Abstract
Background:
Few studies have evaluated the supernatural beliefs of patients with schizophrenia. This study aimed to study the personal beliefs, aetiological models and help seeking behaviour of patients with schizophrenia using a self-rated questionnaire.
Materials and Methods:
Seventy three patients returned the completed supernatural Attitude questionnaire.
Results:
62% of patients admitted that people in their community believed in sorcery and other magico-religious phenomena. One fourth to half of patients believed in ghosts/evil spirit (26%), spirit intrusion (28.8%) and sorcery (46.6%). Two-third patients believed that mental illness can occur either due to sorcery, ghosts/evil spirit, spirit intrusion, divine wrath, planetary/astrological influences, dissatisfied or evil spirits and bad deeds of the past. 40% of the subjects attributed mental disorders to more than one of these beliefs. About half of the patients (46.6%) believed that only performance of prayers was sufficient to improve their mental status. Few patients (9.6%) believed that magico-religious rituals were sufficient to improve their mental illness but about one-fourth (24.7%) admitted that during recent episode either they or their caregivers performed magico-religious rituals.
Conclusion:
Supernatural beliefs are common in patients with schizophrenia and many of them attribute the symptoms of mental disorders to these beliefs.
Keywords: Aetiological models, schizophrenia, supernatural beliefs
Help seeking behaviour of mentally ill subjects and their adherence to treatment, can be best understood in the context of the beliefs held by the patients and their family members with respect to the causation and treatment of various psychiatric disorders.
According to ancient Hindu literature, mental disorders are a reflection of abstract metaphysical entities, supernatural agents, sorcery or witchcraft. According to principles of Ayurveda, ill health is an outcome of an imbalance among three kinds of bodily fluids or forces called Dosha and factors which contribute to these imbalances include inappropriate diet; disrespect to the gods, teachers or others; excessive fear or joy leading to mental shock and faulty bodily activity. Accordingly treatments were suggested in the form of herbs and ointments, charms and prayers, moral or emotional persuasion etc.[1] All these beliefs till today influence the causal models and help seeking behaviour.
Many studies from India and other developing countries have assessed explanatory models of schizophrenia as understood by the caregivers of the patients of schizophrenia.[2–8] Studies have also evaluated lay public views about causation of psychiatric disorders.[9,10] Most of these studies suggest that beliefs in supernatural factors are quite prevalent in lay public and caregivers of mentally ill patients.[2–9] Studies also show that many patients and their caregivers seek help of faith healers to get rid of patient's symptoms[2] and it has also been shown that indigenous healing methods are considered complementary to the medical management of mental illness.[11]
In contrast to numerous studies done on the caregivers of patients with schizophrenia, few studies have evaluated causal models and help seeking behaviour in patients with schizophrenia. These studies suggest that although some patients do hold biomedical models, many patients have non-biomedical causal models of schizophrenia.[3,4,12] A study from Tamil Nadu, India, which evaluated the causal models as understood by patients with schizophrenia, reported that 70% of patients with schizophrenia have many non-biomedical causal models.[12]
Over the years urban population and Westernization of India have increased. Due to this, in contrast to the past, many patients now talk of autonomy and participation in treatment decisions. Hence, it is important to understand the causal models held by patients with schizophrenia and their understanding about treatment. The only study, which has evaluated the casual models of patients with schizophrenia, has come from South India and thus there is a lack of data from other parts of India. Further, the studies which have evaluated the causal models have done about 5 years back from South India and about a decade back from North India. So it makes prudent to look at these beliefs in the changing cultural context.
Most of the studies which have evaluated causal models have used semi-structured interview.[12,13] Studies have shown that the interviewer's characteristics can influence the reporting of magico-religious beliefs by the patients and their caregivers.[12] It is also noted that caregivers give socially desirable answers when they are specifically asked about their personal magico-religious beliefs.[2] In this background the present study attempted to study the personal beliefs, aetiological models (magico-religious, stress and biochemical) and help seeking behaviour of patients with schizophrenia using a self-rated questionnaire.
