Abstract
This study was performed to estimate the direct medical costs and epidemiology of pneumonia in adults of Korea. We conducted a multi-center, retrospective, observational study and collected data targeting for community-acquired pneumonia patients ( ≥ 50 yr) from 11 hospitals. Costs attributable to the treatment of pneumonia were estimated by reviewing resource utilization and epidemiology data (distribution of pathogen, hospital length of stay, overall outcome) were also collected. A total 693 patients were included; average 70.1 ( ± 10.5) aged, 57.3% male and average 1.16 CURB-65 (confusion, blood urea nitrogen, respiratory rate, blood pressure, age > 65 yr) scored. The pathogen was identified in the 32.9% (228 patients); Streptococcus pneumoniae accounted for 22.4% (51 patients) of identified pathogens. The hospital mortality was 3.2% (especially, for S. pneumoniae was 5.9%) and average length of stay was 9 days. The mean total cost for the treatment of pneumonia was US dollar (USD) 1,782 (SD: USD 1,501). Compared to the cost of all caused pneumonia, that of pneumococcal pneumonia was higher, USD 2,049 ( ± USD 1,919), but not statistically significant. Charge of hospitalization accounted the greatest part of total medical costs. The economic burden of pneumonia was high in Korea, and the prevention of pneumonia should be considered as effective strategy.
Keywords: Pneumonia, Streptococcus pneumonia, Cost of Illness, Adult, Korea
INTRODUCTION
Community acquired pneumonia (CAP) shows high mortality rate despite antibiotics treatment. In the US, it is the leading cause of death among infectious diseases, with approximately 5.6 million new cases every year and mortality of 2%-3% (1). In Korea, it ranked 9th among all causes of death in 1999 but jumped to 6th in 2010 which shows the highest mortality among causes of death due to infection included in top 10 causes of death in Korea (2). Mortality due to pneumonia rapidly increases after 45 yr of age and is expected to further increase in the elderly given the accelerating trend of aging population in Korea. Since incidence of pneumonia is higher in the elderly (3) and patients with chronic diseases (4), it is warranted to investigate these high risk groups and pursue intensive management based on such investigation.
Streptococcus pneumoniae (pneumococcus) is known as the most common pathogen causing pneumonia. From a metaanalysis of 127 studies on pathogens of pneumonia, pneumococcal pneumonia accounted for 24% of all cases (5). In a study for 588 pneumonia patients hospitalized in domestic university hospitals, pathogens were identified in 38.3% of cases in which pneumococcal pneumonia represented 21.7% or 57 cases (6). However, identification of a pneumonia pathogen may differ depending on the capacity of the relevant in-hospital laboratory, study design, season or region of the study conduct. In patients who cannot be diagnosed with conventional culture method, S. pneumoniae is identified as the pathogen in approximately 50% of such cases by use of phenotype-specific antibody test. Therefore, the chance of S. pneumoniae being the pathogen is expected to be higher (7). In approximately 40%-60% of pneumonia patients up to date, pathogen has not been identified (8).
Economic burden due to pneumonia depends on patient's age; ≤ 4 or ≥ 70 yr old groups exhibit the highest pneumonia incidence and high admission rate, resulting in the highest economic burden. In Korea, pneumonia patients aged ≥ 65 yr old spend medical costs of Korean Won (KRW) 479.6 billion ever year for pneumonia treatment. This is 6.7 times higher than that in 15-44 yr old pneumonia patient group and 74% of this expense is used for charge of hospitalization (9).
Of pneumococcal diseases, pneumonia accounts for 90% or above, and roughly 5% of cases result in death. In the US, approximately 500,000 new cases of pneumococcal pneumonia are reported every year including approximately 30,000 patients with invasive pneumococcal diseases (sepsis, encephalomeningitis) and overall 20,000 cases of death (10). Given the relatively large number of patients with pneumococcal pneumonia, effective prevention of pneumococcal pneumonia may reduce pneumococcus-induced mortality.
To assess the effectiveness of prevention efforts to reduce pneumonia occurrence, epidemiological data such as incidence, cause of death, and economic burden of pneumonia patients are required primarily. In particular, to investigate the impact on the burden-of-illness, accurate knowledge on economic and clinical indices prior to preventive action would be necessary in confirming the effectiveness after prevention. Nevertheless, there are no sufficient basic data on the level of economic burden resulting from pneumonia in Korea. Although burden of medical costs can be derived from data offered by Health Insurance Review & Assessment Service (HIRA), these data has limitations in that disease codes are not reliable enough, and only insurance claimed charges can be confirmed but not the expenses of uninsured items.
