Abstract
Background:
In adults, throughout life, uniqueness maintains the equivalent; but, it might be tailored in the track of neurological disarrays. As in the partition of cognitive function associated with multiple sclerosis (MS), numerous studies have been performed, but there are very few reports in this area of behavior. The aim of this study was to investigate the prevalence of personality types A and B in relation to individuals’ behaviors with MS and type A behavior with demographic characteristics and the level of disability.
Methods:
A cross-sectional descriptive study was performed between September 2010 and March 2011 on 50 patients who were referred to MS clinic (located at the Kashani hospital), Isfahan Neurosciences Research Centre (INRC). The subjects were evaluated using Friedman and Rosenman questioner and the Expanded Disability Status Scale (EDSS). The data were analyzed by SPSS software (version 17) based on Chi-square test and independent T-test.
Results:
Of the subjects, 65% were of personality type A and 35% were of personality type B (X2: 3.5, P < 0.05). There were no significant differences in individuals with type A behavior in relation to gender and marital status. In connection to EDSS (EDSS < 4.5 or EDSS > 4.5), patients with higher EDSS score, i.e., individuals with EDSS > 4.5 mostly had type A behavior pattern.
Conclusions:
People with type A behavior pattern are reported to have more stress, nervousness, and anxiety. In this study, MS patients had more characteristics of type A than type B behavior. This behavior was increased in individuals with EDSS score > 4.5.
Keywords: Behavior, behavior patterns, Iranian, multiple sclerosis, type A
INTRODUCTION
Multiple sclerosis (MS) is the most persistent, widespread neurological turmoil that is categorized as localized disease that myelin sheath (lipid that surrounds nerve fibers) is spoiled and irritated. The covering provided by the myelin sheath, action potentials can travel more quickly along myelinated axons than along un-myelinated axons. The injured or destroyed myelin cause problems in nerve communication or generally blocks them. Side effects of this condition includes damage to eye nerves, paralytic spastic limbs, ataxia, tremor, difficulty in controlling sphincters, impotence, disability, aphasia, epilepsy and depression. MS initiation occurs generally between the age of 20 and 40 years, with a male:female ratio of 3:1 or 4:1. The disease in some patients has unpredictable chronic clinical course, i.e., sometimes with relapsing or progressive phase that could lead to disability. The prevalence of MS differs greatly around the nation. Due to inter- and intra-individual variability, the models of disease occurrence, its’ power, circumstances, and outcome are complicated and unpredictable. The prevalence is distinguished by major discrepancy, which is mediated by hereditary, environmental, and demographic factors.[1–9] In Isfahan/Iran, an increase in prevalence and incidence figures (73.3; 9.1:2004-2005 vs. 43.8; 3.64:2003-2010 per 100000) was reported. It has been mentioned that Isfahan could be considered as the area with the maximum incidence of MS in Asia and Oceania.[7,10] In adults, throughout existence, the personality remains the same; but it might be modified in the course of neurological disorders. Although many studies have been performed in the division of cognitive function related to MS, there are only diminutive records in the part of personality. In fact, MS patients are faced with a serious disorder that could affect their daily operation and life. Previous publication suggested that ambiguous interface between psychological and physical factors could lead patients toward unpredictable syndrome period. The most important of these factors is related to the type A behavior, for which only a small number of research exists. The pattern related to type A behavior can be determined as dictatorship, agitation, tolerate uncertainty, ambitious, high energy, competitive, anxious, rashness, precipitous, and aggression; this pattern was first described by cardiologists Friedman and Rosenman. Based on clinical observations, they reported that patients with heart disease expressed more stress, alertness, and aggression as compared to normal subjects.[11–20] To attain their objective and plans with the greatest development in lowest time, individuals with type A behavior form a constant and repeated odious and refuse to accept their condition. To achieve such a demand, it is essential for them to abandon against stuff and people. Researchers are always in a hurry to achieve results and are impatient within inter-personal relationship. Within diverse stages of work, they demonstrate anxiety and thrill. Their performance is a combination of right and left hemispheric power. They are rigid, devastated, undeniable, take risk, and are aggressive wherever assessed.[21,22] Type A behavior continuously suffer from being unable to manage situation and people; this might be the ground to a considerable pressure and accompany mental and physical illness.[23] Due to stimulation of sympatic nerve, the pressure on other vital organs could be increased. Mental and emotional health has an important collision on physical health. Previous publication reported that, in answer to pressure, there is a close correlation between the immune system and neurotransmitters. In fact, steady pressure can put a person in a regular condition of fight-or-flight response.[24] Additional stress is one of the majority widespread consequences that type A handle. There are reports and observation related to increased stress and anxiety in MS patients.[25] However, in the phase of pressure, it is relatively possible that symptoms do not come into view, but an attack and deterioration can be seen later. At this stage, the body's response to the production of stress hormones seems to return to the normal phase. Several studies have reported that, in MS patients, there is an increasing sign of delayed response to stress.[26] Previous publication reported that psychological features such as individuality style or reappearance of signs could affect MS patients.[27] Even though the type A behavior could be a significant aspect distressing the central nervous system, this peculiarity in MS patients has been rarely studied. Considering the psychological characteristics of MS patients, it is expected that type A behavior could be seen more in this population. Previous publication reported that there is a significant correlation between type A and type B behaviors in MS patients. They reported 63% and 37% of MS patients with type A and B behaviors, respectively.[28,29]
The aim of this study was to investigate type A behavior in MS patients in relation to variables of gender, age, and disability.
