Abstract
Background:
Parkinson's disease (PD) is a progressive neurodegenerative disorder causing motor and non-motor symptoms. The latter are common and include autonomic dysfunction, cognitive impairment, and sleep difficulties. Many of the non-motor aspects of PD such as sleep disturbance are more common and significantly affect the day-to-day activities of patients and their quality of life. The most important aim of this study was to evaluate the sleep quality in patients with PD.
Methods:
This case-control study was performed on patients with PD referred to the Neurology Clinic of our teaching hospital in 2011. Thirty-four patients with PD and 34 healthy people as control group were enrolled in this study. Sleep quality of patients and control was evaluated by Parkinson's disease sleep scale (PDSS) questionnaire. PDSS is a reliable and valid tool to measure sleep disorders in PD.
Results:
The mean total PDSS score in patient group was 55.29 (SD = 26.92) indicating moderate to severe sleep disturbances whereas, the mean total score in control group was 20.34 (SD = 10.65). Difference between the two groups’ mean scores was significant (P < 0.05).
Conclusions:
Our study demonstrated that patients with PD experienced poorer nocturnal sleep quality than the control group.
Keywords: Parkinson's disease, Parkinson's disease sleep scale, sleep disturbances, sleep quality
INTRODUCTION
Parkinson's disease (PD) is a progressive neurodegenerative disorder that affects nerve cells in part of the brain that controls muscle movements. It produces movement symptoms such as tremor, rigidity, bradykinesia, akinesia, and postural instability.[1,2] Furthermore, non-motor symptoms including, autonomic dysfunction, cognitive impairment, mood disorders, and specially sleep problems are frequent.[3,4] Sleep disorders are commonly presented in patients with PD and other neurodegenerative disease. Epidemiological studies estimated, the prevalence of 60-98% of sleep disturbances in patients with PD[5,6] and they are more often affected than the age matched control group.[1] Patients with PD often complain of poor sleep, non-restorative sleep, excessive daytime sleepiness, delay in falling asleep, difficulty in staying asleep, unexpectedly asleep during daytime and rapid eye movement sleep behavior disorder.[7–10] Additionally, sleep disordered breathing, restless legs syndrome, behavioral and mood disorders, and periodic limb movements in sleep are frequently observed in this population.[6,11] Despite well-known sleep disturbances in PD, sleep has been a rare and mostly neglected topic in Parkinson research. The etiology of sleep problems in PD is not well-understood, as they may arise from the pathology of the disease or from other disease-related factors such as motor dysfunction, dopaminergic medication, and mood disturbances.[12–14] Different questionnaires were developed to assess the presence or absence of sleep disorders and also to provide a guide for response to treatment.[15–23] Better treatment of non-motor aspects of the illness could reduce their sufferings.[24–26] The aim of this study was to evaluate quality of sleep in patients with PD using Parkinson disease sleep scale (PDSS).
METHODS
This was a case-control study carried out on patients with PD and healthy control group in an academic hospital in 2011. Ethical Committee of the hospital approved the study. Included patients were those with PD referred to Neurology Clinic of the university hospital. These patients were selected by convenience sampling method. Patients with either early PD, unwillingness to take part in the study, or Parkinson plus syndrome and those on sedative drugs were excluded. The patients gave informed consent. Sleep quality of patients was asked face-to-face using PDSS questionnaire. PDSS assesses wide spectrum of nocturnal symptoms and is easy to use for patients. It has been successfully validated and is a reliable tool to measure sleep disorders and response to treatment in patients with PD.[27] PDSS is based on visual analog scoring method, addressing 15 commonly reported symptoms associated with sleep disturbances in PD. It was completed in the clinic or at the patient's bedside. Scores for every question varied from ever (0) to never (10), except for the first question, which was scored from bad (0) to excellent (10). Top score was 150. PDSS questions are grouped according to sleep quality (questions 1-3), night fatigue (questions 4 and 5), distressed dreams and hallucinations (questions 6 and 7), nocturia (question 8), urinary incontinence (question 9), numbness or tingling (question 10), painful cramps (question 11), early wake up (question 12), tremor on wake up (question 13), tired after wake up (question 14), and unexpectedly falling asleep (question 15).[28] This study evaluated 34 patients with PD, and 34 healthy age and sex matched control group. The data were analyzed using Chi-square test, t-test, and Pearson correlation by SPSS-18 (SPSS Inc., Chicago, IL) and P value ≤0.05 was considered significant.
