Abstract
Background:
To manage relapsing-remitting multiple sclerosis (MS) in the course of acute exacerbations, methylprednisolone (MP) (Medrol or Solu-Medrol), has the ability to lock the injured blood-brain barrier and decrease irritation in the central nervous system. The aim of this preliminary study was to investigate the frequency and time interval related to MP pulse therapy in patients with MS.
Methods:
This Study is conducted in the MS clinic of the Isfahan Kashani hospital, that was carried out on patients (n = 901) from June 2011 to December 2012. Patients who visited MS clinic just for once disinterested from analysis. According to the incidence of MP pulse therapy in females and males, two groups were made. Group 1 included patients with 2-3 times and Group 2 included patients with more than 4 times pulse therapy. Demographical data, pharmacological variables including number and time interval related to pulse therapy for each individual were recorded in dBase. The statistical analyses of d-Base were performed using SPSS.
Results:
901 patients in 1592 occasions were studied. The mean age of patients was 34.6 years old (ranged: 8-87 years old). 586 patients included 465 females and 121 males visited MS clinic just for once. 245 females in 797 occasions and 70 males in 209 occasions received pulse therapy with a mean of 4 times (ranged: 2-11 times). 51.1% and 48.9% of patients received MP pulse therapy for two and more than two up to 11 times respectively. In the 70% of the patients’ time interval between pulse therapy was with a mean of 137 days (ranged: 28-480 days).
Conclusions:
For pulse therapy, it seems that the female subjects refer to clinic are approximately 3.7 times higher than male subjects. To reduce the demand of patients to pulse therapy, disease management could be rationalized on the basis of illness expansion and its correlation to inter and intra individual variability. Finally, to understand the effectiveness of pharmacotherapy, in MS population (Isfahan/Iran), clinical neuropharmacology in relation to better understand of the individualized pharmacokinetics could be useful.
Keywords: Incidence, methylprednisolone, pulse, female
INTRODUCTION
The discrepancy judgment of multiple sclerosis (MS) is widespread and preserves to be demanding to detect originally in the non-existence of pathognomonic medical manifestation. In spite of subsistence of remedial strategy, management of MS relapse still remains heterogeneous.[1–15] Previous publication reported that hasty dealing with corticosteroids significantly recover patient signs. The remedial profit of adrenocorticotropic hormone in MS is typically attributed to its corticotropic events. Adrenocorticotropic hormone proceeds via corticosteroid-independent melanocortin tracks to provoke down-modulating events on immune- system cells and the cytokines they produce. In the dynamic stage of MS, steroid pulse therapy has been recognized as a cure for individuals.[16–23] Burton et al. in 2012 reported that oral steroid therapy might also be an effective alternative to intravenous steroids pulse therapy.[22]
Glucocorticoids characterize the adapted management for acute disease attacks in MS patients, for which methylprednisolone (MP) pulse therapy is the most frequently used protocol. MP (Medrol or Solu-Medrol), a synthetic glucocorticoid drug prescribed for non-penetrating spinal cord injuries characterize the regular management for severe disease attacks in MS. It has a wide range of effects, including changes to metabolism and immune responses. Due to activation and transformation of T-cells into blood brain barrier in inflammatory processes optic neuritis due to repugnance response to neuronal structures occurs.[21,24–26]
Shaygannejad et al. in 2013 reported that high-dose intravenous MP could be a safe treatment in MS attacks. The short-term adverse effects were described as slight and momentary.[27]
The aim of this preliminary study was to investigate the frequency and time interval related to MP pulse therapy in-patients who visited MS clinic of the Isfahan Kashani Hospital.
METHODS
A cross-sectional study of 901 patients (females; n = 710 and males; n = 191) in 1592 occasions was carried out between June 2011 and December 2012. All patients attended MS clinic located at the Kashani Hospital (conducted to Isfahan Neurosciences Research Center). Out of total patients studied in here, 586 integrated 465 females and 121 males pre- arranged MS clinic on one occasion. They removed from analysis. The extra 315 patients intended in 1006 circumstances. Demographical data, patient hospital record's code, the exact interlude (date-frequency-time) were noted in d-Base. According to the incidence of MP pulse therapy two groups were made. Cluster 1 integrated patient with two or three times and cluster two incorporated patients with more than four times pulse therapy respectively. There was no induction in treatment procedure. The statistical analyses of dBase were performed using Microsoft Excel and SPSS for windows.
