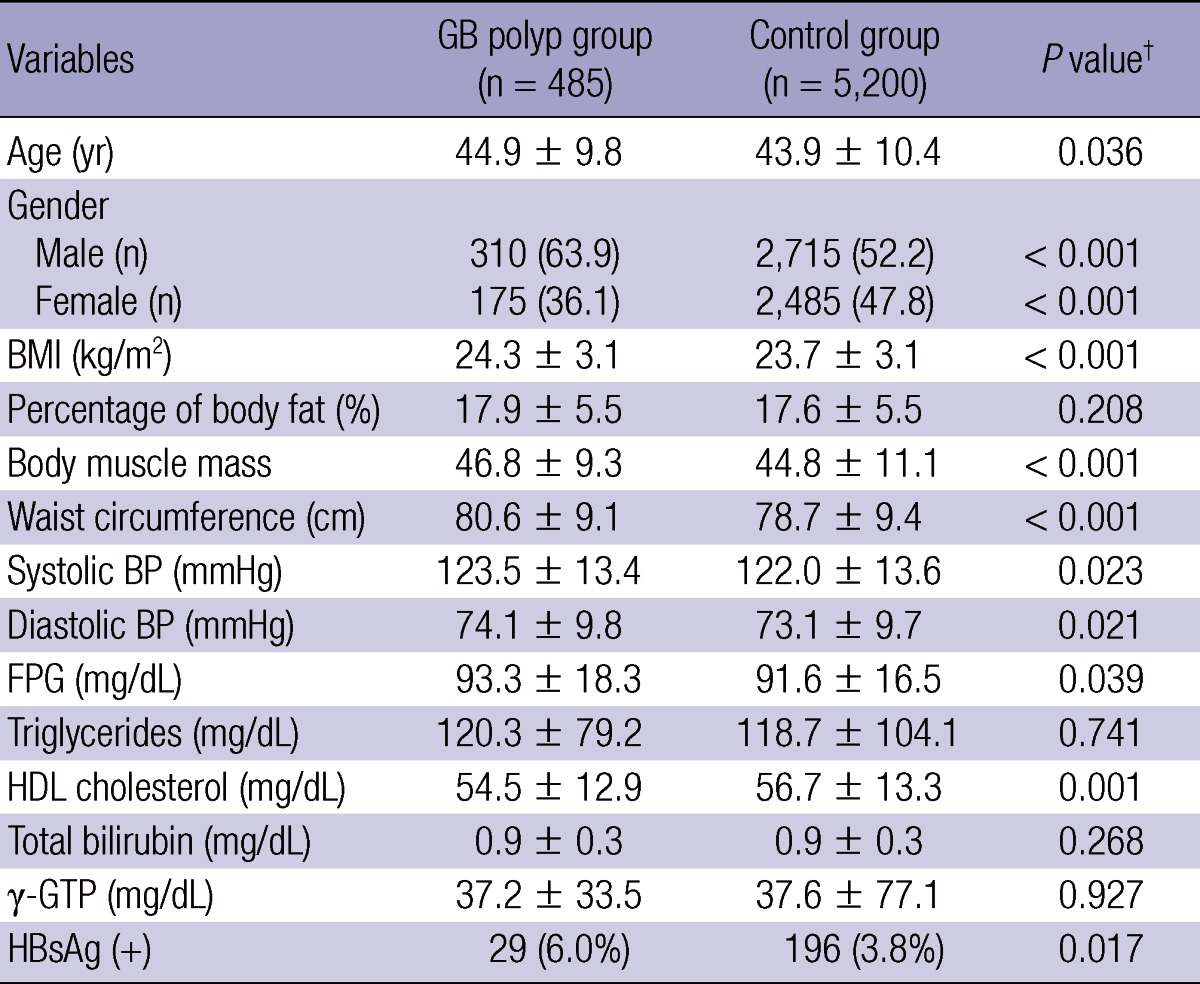
*Values (Gender and HBsAg) are presented as number (%). Other values are presented as mean ± standard error. †P values were calculated by t-test and chi-square test. BMI, body mass index; BP, blood pressure; FPG, fasting plasma glucose; HDL, high density lipoprotein.