RESULTS
We interviewed 34 patients with PD in the case group and 34 healthy people as the control group. The mean age ± SD of the case and control groups was 62.7 ± 13.4 and 61.7 ± 11.5 years, respectively. According to t-test, no statistically significant difference between the two groups’ mean age was seen (P = 0.71). The age distribution is shown in Figure 1. 26 (76.5%) and 23 (67.6%) in the case and control groups were male. According to Chi-square test, there was no statistically significant difference between the two groups’ gender distribution (P = 0.42). The mean score ± SD of sleep scale in the case and control groups was 55.29 ± 26.9 and 20.34 ± 10.65, respectively. According to t-test, the difference between the two groups was statistically significant (P < 0.001). The distribution of sleep scales is shown in Figure 2. Furthermore, the mean score ± SD in males and females was 40.98 ± 27.5 and 31.84 ± 25.44, respectively, and no statistically significant difference between two genders was seen (P = 0.22). To determine, if sex and age were confounding factors, linear regression analysis was carried out and sex and age revealed no confounding effects on the relationship of PD and quality of sleep (P = 0.44 for sex and P = 0.77 for age). The mean ± SD of disease duration was 4.5 ± 4.26 years (range, 0.16-20). Pearson's correlation demonstrated no relationship between sleep scale and duration of disease in patients with PD (P ≥ 0.64). The relationship between disease duration and sleep scale is shown in Figure 3.
Figure 1.
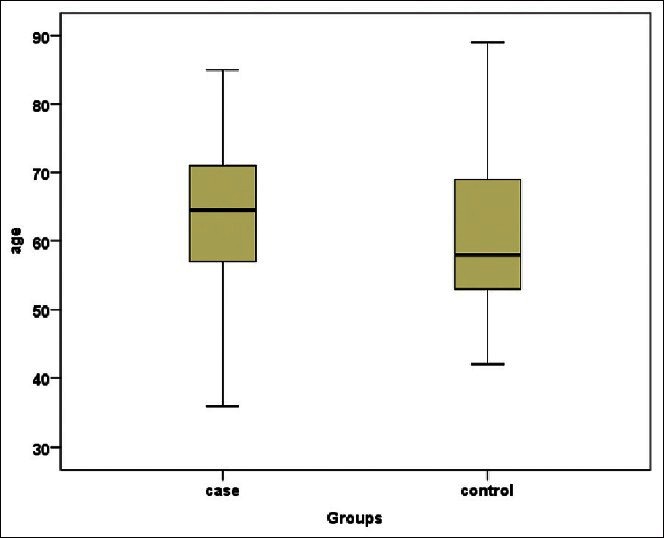
Age distribution between case and control groups
Figure 2.
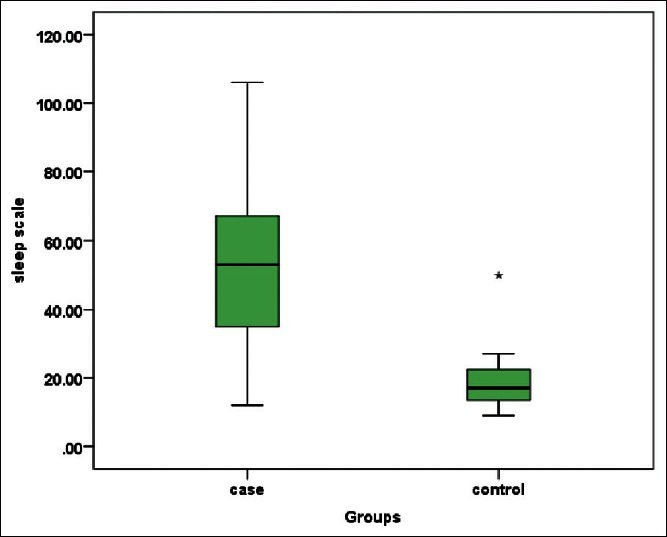
Sleep scale distribution between case and control groups
Figure 3.