This study investigated the economic burden and baseline epidemiology in Korean pneumonia patients aged ≥ 50 yr. The primary objective was to estimate the economic burden through investigation of direct medical costs incurred from pneumoniarelated utilization of medical institutions, and to obtain epidemiologic data such as patient disposition and death profile in pneumonia patients. The secondary objective was to establish direct medical costs and epidemiology in pneumococcal pneumonia patients only.
MATERIALS AND METHODS
Study design and patient samples
This was a retrospective observational study of 764 patients aged ≥ 50 yr who received inpatient care due to pneumonia in 11 Pulmonary Divisions in domestic medical institutions of general hospital or referral hospital (all university hospitals). Patients were enrolled in the reverse temporal order from the end of treatment on 2010.12.31 (the entire treatment period for all patients covered 2008.01.01-2010.12.31). Of these, 56 patients with present status of malignant cancer and 15 patients with only fungal pathogen detection were excluded from analysis; the former was due to the predicted high burden-of-illness and the latter was due to the clinical judgment that it would be difficult to define the fungus as the pathogen for pneumonia.
The study targeted only patients with community acquired pneumonia that required inpatient care due to these pneumonia. Healthcare-associated pneumonia and H1N1 infected pneumonia patients were excluded; patients who participated in other clinical study or determined by the investigator as ineligible for this study were also excluded.
Data collection
General characteristics, clinical characteristics, treatment outcome, type of antibiotics used for treatment were surveyed in pneumonia patients. General characteristics included sex and age; clinical characteristics included underlying disease, pathogen and identification method, severity (confusion, blood urea nitrogen, respiratory rate, blood pressure, age > 65 [CURB-65]), and treatment period; treatment outcomes included treatment response and survival status.
Resource utilization
The scope of medical resources covered 6 areas of hospitalization, medication, diagnostic test, laboratory test, imaging test, and procedures or surgery. For hospitalization, admission frequency and period by outpatient and inpatient type (emergency room, general ward, intensive care unit [ICU]), referral frequency and optional hospitalization status were surveyed. In patients who were admitted for 2 days or more, the transfer and discharge day were excluded when counting the length of hospital stay, and only the medical resource utilization was applied. For medication, the generic name, dosing route, dose and dosing period were surveyed for antibiotics and other pneumonia-related drugs. In diagnostic test, bacteria identification tests and necessary procedures (bronchoscopy, thoracentesis, histology, etc.) using samples such as sputum, blood, urine, and pleural fluid were surveyed. For laboratory test, names and frequency of tests such as hematology or urinalysis other than diagnostic tests were investigated and for imaging tests, names and frequency of tests such as simple chest radiography, chest CT, MRI, ultrasound, and echocardiography were surveyed. In procedures or surgery, the status of treatment of pneumonia and pneumonia-induced complications and relevant surgery and procedure status were investigated.
This study was a cost study that calculated direct medical costs based on the medical resource utilization survey results, and direct medical costs were calculated by including not only insured charges but also uninsured, actual expenses. The standard unit price of converting the surveyed medical resource utilization to the direct medical costs was differently applied by the insured/uninsured status of the relevant medical resource item.
For medical resource items that corresponded to insured charges, the 2010 health insurance fees by each insured medical resource item were consistently applied. In addition, in case of items applicable to additionally adjusted insured charges such as addition by type and nursing (or intensive patient care) personnel category, etc., the actual status was investigated and applied for each relevant institution. In case medical resource items corresponded to uninsured expenses, the publicly available uninsured data from each institution's website were surveyed and the actual non-insured unit price for the relevant medical institution was calculated in order to reflect the actual status in each site. Relevant key items included ultrasound fees, uninsured antibiotics, and uninsured tests. Nevertheless, differential costs by ward and optional medical fees based on a patient's preference were excluded from expenses.
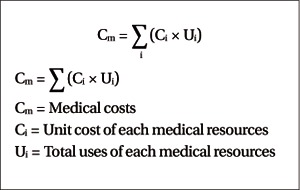
Calculation methods for cost analysis
Medical costs were calculated by multiplying the total use of the relevant medical resource item during the relevant hospital length of stay with the medical cost unit price for the item.
Statistical analysis
SPSS statistical program was used for analysis in this study. For epidemiological survey data, descriptive statistics were presented for results on general and clinical characteristics of all pneumonia patients and pneumococcal disease patients, and the Multivariate (Linear Regression, Logisitic Analysis) was used to analyze factors that affected severity (CURB-65), treatment period, and treatment outcome (survival/death) of all pneumonia patients.
