Abstract
Background:
Migraine is a common disorder which has psychiatric sequelae.
Objective:
The objective of this study was to determine the clinical pattern and psychiatric comorbidity of migraine.
Materials and Methods:
100 cases of migraine seen over a period of one year were analysed to know the sociodemographic characteristics, clinical pattern and psychiatric morbidity.
Results:
Maximum patients were between 31-40 years of age group (40%), females (78.0%), married (76%) and housewives (56.0%). Family history of migraine was present in 12% cases. Average age of onset was 22 years. Unilateral and throbbing type of headache was most common. The commonest frequency was one to two per week. Migraine without aura was commonest sub-type (80%). Generalized anxiety disorder (F41.1) was the most common psychiatric disorder (34%), followed by mixed anxiety and depressive disorder (F41.2) (18%) and depressive episode (F32) (14%). In 22% cases, no psychiatric disorder could be elicited.
Conclusion:
The present study confirms that majority patients with migraine had psychiatric disorders. This needs timely detection and appropriate intervention to treat and control the migraine effectively.
Keywords: Migraine, pattern, psychiatric comorbidity
The awareness about the psychological consequences of physical illness is increasing. The research has mainly focused on the common chronic physical illnesses[1] e.g., stroke, coronary artery disease, chronic obstructive airway disease, psoriasis, diabetes mellitus etc., Therefore, disorders such as migraine have not been paid due attention for research or thought of as having fewer consequences.[2] Migraine is a common disorder which has psychiatric sequelae.[3–6] The psychic manifestations of migraine, including confusion, depression, memory impairment, drowsiness, fearfulness and ill humour were described more than a century ago.[7] In further studies,[8–13] general distress, anxiety, fear of impending doom, depression, irritability, fatigue, lethargy, apathy, dullness, changes in motor activity, appetite and sleep have been reported.
The aim of the present study was to study the sociodemographic profile, phenomenology and psychiatric comorbidity in subjects suffering from migraine.
MATERIALS AND METHODS
The present study was conducted in the psychiatry outpatient department of a tertiary care hospital during one year after obtaining clearance from Institutional Ethical Committee. One hundred persons suffering from migraine constituted the study. Their sociodemographic profile, characteristics of migraine, psychiatric history, detailed physical examination as well as mental status examination was recorded. The patients were subjected to specialists opinion (e.g., ophthalmologist, ENT or medical specialist) and relevant investigations (e.g., fundus, X-ray skull, C.T. Scan, EEG, blood sugar etc.,) whenever required. The cases suffering from organic mental disorders, chronic psychiatric disorders, epilepsy or drug dependence were excluded from the study. Migraine was diagnosed according to New International Headache Society definition (1988). International Classification of Diseases 10th revision was used to classify the psychiatric disorders. The results were analyzed at the end of the study.
RESULTS
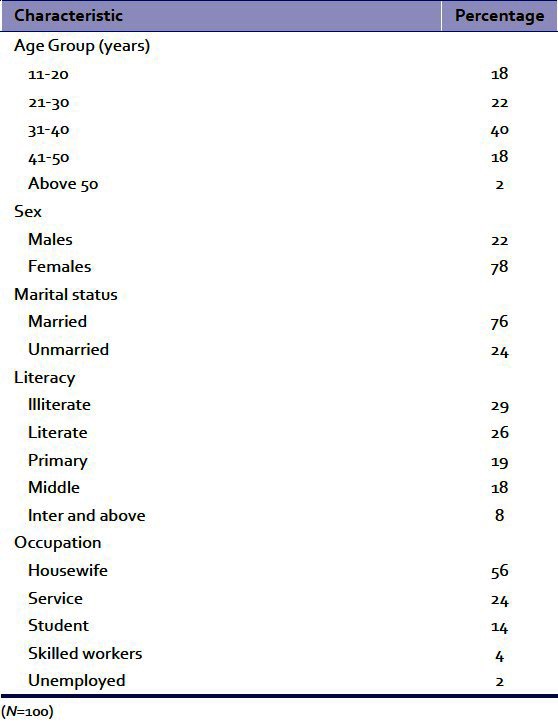
Out of 3245 patients seen during the study period, 100 (3.2%) were suffering from migraine. Maximum patients belonged to age-group of 31-40 years (40%) followed by 21-30 years (22%). Females outnumbered the males significantly (78% versus 22%). A majority of migraineurs were married (76%), illiterate or just literate (55%), Hindus (86%) and housewives (56%) [Table 1].
