Abstract
This study aimed to identify the risk factors associated with acute hepatitis A virus (HAV) infection in the Korean population. Participants were recruited from five referral hospitals across the country in 2007 and from 11 hospitals in 2009. Patients with positive anti-HAV IgM antibody tests became the case group, while patients treated for non-contagious diseases at the same hospitals were recruited as controls. A total of 222 and 548 case-control pairs were studied in the 2007 and 2009 surveys, respectively. Data from the surveys were analyzed jointly. In a multivariate analysis, sharing the household with HAV-infected family members (OR, 6.32; 95% CI, 1.4-29.6), contact with other HAV-infected individuals (OR, 4.73; 95% CI, 2.4-9.4), overseas travel in 2007 (OR, 19.93; 95% CI, 2.3-174.4), consumption of raw shellfish (OR, 2.51; 95% CI, 1.8-3.5), drinking bottled water (OR, 1.64; 95% CI, 1.3-8.4), and occupation that involve handling food (OR, 3.30; 95% CI, 1.3-8.4) increased the risk of HAV infection. Avoiding contact with HAV-infected individuals and avoiding raw foods eating could help minimize the risk of hepatitis A infection. Immunization must be beneficial to individuals who handle food ingredients occupationally or travel overseas to HAV-endemic areas.
Keywords: Case-Control Studies, Hepatitis A, Korea, Risk Factors
INTRODUCTION
Hepatitis A virus (HAV) is the main cause of acute viral hepatitis in Korea, and typically affects adults in their 20s and 30s (1). HAV infection may be transmitted via the fecal-oral route and intake of contaminated water or food. Non-oral routes of transmission include male homosexual sex, drug use, and blood transfusions (2, 3). The incubation period of hepatitis A is 2-6 weeks. Children with hepatitis A usually do not have any clinical symptoms, while adults experience nausea, weight loss, and jaundice. In some cases, hepatitis A may progress to acute hepatic failure or fulminant hepatitis (1, 4, 5).
In the past, during a period of economic underdevelopment in Korea, children frequently developed HAV immunity through asymptomatic infections (6). However, fast economic growth in the past decades and the subsequent improvement in sanitary conditions have limited HAV transmission among children and increased the non-immune states in adults (7). As a result, since 1997 hepatitis A vaccination in Korea is now recommended for those who travel to areas of high endemicity, laboratory staff handling HAV pathogens, patients with blood clotting disorders, homosexuals, and adults in their 20s or 30s (8). Despite the recommendation, the immunization rate is very low among young adults (9). In a local study, the prevalence of seropositive individuals was just 6.2% in the 20-29 age group (10). Hepatitis A cases in Korea have been increasing since 1998, as shown in the number of patients who receive liver transplants or death due to the disease (11).
Currently, the risk factors for hepatitis A include travel to high-endemic areas, living with school-age children, who may be an asymptomatic reservoir of infection, consumption of raw shellfish, drinking unpurified water, male homosexuality, not washing hands after defecation or before eating, and contact with HAV-infected individuals (3, 12-15). According to a local study in Korea, the risk factors included contact with HAV-infected individuals, living with a child under five years old, consumption of raw vegetables, eating out, and drinking tap water (16). The prevalence and risk factors for hepatitis A are also related to the socioeconomic and sanitary conditions, which vary by country (13, 17).
Because the hepatitis A incidence rate in Korea has risen sharply from 24.1 per 100,000 population in 2007 to 61.7 in 2008 (18), it is thought that the risk factors for HAV infection have changed in parallel with the increase. A large study was recently conducted to estimate the seroprevalence of HAV (19). However, the risk factors for hepatitis A infection have not been investigated in national scale in the Korean population. Therefore, we conducted two case-control studies in hepatitis A patients of tertiary hospitals across the country in 2007 and 2009, in order to identify the risk factors associated with HAV infection in Korea.