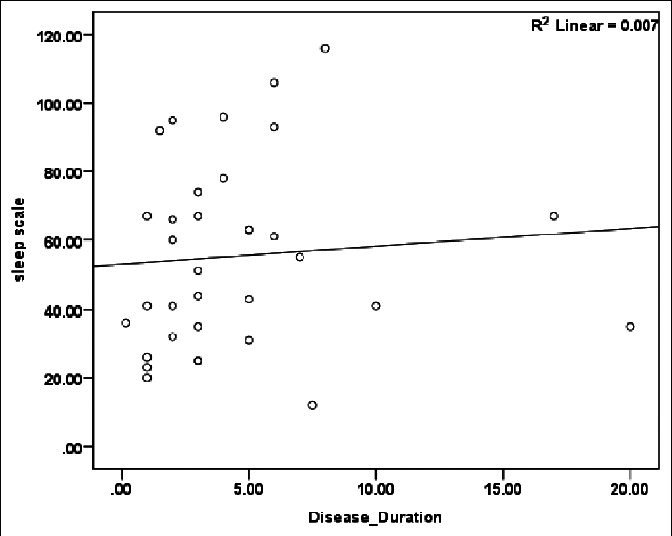
The relationship between sleep scale and duration of disease
DISCUSSION
The purpose of this study was to determine, the quality of sleep in patients with PD in comparison with that in the control group. PDSS can be used as a simple bedside screening method of sleep disturbances.[3,11] The study of Menza et al. demonstrated that sleep problems were very common in PD, affecting about three quarters of the patients.[2] The most common disturbance was difficulty staying asleep through the night, however, may actually affect any aspect of sleep. Other co-occurring sleep disorders, such as sleep apnea, REM behavior disorder, and restless legs syndrome are also very common.[29]
These sleep problems are associated with a poor quality of life for the patient and the caregiver.[27,30] The etiology of insomnia in PD is multi-factorial. Previously, established causes include, advanced age, nocturnal motor symptoms, and psychiatric complications such as depression and hallucinations, and also medication effects, which may disrupt the sleep architecture and lead to motor fluctuations.[3,13]
This study showed no significant relationship between poor sleep quality and duration of disease. Previous research has indicated an association between poor sleep and duration of diseases.[31] Our study demonstrated poor nocturnal sleep quality in patients with PD compared with the control group. New ways such as skin patches to improve quality of sleep in patients with PD are recently introduced in the literature.[32] Better treatment of sleep disturbances can improve the quality of life in the Parkinson disease.
CONCLUSION
Our study demonstrated poor nocturnal sleep quality in patients with PD compared with the control group. Better treatment of sleep disturbances can improve the quality of life in Parkinson disease.
ACKNOWLEDGMENTS
We appreciate Ali Mehrabi, epidemiologist, who conducted the data analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Scheller D, Dürmüller N, Moser P, Porsolt RD. Continuous stimulation of dopaminergic receptors by rotigotine does not interfere with the sleep-wake cycle in the rat. Eur J Pharmacol. 2008;584:111–7. doi: 10.1016/j.ejphar.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 2.Menza M, Dobkin RD, Marin H, Bienfait K. Sleep disturbances in Parkinson's disease. Mov Disord. 2010;25:S117–22. doi: 10.1002/mds.22788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perez-Lloret S, Rossi M, Nouzeilles MI, Trenkwalder C, Cardinali DP, Merello M. Parkinson's disease sleep scale, sleep logs, and actigraphy in the evaluation of sleep in parkinsonian patients. J Neurol. 2009;256:1480–4. doi: 10.1007/s00415-009-5141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Müller T, Jugel C, Ehret R, Ebersbach G, Bengel G, Muhlack S, et al. Elevation of total homocysteine levels in patients with Parkinson's disease treated with duodenal levodopa/carbidopa gel. J Neural Transm. 2011;118:1329–33. doi: 10.1007/s00702-011-0614-9. [DOI] [PubMed] [Google Scholar]
- 5.Jáuregui-Barrutia A, Tijero-Merino B, Gómez-Esteban JC, Zarranz JJ. Sleep disorders in Parkinson's disease: REM sleep behaviour disorder and restless legs syndrome. Rev Neurol. 2010;50:S15–9. [PubMed] [Google Scholar]