Multivariate analysis of factors related to GB polyps
Age-adjusted multivariate analysis was performed using significant factors from univariate analysis. Results showed that male subjects had a higher odds ratio (1.493, 95% CI, 1.11-2.00) than female subjects and the HBsAg positive group had a higher odds ratio (1.591, 95% CI, 1.06-2.38) than the HBsAg negative group (Table 2). An age-adjusted multivariate analysis of these factors showed that only male gender and HBsAg status were significant independent factors to the occurrence of GB polyps.
Table 2.
Risk of GB polyps according to metabolic syndrome components and GB polyp risk factors
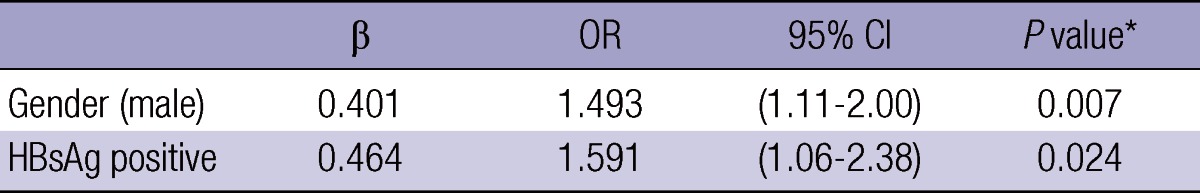
†P value calculated by multiple logistic regression analysis after adjusting for age. GB, gallbladder; OR, odds ratio; CI, confidence interval.
Relation between presence of metabolic syndrome and GB polyp
A multivariate analysis was performed after adjusting for age, gender and HBsAg positivity to determine how metabolic syndrome affects gallbladder polyps. When metabolic syndrome was present, the odds ratio of GB polyps was 1.315 (95% CI, 1.01-1.69), which is significantly higher than when metabolic syndrome was not present.
DISCUSSION
The prevalence rate of GB polyps is different between countries (21), and even within countries, urban areas and agricultural areas (22). According to reports from countries other than Korea, the prevalence rate of GB polyps is approximately 5% (16). The prevalence rate in Korea is 3% (6) with a report of 2.2% (9) in one single institution study.
Though the survival rate of GB cancer has improved with the development of radiological examination equipment and advanced therapy, it still easily metastasizes at early stages with almost no symptoms and thus is typically diagnosed in advanced stages when surgery is no longer an option. Therefore, the prognosis for GB cancer is generally very poor. The primary risk factor for gallbladder cancer is GB polyps. It is difficult to distinguish between malignant and benign GB polyps, despite efforts by numerous studies to differentiate them and to find the risk factor of GB polyps.
So far, most research, including the present study, has shown that GB polyp frequency is higher in males than in females (7, 11, 16). And this study shows the same result. Therefore, being male is considered to be a risk factor for GB polyps.
Cholesterol polyps are the most common type of GB polyp. Some hypothesize that GB polyps are formed when cholesterol is directly deposited on the gallbladder, similar to the plaque formation in arteriosclerosis (23). There are reports that free sterol can transform from gall to gallbladder mucous membrane, and cholesterol polyps are related to intrahepatic cholesterol synthesis changes (24). But a comparison of GB polyps and various blood lipids did not produce any significant results, and lipid was not a risk factor of polyps in this study.
Some studies have reported that obesity has an effect on GB polyps (6, 11). Meanwhile, others did not find a relationship between obesity and GB polyps (7, 16). The present study observed an insignificant relationship between obesity and GB polyps.
Impaired glucose tolerance is known to be a risk factor (7) of GB polyps, leading to the hypothesis that high glucose hinders the contraction of gallbladder and suppresses the secretion of gall. However, there was no relationship between GB polyps and diabetes in this study.
This study also found that the odds ratio of GB polyps was higher in the HBsAg positive group, which is similar to results from other studies in Korea (6, 12). It remains unclear whether the infection of hepatitis B itself is a risk factor of GB polyps, or if GB polyps are formed as a result of chronic hepatitis B or liver cirrhosis.