Table 1.
Socio-demographic characteristics of patients with migraine
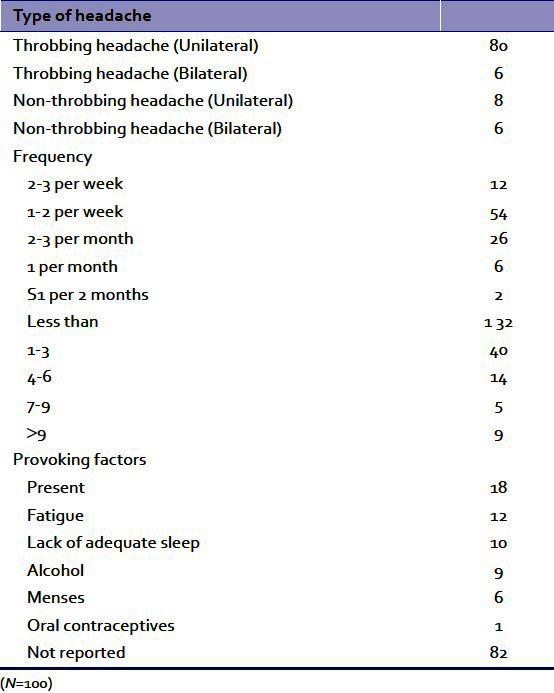
Family history of migraine was present in 12% cases whereas family history of depression was present in 6%. Unilateral headache was present in 88% whereas bilateral headache was seen in 12% cases. Mean age of onset was 22 years. Maximum patients had a total duration of migraine as one to three years (40%) followed by less one year duration (32%). The commonest frequency of migraine was 1-2/week (54%) or 2-3/month (26%). The provoking factors were reported in 18 patients (18%) [Table 2]. Migraine without aura (previously called common migraine) was the commonest variety (81%) followed by migraine with aura (previously called classis migraine) (17%) and complications of migraine (2%) (Only two cases reported complications due to migraine – both with fainting spells). The personality profile of the patients showed anankastic traits (25%), dysthymic traits (20%), histrionic traits (17%), anxious traits (14%), schizotypal traits (10%), cyclothymic traits (6%) and others (8%). The physical comorbidity included hypertension (12%), cervical spondylosis (8%), refractive errors (7%), chronic sinusitis (3%) and diabetes mellitus (2%).
Table 2.
Characteristic of migraine
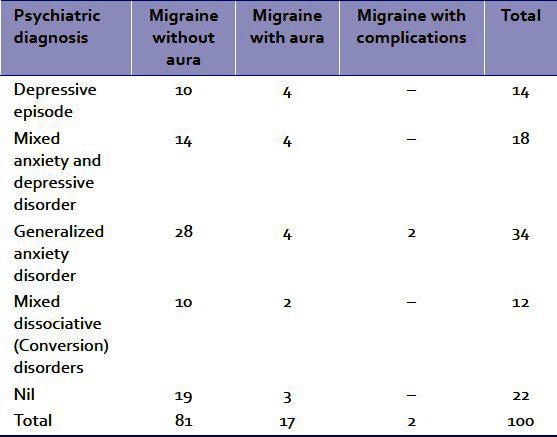
Generalized anxiety disorder (F41.1) was the commonest psychiatric diagnosis (34%) followed by mixed anxiety and depressive disorder (F41.2) (18%), 22 patients (22%) did not have any psychiatric disorder [Table 3].
Table 3.
Psychiatric disorders among subjects with migraine
DISCUSSION
Migraine is reported to be more common in persons between the age of 20 and 45 years.[14] In the present study also, migraine was found to be more common among age group of 31-40 years (40%) followed by 21-30 years of age (22%).
Females were found to suffer more commonly than males (3.5:1). This is also consistent with other studies[9,14–16] and a majority of patients were married (76%). This may be because of the age group commonly affected by migraine.