MATERIALS AND METHODS
Study design and subjects
In 2007, patients with hepatitis A were recruited for a survey at five tertiary hospitals in the Chungnam (one site), Gyeonggi (three sites), and Jeonbuk (one site) provinces. Patients with non-infectious diseases at the same sites were recruited as case-controls. Between October and December 2007 the participants were interviewed over the telephone. In 2009, in- and outpatients with HAV and their respective controls were recruited at 11 major tertiary hospitals in the Busan (one site), Daegu (one site), Daejeon (one site), Gyeonggi (three sites), Jeonbuk (one site), and Chungnam (one site) provinces. Face-to-face interviews were conducted between April and September 2009.
In both studies, hepatitis A infection was diagnosed when patients showed clear clinical symptoms such as fatigue, stomach-ache, loss of appetite, and nausea. The controls were matched to cases on the basis of gender, age ( ± 2 yr old), and hospitalization or visit dates ( ± 15 days). Patients with a history of hepatitis A infection or vaccination were excluded from the control groups.
A total of 234 and 556 case-control pairs were surveyed in the 2007 and 2009 studies, respectively. Whenever an outbreak was suspected, only the initial case was included in the study. Consequently, 12 and 8 patients were excluded from the 2007 and 2009 surveys, respectively. Survey data from 222 case-control pairs in the 2007 study, and from 548 pairs in the 2009 study, were used in the analysis.
Survey variables
In the 2007 survey, the variables of interest included gender, age, occupation, and exposure to HAV transmission through contact with family members living in the same household and non-family members, shared communal facilities such as orphanages and nursing homes, sexual behaviors, everyday contact, medical contact, use of syringes, overseas travel, intake of raw shellfish (including oysters, mussels, and clams) or other raw foods, and types of water used for drinking 2-6 weeks before diagnosis. It was adequate to analyze separately of seafood and meat, however they were not separately investigated in the initial questionnaire. In addition to the 2007 variables, the 2009 survey included educational level, household income, communal living, living with children under 12 yr old, and hygiene-related behaviors such as hand washing habit (after defecation, after going out, or before eating), use of personal towels, and sharing glasses when drinking alcohol.
Data analysis
The data from both surveys were combined for analysis. Descriptive statistics were used to show the distribution of gender, age, and occupational activities. The Cochran-Mantel-Haenzel test adjusted for study year was used to determine any significant associations between the cases and categorical variables, and McNemar's test was used to estimate percentages and P values. To identify the risk factors for hepatitis A infection, conditional logistic regression analyses were performed. Variables that were significant in the univariate analysis were used in a multivariate model. Results are expressed as odds ratios (OR) with 95% confidence intervals (CI). The threshold for significance was set at P < 0.05. All statistical analyses were performed using SAS 9.2 software (SAS Inc., Cary, NC, USA).
Ethics statement
These studies were reviewed and approved by the institutional review boards of Hanyang University and Eulji University (2007-266 and 09-09). Written informed consent was obtained from all participants in the study.
RESULTS
Sociodemographic characteristics of the combined study population
Table 1 presents the sociodemographic characteristics of the subjects of both surveys. As intended in the study design, there were no significant differences between cases and controls with respect to age or gender. Subjects in their 30s were the largest group among the cases (42.6%). Although occupation and educational levels were significantly different between the groups, household income distribution was similar for cases and controls (P = 0.257).
Table 1.
