Abstract
The laser photocoagulation is now treatment of choice for various retinovascular disorders. Conventional slit-lamp based laser delivery systems have many limitations including, questionable accuracy, need of contact lens with local anesthesia, and inadvertent damage to fovea. Navigated laser system, a fundus camera based laser delivery system with computer based laser planning and laser treatment without contact lens achieves improved patient compliance, improved accuracy, and treatment ease for the physician, efficient panretinal photocoagulation pattern laser, excellent documentation, and advanced laser training. This article compares navigated laser systems with available conventional and PASCAL laser systems based on the literature and personal experience of the authors.
Keywords: Conventional laser system, navigated laser system, slit-lamp laser system
Introduction
Retinal photocoagulation was introduced by Meyer-Schwickerath in the 1950s.[1] Over time, laser photocoagulation became the standard of care for various retinovascular disorders. Two large, prospective, randomized, multicenter trials (the Diabetic Retinopathy Study and the Early Treatment Diabetic Retinopathy Study) confirmed the effectiveness of laser photocoagulation and established indications and parameters for the treatment of clinically significant macular edema and diabetic retinopathy.[2,3] Conventional laser systems use slit-lamp delivery of the laser treatment, and benefits were appreciated using these systems. However, uncontrolled eye movements and necessity of local anesthesia to avoid the painful experience has always been a matter of concern. Moreover, retinal scarring leads to significant and permanent side effects, such as scar expansion over time, peripheral field loss, as well as decreased color and night vision.[4–6]
The patient comfort, and thus compliance, may be improved by using the shorter exposure burns, avoiding red or infrared (IR) wavelengths with deeper penetration, and by decreasing overall treatment time. To achieve this, Blumenkranz and associates introduced a new laser system in 2005 called as PASCAL (Pattern Scan Laser, OptiMedica, Santa Clara, California).[7] The PASCAL system is a 532 nm frequency-doubled Nd: YAG solid-state laser. It is a semi-automated system that delivers laser pulses with shorter pulse duration in a rapid, predetermined spot pattern. The shorter pulse durations require less total energy to produce burns, providing less scar expansion, less choroidal heating and more uniform energy distribution. Shorter pulse duration and less choroidal penetration also help to reduce pain during the laser treatment. The burns are smaller and more homogeneous and precise, with less inner retinal injury, and potentially, less visual field loss and better clinical outcomes. Initial experience with the PASCAL system was promising;[8,9] however, recent retrospective comparative case series between conventional and PASCAL systems showed that short-duration-pattern retinal burns were less effective in regressing neovascularization in severe diabetic retinopathy.[10]
Conventional laser systems and PASCAL are both based on live fundus viewing through a slit-lamp. Many challenges need to be resolved using a slit-lamp delivery system, including identification of fluorescein angiography (FA)-visible leaking microaneurysms on live fundus view, laterally reversed and vertically inverted orientation, and inadvertent foveal damage due to unexpected eye movements. Another challenge is the exact documentation of the treated area and the treatment parameters, which are essential for future reference. A computer-based targeting system with live view of the fundus on a screen and an eye-tracking system would be useful to overcome these problems.[11] This article compares navigated laser systems with available conventional and PASCAL laser systems based on the literature and personal experience of the authors.
A new, navigated laser approach is recently gaining favor by providing the physician with real-time visibility and treatment control. The Navilas® photocoagulation system (OD-OS, Teltow, Germany) is a unique technology that combines color fundus photography, FA, and IR imaging with a target locked frequency-doubled solid-state laser (wavelength 532 nm). Navilas® is a fundus camera-based laser system as opposed to the conventional slit lamp-based laser systems. In the Navilas® approach, real-time high-resolution images of the retina are obtained with an eye-tracking system at a rate of 25 images/s. The detailed physics of the Navilas® system have been described in previous publications.[12] The system includes both navigated single-spot laser treatment as well as pattern retinal photocoagulation, with distinct advantages over the conventional and pattern laser systems.
Advantages of the navigated laser over conventional and pattern laser systems [Table 1]:
Table 1.