RESULTS
The mean age of all patients was 34.6 years old (ranged; 8-87 years old). 901 patients in 1592 episode were studied. 465 females (51.6%) and 121 (13.4%) males attended MS clinic just for once. After their exclusion from total number, 315 patients were remained (35%), 245 females (77.7%), and 70 males (22.3%) were studied in 797 and 209 events respectively. The mean age of 315 patients was 33.1 years (ranged: 8-50 years old). The remaining patients (n = 315) were studied in 1006 stages. As it is shown in Figure 1, the highest rate of the demand for pulse therapy belongs to the age groups of 20-49 years old (87%), followed by the age groups of 50-59 years old (9.5%), 10-19 years old (2.2%), 60-69 years old, and one girl with the age of 8 years old.
Figure 1.
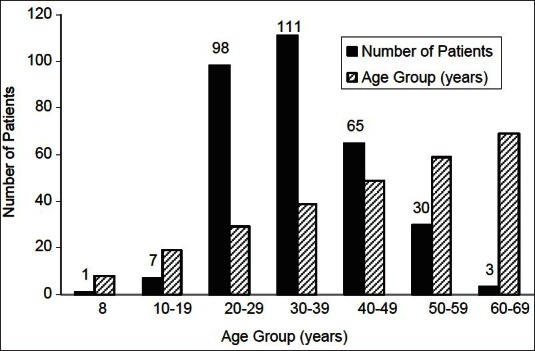
Distribution of different age groups in patients those received methylprednisolone pulse therapy for 2 or more times
The incidence of pulse therapy was with a mean of 4 times (ranged: 2-11 times). A total of 154 patients comprised, 125 females (81.2%) and 29 males (18.8%) received MP for 2 times [as shown in Figure 2]. 70, 74, and 16 patients received MP pulse therapy for 3, 4-6, and 7-10 times respectively. One patient received pulse therapy 11 times.
Figure 2.
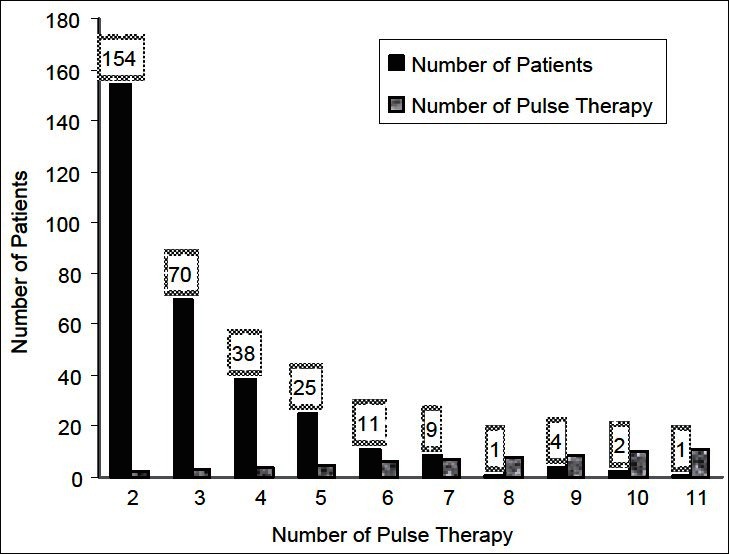
The number of methylprednisolone pulse therapy (n = 315)
Figure 3, shows the time intervals related to pulse therapy. As it is shown in three patient time intervals was 1 day. In eight and nine patients time intervals were 5-9, 10-19 days respectively. In the 70% of patients studied here, the time interval between pulse therapy was with a mean of 137 days (ranged: 28-480 days).
Figure 3.