Sociodemographic characteristics of the combined study populations in the two surveys (2007 and 2009)
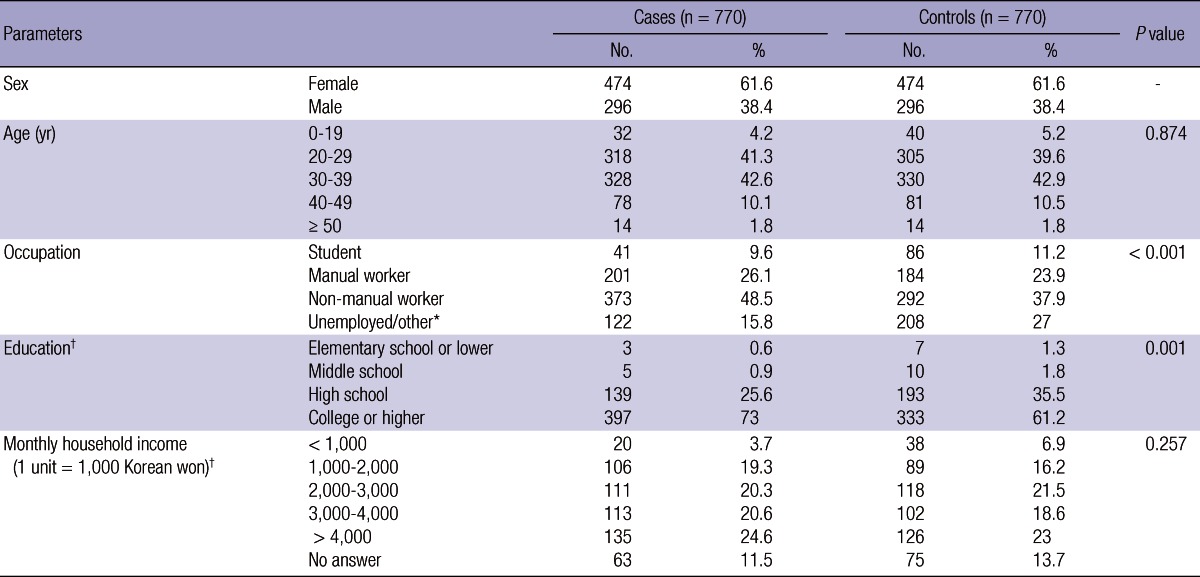
*Including housewives; †Variables applicable only to the 2009 survey (n = 548 case-control pairs).
Risk factors associated with acute hepatitis A infection
Table 2 shows the risk factors associated with acute hepatitis A. In univariate analysis, factors associated with HAV infection included contact with HAV-infected family members in the same household (OR, 8.00; 95% CI, 1.8-34.8), contact with other HAV-infected individuals (OR, 3.97; 95% CI, 2.2-7.1), overseas travel in 2007 (OR, 10.00; 95% CI, 1.3-78.1), consumption of raw shellfish (OR, 2.46; 95% CI, 1.9-3.3), consumption of raw fish (other than shellfish), meat, and other raw food products (OR, 1.55; 95% CI, 1.2-1.9), drinking commercially bottled water (e.g. mineral water) instead of purified tap water (OR, 1.50; 95% CI, 1.2-1.9), and occupation that involves handling food (OR, 2.38; 95% CI, 1.1-5.4). Similarly, multivariate analysis showed that contact with HAV-infected family members in the household (adjusted OR, 6.32; 95% CI, 1.4-29.6), contact with other HAV-infected individuals (adjusted OR, 4.73; 95% CI, 2.4-9.4), overseas travel in 2007 (adjusted OR, 19.93; 95% CI, 2.3-174.4), consumption of raw shellfish (adjusted OR, 2.51; 95% CI, 1.8-3.5), drinking commercially bottled water (e.g. mineral water) instead of purified tap water (adjusted OR, 1.64; 95% CI, 1.3-8.4) and occupation that involves handling food (adjusted OR, 3.30; 95% CI, 1.3-8.4) were independently associated with HAV infection.
Table 2.