Waist circumference, blood pressure, fasting glucose, HDL cholesterol, age, gender, BMI, and HBsAg status were all significant GB polyp risk factors in univariate analysis. However, gender and a positive HBsAg status were the only risk factor of GB polyps that were found to be significant in multivariate analysis. The metabolic syndrome group had a higher odds ratio of GB polyps (1.315, 95% CI, 1.01-1.69) than the group without metabolic syndrome, after adjusting for age and gender.
This study has several limitations. First, the subject group consisted of patients who visited one university hospital health screening center and therefore does not represent the entire community. Also, subjects without waist circumference, body fat, and muscle mass measurements were excluded, which could falsely indicate that these indices are not risk factors of GP polyps. This is supported by the fact that BMI was an insignificant risk factor (P = 0.155), while the odds ratio was 1.041. Future studies should compare randomly selected members of the general public with and without GB polyps. Another limitation of this study is that small polyps under 5 mm may be hard to distinguish from GB stones. Most polyps are less than 5 mm; thus, in this study the presence of GB polyps was based on movement following change in posture, and posterior acoustic results. Finally, cholesterol polyps, adenomatous polyps, and inflammatory polyps were all regarded as GB polyps during this study. The fact that all polyps were included in the polyp group, regardless of size and type, may have affected the results. However, it is very difficult to make a clear histological diagnosis of GB polyps except through histopathological confirmation after surgery, and therefore all polyps had to be classified in the same group. Future studies should attempt to classify polyps by size and number according to histological findings.
Despite the limitations described above, this study has several strengths. There has not been much of a study, attempt to determine the association between GB polyps and metabolic syndrome. And most previous studies have focused on the risk factors of GB polyps. However, this study clarified that the metabolic syndrome group had a higher odds ratio of GB polyps than the control group.
Since there was a study showing that metabolic syndrome was related to the increase of GB stone (20), the significance of this study is that association between GB polyp and metabolic syndrome was compared by classifying a group with only GB polyp and control group. In addition, this study focused on physical characteristics unique to Koreans by using standards from the Korean Society for the Study of Obesity (15) when diagnosing abdominal obesity ( ≥ 90 cm in men and ≥ 85 cm in women for Korean). Finally, this study used the most current standards and considered fasting blood glucose ≥ 100 to be a component of metabolic syndrome.
In conclusion, we confirmed that being male and having an HBsAg-positive status are significant risk factors of GB polyps, and that metabolic syndrome is independently related to increased odds ratio of GB polyps in Koreans. In the future, a prospective longitudinal study would be necessary to explain the association of metabolic syndrome and GB polyps.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill; 2008. pp. 1509–1514. [Google Scholar]
- 2.Lim S, Shin H, Song JH, Kwak SH, Kang SM, Won YJ, Choi SH, Cho SI, Park KS, Lee HK, et al. Increasing prevalence of metabolic syndrome in Korea: the Korean National Health and Nutrition Examination Survey for 1998-2007. Diabetes Care. 2011;34:1323–1328. doi: 10.2337/dc10-2109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SM, Kim KM, Lee DJ. Relationship of uric acid concentration to free fat acid, cardiovascular risk factors and intraperitoneal fat. J Korean Soc Study Obes. 1997;6:51–58. [Google Scholar]
- 4.Christensen AH, Ishak KG. Benign tumors and pseudotumors of the gallbladder: report of 180 cases. Arch Pathol. 1970;90:423–432. [PubMed] [Google Scholar]
