Abstract
A client’s expectation that therapy will be beneficial has long been considered an important factor contributing to therapeutic outcomes, but recent empirical work examining this hypothesis has primarily yielded null findings. The present study examined the contribution of expectancies for treatment outcome to actual treatment outcome from the start of therapy through 12-month follow-up in a clinical sample of individuals (n=72) treated for fear of flying with either in vivo exposure or virtual reality exposure therapy. Using a piecewise hierarchical linear model, outcome expectancy predicted treatment gains made during therapy but not during follow-up. Compared to lower levels, higher expectations for treatment outcome yielded stronger rates of symptom reduction from the beginning to the end of treatment on 2 standardized self-report questionnaires on fear of flying. The analytic approach of the current study is one potential reason that findings contrast with prior literature. The advantages of using hierarchical linear modeling to assess interindividual differences in longitudinal data are discussed.
Individual benefit from psychotherapy is related to numerous factors, including specific components of the treatment (DeRubeis, Brotman, & Gibbons, 2005), as well as broader nonspecific factors (Glass, Arnkoff, & Shapiro, 2001). Outcome expectancy, defined as the extent clients believe they will benefit from therapy, has been identified as one of the most important nonspecific determinants of treatment gains (Arnkoff, Glass, Shapiro, & Norcross, 2002). Theorists have suggested that having confidence in oneself and having confidence in treatment are critical factors underlying positive change (Bandura, 1986). Reviews of the literature indicate that high levels of outcome expectancy are associated with better overall treatment outcome, a stronger therapeutic alliance, improved compliance with treatment exercises, and lower attrition (Connolly Gibbons, Crits-Christoph, de la Cruz, Barber, Siqueland, & Gladis, 2003; Dew & Bickman, 2005; Shuman & Shapiro, 2002). However, much of the research on outcome expectancy was conducted over 20 years ago (for a review, see Greenberg, Constantino, & Bruce, 2006), and therapies and therapeutic techniques have changed greatly since then (Lambert, Archer, Good-heart, Kazdin, & Sternberg, 2006). As a result, the impact of outcome expectancy on treatment may have also changed. Results from recent studies on the impact of outcome expectancy on the treatment of anxiety disorders are mixed, with three studies yielding null findings (Borkovec, Newman, Pincus, & Lytle, 2002; Chambless, Tran, & Glass, 1997; Vogel, Hansen, Stiles, & Gotestam, 2006) and two studies showing a positive relation (Dozois & Westra, 2005; Safren, Heimberg, & Juster, 1997).
Chambless et al. (1997) did not find a significant relation between expectancy and posttreatment outcome in a clinical sample of individuals with social phobia undergoing 12 sessions of cognitive behavioral group therapy (CBGT), although at 6-month follow-up, clients with higher expectancies reported a greater reduction on one of the five primary outcome measures. Another study examined individuals treated for generalized anxiety disorder with 14 sessions of cognitive behavioral therapy (CBT). Results showed no correlation between expectancy and treatment outcome at posttreatment, 6-, 12-, and 24-month follow-up (Borkovec et al., 2002). Finally, results from a study of individuals treated for obsessive-compulsive disorder using exposure and response prevention (Vogel et al., 2006) suggested that the relation between expectancy and treatment outcome approached significance at the conclusion of treatment but was no longer evident at 12-month follow-up.
Two recent studies supported a positive relation between outcome expectancy and treatment gains (Dozois & Westra, 2005; Safren et al., 1997). Safren et al. found a positive relation between outcome expectancy and treatment outcome on six of eight posttreatment self-report measures after 12 sessions of CBGT for social phobia (Safren et al., 1997). Similarly, Dozois and Westra (2005) showed a positive relation between outcome expectancy and improvement over the course of eight sessions of CBT in a sample of participants with generalized anxiety disorder. In summary, although early literature supported a relationship between outcome expectancy and treatment outcome, results from recent studies using CBT treatments for anxiety disorders have been mixed.
One of the difficulties in assessing the relationship between outcome expectancy and treatment outcome is handling the longitudinal, or nested, component of the data (Singer & Willett, 2003). Nested data occur when multiple measurements share a common source that results in shared variance across waves. In treatment outcome studies, it is expected that responses from any given individual will be related across time points because the data share a common source of variance: the person providing the information. The majority of the prior studies addressed the nested component with a regression approach in which pre-treatment scores were used as a covariate (Chambless et al., 1997; Dozois & Westra, 2005; Safren et al., 1997; Singer & Willett, 2003; Vogel et al., 2006). However, nested data violate the assumption of independence for regression. An alternative analytic method that does not require this assumption would be better suited to address the impact of outcome expectancy on treatment gains.
The only study that did not use a regression approach was Borkovec et al. (2002). This study defined treatment outcome as the number of measures on which a person demonstrated a 25% decrease. This was then correlated with outcome expectancy. Although this approach does not have the problem of independent observations, the cutoff criterion limits the variability of improvement during treatment. This may have contributed to the weak correlation. For example, a participant whose anxiety score improved by 50% may have provided a higher rating of outcome expectancy than a participant whose anxiety score improved by 25%, which would have been obscured by the use of cutoff scores.