Risk factors associated with acute hepatitis A infection
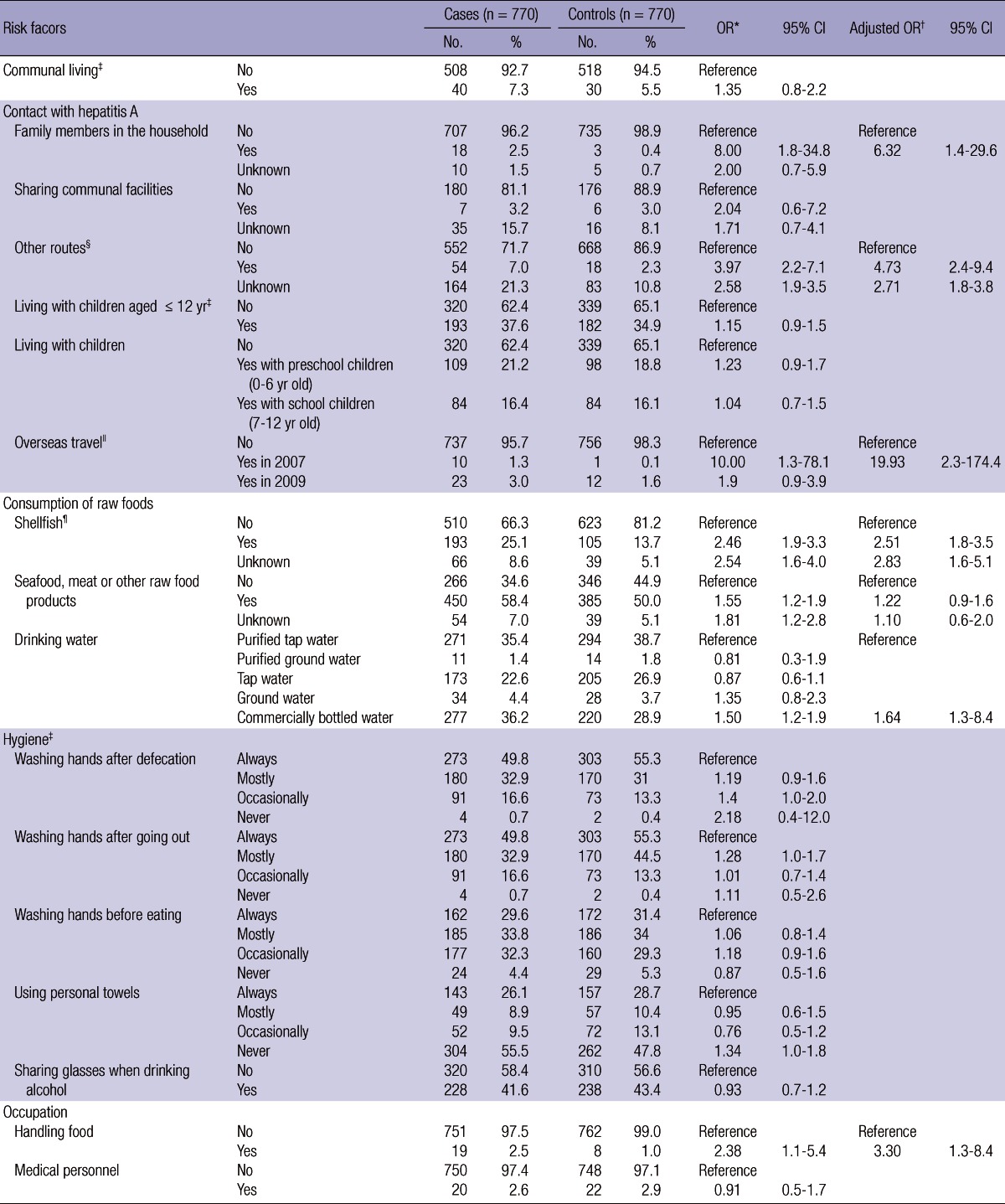
*Adjusted for study year; †Adjusted for study year, contact with HAV-infected family members in the same household or exposure to HAV via other routes, overseas travel, consumption of raw shellfish, seafood, meat and other raw foods, drinking bottled water, and occupation that involves handling food; ‡Variables applicable only to the 2009 survey (n = 548 case-control pairs); §Sexual intercourse, everyday contact, medical contact, use of syringes, etc; ∥Overseas travel 2-6 weeks before diagnosis; ¶Including oysters, mussels and clams. OR, odds ratio; CI, confidence interval.
Transmission of HAV via routes other than through family members was also found to be significant. 54 subjects reported contact with HAV through other routes: 43 (80%) through regular everyday contact, 1 (2%) through sexual contact, 3 (6%) through medical contact as health care worker and 4 (7%) through the use of common syringes. The remaining three respondents reported routes not covered by the surveys. Factors that did not show any significant association with HAV infection were medical professionals, communal living such as orphanages and nursing homes, living with children ≤ 12 yr, washing hands, using personal towels, and sharing glasses when drinking alcohol.