MATERIALS AND METHODS
The study was approved by the Ethics Review Committee of the Institute. This study was conducted at the Department of Psychiatry, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh. A cross-sectional design was employed. For this study 73 patients with diagnosis of schizophrenia were recruited by purposive sampling. To be included in the study, patients were required to be aged between 20-60 years, of either gender with diagnosis of schizophrenia (as per MINI).[14] Self-proclaimed proficiency in reading Hindi was essential. Patients with comorbid axis-I psychiatric disorders (except nicotine dependence), personality disorders, mental retardation and comorbid physical disorder were excluded.
A 17 item Hindi questionnaire was designed specifically to study individual's beliefs in various types of magico-religious beliefs, the role of magico-religious beliefs in causation of mental illness/behavioural abnormalities and the role of treatment based on such beliefs. Additionally, the questionnaire also had the provision to assess the role of stress (which is understood more as tension in our community) and changes in neuro-chemicals in causation of schizophrenia. The questions were developed in the line of Supernatural Attitude Questionnaire, an instrument which was developed about a decade ago by one of the authors (PK). Various items of the questionnaire were based on commonly prevalent magico-religious beliefs in our society. One item in the questionnaire covered the role of stress in development of mental illness and another item evaluated the understanding of patients with respect to the role of change in neuro-chemicals in the brain as the aetiology of mental illness. Regarding treatment, the questionnaire covered areas like seeking treatment from faith healers and performing religious rituals. The last question asked about the prevalence of magico-religious beliefs in the locality to which the patient belongs. The language of the questionnaire was simple and the responders were instructed to answer the questions in “yes” or “no”.
Procedure
Patients were recruited by purposive sampling. Patients with diagnosis of schizophrenia attending the psychiatric outpatient were approached. They were explained the nature of the study and written informed consent was obtained from the patients. Patients were first assessed on MINI to confirm the diagnosis of schizophrenia and to rule out other comorbid psychiatric disorders. Physical comorbidity was ruled on the basis of available history. Only those patients who fulfilled the inclusion and exclusion criteria were recruited.
RESULTS
As shown in Table 1, the mean age of the study sample was 31.65 (SD 8.76) years and mean number of years of education was 12.75 (SD 4.43). Majority of the patients were males, unemployed, Hindu, from non-nuclear family and came from rural background. Nearly half of the patients were married at the time of filling the questionnaire.
Table 1.
Sociodemographic and clinical profile of the patients
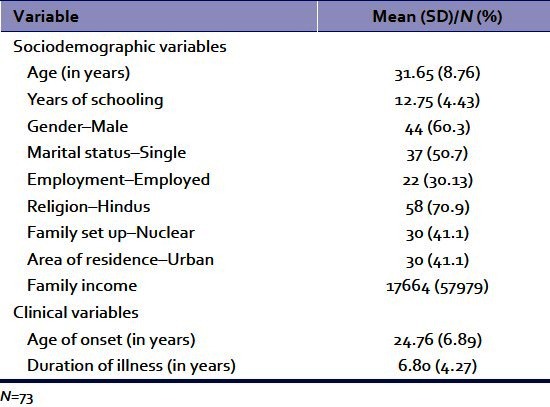
The mean age of onset of schizophrenia was 24.76 (SD 6.89) years and the mean duration of illness was 6.80 (SD 4.27) years. About half of the sample was diagnosed to have paranoid schizophrenia (47.9%) and another 43.8% were diagnosed to have undifferentiated schizophrenia and the rest (8.2%) had other subtypes of schizophrenia.
Of the 73 patients, 40 (58%) had personal convictions in magico-religious beliefs. Nearly similar percentage of patients (61.6%) admitted that people in their community also held these beliefs. As shown in Table 2, the most common among the various magico-religious beliefs were those of sorcery/witchcraft (Jaadu Tona) followed by spirit intrusion (Opari Kasar). Of the patients who had personal magico-religious beliefs, 75% (30 out of the 40 patients) had more than one magico-religious belief.