- 6.Covassin N, Neikrug AB, Liu L, Corey-Bloom J, Loredo JS, Palmer BW, et al. Clinical correlates of periodic limb movements in sleep in Parkinson's disease. J Neurol Sci. 2012;316:131–6. doi: 10.1016/j.jns.2012.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Iranzo de Riquer A, Bergareche A, Campos V. Sleep disorders in Parkinson disease. Neurologist. 2011;17:S38–42. doi: 10.1097/NRL.0b013e31823966f8. [DOI] [PubMed] [Google Scholar]
- 8.Kotagal V, Albin RL, Müller ML, Koeppe RA, Chervin RD, Frey KA, et al. Symptoms of rapid eye movement sleep behavior disorder are associated with cholinergic denervation in Parkinson disease. Ann Neurol. 2012;71:560–8. doi: 10.1002/ana.22691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao J, Huang X, Park Y, Hollenbeck A, Blair A, Schatzkin A, et al. Daytime napping, nighttime sleeping, and Parkinson disease. Am J Epidemiol. 2011;173:1032–8. doi: 10.1093/aje/kwq478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayer G, Jennum P, Riemann D, Dauvilliers Y. Insomnia in central neurologic diseases: Occurrence and management. Sleep Med Rev. 2011;15:369–78. doi: 10.1016/j.smrv.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 11.Margis R, Donis K, Schönwald SV, Fagondes SC, Monte T, Martín-Martínez P, et al. Psychometric properties of the Parkinson's disease sleep scale: Brazilian version. Parkinsonism Relat Disord. 2009;15:495–9. doi: 10.1016/j.parkreldis.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 12.Naismith SL, Hickie IB, Lewis SJ. The role of mild depression in sleep disturbance and quality of life in Parkinson's disease. J Neuropsychiatry Clin Neurosci. 2010;22:384–9. doi: 10.1176/jnp.2010.22.4.384. [DOI] [PubMed] [Google Scholar]
- 13.Norlinah MI, Afidah KN, Noradina AT, Shamsul AS, Hamidon BB, Sahathevan R, et al. Sleep disturbances in Malaysian patients with Parkinson's disease using polysomnography and PDSS. Parkinsonism Relat Disord. 2009;15:670–4. doi: 10.1016/j.parkreldis.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Suzuki K, Okuma Y, Hattori N, Kamei S, Yoshii F, Utsumi H, et al. Characteristics of sleep disturbances in Japanese patients with Parkinson's disease. A study using Parkinson's disease sleep scale. Mov Disord. 2007;22:1245–51. doi: 10.1002/mds.21257. [DOI] [PubMed] [Google Scholar]
- 15.Pacchetti C, Manni R, Zangaglia R, Glorioso M, Cristina S, Terzaghi M, et al. A questionnaire on sleep and mental disorders in Parkinson's disease (QSMDPD): Development and application of a new screening tool. Funct Neurol. 2004;19:83–99. [PubMed] [Google Scholar]
- 16.Högl B, Gschliesser V. RLS assessment and sleep questionnaires in practice: Lessons learned from Parkinson's disease. Sleep Med. 2007;8:S7–12. doi: 10.1016/j.sleep.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 17.Perez Lloret S, Rossi M, Cardinali DP, Merello M. Validation of the sleep related items of the Non-motor symptoms questionnaire for Parkinson's disease (NMSQuest) Parkinsonism Relat Disord. 2008;14:641–5. doi: 10.1016/j.parkreldis.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 18.Vibha D, Shukla G, Singh S, Goyal V, Srivastava AK, Behari M. Lower prevalence of sleep disturbances in familial versus sporadic Parkinson's disease: A questionnaire based study. J Neurol Sci. 2010;295:27–30. doi: 10.1016/j.jns.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 19.Huang TT, Hsu HY, Wang BH, Chen KH. Quality of life in Parkinson's disease patients: Validation of the short-form eight-item Parkinson's disease questionnaire (PDQ-8) in Taiwan. Qual Life Res. 2011;20:499–505. doi: 10.1007/s11136-010-9777-3. [DOI] [PubMed] [Google Scholar]