METHODS
A cross-sectional descriptive study on 50 patients who visited Multiple Sclerosis Clinic (Kashani Hospital, Isfahan Neurosciences Research Centre, INRC) was carried out between September 2010 and March 2011. Patients’ selection was based on their agreement to participate in this study. The patients having the following criteria were selected: (1) Diagnosed by a neurologist based on systemic examination and laboratory findings such as magnetic resonance imaging (MRI) and (2) no other neurological and psychiatric disorders. The tools used in this study to inspect the behavior of type A personality was based on Friedman and Rosenman questionnaire that has 25 questions. The answers to this questionnaire were required in yes or no format. The credit for majority of patients has been reported as 0.7-0.8. Patients who received a score of ≥13 or < 13 were considered as type A and type B, respectively.[27] Expanded Disability Status Scale (EDSS) is the most common measurement tool to evaluate the extent of disability, which is scored from 0 to 10 by a neurologist. At this scale, higher score indicates a higher degree of disability. EDSS for each individual patient in this study were extracted from patients’ files. Data collected in this study was analyzed based on Chi-square test and independent t-test using SPPSS software (version 17).
RESULTS
The age range of the patients was 20-45 years. Of the patients, 64% were of age < 35 years and 36% were of > 35 years. Sequentially, in respect to marital status, 67% was married and 33% were single. According to expanded disability status scale, 88% had EDSS < 4.5 and 12% had EDSS > 4.5. Table 1 shows the distribution of types A and B personality.
Table 1.
Distribution of types A and B personality in patients with multiple sclerosis
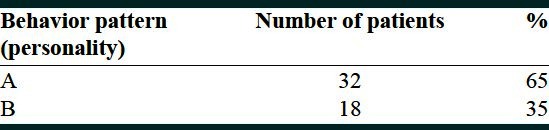
Of the total patients studied, 65% and 35% of patients were of type A and type B personality, respectively. Table 2 shows the mean scores of personality type A behavior pattern and its’ association with the EDSS score, marital status, and sex. The results of comparison related to different groups are given in this table.
Table 2.
A comparison of the mean scores for the pattern type A variables in patients with multiple sclerosis
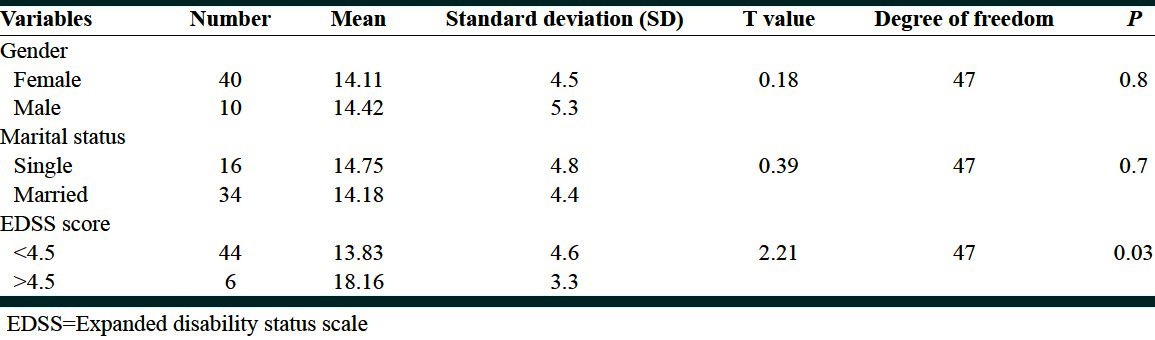
As shown in Table 2, there was no correlation between gender and marital status in MS patients with type A personality. However, according to EDSS score (EDSS < 4.5 or EDSS, P > 4.5) patients with type A behavior pattern showed significant differences.