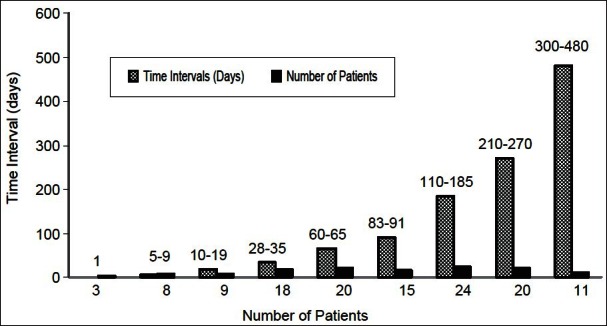
The time interval related to methylprednisolone pulse therapy (n = 128)
CONCLUSIONS
Data sustaining the effectiveness of different managements for MS is resulted mostly from potential medical examinations.[1–23,27–29]
Previous publications reported that high-dose intravenous MP is the most common therapeutic modality to care for sharp exacerbations in MS.[20–23,27,28] An alteration in sex ratio, disease course, and age at diagnosis has been reported by Celius and Smestad in 2009. They proposed that it is possible that an ecological factor mostly affect women.[14]
The results of this study is in agreement with previous publications that confirmed an increase in female/male ratio over time in many countries around the world,[1–15] but up to now, there are no reports, which confirm the higher incidence of MP pulse therapy in females. Analysis of data (obtained from MS clinic at the Isfahan/Kashani Hospital) in respect to the incidence of MP pulse therapy (from June 2011 to December 2012), showed a significant increase in proportion of females (77.7%) to males (22.3%). The incident of pulse therapy was ranged from 2 times to 11 times with a mean of 4 times. 49% and 51% of patients received MP for two (included 81.2% females versus males18.8%) and more than 2 times (3-11 times) respectively. The time interval between pulse therapy was with a mean of 137 days (ranged: 28-480 days). Published literature confirms that chronic administration of MP might be related to hyperglycemia, decreased resistance to infection, weight gain, glaucoma, osteoporosis, and psychosis, especially, when used at high dosage. The most serious side-effect occurs after the adrenal glands terminate ordinary construction of cortisol, which MP will restore.[20–23,27,28]
Wüst et al. in 2012 recommended that in the second phase a partial reduction of peripheral T cells by MP activates homeostatic propagation, which most likely consequences in an improved leading of auto reactive T cells and motives an aggravated disease course. They concluded that, the timing and assortment of glucocorticoids derivative necessitate vigilant contemplation in MS.[28]
Burton et al. in 2012 declared that intravenous MP necessitates frequent infusions that might interfered with patients’ daily duties.[22]
Many studies reported that in patients with optic neuritis the first line of treatment could be intravenous MP with quicker healing and fewer possibility of reappearance of optic neuritis and conversion to MS. However, oral therapy using prednisolone is contraindicated due to augmented risk of a second episode.[21,24–26]
Finally, due to enormous variability from one patient to another[1–37] in order to better management of patients with MS and to enhance our understanding of different drugs, studies of individualized pharmacokinetics attitude might be beneficial.
ACKNOWLEDGMENTS
This article was supported by Isfahan Neurosciences Research Center. We would like to gratefully acknowledge the Research Deputy of Isfahan University of Medical Sciences for its support to this research.
Footnotes
Source of Support: This article was supported by Isfahan Neurosciences Research Centre
Conflict of Interest: None declared.
REFERENCES
- 1.Compston A, Coles A. Multiple sclerosis. Lancet. 2008;372:1502–17. doi: 10.1016/S0140-6736(08)61620-7. [DOI] [PubMed] [Google Scholar]
- 2.Ashtari F, Shaygannejad V, Farajzadegan Z, Amin A. Does early-onset multiple sclerosis differ from adult-onset form in Iranian people. J Res Med Sci. 2010;15:94–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Shaygannejad V, Janghorbani M, Ashtari F, Zanjani HA, Zakizade N. Effects of rivastigmine on memory and cognition in multiple sclerosis. Can J Neurol Sci. 2008;35:476–81. doi: 10.1017/s0317167100009148. [DOI] [PubMed] [Google Scholar]