The average per-capita direct medical costs and average percapita daily direct medical costs for all pneumonia patients and pneumococcal disease patients were calculated using direct medical cost results estimated from medical resource utilization. Furthermore, expenses by general and clinical characteristics were analyzed using descriptive statistics, and multivariate (linear regression) was used to analyze factors that influence the average per-capita direct medical costs in all pneumonia patients.
Ethics statement
All joint institutions involved in this study were approved by the institutional review board in each site and written informed consent was obtained from all patients. The approval number at Hallym University Sacred Heart Hospital was 2011-S016.
RESULTS
Baseline characteristics
Results were analyzed in a total of 693 patients after excluding 71 (56 patients with active malignancy, 15 patients with single fungal pathogen detection) from 764 patients from whom data were collected.
Of pneumonia patients, 57.3% was men (397 patients), and mean age was 70.1 ( ± 10.5) yr (Table 1). Across the entire study subjects, a pathogen was identified in 32.9% (228 patients), and of all pneumonia patients, S. pneumoniae was a pathogen in 51 pneumonia patients (7.4%) (among patients with identified pathogen, S. pneumoniae accounted for 22.4%), with less men 49% (25 patients) than women, and mean age of 69.6 yr. Distribution of pneumonia pathogens is presented in Table 2. Of all pneumonia patients, 83.4% (578 patients) had an underlying disease.
Table 1.
Demographic and clinical characteristics of Pneumonia patients

CNS, central nervous system.
Table 2.
Distribution of pneumonia pathogens
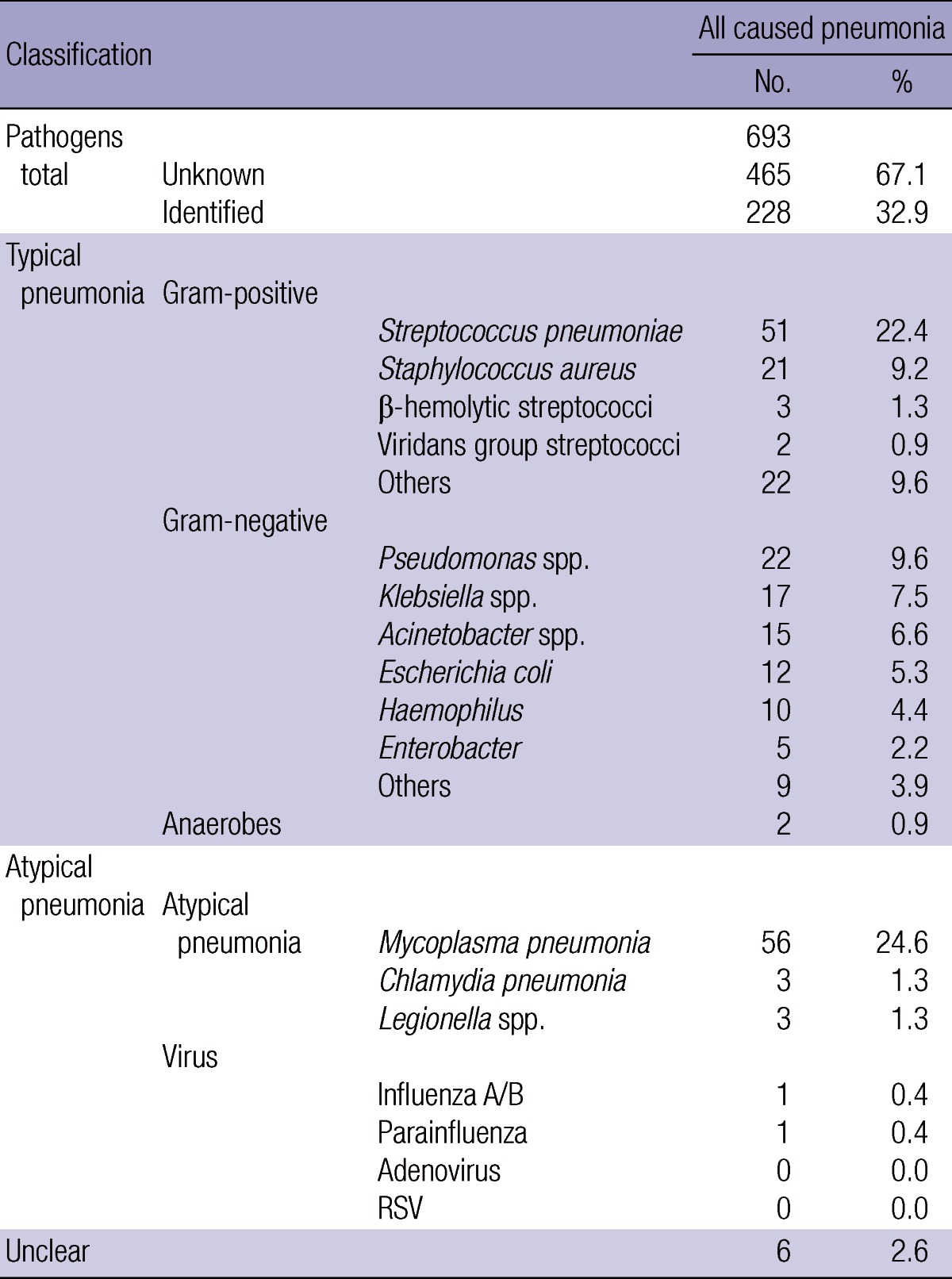
RSV, respiratory syncytial virus.