Comparison of the Navigated Laser with conventional and Pattern scanning (PASCAL) Laser Systems
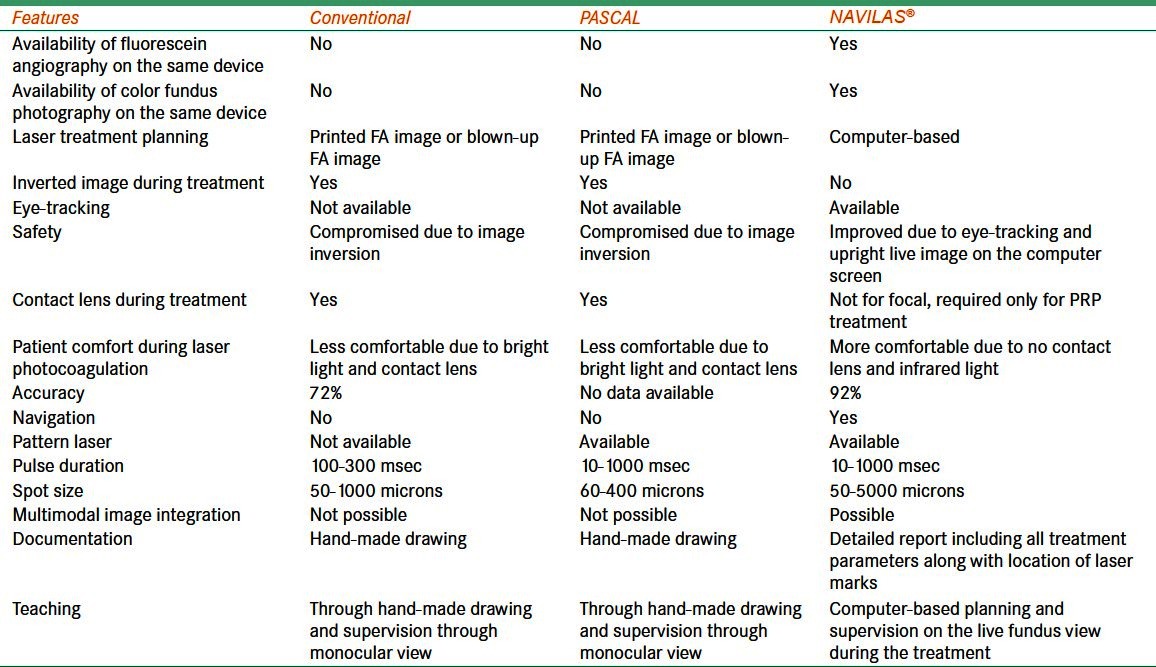
-
Computer-based laser treatment planning: Once fluorescein images are acquired, the physician can easily identify and target microaneurysms or areas of leakage on a single FA image. Because planning is performed directly on the FA image, individual microaneurysms are easily targeted, as well as areas of leakage and capillary dropout. The fluorescein-based treatment plan is projected onto the live IR image of the fundus automatically. Once aligned, the FA image can be turned off to reveal the live IR image of the fundus, with superimposing the designated treatment plan. Each treatment may be quickly and easily tailored for each microaneurysm in respect to laser spot size, pulse duration and laser power [Figure 1]. The treatment may also be planned on the color fundus image.
The Navilas® system represents a significant technological advance in the treatment of retinovascular disorders. With proprietary computer-precise imaging, Navilas® introduces many advantages over the conventional approach. Using a conventional technique, the physician must constantly refer to a printed FA image or a blown-up FA image on the computer screen to visualize leaking microaneurysms. Treatment with the Navilas® system does not require consultation of a printed FA image, and the physician does not have to remember precisely the targeted areas since they have been already planned. The navigated laser treatment plan is always completed, which is not always the case with conventional laser systems.
Safety/eye-tracking: The navigated laser also features an eye-tracking system during laser treatment to minimize inadvertent laser applications, especially near the fovea. Laser application stops immediately with any eye movement, significantly improving the accuracy of treatment delivery compared with conventional laser procedures. Titration of the test burn is performed as per conventional method with power and/or pulse duration modification. Laser power can be individualized for each laser spot during the planning stage and still could be modified for each laser spot during treatment as per the desired burn intensity.