DISCUSSION
The overall plan of this investigation was evaluation of type A behavior pattern in MS patients. Of total population studied, 65% were of personality type A and 35% were of type B behavior. With increasing EDSS score, patients showed more type A behavior pattern. The results of this study could be discussed from two directions: (1) MS is one of the most common disabling neurological disorders that affect a large number of people every year. It seems that the etiology of MS involves destruction of autoimmune and then an attack to central nervous system that could lead to appearances of neurological symptoms. In the past hundred year, studies have shown that stress could be one of the potential factors in the onset and progression of MS. Previous publication reported that stress could be one of the frustrating factors in MS.[30,31] Strong evidence shows that stress and other psychological factors could affect functions of immune system. Anxiety and chronic anxiety disorders is common in MS patients.[32] Additional stress and anxiety could be caused by patients’ concern for treatment fees, future of children, marriage, reduced job performance, low communication and social skills, disease obsession, and fright of deteriorating.[33] Also, part of it could be due to personality traits such as boasting a type A personality. People with type A behavior pattern reported more stress, nervousness, and anxiety. The surroundings of these manifestations could make symptoms worse. In another point of view, within patients with MS an increase in type A behavior with increasing severity of disability, could be considered as a coping response to the conditions created by stress. MS can affect many areas of performance that could be described as reducing physical performance and leading patients to incapability. Disease could also affect education and employment status, familial and sexual function, friends, and daily activities.[34] Developing disorder and increasing disability have a vast collapse on patients’ sense of life, community, and social functions.[35] In addition, feeling ambiguity due to lack of control on daily health and imprecise future increases.[36,37] When a person is faced with a situation wherein he has no control over himself, the person needs to increase the effort to maintain or obtain control. This circumstance shows itself as an increased motivation to progress, increased competition, and aggressive behaviors.
CONCLUSIONS
As the personality could be modified in the course of neurological disorders, the result of this preliminary study confirmed that in the 65% of the patients type A behavior (such as agitation, ambitious, anxious, rashness, aggression) have been observed. With escalating EDSS score of > 4.5, patients showed more type A behavior pattern. Therefore, people with MS who have an increased in their level of disability may consider a coping strategy with little control over conditions related to type A behavior pattern. The limitations of this study were the lack of a control group. Furthermore, patients who participated in this research in terms of disability were mild to moderate. Therefore, a comparison between personality types of patients (with neurological and psychiatric disorders) and healthy controls could be suggested in future studies. Also, differences in personality within MS subgroups and in patients with severe disability could be suggested. Moreover, whereas MS patients sometimes show little awareness, it is suggested that, in future studies, views of relatives and others related to patients’ condition before and after disease could be explored.
ACKNOWLEDGMENT
We would like to gratefully acknowledge Isfahan Neurosciences Research Centre (INRC) for its support throughout this research.
Footnotes
Source of Support: Isfahan Neurosciences Research Centre
Conflict of Interest: None declared.