Table 2.
Beliefs of patients about magicoreligious beliefs
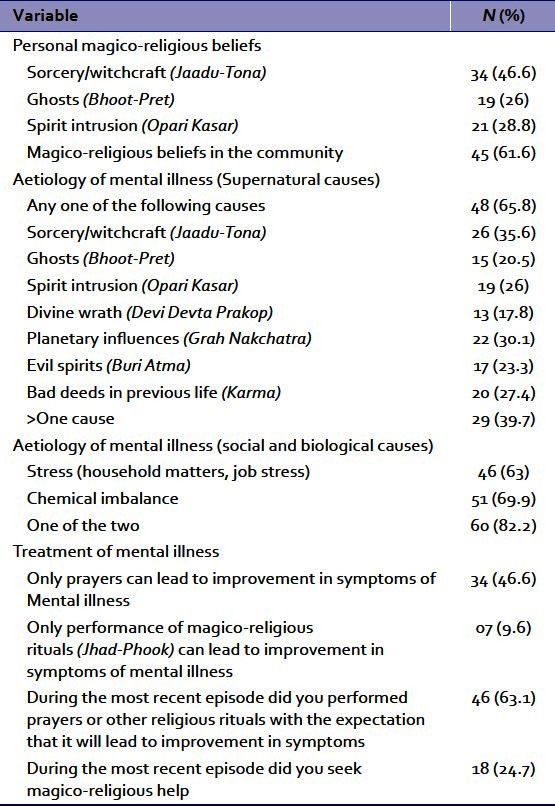
Aetiological models of schizophrenia as held by patients
On questions of causation of mental illness, as shown in Table 2, about one-third of the patients attributed their illness to sorcery/witchcraft (Jaadu Tona) and this was the most commonly attributed supernatural cause. This was followed by planetary/celestial influences (Grah Nakchatra), bad deeds in previous life (Karma), spirit intrusion (Opari Kasar), evil spirits (Buri Atma), ghosts (Bhoot-Pret) and divine wrath (Devi Devta Prakop). Overall, about two-third of the sample attributed their symptoms to one of the above stated causes and about 40% attributed their symptoms to more than one of the above causes.
Additionally, 63% of patients also accepted that stress can lead to the development of mental illness and 70% also agreed that change in neuro-chemical balance can lead to symptoms of mental illness. When both these factors were taken together, 60 (82.2%) patients attributed the symptoms of mental illness to either of these causes, with majority 37 (51%) attributing the same to both.
Of the 60 patients who attributed their symptoms to stress or change in neuro-chemical balance, 42 also attributed their symptoms to magico-religious causes. Only 6 patients attributed their symptoms exclusively to stress or change in neuro-chemical balance, and these 6 patients did not have any conviction in magico-religious beliefs.
Of the total 73 patients, only 7 (10%) did not attribute their mental illness to either magico-religious belief, or stress/change in neurochemicals in the brain.
Beliefs about treatment and help seeking behavior
Offering prayers only was considered sufficient for treatment of mental illnesses by 46% of the patients. A minority of the patients (10%) considered that performing magico-religious rituals only may be sufficient for the management of symptoms of mental illness. In terms of actual practice, about two-third (63.1%) actually performed prayers during the most recent episode to get rid of their symptoms and about one-fourth (24.7%) admitted that magico-religious rituals were performed during their most recent episode of symptoms.
Relationship between supernatural beliefs and sociodemographic and clinical variables Compared to females, males more frequently believed in spirit intrusion (Opari Kasar) (Chi-square test with Yate's correction - 4.12*; P=0.04). Significantly higher percentage of married patients believed in sorcery/witchcraft (Jaadu-Tona) (Chi-square test - 3.94*; P=0.04). Older patients (Spearman Rank Correlation coefficient - 0.266*; P=0.023) and those who were less educated (Spearman Rank Correlation coefficient - 0.290*; P=0.013) more frequently believed in sorcery/witchcraft (Jaadu-Tona). None of the other sociodemographic and clinical variables had any association with personal belief system.