- 5.Kozuka S, Tsubone N, Yasui A, Hachisuka K. Relation of adenoma to carcinoma in the gallbladder. Cancer. 1982;50:2226–2234. doi: 10.1002/1097-0142(19821115)50:10<2226::aid-cncr2820501043>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 6.Shim SG, Lee KT, Lee JK, Park JH, Ryu KH, Rhee PL, Kim JJ, Koh KC, Paik SW, Rhee JC, et al. Prevalence and risk factors of gallbladder polyps in health screening subjects. Korean J Med. 1999;57:1014–1020. [Google Scholar]
- 7.Chen CY, Lu CL, Chang FY, Lee SD. Risk factors for gallbladder polyps in the Chinese population. Am J Gastroenterol. 1997;92:2066–2068. [PubMed] [Google Scholar]
- 8.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 9.Kuriyama S, Tsubono Y, Hozawa A, Shimazu T, Suzuki Y, Koizumi Y, Suzuki Y, Ohmori K, Nishino Y, Tsuji I. Obesity and risk of cancer in Japan. Int J Cancer. 2005;113:148–157. doi: 10.1002/ijc.20529. [DOI] [PubMed] [Google Scholar]
- 10.Larsson SC, Wolk A. Obesity and the risk of gallbladder cancer: a metaanalysis. Br J Cancer. 2007;96:1457–1461. doi: 10.1038/sj.bjc.6603703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Segawa K, Arisawa T, Niwa Y, Suzuki T, Tsukamoto Y, Goto H, Hamajima E, Shimodaira M, Ohmiya N. Prevalence of gallbladder polyps among apparently healthy Japanese: ultrasonographic study. Am J Gastroenterol. 1992;87:630–633. [PubMed] [Google Scholar]
- 12.Kim SY, Lee HS, Lee YS, Chung KW, Jang BK, Chung WJ, Park KS, Cho KB, Hwang JS. Prevalence and risk factors of gallbladder polyp in adults living in Daegu and Gyeongbuk Provinces. Korean J Gastroenterol. 2006;48:344–350. [PubMed] [Google Scholar]
- 13.Alberti KG, Zimmet P, Shaw J IDF Epidemiology Task Force Consensus Group. The metabolic syndrome: a new worldwide definition. Lancet. 2005;366:1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- 14.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 15.Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, Kim DY, Kwon HS, Kim SR, Lee CB, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007;75:72–80. doi: 10.1016/j.diabres.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 16.Jørgensen T, Jensen KH. Polyps in the gallbladder: a prevalence study. Scand J Gastroenterol. 1990;25:281–286. [PubMed] [Google Scholar]
- 17.Shinchi K, Kono S, Honjo S, Imanishi K, Hirohata T. Epidemiology of gallbladder polyps: an ultrasonographic study of male self-defense officials in Japan. Scand J Gastroenterol. 1994;29:7–10. doi: 10.3109/00365529409090429. [DOI] [PubMed] [Google Scholar]
- 18.Collett JA, Allan RB, Chisholm RJ, Wilson IR, Burt MJ, Chapman BA. Gallbladder polyps: prospective study. J Ultrasound Med. 1998;17:207–211. doi: 10.7863/jum.1998.17.4.207. [DOI] [PubMed] [Google Scholar]
- 19.Ozdemir A, Ozenc A, Bozoklu S, Cosķun T. Ultrasonography in the diagnosis of gallbladder polyps. Br J Surg. 1993;80:345. doi: 10.1002/bjs.1800800326. [DOI] [PubMed] [Google Scholar]
- 20.Kim J, Lee K. Relationship between metabolic syndrome and gallbladder stone. Korean J Fam Med. 2009;30:610–616. [Google Scholar]
- 21.Lin WR, Lin DY, Tai DI, Hsieh SY, Lin CY, Sheen IS, Chiu CT. Prevalence of and risk factors for gallbladder polyps detected by ultrasonography among healthy Chinese: analysis of 34 669 cases. J Gastroenterol Hepatol. 2008;23:965–969. doi: 10.1111/j.1440-1746.2007.05071.x. [DOI] [PubMed] [Google Scholar]
- 22.Hayashi Y, Liu JH, Moriguchi H, Takenawa H, Tazawa J, Nakayama E, Marumo F, Sato C. Prevalence of polypoid lesions of the gallbladder in urban and rural areas of Japan: comparison between 1988 and 1993. J Clin Gastroenterol. 1996;23:158–159. doi: 10.1097/00004836-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Salmenkivi K. Cholesterolosis of the gall-bladder: a clinical study based on 269 cholecystectomies. Acta Chir Scand. 1964;105:1S–93S. [PubMed] [Google Scholar]
- 24.Tilvis RS, Aro J, Strandberg TE, Lempinen M, Miettinen TA. Lipid composition of bile and gallbladder mucosa in patients with acalculous cholesterolosis. Gastroenterology. 1982;82:607–615. [PubMed] [Google Scholar]