REFERENCES
- 1.Etemadifar M, Abtahi SH. Multiple sclerosis in Isfahan, Iran: Past, Present and Future. Int J Prev Med. 2012;3:301–2. [PMC free article] [PubMed] [Google Scholar]
- 2.Najafi MR, Shaygannajad V, Mirpourian M, Gholamrezaei A. Vitamin B (12) Deficiency and Multiple Sclerosis; Is there Any Association? Int J Prev Med. 2012;3:286–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Evans C, Beland SG, Kulaga S, Wolfson C, Kingwell E, Marriott J, et al. Incidence and Prevalence of Multiple Sclerosis in the Americas: A Systematic Review. Neuroepidemiology. 2013;40:195–210. doi: 10.1159/000342779. [DOI] [PubMed] [Google Scholar]
- 4.Tennant A. Epidemiology of neurologically disabling disorders. Handb Clin Neurol. 2013;110:77–92. doi: 10.1016/B978-0-444-52901-5.00007-1. [DOI] [PubMed] [Google Scholar]
- 5.Oreja-Guevara C, González-Segura D, Vila C. Spasticity in multiple sclerosis: Results of a patient survey. Int J Neurosci. 2013 doi: 10.3109/00207454.2012.762364. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 6.Koch-Henriksen N, Stenager E, Laursen B. The use of epidemiological multiple sclerosis registers in research: The Danish MS Registry. Acta Neurol Scand Suppl. 2012;195:7–12. doi: 10.1111/ane.12022. [DOI] [PubMed] [Google Scholar]
- 7.Etemadifar M, Janghorbani M, Shaygannejad V, Ashtari F. Prevalence of multiple sclerosis in Isfahan, Iran. Neuroepidemiology. 2006;27:39–44. doi: 10.1159/000094235. [DOI] [PubMed] [Google Scholar]
- 8.Najim Al-Din AS, Kurdi A, Mubaidin A, El-Khateeb M, Khalil RW, Wriekat AL. Epidemiology of multiple sclerosis in Arabs in Jordan: A comparative study between Jordanians and Palestinians. J Neurol Sci. 1996;135:162–7. doi: 10.1016/0022-510x(95)00276-8. [DOI] [PubMed] [Google Scholar]
- 9.al-Din AS, Khogali M, Poser CM, al-Nassar KE, Shakir R, Hussain J, et al. Epidemiology of multiple sclerosis in Arabs in Kuwait: A comparative study between Kuwaitis and Palestinians. J Neurol Sci. 1990;100:137–41. doi: 10.1016/0022-510x(90)90024-h. [DOI] [PubMed] [Google Scholar]
- 10.Etemadifar M, Maghzi AH. Sharp increase in the incidence and prevalence of multiple sclerosis in Isfahan, Iran. Mult Scler. 2011;17:1022–7. doi: 10.1177/1352458511401460. [DOI] [PubMed] [Google Scholar]
- 11.Friedman M, Rosenman RH. Type A behavior and your heart. New York: Knopf; 1974. [Google Scholar]
- 12.Friedman M, Ulmer D. Treating type a behavior and your heart. New York: Knopf; 1984. [Google Scholar]
- 13.Anderson NB, Williams RB, Jr, Lane JD, Haney T, Simpson S, Houseworth SJ. Type A behavior, family history of hypertension, and cardiovascular responsivity among black women. Health Psychol. 1986;5:393–406. doi: 10.1037//0278-6133.5.4.393. [DOI] [PubMed] [Google Scholar]
- 14.Rosenman RH, Friedman M. Neurogenic factors in pathogenesis of coronary heart disease. Med Clin North Am. 1974;58:269–79. doi: 10.1016/s0025-7125(16)32158-7. [DOI] [PubMed] [Google Scholar]
- 15.Williams RB, Jr, Barefoot JC, Haney TL, Harrell FE, Jr, Blumenthal JA, Pryor DB, et al. Type A behavior and angiographically documented coronary atherosclerosis in a sample of 2289 patients. Psychosom Med. 1988;50:139–52. doi: 10.1097/00006842-198803000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Young LD, Barboriak JJ, Hoffman RG, Anderson AJ. Coronary-prone behavior attitudes in moderate to severe coronary artery occlusion. J Behav Med. 1984;7:205–15. doi: 10.1007/BF00845387. [DOI] [PubMed] [Google Scholar]
- 17.Myrtek M. Meta-analyses of prospective studies on coronary heart disease, type A personality, and hostility. Int J Cardiol. 2001;79:245–51. doi: 10.1016/s0167-5273(01)00441-7. [DOI] [PubMed] [Google Scholar]
- 18.Myrtek M. Type A behavior pattern, personality factors, disease, and physiological reactivity. A Meta-Analytic Update. 1995;18:491–502. [Google Scholar]