Unilateral type of headache was much more common than the bilateral type and the headache was throbbing in nature in a majority of migraneurs. This is also consistent with previous studies.[10,17] The frequency of migraine most commonly reported was one to two per week. The mean age of onset was 22 years. There is a wide range of age of onset of migraine reported in the literature (5 to 28 years) with an average age at onset in mid-teens.[17] The provoking factors of migraine were reported by only 18% of patients. They were fatigue, lack of adequate sleep, intake of alcohol, menstruation and oral contraceptives. The other provoking factors for migraine as reported in the literature[17,18] e.g., aged cheeses, caffeine, chocolate, concentrated sugar, dairy products, fermented, pickled food, fruits (bananas, figs, raisins, pineapple etc.,) vegetables (onions, pea, pods, nuts, peanuts), yeast products, meats with nitrites, monosodium glutamate, saccharin etc., could not be identified or reported by the patients in the present study.
Migraine without aura (previously called common migraine) was the commonest subtype seen (in 81%). This is consistent with the reported findings[17] that lifetime prevalence of migraine without aura is about 13% as compared to migraine with aura seen in less than 4% population.
Migraine was strongly associated with psychiatric disorders (in 78%). Generalized anxiety disorder (F41.1) was the commonest disorder followed by mixed anxiety and depressive disorder (F41.2) and depressive episode (F32). Mixed dissociative (coversion) disorders (F44.7) (fits and fainting) were also seen among female migraineurs. Previous clinical and community studies[17–24] have also reported a strong association between migraine and depression as well as anxiety disorders and also vice-versa.[22,25] Migraine is more commonly associated with anxiety disorder than with depression.[5,17] The literature also indicates that patients with migraine are at reduced risk of suffering from anxiety, mood disorders and substance-related disorders compared with medication overuse headache sufferers.[26] Retrospective studies[12,17] on the onset and course of these syndromes showed that the onset of anxiety generally preceded that of migraine whereas the onset of depression tended to occur after that of migraine. The studies on association of personality traits and migraine demonstrate increased prevalence of neuroticism-anxiety and depression as compared to healthy controls.[27,28] But the present study, a cross sectional one, did not determine whether the onset of anxiety disorder and depression preceded or followed the migraine. Health-related outcomes were worst in those with both migraines and a psychiatric disorder and intermediate in those with either condition alone.[16] Future long term follow up studies on larger sample are warranted to study this association.
CONCLUSIONS
The present study confirms that majority (78%) of patients with migraine had psychiatric disorders. This needs timely detection and appropriate intervention to treat and control the migraine effectively.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Jenkinson C. Health status and mood state in migraine sample. Int J Soc Psychiatry. 1990;36(Spring):42–8. doi: 10.1177/002076409003600105. [DOI] [PubMed] [Google Scholar]
- 2.Cox D, Thomas D. Relationship between headache and depression. Headache. 1981;21:261–3. doi: 10.1111/j.1526-4610.1981.hed2106261.x. [DOI] [PubMed] [Google Scholar]
- 3.Gupta R, Bhatia MS. Comparison of clinical characteristics of migraine and tension type headache. Indian J Psychiatry. 2011;53:134–9. doi: 10.4103/0019-5545.82538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hemelsky SW, Lipton RB. Psychiatric comorbidity of migraine. Headache. 2006;46:1327–33. doi: 10.1111/j.1526-4610.2006.00576.x. [DOI] [PubMed] [Google Scholar]
- 5.Breslau N, Davies GC, Andreski P. Migraine, psychiatric disorders, and suicide attempts: An epidemiologic study of young adults. Psychiatry Res. 1991;37:11–23. doi: 10.1016/0165-1781(91)90102-u. [DOI] [PubMed] [Google Scholar]