Overseas travel was associated with HAV infection only in the 2007 survey. Of the 10 HAV-infected subjects who had travelled abroad, two had been in China, seven to India and Southeast Asia, and one had travelled to Western Europe. Only one subject in the control group had travelled (to South-east Asia). The average time spent abroad was 6.5 ± 2.6 days, and the interval between the travel and HAV diagnosis was 13.5 ± 3.6 days.
DISCUSSION
In this study, we report that the risk factors for hepatitis A include contact with HAV-infected individuals, overseas travel in 2007, consumption of raw shellfish, drinking commercially bottled water instead of purified tap water, and occupations food handling. The highest odds ratio was associated with overseas travel in 2007, and HAV transmission through contact with family members in the same household was in second place.
In line with previous research, there were a considerably higher proportion of non-manual workers and highly-educated individuals among the cases than controls. Previous studies found that highly-educated adults, or adults with highly-educated mothers, were less likely to be immune and were therefore more prone to symptomatic infections (13, 20-24). The HAV-infected subjects in our study were better educated than the control which suggests that they may have grown up in more sanitary environments with less exposure to HAV.
In contrast to previous research, the distribution of household income in our study was similar in cases and controls. Previous studies demonstrated that the more economically active the families were, the less immune were individuals to hepatitis A (23). However, this correlation could be due to the use of education level as variable rather than household income as the indicator of socioeconomic status in those studies (20-22, 25).
Communal living, investigated in the 2009 survey, was not significantly related to acute HAV infection. However, we found that contact with hepatitis A through infected family members, extramarital sexual contact, everyday contact, medical contact, and contact through other routes such as shared syringes were independent risk factors for hepatitis A infection. Our findings support the results of previous studies, which reported the existence of person-to-person HAV transmission in addition to the usual fecal-oral route (16, 26).
Typically asymptomatic elementary school children can be a reservoir of HAV, and living with children ≤ 12 yr is a known risk factor for hepatitis A infection (14, 16). However, this association was not significant in our study (OR, 1.15; 95% CI, 0.9-1.5). The association was also insignificant when we analyzed into preschool and school children (OR, 1.23; 95% CI, 0.9-1.7 in preschool children and OR, 1.04; 95% CI, 0.7-1.5 in school children).
Travelling to regions where hepatitis is endemic is a well-known risk factor for acute HAV infection (12, 17, 20, 25, 26). Interestingly, overseas travel was a predictor of HAV in 2007 but not in 2009. A sudden spike in hepatitis A cases was observed in Korea in 2008, which suggests that most HAV transmissions occurred during travel abroad until 2007, and that since 2008 when HAV has been endemic.
In the multivariate analysis, eating raw shellfish was shown to be a significant predictor of HAV infection. A small study in 2008 showed that consumption of raw fish, but not raw shellfish, was associated with a significantly high odds ratio (16). On the other hand, eating raw shellfish significantly increased the odds ratio of HAV infection in an Italian study (26). Most studies support the correlation between eating raw shellfish and the risk of hepatitis A infection.
The association between access to drinking water and the risk of hepatitis A has been the subject of many investigations. In our report, drinking commercially bottled water was a significant predictor of HAV infection. Korean national tap water supply is more than 90% and the qualities of drinking commercially bottled water by brands were not so different in the whole country, so the influence of drinking water among different region is not considered (18). In another study, there was no link between drinking bought water and the risk of infection; however, the same study showed that drinking purified tap water or potable spring water was associated with a higher risk of HAV (16). Increased HAV seroprevalence was associated with drinking ground water in a study of elementary school children in Taiwan (27), while another report suggested that an extensive water supply network could contribute to a decrease in HAV infections (13). Access to safe water sources is crucial in preventing hepatitis A, and the issue of waterborne hepatitis A infection is controversial in countries that are completely covered by an infrastructure of water supply as is the case in Korea.