Disease severity
Mean CURB-65 score in all pneumonia patients was 1.16 points; it was 1.16 in non-pneumococcal pneumonia patients and 1.14 in pneumococcal pneumonia patients (Table 3, P = 0.821). Patients with high severity of 3 points or higher accounted for 7.2% and factors that increased severity were male sex, age, high risk factors among underlying diseases (malignancy, HIV infection, chronic renal failure), and a co-morbid condition of immunosuppressive state.
Table 3.
Disease severity according to CURB-65 score
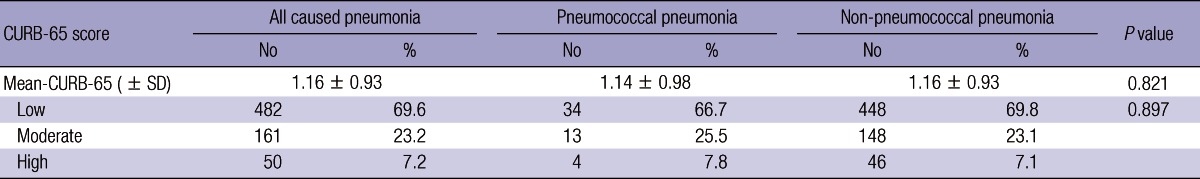
Note1: Score range group was defined as 'Low' for CURB-65 total score of 0-1 point, 'Moderate' for 2 points, and 'High' for 3-5 points.
Treatment duration
Mean treatment period in all pneumonia patients was 22.1 days, mean length of stay was 9.0 days; mean treatment period was 22.3 days in non-pneumococcal pneumonia patients and 19.7 days in pneumococcal pneumonia patients. Mean outpatient visit frequency was 1.3 times in all pneumonia patients, 1.3 times in non-pneumococcal pneumonia patients and 1.1 times in pneumococcal pneumonia patients. Of all pneumonia patients, 68 patients or 9.8% were treated in the ICU and the mean ICU length of stay was 6.3 days. 9.5% of non-pneumococcal pneumonia patients were treated in the ICU and the mean ICU length of stay was 5.9 days; it was 13.7% (7 patients) and 6.6 days, respectively, for pneumococcal pneumonia patients.
Treatment outcomes
Twenty-two (22, 3.2%) of the entire 693 pneumonia patients died and of these, pneumonia-related mortality was 2.6%. Pneumonia-related mortality was 2.3% (15 patients) in non-pneumococcal pneumonia patients and 5.9% (3 patients) in pneumococcal pneumonia patients.
Cost analysis
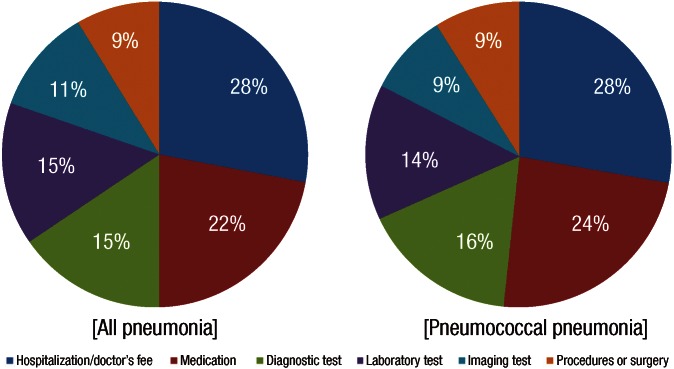
Total per-capita medical fees in all pneumonia patients were KRW 1,969,303 (USD 1,782 ± 1,501); they were KRW 1,945,848 in non-pneumococcal pneumonia patients and KRW 2,264,560 in pneumococcal pneumonia patients (Table 4). Of the total per-capita medical fees in all pneumonia patients, 96.6% (KRW 1,902,434) was incurred as the charge of hospitalization. In terms of the proportion of medical fees by service area, hospitalization (medical fees) represented 28.1%, followed by medication at 22%, and diagnostic test at 15.5%, in all pneumonia patients (Fig. 1).