- 4.Ashtari F, Fatehi F, Shaygannejad V, Chitsaz A. Does amantadine have favourable effects on fatigue in Persian patients suffering from multiple sclerosis? Neurol Neurochir Pol. 2009;43:428–32. [PubMed] [Google Scholar]
- 5.Evans C, Beland SG, Kulaga S, Wolfson C, Kingwell E, Marriott J, et al. Incidence and Prevalence of Multiple Sclerosis in the Americas: A Systematic Review. Neuroepidemiology. 2013;40:195–210. doi: 10.1159/000342779. [DOI] [PubMed] [Google Scholar]
- 6.Tennant A. Epidemiology of neurologically disabling disorders. Handb Clin Neurol. 2013;110:77–92. doi: 10.1016/B978-0-444-52901-5.00007-1. [DOI] [PubMed] [Google Scholar]
- 7.Oreja-Guevara C, González-Segura D, Vila C. Spasticity in multiple sclerosis: results of a patient survey. Int J Neurosci. 2013 doi: 10.3109/00207454.2012.762364. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 8.Koch-Henriksen N, Stenager E, Laursen B. The use of epidemiological multiple sclerosis registers in research: The Danish MS Registry. Acta Neurol Scand Suppl. 2012;195:7–12. doi: 10.1111/ane.12022. [DOI] [PubMed] [Google Scholar]
- 9.Etemadifar M, Janghorbani M, Shaygannejad V, Ashtari F. Prevalence of multiple sclerosis in Isfahan, Iran. Neuroepidemiology. 2006;27:39–44. doi: 10.1159/000094235. [DOI] [PubMed] [Google Scholar]
- 10.Najim Al-Din AS, Kurdi A, Mubaidin A, El-Khateeb M, Khalil RW, Wriekat AL. Epidemiology of multiple sclerosis in Arabs in Jordan: A comparative study between Jordanians and Palestinians. J Neurol Sci. 1996;135:162–7. doi: 10.1016/0022-510x(95)00276-8. [DOI] [PubMed] [Google Scholar]
- 11.Al-Din AS, Khogali M, Poser CM, al-Nassar KE, Shakir R, Hussain J, et al. Epidemiology of multiple sclerosis in Arabs in Kuwait: A comparative study between Kuwaitis and Palestinians. J Neurol Sci. 1990;100:137–41. doi: 10.1016/0022-510x(90)90024-h. [DOI] [PubMed] [Google Scholar]
- 12.Kampman MT, Aarseth JH, Grytten N, Benjaminsen E, Celius EG, Dahl OP, et al. Sex ratio of multiple sclerosis in persons born from 1930 to 1979 and its relation to latitude in Norway. J Neurol. 2013 doi: 10.1007/s00415-012-6814-x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Trojano M, Lucchese G, Graziano G, Taylor BV, Simpson S, Jr, Lepore V, et al. Geographical variations in sex ratio trends over time in multiple sclerosis. PLoS One. 2012;7:e48078. doi: 10.1371/journal.pone.0048078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Celius EG, Smestad C. Change in sex ratio, disease course and age at diagnosis in Oslo MS patients through seven decades. Acta Neurol Scand Suppl. 2009;189:27–9. doi: 10.1111/j.1600-0404.2009.01208.x. [DOI] [PubMed] [Google Scholar]
- 15.Shaygannejad V, Sadr-Ameli M. Successful life with multiple sclerosis. Vajiran, Mashhad, Iran: 2010. [Google Scholar]
- 16.Ohji S, Nomura K. The indication of steroid pulse therapy and apheresis therapy for multiple sclerosis. Nihon Rinsho. 2008;66:1127–32. [PubMed] [Google Scholar]
- 17.Antoniol C, Jilek S, Schluep M, Mercier N, Canales M, Le Goff G, et al. Impairment of JCV-specific T-cell response by corticotherapy: Effect on PML-IRIS management? Neurology. 2012;79:2258–64. doi: 10.1212/WNL.0b013e3182768983. [DOI] [PubMed] [Google Scholar]
- 18.Annovazzi P, Tomassini V, Bodini B, Boffa L, Calabrese M, Cocco E, et al. A cross-sectional, multicentre study of the therapeutic management of multiple sclerosis relapses in Italy. CNS Neurol Disord Drug Targets. 2009;8:167–74. doi: 10.1007/s10072-012-0981-5. [DOI] [PubMed] [Google Scholar]
- 19.Kalincik T, Horakova D, Dolezal O, Krasensky J, Vaneckova M, Seidl Z, et al. Interferon, azathioprine and corticosteroids in multiple sclerosis: 6-year follow-up of the ASA cohort. Clin Neurol Neurosurg. 2012;114:940–6. doi: 10.1016/j.clineuro.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 20.Anlar O. Treatment of multiple sclerosis. CNS Neurol Disord Drug Targets. 2009;8:167–74. doi: 10.2174/187152709788680670. [DOI] [PubMed] [Google Scholar]