Relationship between aetiological models and sociodemographic and clinical variables
There was no significant difference between the genders with respect to attribution of symptoms to various magico-religious beliefs, stress or change in neuro-chemical balance. Compared to patients who were single at the time of assessment, significantly higher percentage of married patients attributed their symptoms to Ghosts (Bhoot-Pret) (Chi-square test - 4.35*; P=0.037). Significantly lower percentage of patients from rural background attributed their symptoms to stress (Chi-square test - 6.30*; P=0.012). Additionally, patients with lower level of education believed that mental illness can be caused by sorcery/witchcraft (Jaadu-Tona) (Spearman Rank Correlation coefficient - 0.231*; P=0.049) and Ghosts (Bhoot-Pret) (Spearman Rank Correlation coefficient - 0.236*; P=0.044). None of the other sociodemographic variables and clinical variables had any significant association with aetiological models.
None of the sociodemographic variable had significant association when the patients with one or more supernatural etiological model were compared with those without any super-natural causation. Similarly, none of the sociodemographic variable had significant association when the patients with social and biological aetiological model were compared with those without any social and biological aetiological model except for education level of patients.
Relationship between beliefs about treatment, help seeking behaviour models and sociodemographic and clinical variables
There was no significant difference between the genders with respect to performing prayers, magico religious rituals, or beliefs about the usefulness of prayers and magico-religious rituals in symptoms removal. Patient with lower level of education more frequently resorted to magico-religious treatment (Spearman Rank Correlation coefficient - 0.275*; P=0.019), whereas patients from higher income indulged in prayers (Spearman Rank Correlation coefficient - 0.290*; P=0.013). None of the other sociodemographic variables and clinical variables had any significant association with beliefs about treatment and help seeking behaviour.
DISCUSSION
India is in a socio-cultural and economic flux. Due to globalization, there is Westernization in every aspect of life. Hence, the traditional beliefs about mental illnesses are being challenged by the Western biomedical models. In contrast to traditional Indian model, where family members take most of the treatment decisions, the Western biomedical model emphasizes the concept of autonomy and patient's/caregiver's active participation in treatment decisions. Hence, understanding personal beliefs and explanatory models about mental illness as understood by the patients may be useful in planning management strategies. In this era of flux, from social anthropology point of view it is important to understand the behaviour of contemporary human beings.
The present study evaluated personal magico-religious beliefs, role of magico-religious beliefs in causation of symptoms, role of biological and social factors in causation of symptoms and help seeking behaviour of patients with schizophrenia attending psychiatry outpatient clinic of a general hospital psychiatric unit. Previous studies which evaluated aetiological models used semi-structured interviews. Further, some of the studies had used qualitative methods and then presented the data in the quantitative form. It is quite possible that some of the patients gave socially desirable answers to some of these questions when asked directly. Hence, the present study evaluated the personal supernatural beliefs and etiological models using a self-rated questionnaire in which the patients had the option of rating each question as ‘yes’ or ‘no’.
The study sample comprised of patients of schizophrenia of fairly long duration of illness, with a comparatively high degree of education (mean number of years of education - 12.75), primarily from rural background. With increase in literacy rates in the country and availability of treatment for schizophrenia, in future more and more patients of this profile will emerge. Hence, findings of the present study can be generalized to large extent.
This study demonstrates that magico-religious beliefs are quite common in north Indian community and majority of patients have personal magico-religious beliefs. In their study on key relatives from our centre, Kulhara et al.[2] had enquired about the patients supernatural beliefs from the relatives and reported that 35% patients had belief in sorcery during the course of the illness, 25% each believed in ghost/evil spirit and spirit intrusion. The findings of the present study are more or less similar, suggesting that over the years there is no appreciable change in the prevalence of super-natural beliefs in patients with schizophrenia.