Table 4.
Total cost for the treatment of pneumonia per patient (unit: KRW)
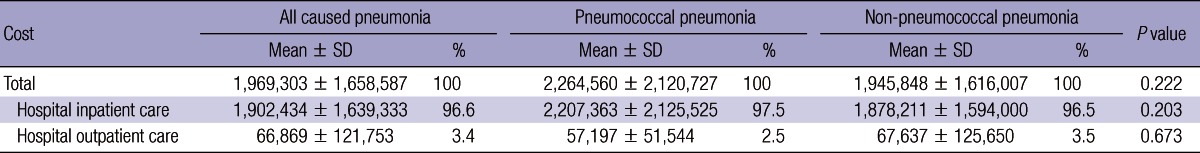
Fig. 1.
Distribution of hospital services costs per patient. *Diagnostic test, test for pathogen diagnosis defined by reference (6); sputum test, blood culture and serology test, etc.
DISCUSSION
This study surveyed patient characteristics and medical costs in 764 pneumonia patients aged ≥ 50 yr who received inpatient care in the Pulmonary Division in 11 medical institutions of general hospital or higher level including local university hospitals. A total of 83.4% of the entire study population had underlying diseases; severity of pneumonia in terms of CURB-65 scores was 1.16 points on average; and S. pneumoniae was identified as the pathogen in 7.4%. Total pneumonia treatment period was 22 days on average and of these, 3.2% patients died during treatment. Total per-capita medical fees for a pneumonia patient were KRW 1,969,303 of which most were incurred as the charge of hospitalization.
In 2010, the mortality due to pneumonia in Korea ranked 6th among all fatal diseases, which is the highest among infectious diseases, warranting various measures to lower the incidence of pneumonia in the future. There are no accurate domestic data available on the incidence and pathogens for pneumonia; this is due to highly difficult diagnosis of atypical pathogens, different test methods used for pathogen diagnosis in each hospital, and different pathogen detection rate by study area or study design. Furthermore, the HIRA data used as the source of epidemiological study on medical cost have weaknesses since reliability on diagnosis is poor and only insurance claims can be confirmed. Given such limitations, this study can provide relatively clear diagnosis of pneumonia since it was conducted in general hospitals and allows accurate calculation of economic expenses by including uninsured spending in the study.
In this study, the pneumonia pathogen was identified in approximately 50% of patients, as in other studies. However, pneumococcus was identified as the cause of pneumonia in 7.4% (15% in patients with an identified pathogen), which was lower than in other studies. The pneumococcal pneumonia rate in Korea has been reported as 13.5% (11) at the lowest when all patients were considered, and 12% (12) in a study in the elderly aged ≥ 65 yr. These rates were higher than the result of this study. The prospective study by Sohn et al. (11), conducted in only 5 institutions in patients aged ≥ 16, made aggressive efforts to detect pathogens by including serology tests. In the study by Yu et al. (12), conducted in a relatively small number of patients (n = 119) in one hospital, the diagnosis rate might have been higher owing to the merit of being conducted in a university hospital.
Pneumococcus and haemophilus tend to be undetected in a sputum culture even shortly after (several hours) antibiotics treatment but this problem can be overcome with the help of a urine antigen test. As this study was conducted only in inpatients ≥ 50 yr mostly in high-level medical institutions, patients are likely to have been prescribed with the first-line antibiotics in local hospitals, possibly resulting in a low pneumococcus detection rate. The low pathogen detection rate might also be attributable to the limitation of a retrospective study.
In this study, the mean treatment period of pneumonia patients was 22 days; 3.2% patients died during treatment; and the pneumonia mortality was approximately 6% for pneumococcal pneumonia. Although the conventional pneumonia treatment period is 7-10 days (13), there have been no sufficient studies on the optimum treatment period and no difference in treatment effect has been reported for shorter treatment duration (14). The reason for a long treatment period in this study is speculated to be the absence of worsening such as the transfer to the ICU during treatment, and inclusion up to the last outpatient visit after a patient's symptom improved, rather than choosing inappropriate antibiotics by considering the low mortality.