- 21.Shaygannejad V, Golabchi K, Dehghani A, Ashtari F, Haghighi S, Mirzendehdel M, et al. Color blindness among multiple sclerosis patients in Isfahan. J Res Med Sci. 2012;17:254–7. [PMC free article] [PubMed] [Google Scholar]
- 22.Burton JM, O’Connor PW, Hohol M, Beyene J. Oral versus intravenous steroids for treatment of relapses in multiple sclerosis. Cochrane Database Syst Rev. 2012;12:CD006921. doi: 10.1002/14651858.CD006921.pub3. [DOI] [PubMed] [Google Scholar]
- 23.Vasheghani-Farahani A, Sahraian MA, Darabi L, Aghsaie A, Minagar A. Incidence of various cardiac arrhythmias and conduction disturbances due to high dose intravenous methylprednisolone in patients with multiple sclerosis. J Neurol Sci. 2011;309:75–8. doi: 10.1016/j.jns.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 24.Hoorbakht H, Bagherkashi F. Optic neuritis, its differential diagnosis and management. Open Ophthalmol J. 2012;6:65–72. doi: 10.2174/1874364101206010065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fujihara K. Treatment of neuromyelitis optica. Nihon Rinsho Meneki Gakkai Kaishi. 2012;35:129–35. doi: 10.2177/jsci.35.129. [DOI] [PubMed] [Google Scholar]
- 26.Acar M, Gedizlioglu M, Koskderelioglu A, Ozturk F, Kilinc S, Talay N. Effect of high-dose intravenous methyl-prednisolone treatment on intraocular pressure in multiple sclerosis patients with relapse. Eur Neurol. 2012;68:20–2. doi: 10.1159/000337615. [DOI] [PubMed] [Google Scholar]
- 27.Shaygannejad V, Ashtari F, Alinaghian M, Norouzi R, Salari M, Fatehi F. Short-term safety of pulse steroid therapy in multiple sclerosis relapses. Clin Neuropharmacol. 2013;36:1–3. doi: 10.1097/WNF.0b013e3182764f91. [DOI] [PubMed] [Google Scholar]
- 28.Wüst S, van den Brandt J, Reichardt HM, Lühder F. Preventive treatment with methylprednisolone paradoxically exacerbates experimental autoimmune encephalomyelitis. Int J Endocrinol. 2012;2012:417017. doi: 10.1155/2012/417017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arnason BG, Berkovich R, Catania A, Lisak RP, Zaidi M. Mechanisms of action of adrenocorticotropic hormone and other melanocortins relevant to the clinical management of patients with multiple sclerosis. Mult Scler. 2013;19:130–6. doi: 10.1177/1352458512458844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tolou Ghamari Z. Antiepileptic Drugs (AEDs) Polypharmacy Could Lead to Buried Pharmacokinetic Interactions due to CYP450. Drug Metab Lett. 2012 doi: 10.2174/1872312811206030008. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 31.Tolou Ghamari Z. Nephro and neurotoxicity of calcineurin inhibitors: Mechanisms of rejection, A brief review on tacrolimus and cyclosporine in organ transplantation. J Nephropathol. 2012;1:23–30. doi: 10.5812/jnp.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tolou Ghamari Z, Palizban AA. Laboratory monitoring of cyclosporin pre-dose (C0) concentration after kidney transplantation in Isfahan/Iran. Iran J Med Sci. 2003;28:81–5. [Google Scholar]
- 33.Tolou Ghamari Z, Palizban AA, Gharavi M. Cyclosporin trough Concentration_Rejection relationship after kidney transplantation. Indian J Pharmacol. 2003;35:395–6. [Google Scholar]
- 34.Tolou-Ghamari Z, Palizban AA, Michael Tredger J. Clinical monitoring of tacrolimus after liver transplantation using pentamer formation assay and microparticle enzyme immunoassay. Drugs R D. 2004;5:17–22. doi: 10.2165/00126839-200405010-00003. [DOI] [PubMed] [Google Scholar]
- 35.Tolou-Ghamari Z, Palizban AA. Kidney transplant recipients and the incidence of adverse reactions to cyclosporin. Saudi Med J. 2004;25:1499–500. [PubMed] [Google Scholar]
- 36.Tolou Ghamari Z, Palizban AA, Wendon J, Tredger JM. Pharmacokinetics of tacrolimus on days one or two after liver transplantation. Transplant Med. 2004;16:112–6. [Google Scholar]
- 37.Tolou Ghamari Z, Palizban AA, Tredger JM. Modelling tacrolimus AUC in acute and chronic liver disease immediately after transplantation. Transplant Med. 2004;16:109–11. [Google Scholar]