- 20.Nomura T, Inoue Y, Kagimura T, Uemura Y, Nakashima K. Utility of the REM sleep behavior disorder screening questionnaire (RBDSQ) in Parkinson's disease patients. Sleep Med. 2011;12:711–3. doi: 10.1016/j.sleep.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 21.Nogawa S, Takahashi H, Hattori N. The development and validation of a new comprehensive self-completing questionnaire for symptoms in Parkinson's disease (MASAC-PD 31) Rinsho Shinkeigaku. 2011;51:321–9. doi: 10.5692/clinicalneurol.51.321. [DOI] [PubMed] [Google Scholar]
- 22.Focke NK, Trenkwalder C. Idiopathic REM sleep behavior disorder and Parkinson's disease-Two sides of one coin? Sleep. 2010;33:731–2. doi: 10.1093/sleep/33.6.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martinez-Martin P, Visser M, Rodriguez-Blazquez C, Marinus J, Chaudhuri KR, van Hilten JJ, et al. SCOPA-sleep and PDSS: Two scales for assessment of sleep disorder in Parkinson's disease. Mov Disord. 2008;23:1681–8. doi: 10.1002/mds.22110. [DOI] [PubMed] [Google Scholar]
- 24.Martinez-Martin P, Rodriguez-Blazquez C, Abe K, Bhattacharyya KB, Bloem BR, Carod-Artal FJ, et al. International study on the psychometric attributes of the non-motor symptoms scale in Parkinson disease. Neurology. 2009;73:1584–91. doi: 10.1212/WNL.0b013e3181c0d416. [DOI] [PubMed] [Google Scholar]
- 25.Raggi A, Leonardi M, Carella F, Soliveri P, Albanese A, Romito LM. Impact of nonmotor symptoms on disability in patients with Parkinson's disease. Int J Rehabil Res. 2011;34:316–20. doi: 10.1097/MRR.0b013e32834d4b66. [DOI] [PubMed] [Google Scholar]
- 26.Stavitsky K, Cronin-Golomb A. Sleep quality in Parkinson disease: An examination of clinical variables. Cogn Behav Neurol. 2011;24:43–9. doi: 10.1097/WNN.0b013e31821a4a95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Trenkwalder C, Kohnen R, Högl B, Metta V, Sixel-Döring F, Frauscher B, et al. Parkinson's disease sleep scale: Validation of the revised version PDSS-2. Mov Disord. 2011;26:644–52. doi: 10.1002/mds.23476. [DOI] [PubMed] [Google Scholar]
- 28.Chaudhuri KR, Pal S, DiMarco A, Whately-Smith C, Bridgman K, Mathew R, et al. The Parkinson's disease sleep scale: A new instrument for assessing sleep and nocturnal disability in Parkinson's disease. J Neurol Neurosurg Psychiatry. 2002;73:629–35. doi: 10.1136/jnnp.73.6.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Najafi MR, Saadatnia M, Saffarifard A, Keyhanian K, Davoudi V. Epidemiology of restless legs syndrome in the Iranian population. Sleep Biol Rhythms. 2011;9:56–9. [Google Scholar]
- 30.Havlikova E, van Dijk JP, Nagyova I, Rosenberger J, Middel B, Dubayova T, et al. The impact of sleep and mood disorders on quality of life in Parkinson's disease patients. J Neurol. 2011;258:2222–9. doi: 10.1007/s00415-011-6098-6. [DOI] [PubMed] [Google Scholar]
- 31.Lima MM, Martins EF, Delattre AM, Proenca MB, Mori MA, Carabelli B, et al. Motor and non-motor features of Parkinson's disease-A review of clinical and experimental studies. CNS Neurol Disord Drug Targets. 2012;11:439–49. doi: 10.2174/187152712800792893. [DOI] [PubMed] [Google Scholar]
- 32.McSharry C. Parkinson disease: Skin patch improves sleep in PD. Nat Rev Neurol. 2011;7:64. doi: 10.1038/nrneurol.2010.208. [DOI] [PubMed] [Google Scholar]