In the US, the pneumonia mortality is 2%-3% in all pneumococcal diseases, and approximately 20% in invasive pneumococcal diseases (15). Pneumonia mortality is very high in young children of < 2 yr and the elderly of ≥ 65 yr; the death rate progressively increases from 45 yr and by age 65, it is 60 times higher than that of 30 yr in women, and 40 times higher in men (16). A domestic study in the elderly aged ≥ 65 reported the pneumonia mortality as 28% (12) which warrants intensive management and active preventive efforts for the elderly pneumonia patients. Mortality is also high in chronically ill patients, independently of age-related risks, especially in patients with chronic lung disease, chronic cardiovascular disease, and diabetes (17). For example, the mortality rate increases 4.2-fold in asthma patients, 3.0-fold in lung disease patients and 1.9-fold in cardiovascular disease patients (18). A prospective study in 955 Asian CAP patients has shown that the most common co-morbid conditions were lung disease and cardiovascular disease (19). In this study also, approximately 80% of study subjects had an underlying disease of which chronic cardiovascular disease, chronic lung disease and diabetes were common co-morbid conditions. Given this finding, it would be necessary to implement intensive preventive management in the age group with an identified concurrent underlying disease or a likely co-morbid condition (20).
In pneumococcal-infected patients, the number of pneumonia patients is 17 times higher than that of invasive pneumococcal disease patients. Therefore, we need to focus on pneumonia prevention to lower the overall mortality. Pneumococcal disease is the most common disease for which mortality can be reduced by vaccination. Pneumococcal vaccination rates in young children differ by investigators, ranging from 13% (21) for the single-dose vaccination to approximately 40% vaccination rate in 2007 (22) as estimated in one report. In Korea, adult pneumococcus vaccination is recommended for all adults of ≥ 65 yr or high risk patients aged < 65 yr (23), but public awareness of adult pneumococcus vaccination is low. The adult vaccination rate was 3.4% from a survey of 1,000 adults aged ≥ 65 yr in 15 cities and provinces across the country in 2007. Therefore, it would be crucial to improve the pediatric and adult vaccination rate to reduce the prevalence and mortality of pneumococcal pneumonia as well as the resulting economic burden in Korea. Also, epidemiological data based on accurate diagnosis, as reported in this study, would be critical for accurate judgment of the effectiveness of such strategy.
In this study, total per-capita medical fees were KRW 1,969,303 per pneumonia patient, and medical fees varied by up to 1.5 times among hospitals. This indicates the lack of a physician's willingness to conduct a test or consistent treatment guidelines for pneumonia treatment, rather than the concentration of more severe patients in some hospitals. In Europe, the economic burden of pneumonia is approximately 10 trillion Euros, of which about 60% is spent as the charge of hospitalization, and the economic burden increases with patient's age (24). In 2006, the annual burden-of-illness of pneumococcus (it includes all of the pneumococcal diseases) in Korea was reported as KRW 727.2 billion (9), but as there are no domestic data on pneumococcal incidence, the rationale for this number is weak since this number was calculated by estimating from overseas incidence by age (24). Still, pneumonia accounts for 74% of the entire economic burden of pneumococcal diseases and the burden-ofillness from pneumococcal pneumonia in Korea can be estimated from this number.
For assessment of severity of pneumonia patients, CURB-65 and pneumonia severity index (PSI) are used, and the place of treatment (outpatient, inpatient, ICU admission), selection of antibiotics and prediction of prognosis can be made based on a patient's initial severity (25). PSI is not appropriate for use in a retrospective study due to numerous measurement items. Instead CURB-65 is usually used as it can be readily measured and shows a good correlation with PSI results (26). For patients with the CURB-65 mean score of 1-2 points, hospitalization in a general ward is recommended, and for 3 points, mean mortality rate is 14% and ICU admission is indicated. The mean score for subjects in this study was 1.16, representing the severity that can be treated in a general ward. A retrospective study in 3 university hospitals in Seoul, involving 487 patients aged ≥ 65 yr who were hospitalized due to pneumonia reported the CURB-65 score of mean 1.5 points, similar to this study (27).