- 6.Abbas MA, Ismaiel H, Young WB, Hopkins M, Silberstein SD. Psychiatric comorbidity in transformed migraine: Presentation, treatment, impact and outcome. Jefferson J Psychiatry. 2010;23:1–18. [Google Scholar]
- 7.Sick Headache and Some Allied Disorders: A contribution to the Pathology of Nerve Storms. London: J and A Churchill; 1973. Living E – On Megrin; pp. 86–7. [Google Scholar]
- 8.Moersck FP. Psychic manifestations in migraine. Am J Psychiatry. 1974;3:698–716. [Google Scholar]
- 9.Crisp AH, Kalucy RS, McGuinness B, Ralph PC, Harris G. Some clinical, social and psychological characteristics of migraine subjects in the general population. Postgrad Med J. 1977;53:691–7. doi: 10.1136/pgmj.53.625.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kudrow L. Current aspects of migraine headache. Psychosomatics. 1978;19:48–57. doi: 10.1016/S0033-3182(78)71035-2. [DOI] [PubMed] [Google Scholar]
- 11.Garvey MJ, Tollefson GD, Schaffer CB. Migraine headaches and depression. Am J Psychiatry. 1984;141:986–8. doi: 10.1176/ajp.141.8.986. [DOI] [PubMed] [Google Scholar]
- 12.Evans RW, Rosen N. Migraine, psychiatric comorbidities and treatment. Headache. 2008;48:952–8. doi: 10.1111/j.1526-4610.2008.01074.x. [DOI] [PubMed] [Google Scholar]
- 13.Lipton RB, Hamelsky SW, Kolodner KB, Steiner TJ, Stewart WF. Migraine, quality of life and depression: A population-based case-control study. Neurology. 2000;55:629–35. doi: 10.1212/wnl.55.5.629. [DOI] [PubMed] [Google Scholar]
- 14.Waters WE, O'Connor PP. Prevalence of migraine. J Neurosurg Psychiatry. 1957;38:613–6. doi: 10.1136/jnnp.38.6.613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Linet MS, Stewart WF. Migraine headache: Epidemiologic perspectives. Epidemiol Rev. 1984;6:107–39. doi: 10.1093/oxfordjournals.epirev.a036268. [DOI] [PubMed] [Google Scholar]
- 16.Jette N, Petten S, Williams J, Becker W, Wiebe S. Comorbidity of migraine and psychiatric disorders-A national population-based study. Headache. 2008;48:501–16. doi: 10.1111/j.1526-4610.2007.00993.x. [DOI] [PubMed] [Google Scholar]
- 17.Merikangas KR, Risch NJ, Merikangas JR, Welssman MM, Kidd KK. Migraine and depression; association and familial transmission. J Psychiatr Res. 1988;22:119–29. doi: 10.1016/0022-3956(88)90076-3. [DOI] [PubMed] [Google Scholar]
- 18.Blau JN. Premonitory symptoms of migraine. In: Olesen J, Edvinson L, editors. Basic mechanisms of Headache. New York: Elsevier; 1988. pp. 345–51. [Google Scholar]
- 19.Kashiwagi T, McClure JN, Wetzel RD. New York: Oxford University Press; 1990. Headache asum of ideas; pp. 248–58. [Google Scholar]
- 20.Sheftell FD, Atlas SJ. Migraine and Psychiatric Comorbidity: From Theory and Hypotheses to Clinical Application. Headache. 2002;42:934–44. doi: 10.1046/j.1526-4610.2002.02217.x. [DOI] [PubMed] [Google Scholar]
- 21.Hussain AM, Mohit MA, Ahad MA, Alim MA. A study on psychiatric comorbidity among the patients with migraine. TAJ. 2008;21:108–11. [Google Scholar]
- 22.Ortiz A, Cervantes P, Zlotnik G, van de Velde C, Slaney C, Garnham J, et al. Cross-prevalence of migraine and bipolar disorder. Bipolar Disord. 2010;12:397–403. doi: 10.1111/j.1399-5618.2010.00832.x. [DOI] [PubMed] [Google Scholar]
- 23.Lal V, Singla M. Migraine comorbidities-a discussion. J Assoc Physicians India. 2010;54:18–20. [PubMed] [Google Scholar]
- 24.Negro A, D'Alonzo L, Martelletti P. Chronic migraine: Comorbidities, risk factors and rehabilitation. Intern Emerg Med. 2010;5:S13–9. doi: 10.1007/s11739-010-0457-7. [DOI] [PubMed] [Google Scholar]
- 25.Torreli P, D'Amico D. An updated review of migraine and comorbid psychiatric disorders. Neurol Sci. 2004;25:S234–5. doi: 10.1007/s10072-004-0294-4. [DOI] [PubMed] [Google Scholar]
- 26.Radal F. Migraine and psychiatric comorbidity. Rev Neurol (Paris) 2005;161:675–6. doi: 10.1016/s0035-3787(05)85113-6. [DOI] [PubMed] [Google Scholar]
- 27.Cao M, Zhang S, Wang K, Wang Y, Wang W. Personality traits in migraine and tension-type headache: A five factor model study. Psychopathology. 2002;35:254–8. doi: 10.1159/000063829. [DOI] [PubMed] [Google Scholar]
- 28.Tan HJ, Suganthi C, Dhachayani S, Rizal AM, Raymond AA. The coexistence of anxiety and depressive personality traits in migraine. Singapore Med J. 2007;48:307–10. [PubMed] [Google Scholar]