Accuracy: In conventional laser technique, accuracy of the treatment is always a concern. The physician must rely upon photographic paper printouts of FA images to base the treatment, or through direct review of images displayed on an electronic monitor. Availability of simultaneous real-time FA image and live fundus view during laser application improves the treatment accuracy. Our group showed that Navilas® achieved a microaneurysm target rate of 92% compared to 72% for the conventional laser group.[12]
Multimodal image integration: The navigated Navilas® system also has the unique capability to import and save multimodal images taken with other instruments, such as fundus autofluorescence, optical coherence tomography (OCT) retinal thickness maps, and indocyanine green (ICG) angiography images. After importing these images, the Navilas® system is able to align them with the real-time FA image or IR reflectance image of the patient. With this feature, many other clinical applications may be used, e.g. direct treatment applied to leaking spots on FA image in central serous retinopathy, laser photocoagulation of leaking polyps on ICG image in polypoidal choroidovasculopathy, and laser photocoagulation of extrafoveal choroidal neovascularization. Moreover, it is possible to perform treatment of diffuse macular edema directly based on the imported OCT retinal thickness map. This approach achieves more accurate and effective laser treatment. OCT thickness map integration is particularly important in diabetic macular edema to identify areas of retinal thickening that are not visible on FA image, and otherwise would not be treated if only FA images were used as a treatment template [Figure 2]. Sometimes diffuse leakage is visible on FA image, but it is not necessarily associated with retinal thickening or cyst formation on OCT scans, because mild diffuse leakage may not be sufficient to create obvious patterns of intraretinal edema, or because the edema may be intracellular. Therefore, additional clinical information from OCT thickness map helps to maximize the advantages of retinal photocoagulation.
Patient comfort: The Navilas® system is fundus-camera based, not slit-lamp based, like other available laser systems. High frequency of image acquisition (25 frames/s) provides composite live view of the fundus, free of reflexes, at all times. Laser treatment can be performed with IR light without a contact lens, resulting in more comfort for the patients. Treatment-related pain following Navilas® laser has been reported to be significantly lower compared to that of conventional laser system.[13]
Treatment ease: The Navilas® system provides live fundus view on the computer screen during laser treatment, which avoids loss of orientation on the fundus of the patient due to inverted and reversed images. Toggling between color and IR image can be done easily to assure accurate and sufficient whitening of the retinal burns.
-
Efficient panretinal photocoagulation (PRP): PASCAL laser significantly improved the patient comfort with much faster laser application for PRP compared to conventional laser. However, peripheral burns are poorly focused and so are not uniformly circular in shape and therefore, less intense. This could be the cause of reduced efficacy of PASCAL laser compared to conventional panretinal laser. Moreover, this distortion could be compressed into a linear pattern and may cause damage to Bruch’s membrane.
The fundus-camera-based Navilas® system avoids this image distortion and results in a maintained circular, focused projection. This provides a uniform and equally intense laser pattern in the periphery [Figure 3].
Documentation: The Navilas® laser system provides a photographic report of each laser application of the planned treatment marked with a circle. All the information including, fluorescein angiogram, laser treatment plans and also detailed report of the treatment session (including total power, average power, pulse duration, number of delivered laser spots) is saved electronically. This information could be useful for follow-up and further treatments, especially for sub-threshold laser treatments, which are not visible and need to be documented. This brings a new level of transparency to the laser treatment [Figure 4].
Teaching process: In conventional laser system, teaching laser treatment included hand-drawing and supervision/observation through monocular view. The Navilas® system provides a clear large view on the computer screen for physicians in training to learn the planning and application of laser treatment under the supervision of the trained attending. This ensures patient safety as well.
Financial benefits: The Navilas® laser system comprises high-resolution color fundus photography, FA and laser system. This single system conserves office space by combining three imaging modalities into one platform. Patient flow is also optimized while utilizing existing technical staff without the need for additional specialists.
Figure 1.

Screen shot of the navigated laser system showing laser plan for an eye with diabetic macular edema. Yellow circles (thin arrows) show “no treatment zone” and planned laser spots to individual microaneurysm are seen as multiple green small circles (thick arrow). Left panel shows various laser patterns and parameters
Figure 2.