The strengths of this study is first of all, accuracy of pneumonia diagnosis as data were surveyed in patients admitted to Pulmonary Division in medical institutions of a general hospital or higher level. Second, pneumonia patients were identified in the reverse temporal order from the treatment completion date of 2010.12.31 in each hospital and were relatively randomly extracted even though this was a retrospective study, resulting in little bias in patient disposition by severity, age, sex, or underlying disease. Third, data calculation was based on confirmation of the accurate medical resource utilization that included uninsured items. Insured items were adjusted for yearly inflation by consistently applying the 2010 insurance fees and the addition by type and nursing (or ICU nursing) personnel category was applied by identifying the actual status in each institution. For uninsured items, the accurate economic burden was calculated by focusing on publicly available uninsured data as disclosed on the website of each institution. Fourth, the study was conducted mostly in referral hospitals (university hospitals), so the assessment of underlying diseases was accurate and there were few transfers to other hospitals, allowing the assessment of treatment outcomes in more than 90% of patients.
There were also limitations in this study. The first limitation is the retrospective study design. Therefore, identification of pathogen strain was not aggressive enough, the level of laboratory facilities and ability of pathogen detection of each center might be different, and may have involved patients who prolonged admission due to other reasons even after pneumonia was treated. Second, as only patients' aged ≥ 50 yr in medical institutions of a general hospital or higher level were included, it may not represent the trend in the entire pneumonia patient population in Korea. Nevertheless, as joint institutions were distributed across the country, it may provide an overall trend.
In summary, this study investigated the characteristics of Korean patients aged ≥ 50 yr who received inpatient care due to pneumonia and the relevant medical costs. When outpatient care was also included, treatment lasted approximately 22 days and KRW 2,000,000 of treatment expenses was incurred on average. This indicates a high level of burden for an individual and society. Given that pneumococcal disease is the most common among infectious diseases for which mortality can be reduced with vaccination, and pneumonia is the most common pneumococcal disease and directly influences mortality, the necessity of vaccination should be stressed. It is revealed that the economic burden of pneumonia is high in Korea, and that the prevention can be considered as an effective strategy.
Footnotes
This study was sponsored by Pfizer Pharmaceuticals Korea Limited.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infect Dis Clin North Am. 2004;18:761–776. doi: 10.1016/j.idc.2004.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Korea National Statistical Office. 2010 annual report on the cause of death statistics: Nationwide. Daejeon: Korea National Statistical Office; 2010. [Google Scholar]
- 3.Marrie TJ. Epidemiology of community-acquired pneumonia in the elderly. Semin Respir Infect. 1990;5:260–268. [PubMed] [Google Scholar]
- 4.Riquelme R, Torres A, El-Ebiary M, de la Bellacasa JP, Estruch R, Mensa J, Fernández-Solá J, Hernández C, Rodriguez-Roisin R. Community-acquired pneumonia in the elderly: a multivariate analysis of risk and prognostic factors. Am J Respir Crit Care Med. 1996;154:1450–1455. doi: 10.1164/ajrccm.154.5.8912763. [DOI] [PubMed] [Google Scholar]
- 5.Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, Kapoor WN. Prognosis and outcomes of patients with community-acquired pneumonia: a meta-analysis. JAMA. 1996;275:134–141. [PubMed] [Google Scholar]
- 6.Woo JH, Kang JM, Kim YS, Shin WS, Ryu JH, Choi JH, Kim YR, Cheong HJ, Uh ST, Park CS, et al. A prospective multicenter study of community-acquired pneumonia in adults with emphasis on bacterial etiology. Korean J Infect Dis. 2001;33:1–7. [Google Scholar]