Hygienic practices such as washing hands or using personal towels, covered in the 2009 survey, were not found to influence the risk of acute hepatitis A. However, a previous study demonstrated that lack of hand washing among intravenous drug users increased their risk of HAV infection (15). Another study suggested that the incidence of hepatitis A declined as people became more aware of the importance of personal hygiene in the wake of the influenza A (H1N1) pandemic in 2009 (28). Although hand washing and personal hygiene failed to show a significant association with the risk of HAV in this study, there may be a cumulative effect that could not be detected by the present study design. On balance, the evidence suggests that sanitation is an important factor in preventing hepatitis A.
In our study, working in an occupation that involves handling food was a significant variable, while working in a medical occupation was not. Handling food included not only the persons who handle raw food materials but also all employees in restaurants. Our findings differ from those of a previous study, which did not recommend vaccinating food industry workers or medical personnel (17). Our results suggest that the risk of hepatitis A transmission cannot be completely ruled out in food-handling occupations, and care is needed to avoid infection in food factories and restaurants.
Our study has several limitations. First, some participants in the 2007 survey were interviewed up to 12 months after hospitalization, and recall bias cannot be ruled out. Second, different questionnaires were used in the two surveys, and some variables could not be integrated into the analysis. Third, because antibody testing could not be performed, it is possible that some subjects in the control group were seropositive as a result of asymptomatic infections, even though they had not been diagnosed with hepatitis A.
In 2011, hepatitis A was reclassified as a class 1 legal infectious disease instead of a designated contagious disease. In 2007, the Korean Society of Infectious Diseases recommended that all adults in their 20s should be vaccinated against hepatitis A, as well as adults in their 30s and 40s without immunity (8). In the light of these changes in vaccination policy and the subsequent public health efforts to improve vaccination coverage, our findings may help to raise the awareness of the risk factors for hepatitis A, and prevent its transmission.
We found that direct contact with hepatitis A-infected individuals and consumption of raw shellfish were independent risk factors for hepatitis A infection. Given these findings, direct contact with HAV-infected individuals should be minimized, and caution should be used when preparing and eating raw foods. Personal hygiene must be promoted, while people in contact with hepatitis A patients should be advised to be vaccinated. As handling food is one of the risk factors, improvements in hygiene standards in restaurants should also be encouraged.
In conclusion, this study found that sharing the household with HAV-infected family members, contact with other HAV-infected individuals, overseas travel in 2007, consumption of raw shellfish, drinking commercially bottled water and occupation that involves handling food increased the risk of HAV infection. We recommend that avoiding contact with HAV-infected individuals and using caution when eating raw foods to minimize the risk of hepatitis A infection. Immunization must be beneficial to individuals who handle food ingredients occupationally or travel overseas to HAV-endemic areas.
Footnotes
This study was funded by the Korea Centers for Disease Control and Prevention, Ministry of Health and Welfare, Republic of Korea, grant numbers 2007E0001200 and 2008E0042600.
The authors have no conflicts of interest to disclose.