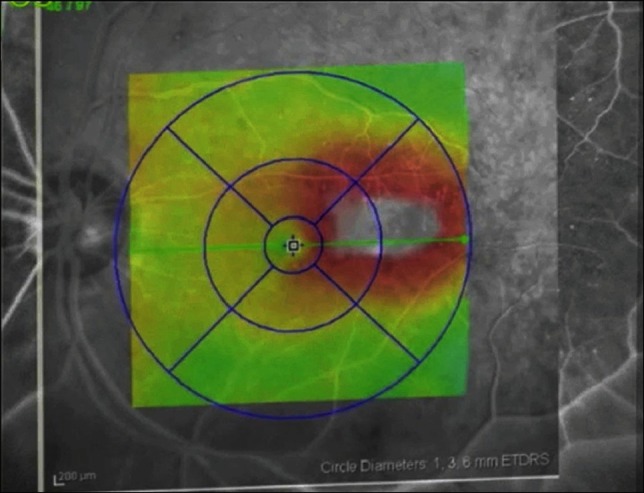
Macular thickness map of spectral domain optical coherence tomography overlaid on fluorescein angiograph for laser treatment planning on navigated laser system
Figure 3.
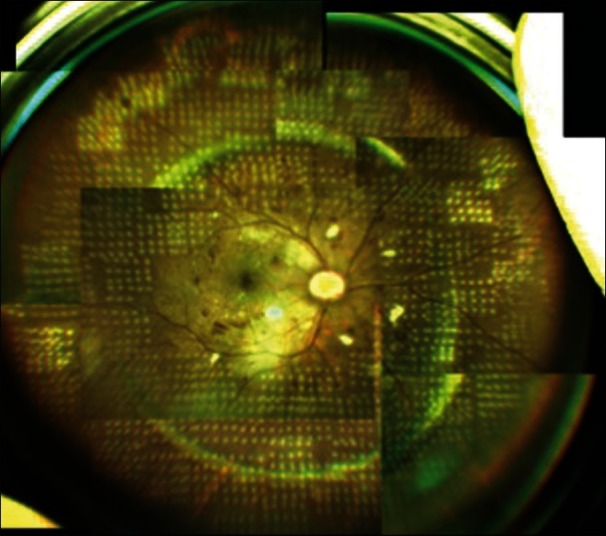
Color fundus image shows panretinal photocoagulation pattern laser spots after navigated laser photocoagulation
Figure 4.
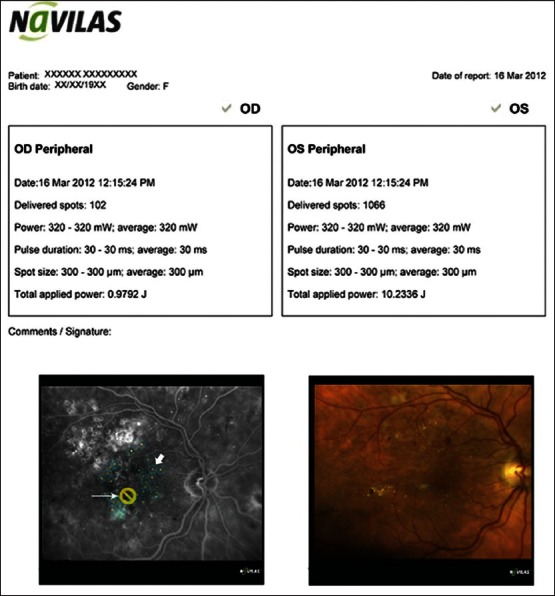
Navigated laser report showing laser parameters along with fluorescein angiograph and color photo after laser photocoagulation. Fluorescein angiograph (lower left image) shows no treatment zone as yellow circle (thin arrow) and lasered spot (central yellow spot with in a blue circle - thick arrow)
One of the limitations about Navilas® laser system is unavailability of ICG angiography on the system, unlike other available system in which we can perform simultaneous FA and ICG. Similarly, autofluorescence imaging and stereoscopic photography is not possible at present in Navilas® laser system. Up to now, only few studies are available which discusses accuracy and short term results of Navilas® laser system in diabetic macular edema. However, further studies with long-term follow-up on a larger group and in proliferative diabetic retinopathy as well as other retinovascular disorders will be needed to prove the efficacy of this laser.