Findings of etiological attribution to magico-religious causes in about two-third of the patients in the present study is in concurrence with one of the earlier studies from India,[12] which reported that a vast majority of the patients attributed the symptoms of schizophrenia to magico-religious and mystical factors. This possibly suggests that the magico-religious beliefs are quite prevalent in various parts of the country and further indicate that patients hold aetiological models which necessarily are not in line with professionals’ understanding of the genesis of mental disorders. The finding of the present study with respect to supernatural causes is also supported by findings from other developing countries.[9] The findings of the present study are also supported by some of the studies conducted on the key relative of patients with schizophrenia,[2] but are in contradiction to some.[8] Further, comparison of the findings of the present study with respect to aetiological attribution with the findings of Kulhara et al,[2] reveals that despite the passage of more than a decade during which awareness of various psychiatric disorders and knowledge available pertaining to treatment have presumably increased, the prevalence of magico-religious attribution continues to be same.
In the present study, more than two third of the patients attributed their symptoms to biological causes. This finding is in contrast to study from South India, in which social and biological causes were reported less frequently.[12] The possible reasons for this disparity could be the type of patients included. The study from south India had drug naive first episode psychosis patients, in contrast to the present study's sample which comprised of patients in various phases of the illness. It is quite possible that many of our patients might have received some kind of psychoeducation about their illness during the long contact with psychiatric services and hence had some understanding about biological and social underpinning of their illness. Further, intake of psychotropics and change in symptomatology may also have facilitated believe in biological and social causation of their illness. However, from social anthropology view point, attribution of symptoms to biological causes by two-third of the patients may be a reflection of the changing cultural values.
In an earlier study from our centre, in which key relatives of patients with schizophrenia were evaluated, 46% of them had admitted that supernatural beliefs are generally accepted in the community. In the present study about two-third of the patients admitted that supernatural beliefs are prevalent in their locality. This increase in reporting in the present study could be due to use of self-report measure.
In the present work, the number of patients who sought magico-religious remedial measures during their most recent episode is less than that reported in some of the studies from other parts of India[15] and a study from our centre.[2] This could be a possible reflection of the change in the attitude of the patients towards mental illnesses. It is also possible that patients are under-reporting such practices.
Taken together, from social anthropology view point, more patients now attribute their symptoms to biological causes and fewer patients seek magico-religious measures. This suggests that over the years, it is possible that more and more patients would accept biological causes for their symptoms and seek help from mental health professional.
The data pertaining to association between various illness models and help seeking behaviour are rather limited. The present study shows that patient with lower level of education are more likely to believe that mental illness can be caused by sorcery/witchcraft (Jaadu-Tona) and Ghosts (Bhoot-Pret). Additionally, present study suggests that significantly lower percentage of patients from rural background attributed their symptoms to stress and patient with lower level of education more frequently sought magico-religious treatment. Taken together, it can be hypothesized that supernatural illness models are more common in less educated rural population and seeking intervention from faith-healers is in conformity with their belief and explanatory systems.
The present study is limited by small sample size, purposive sampling and cross-sectional design. The study included patients attending psychiatry outpatient of a general hospital unit, hence the findings cannot be generalized to patients in primary care or a mental hospital settings. Since the study included patients in psychiatry out-patient care, it is quite possible that the findings of the present study may actually be an underestimate of the true prevalence of the supernatural beliefs and aetiological models based on them. Further, we used a self rated instrument to asses the supernatural beliefs and aetiological models. It is quite possible that many participants would have interpreted questions according to the cultural background and would have responded accordingly. Hence, findings should be interpreted in the light of the same.