References
- 1.Lee EJ, Kwon SY, Seo TH, Yun HS, Cho HS, Kim BK, Choe WH, Lee CH, Kim JN, Yim HJ. Clinical features of acute hepatitis A in recent two years clinical features of acute hepatitis A in recent two years. Korean J Gastroenterol. 2008;52:298–303. [PubMed] [Google Scholar]
- 2.Brown GR, Persley K. Hepatitis A epidemic in the elderly. South Med J. 2002;95:826–833. [PubMed] [Google Scholar]
- 3.Franco E, Giambi C, Ialacci R, Coppola RC, Zanetti AR. Risk groups for hepatitis A virus infection. Vaccine. 2003;21:2224–2233. doi: 10.1016/s0264-410x(03)00137-3. [DOI] [PubMed] [Google Scholar]
- 4.Jung YK, Kim JH. Epidemiology and clinical features of acute hepatitis A: from the domestic perspective. Korean J Hepatol. 2009;15:438–445. doi: 10.3350/kjhep.2009.15.4.438. [DOI] [PubMed] [Google Scholar]
- 5.Kang HM, Jeong SH, Kim JW, Lee D, Choi CK, Park YS, Hwang JH, Kim N, Lee DH. Recent etiology and clinical features of acute viral hepatitis in a single center of Korea. Korean J Hepatol. 2007;13:495–502. doi: 10.3350/kjhep.2007.13.4.495. [DOI] [PubMed] [Google Scholar]
- 6.Lee H, Cho HK, Kim JH, Kim KH. Seroepidemiology of hepatitis A in Korea: changes over the past 30 years. J Korean Med Sci. 2011;26:791–796. doi: 10.3346/jkms.2011.26.6.791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JH. Recent epidemiological status and vaccination of hepatitis A in Korea. J Korean Med Assoc. 2008;51:110–118. [Google Scholar]
- 8.Cheong HJ. Vaccination necessary for Korean adults. J Korean Med Assoc. 2011;54:1289–1296. [Google Scholar]
- 9.Baek JH, Kim CO, Park JY, Jeong SJ, Koo NS, Kim HW, Han SH, Choi JY, Song YG, Kim JM. Clinical factors associated with hepatitis A virus seropositivity in HIV-infected adults living in a country with an epidemiologic shift for hepatitis A virus infection. J Korean Med Sci. 2012;27:969–971. doi: 10.3346/jkms.2012.27.8.969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung GE, Yim JY, Kim D, Lim SH, Park MJ, Kim YS, Yang SY, Yang JI, Cho SH. Seroprevalence of hepatitis a and associated socioeconomic factors in young healthy Korean adults. Gut Liver. 2011;5:88–92. doi: 10.5009/gnl.2011.5.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi HK, Song YG, Kim CO, Shin SY, Chin BS, Han SH, Jin SJ, Chae YT, Baek JH, Kim SB, et al. Clinical features of re-emerging hepatitis A: an analysis of patients hospitalized during an urban epidemic in Korea. Yonsei Med J. 2011;52:686–691. doi: 10.3349/ymj.2011.52.4.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Askling HH, Rombo L, Andersson Y, Martin S, Ekdahl K. Hepatitis A risk in travelers. J Travel Med. 2009;16:233–238. doi: 10.1111/j.1708-8305.2009.00307.x. [DOI] [PubMed] [Google Scholar]
- 13.Jacobsen KH, Koopman JS. The effects of socioeconomic development on worldwide hepatitis A virus seroprevalence patterns. Int J Epidemiol. 2005;34:600–609. doi: 10.1093/ije/dyi062. [DOI] [PubMed] [Google Scholar]
- 14.Roberts RJ, Palmer SR. Exposure to school children as a risk factor in a community outbreak of hepatitis A in young adults: a case control study. Epidemiol Infect. 2006;134:803–807. doi: 10.1017/S0950268805005625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy K, Howie H, Sweeney C, Parry J, Molyneaux P, Goldberg D, Taylor A. Hepatitis A virus and injecting drug misuse in Aberdeen, Scotland: a casecontrol study. J Viral Hepat. 2004;11:277–282. doi: 10.1111/j.1365-2893.2004.00503.x. [DOI] [PubMed] [Google Scholar]