- 19.Ikeda A, Iso H, Kawachi I, Inoue M, Tsugane S JPHC Study Group. Type A behavior and risk of coronary heart disease: The JPHC Study. Int J Epidemiol. 2008;37:1395–405. doi: 10.1093/ije/dyn124. [DOI] [PubMed] [Google Scholar]
- 20.Gallacher JE, Sweetnam PM, Yarnell JW, Elwood PC, Stansfeld SA. Is type A behavior really a trigger for coronary heart disease events? Psychosom Med. 2003;65:339–46. doi: 10.1097/01.psy.0000041608.55974.a8. [DOI] [PubMed] [Google Scholar]
- 21.Miller TQ, Turner CW, Tindale RS, Posavac EJ, Dugoni BL. Reasons for the trend toward null findings in research on Type A behavior. Psychol Bull. 1991;110:469–8. doi: 10.1037/0033-2909.110.3.469. [DOI] [PubMed] [Google Scholar]
- 22.Shaw WS, Dimsdale JE, Patterson TL. Stress and life events measures. Washington DC: American Psychtric Association; 2000. pp. 221–39. [Google Scholar]
- 23.Furnham A, Drakeley R. Work locus of control and perceived organisational climate. Eur Work Organ Psychol. 1993;3:1–9. [Google Scholar]
- 24.Williams RB, Jr, Lane JD, Kuhn CM, Melosh W, White AD, Schanberg SM, et al. Type A behavior and elevated physiological and neuroendocrine responses to cognitive tasks. Science. 1982;218:483–5. doi: 10.1126/science.7123248. [DOI] [PubMed] [Google Scholar]
- 25.Byrne DG. Type A behavior, anxiety and neuroticism: Reconceptualizing the pathophysiological paths and boundaries of coronary-prone behaviour. Stress Med. 1996;12:238–77. [Google Scholar]
- 26.Shaygannejad V, Sadr-Ameli M. Successful life with multiple sclerosis. Iran: Vajiran, Mashhad; 2010. [Google Scholar]
- 27.Smith TW, MacKenzie J. Personality and risk of physical illness. Annu Rev Clin Psychol. 2006;2:435–67. doi: 10.1146/annurev.clinpsy.2.022305.095257. [DOI] [PubMed] [Google Scholar]
- 28.Mazaheri SH, Zarrabian MK, Samadi MJ. Assessment of personality type and locus of control in multiple sclerosis patients. Sci J Hamedan Univ. 2008;48:48–52. [Google Scholar]
- 29.Ganji H. Psychological tests. Iran: Tehran, S Alavan Publications; 2007. [Google Scholar]
- 30.Goodin DS, Ebers GC, Johnson KP, Rodriguez M, Sibley WA, Wolinsky JS. The relationship of MS to physical trauma and psychological stress: Report of the therapeutics and technology assessment subcommittee of the American academy of neurology. Neurology. 1999;52:1737–45. doi: 10.1212/wnl.52.9.1737. [DOI] [PubMed] [Google Scholar]
- 31.Ackerman KD, Stover A, Heyman R, Anderson BP, Houck PR, Frank E, et al. 2002 Robert Ader New Investigator award. Relationship of cardiovascular reactivity, stressful life events, and multiple sclerosis disease activity. Brain Behav Immun. 2003;17:141–51. doi: 10.1016/s0889-1591(03)00047-3. [DOI] [PubMed] [Google Scholar]
- 32.Bruce JM, Arnett P. Clinical correlates of generalized worry in multiple sclerosis. J Clin Exp Neuropsychol. 2009;31:698–705. doi: 10.1080/13803390802484789. [DOI] [PubMed] [Google Scholar]
- 33.Mohammadi RN, Afshar ZH. Determining psychological and social factors causing stress in patients with multiple sclerosis. 2009;40:305–10. [Google Scholar]
- 34.Thomas PW, Thomas S, Hillier C. Psychological Interventions for Multiple Sclerosis (review) Vol. 1. Hoboken: John Wiley and Sons, td. Publishers; 2007. The Cochrane Collaboration; pp. 1–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hakim EA, Bakheit AM, Bryantoe TN, Roberts MW, McIntosh-Michaelis SA, Spackman AJ, et al. The social impact of multiple sclerosis: A study of 305 patients and their relatives. Disabil Rehabil. 2000;22:288–93. doi: 10.1080/096382800296755. [DOI] [PubMed] [Google Scholar]
- 36.Mullins LL, Cote MP, Fuemmeler BF, Jean VM, Beatty WW, Paul RH. Illness intrusiveness, uncertainty and distress in individuals with multiple sclerosis. Rehabil Psychiatry. 2001;46:139–53. [Google Scholar]
- 37.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13:67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]