- 7.Van Mens SP, Meijvis SC, Endeman H, van Velzen-Blad H, Biesma DH, Grutters JC, Vlaminckx BJ, Rijkers GT. Longitudinal analysis of pneumococcal antibodies during community-acquired pneumonia reveals a much higher involvement of Streptococcus pneumoniae than estimated by conventional methods alone. Clin Vaccine Immunol. 2011;18:796–801. doi: 10.1128/CVI.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niederman MS, Mandell LA, Anzueto A, Bass JB, Broughton WA, Campbell GD, Dean N, File T, Fine MJ, Gross PA, et al. Guidelines for the management of adults with community-acquired pneumonia: diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med. 2001;163:1730–1754. doi: 10.1164/ajrccm.163.7.at1010. [DOI] [PubMed] [Google Scholar]
- 9.Lee HJ. Report on economic burden of pneumococcal diseases in Korea 2006. Daejeon: Korea Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 10.Weycker D, Strutton D, Edelsberg J, Sato R, Jackson LA. Clinical and economic burden of pneumococcal disease in older US adults. Vaccine. 2010;28:4955–4960. doi: 10.1016/j.vaccine.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 11.Sohn JW, Park SC, Choi YH, Woo HJ, Cho YK, Lee JS, Sim HS, Kim MJ. Atypical pathogens as etiologic agents in hospitalized patients with community-acquired pneumonia in Korea: a prospective multi-center study. J Korean Med Sci. 2006;21:602–607. doi: 10.3346/jkms.2006.21.4.602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yu CW, Park CW, Hwang BY, Song JY, Park O, Sohn JW, Cheong HJ, Kim WJ, Kim MJ, Park SC. Clinical features and prognosis of community-acquired pneumonia in the elderly patients. Korean J Infect Dis. 2000;32:212–218. [Google Scholar]
- 13.Vogel F. Intravenous/oral sequential therapy in patients hospitalised with community-acquired pneumonia: which patients, when and what agents? Drugs. 2002;62:309–317. doi: 10.2165/00003495-200262020-00005. [DOI] [PubMed] [Google Scholar]
- 14.Dunbar LM, Wunderink RG, Habib MP, Smith LG, Tennenberg AM, Khashab MM, Wiesinger BA, Xiang JX, Zadeikis N, Kahn JB. High-dose, short-course levofloxacin for community-acquired pneumonia: a new treatment paradigm. Clin Infect Dis. 2003;37:752–760. doi: 10.1086/377539. [DOI] [PubMed] [Google Scholar]
- 15.Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infect Dis Clin North Am. 2004;18:761–776. doi: 10.1016/j.idc.2004.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Pnumococcal disease. [accessed on 10 June 2012]. Available at http://www.who.int/entity/ith/diseases/pneumococcal/en.
- 17.Kyaw MH, Rose CE, Jr, Fry AM, Singleton JA, Moore Z, Zell ER, Whitney CG Active Bacterial Core Surveillance Program of the Emerging Infections Program Network. The influence of chronic illnesses on the incidence of invasive pneumococcal disease in adults. J Infect Dis. 2005;192:377–386. doi: 10.1086/431521. [DOI] [PubMed] [Google Scholar]
- 18.Koivula I, Sten M, Mäkelä PH. Risk factors for pneumonia in the elderly. Am J Med. 1994;96:313–320. doi: 10.1016/0002-9343(94)90060-4. [DOI] [PubMed] [Google Scholar]
- 19.Song JH, Jung KS. Treatment guidelines for community-acquired pneumonia in Korea: an evidence-based approach to appropriate antimicrobial therapy. J Korean Med Assoc. 2010;53:20–42. [Google Scholar]
- 20.World Health Organization. Immunization, vaccines and biologicals. [accessed on 20 January 2011]. Available at http://www.who.int/immunization/documents/positionpapers/en.
- 21.Kim KH. Pneumococcal polysaccharide vaccine, performance in local and effectiveness; Presentation at 34th Korean Otologic Society Symposium; 2007. [Google Scholar]
- 22.Choi E. Direct and indirect effects of pneumococcal protein conjugate vaccine. J Korean Med Assoc. 2008;51:119–126. [Google Scholar]
- 23.Kang JH, Kim HB, Sohn JW, Lee SO, Chung MH, Cheong HJ, Choi YH, Choi JH, Choi JY, Choe HJ. Adult immunization schedule recommended by the Korean society of infectious diseases, 2007. Infect Chemother. 2008;40:1–13. [Google Scholar]
- 24.Pneumonia. European lung white book. 2nd ed. Sheffield: European Respiratory Society/European Lung Foundation; 2003. pp. 55–65. [Google Scholar]
- 25.Bartlett JG, Dowell SF, Mandell LA, File TM, Jr, Musher DM, Fine MJ. Practice guidelines for the management of community-acquired pneumonia in adults: infectious diseases society of America. Clin Infect Dis. 2000;31:347–382. doi: 10.1086/313954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Capelastegui A, Espana PP, Quintana JM, Areitio I, Gorordo I, Equrrola M, Bilbao A. Validation of a predictive rule for the management of community-acquired pneumonia. Eur Respir J. 2006;27:151–157. doi: 10.1183/09031936.06.00062505. [DOI] [PubMed] [Google Scholar]
- 27.Kim MJ. Disease burden of pneumococcal infection and serotypes of streptococcus pneumonia in Korean adults. Korea Centers for Disease Control and Prevention; 2007. pp. 30–35. [Google Scholar]