- 16.Yoon YK, Chun BC, Lee HK, Seo YS, Shin JH, Hong YS, Sim HS, Kim JY, Kim JY, Park YS, et al. Epidemiological and genetic analysis of a sustained community-wide outbreak of hepatitis A in the Republic of Korea, 2008: a hospital-based case-control study. J Clin Virol. 2009;46:184–188. doi: 10.1016/j.jcv.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 17.Mohd Hanafiah K, Jacobsen KH, Wiersma ST. Challenges to mapping the health risk of hepatitis A virus infection. Int J Health Geogr. 2011;10:57. doi: 10.1186/1476-072X-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Seo JY, Seo JH, Kim MH, Ki M, Park HS, Choi BY. Pattern of hepatitis a incidence according to area characteristics using national health insurance data. J Prev Med Public Health. 2012;45:164–173. doi: 10.3961/jpmph.2012.45.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee D, Ki M, Lee A, Lee KR, Park HB, Kim CS, Yoon BY, Kim JH, Lee YS, Jeong SH. A nationwide seroprevalence of total antibody to hepatitis A virus from 2005 to 2009: age and area-adjusted prevalence rates. Korean J Hepatol. 2011;17:44–50. doi: 10.3350/kjhep.2011.17.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsou TP, Liu CC, Huang JJ, Tsai KJ, Chang HF. Change in hepatitis A epidemiology after vaccinating high risk children in Taiwan, 1995-2008. Vaccine. 2011;29:2956–2961. doi: 10.1016/j.vaccine.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Kaya D, Guler E, Ekerbicer HC, Dilber C, Karabiber H, Guler S, Davutoglu M, Ciragil P. Hepatitis A seroprevalence and its relationship with environmental factors in children of different age groups in Kahramanmaras, Eastern Mediterranean region of Turkey. J Viral Hepat. 2007;14:830–834. doi: 10.1111/j.1365-2893.2007.00886.x. [DOI] [PubMed] [Google Scholar]
- 22.Ceran N, Yüksel Kocdogan F, Mert D, Erdem I, Dede B, Adaleti R, Ozyürek S, Karagül E, Göktaş P. Hepatitis A seroprevalence in children and young adults in Istanbul, Turkey: seroprevalence change and associated factors. J Viral Hepat. 2012;19:72–76. doi: 10.1111/j.1365-2893.2011.01454.x. [DOI] [PubMed] [Google Scholar]
- 23.De Alencar Ximenes RA, Martelli CM, Merchán-Hamann E, Montarroyos UR, Braga MC, de Lima ML, Cardoso MR, Turchi MD, Costa MA, de Alencar LC, et al. Multilevel analysis of hepatitis A infection in children and adolescents: a household survey in the Northeast and Centralwest regions of Brazil. Int J Epidemiol. 2008;37:852–861. doi: 10.1093/ije/dyn114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Venczel L, Brown S, Frumkin H, Simmonds-Diaz J, Deitchman S, Bell BP. Prevalence of hepatitis A virus infection among sewage workers in Georgia. Am J Ind Med. 2003;43:172–178. doi: 10.1002/ajim.10174. [DOI] [PubMed] [Google Scholar]
- 25.Verhoef L, Boot HJ, Koopmans M, Mollema L, Van Der Klis F, Reimerink J, Van Pelt W. Changing risk profile of hepatitis A in the Netherlands: a comparison of seroprevalence in 1995-1996 and 2006-2007. Epidemiol Infect. 2011;139:1172–1180. doi: 10.1017/S0950268810003043. [DOI] [PubMed] [Google Scholar]
- 26.Tosti ME, Spada E, Romanò L, Zanetti A, Mele A SEIEVA collaborating group. Acute hepatitis A in Italy: incidence, risk factors and preventive measures. J Viral Hepat. 2008;15:26–32. doi: 10.1111/j.1365-2893.2008.01025.x. [DOI] [PubMed] [Google Scholar]
- 27.Tsai CF, Lin DB, Chen SC, Chang YH, Chen CY, Lin JB. Seroepidemiology of hepatitis A virus infection among schoolchildren in Taiwan. J Med Virol. 2011;83:196–200. doi: 10.1002/jmv.22000. [DOI] [PubMed] [Google Scholar]
- 28.Byun JM, Kim SG, Zhang YY, Kim YS, Jeong SW, Lee SH, Jang JY, Hong SJ, Moon JH, Kim HS, et al. Influenza A (H1N1) 2009 pandemic calm down the prevalence of acute hepatitis A in the latter half of 2009: Korean Population Study. Korean J Gastroenterol. 2012;59:360–365. doi: 10.4166/kjg.2012.59.5.360. [DOI] [PubMed] [Google Scholar]