According to the manufacturer Navilas® laser system is less expensive than refractive lasers with eye tracking, but claims a price premium over conventional lasers including pattern lasers, which can be justified with the more sophisticated digital approach to retinal navigation. Furthermore, costs for a more accurate navigated laser need to be viewed in the light of potential patient burden and healthcare cost reduction in the Anti-VEGF era.
In summary, the Navilas® laser system has several advantages compared to conventional laser systems and slit-lamp-based pattern lasers with regard to improved patient compliance, reduced discomfort, improved accuracy, efficient PRP pattern laser, detailed reporting, and advanced laser training. With all these advantages, the Navilas® system takes patient management to a much more advanced and efficacious level.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Meyer-Schwickerath G. Photo-coagulation of the ocular fundus and the retina. Ann Ocul (Paris) 1956;189:533–48. [PubMed] [Google Scholar]
- 2.The Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8. Ophthalmology. 1981;88:583–600. [PubMed] [Google Scholar]
- 3.Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Ophthalmology. 1987;94:761–74. doi: 10.1016/s0161-6420(87)33527-4. [DOI] [PubMed] [Google Scholar]
- 4.Schatz H, Madeira D, McDonald HR, Johnson RN. Progressive enlargement of laser scars following grid laser photocoagulation for diffuse diabetic macular edema. Arch Ophthalmol. 1991;109:1549–51. doi: 10.1001/archopht.1991.01080110085041. [DOI] [PubMed] [Google Scholar]
- 5.Lewen RM. Subretinal neovascularization complicating laser photocoagulation of diabetic maculopathy. Ophthalmic Surg. 1988;19:734–7. [PubMed] [Google Scholar]
- 6.Lewis H, Schachat AP, Haimann MH, Haller JA, Quinlan P, von Fricken MA, et al. Choroidal neovascularization after laser photocoagulation for diabetic macular edema. Ophthalmology. 1990;97:503–10. doi: 10.1016/s0161-6420(90)32574-5. [DOI] [PubMed] [Google Scholar]
- 7.Blumenkranz MS, Yellachich D, Andersen DE, Wiltberger MW, Mordaunt D, Marcellino GR, et al. Semiautomated patterned scanning laser for retinal photocoagulation. Retina. 2006;26:370–6. doi: 10.1097/00006982-200603000-00024. [DOI] [PubMed] [Google Scholar]
- 8.Muraly P, Limbad P, Srinivasan K, Ramasamy K. Single session of Pascal versus multiple sessions of conventional laser for panretinal photocoagulation in proliferative diabetic retinopathy: A comparitive study. Retina. 2011;31:1359–65. doi: 10.1097/IAE.0b013e318203c140. [DOI] [PubMed] [Google Scholar]
- 9.Sheth S, Lanzetta P, Veritti D, Zucchiatti I, Savorgnani C, Bandello F. Experience with the Pascal ® photocoagulator: An analysis of over 1,200 laser procedures with regard to parameter refinement. Indian J Ophthalmol. 2011;59:87–91. doi: 10.4103/0301-4738.77007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chappelow AV, Tan K, Waheed NK, Kaiser PK. Panretinal photocoagulation for proliferative diabetic retinopathy: Pattern scan laser versus argon laser. Am J Ophthalmol. 2012;153:137–42. doi: 10.1016/j.ajo.2011.05.035. e2. [DOI] [PubMed] [Google Scholar]
- 11.Hammer D, Ferguson R, Magill J, White M, Elsner A, Webb R. Image stabilization for scanning laser ophthalmoscopy. Opt Express. 2002;10:1542–9. doi: 10.1364/oe.10.001542. [DOI] [PubMed] [Google Scholar]
- 12.Kozak I, Oster SF, Cortes MA, Dowell D, Hartmann K, Kim JS, et al. Clinical evaluation and treatment accuracy in diabetic macular edema using navigated laser photocoagulator NAVILAS. Ophthalmology. 2011;118:1119–24. doi: 10.1016/j.ophtha.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 13.Kernt M, Cheuteu RE, Cserhati S, Seidensticker F, Liegl RG, Lang J, et al. Pain and accuracy of focal laser treatment for diabetic macular edema using a retinal navigated laser (Navilas) Clin Ophthalmol. 2012;6:289–96. doi: 10.2147/OPTH.S27859. [DOI] [PMC free article] [PubMed] [Google Scholar]