To conclude, the present study demonstrates that super-natural beliefs are quite common in north Indian community and majority of the patients attribute their symptoms to one of the supernatural cause. However, majority of the patient's additionally have a biological model of causation of their symptoms. This possibly also explains dual nature of seeking treatment i.e., seeking psychiatric treatment and at the same time simultaneously participating in religious and magico-religious rituals for possible amelioration of psychiatric distress. From the perspective service planning and health delivery systems, educating the sufferers and their caregivers as well as traditional healers about the virtues of proper medical treatment of such ailments may be a beneficial effort.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Bhugra D. Psychiatry in ancient Indian texts: A review. Hist Psychiatry. 1992;3:167–86. doi: 10.1177/0957154X9200301002. [DOI] [PubMed] [Google Scholar]
- 2.Kulhara P, Avasthi A, Sharma A. Magico-religious beliefs in schizophrenia: A study from north India. Psychopathology. 2000;33:62–8. doi: 10.1159/000029122. [DOI] [PubMed] [Google Scholar]
- 3.Adebowale TO, Ogunlesi AO. Beliefs and knowledge about aetiology of mental illness among Nigerian psychiatric patients and their relatives. Afr J Med Sci. 1999;28:35–41. [PubMed] [Google Scholar]
- 4.Holzinger A, Kilian R, Lindenbach I, Petscheleit A, Angermeyer MC. Patients’ and their relatives’ causal explanations of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2003;38:155–62. doi: 10.1007/s00127-003-0624-5. [DOI] [PubMed] [Google Scholar]
- 5.Phillips MR, Li Y, Stroup TS, Xin L. Causes of schizophrenia reported by patients’ family members in China. Br J Psychiatry. 2000;177:20–5. doi: 10.1192/bjp.177.1.20. [DOI] [PubMed] [Google Scholar]
- 6.Kurihara T, Kato M, Reverger R, Tirta IG. Beliefs about causes of schizophrenia among family members: A community-based survey in Bali. Psychiatric Serv. 2006;57:1795–9. doi: 10.1176/ps.2006.57.12.1795. [DOI] [PubMed] [Google Scholar]
- 7.Angermeyer MC, Matschinger H. Relatives’ beliefs about the causes of schizophrenia. Acta Psychiatr Scand. 1996;93:199–204. doi: 10.1111/j.1600-0447.1996.tb10632.x. [DOI] [PubMed] [Google Scholar]
- 8.Srinivasan TN, Thara R. Beliefs about causation of schizophrenia: Do Indian families believe in supernatural causes? Soc Psychiatry Psychiatr Epidemiol. 2001;36:134–40. doi: 10.1007/s001270050302. [DOI] [PubMed] [Google Scholar]
- 9.Adewuya AO, Makanjuola RO. Lay beliefs regarding causes of mental illness in Nigeria: Pattern and correlates. Soc Psychiatry Psychiatr Epidemiol. 2008;43:336–41. doi: 10.1007/s00127-007-0305-x. [DOI] [PubMed] [Google Scholar]
- 10.Furnham A, Chan E. Lay theories of schizophrenia: A cross-cultural comparison of British and Hong Kong Chinese attitudes, attributions and beliefs. Soc Psychiat Psychiat Epidemiol. 2004;39:543–52. doi: 10.1007/s00127-004-0787-8. [DOI] [PubMed] [Google Scholar]
- 11.Saravanan B, Jacob KS, Deepak MG, Prince M, David AS, Bhugra D. Perceptions about psychosis and psychiatric services: A qualitative study from Vellore, India. Soc Psychiatry Psychiatr Epidemiol. 2008;43:231–8. doi: 10.1007/s00127-007-0292-y. [DOI] [PubMed] [Google Scholar]
- 12.Saravanan B, Jacob KS, Johnson S, Prince M, Bhugra D, David AS. Belief models in first episode schizophrenia in South India. Soc Psychiatry Psychiatr Epidemiol. 2007;42:446–51. doi: 10.1007/s00127-007-0186-z. [DOI] [PubMed] [Google Scholar]
- 13.Ghane S, Kolk AM, Emmelkamp PM. Assessment of explanatory models of mental illness: Effects of patient and interviewer characteristics. Soc Psychiatry Psychiatr Epidemiol. 2010;45:175–82. doi: 10.1007/s00127-009-0053-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- 15.Compion J, Bhugra D. Experiences of religious healing in psychiatric patients in South India. Soc Psychiatry Psychiatr Epidemiol. 1997;32:215–21. doi: 10.1007/BF00788241. [DOI] [PubMed] [Google Scholar]