An alternative method of analysis is hierarchical linear modeling (HLM) or multilevel modeling (Raudenbush & Bryk, 2002). HLM is a relatively underutilized technique in the clinical literature that has several advantages for working with nested data. HLM models change over time on two levels, a Level 1 component representing individual change over time and a Level 2 component representing the extent that change differs across individuals. Each component is further divided into fixed and random effects. Fixed effects are an estimate of the variation attributed to a specified variable such as time or outcome expectancy. Random effects are estimates of individual variation. Through estimating a random effect for within-person (Level 1) variation, the estimates of the between-person fixed and random effects are adjusted for the violation of measurement independence. HLM also provides more accurate estimates of standard errors, which is another benefit when working with nested data (Singer & Willett, 2003). The present study used HLM to examine the influence of expectancy on self-reported treatment outcome in individuals who underwent CBT for fear of flying (FOF). Those participants who reported greater outcome expectancy were hypothesized to show stronger treatment gains over the course of therapy and follow-up relative to participants who reported lower outcome expectancy.
Method
PARTICIPANTS
Participants were 72 individuals volunteering in a treatment outcome study comparing the effects of virtual reality exposure (VRE) to in vivo exposure therapy for flying phobia (Rothbaum, Anderson, Zimand, Hodges, Lang, & Wilson, 2006). Participants were diagnosed with one of the following: specific phobia, situational type (n=63), panic disorder with agoraphobia with a primary fear of flying (n=8), or agoraphobia without panic (n=1), according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR; American Psychiatric Association, 2000). The majority of the participants met criteria for only one diagnosis (52%; n=38). All diagnoses were made using the Structured Clinical Interview for DSM-IV-TR (SCID; First, Gibbon, Spitzer, & Williams, 2002), administered by a licensed psychologist. A second licensed psychologist rated 50% of the pretreatment diagnostic interviews. Ratings showed excellent interrater reliability, with a kappa coefficient of .94. Participants primarily self-identified as female (90%; n=65), married (60%, n=43), with an average of 16.20 (SD=2.44) years of education and a mean age of 40.34 years (SD=10.78). Participants self-identified as Caucasian (88%; n=64), African American (5.6%, n=4), Latino (4%, n=3), and Asian (1%, n=1).
MEASURES
Questionnaire on Attitudes Toward Flying (QAF; Howard, Murphy, & Clarke, 1983)
The QAF is a 36-item measure that assesses FOF by asking participants to rate fears towards specific aspects of flying (e.g., “How much fear do you experience while you feel the plane lift off from the ground?”) on an 11-point scale ranging from 0 (no fear) to 10 (extreme fear). Higher scores indicate greater fear. The QAF has shown excellent test-retest (.92) and split half reliability (.99) in prior work with clinical samples. Also, the measure has been shown to be sensitive to change as a result of treatment (Anderson, Jacobs, Lindner, Edwards, Zimand, Hodges, et al., 2006; Rothbaum et al., 2006). The measure demonstrated good internal consistency within the current sample: pretreatment, Cronbach’s α=.97; midtreatment Cronbach’s α=.97; posttreatment Cronbach’s α=.97; 6-month follow-up Cronbach’s α=.99; and 12-month follow-up Cronbach’s α=.97.
Fear of Flying Inventory (FFI; Scott, 1987)
The FFI is a 33-item measure assessing distress towards different aspects of flying (e.g., “How troubled or distressed would you feel looking out the window during takeoff if you were to fly today?”) on a 9-point scale ranging from 0 (not at all) to 8 (very severely), with higher scores indicating greater distress. This measure appears to be sensitive to change as a result of treatment (Anderson et al., 2006; Rothbaum et al., 2006). For the current study, the measure had excellent internal consistency at all time points: pretreatment Cronbach’s α=.95; midtreatment Cronbach’s α=.97; posttreatment Cronbach’s α=.97; 6-month follow-up Cronbach’s α=.98; and 12-month follow-up Cronbach’s α=.97.
Outcome expectancy
Outcome expectancy was assessed with a three-item questionnaire adapted from a measure developed by Borkovec and Nau (1972). Clients were asked to rate “Confidence that therapy would reduce fear of flying related symptoms,” “Confidence that therapy would reduce other fears,” and “How logical the treatment seemed” on a 9-point (1–9) scale, with higher scores indicating greater expectancy. The measure was administered at the end of the first therapy session in order to allow clients an opportunity to meet with their therapist and hear the rationale for treatment. The internal consistency of these responses was less than satisfactory (Cronbach’s α=.49). As a result, the single item that was thought to best estimate the construct of outcome expectancy was used. This item was “Confidence that therapy would reduce fear of flying related symptoms.” Similar methods have been used in prior work (Vogel et al., 2006).
PROCEDURE
Participants attended a pretreatment assessment, which included a diagnostic interview and the administration of the QAF and FFI. Participants received individualized VRE therapy or in vivo exposure therapy according to random assignment. Treatment consisted of 8 sessions over the course of 6 weeks, administered according to a treatment manual (Rothbaum, Hodges, & Smith, 1999). The first four sessions were weekly 45-minute sessions of anxiety management skills training and cognitive therapy for both treatment conditions. The final four sessions were twice weekly exposure sessions, in which the in vivo exposure group conducted exposure in an actual plane at the airport and the VRE group was exposed to a virtual plane. The QAF and FFI were completed at pretreatment, midtreatment (after the fourth session), posttreatment, 6 months after treatment, and 12 months after treatment. A more detailed description of the clinical trial can be found in Rothbaum et al. (2006).
STATISTICAL ANALYSIS
A piecewise hierarchical model was used to evaluate the association between expectancy and treatment outcome. A piecewise approach models different rates of change for distinct time periods (Raudenbush & Bryk, 2002). For the current study, two distinct periods were identified: treatment and follow-up. The model was developed using the steps recommended by Singer and Willett (2003). First, an unconditional mean model containing a single fixed effect (π0i) and random effect ( ) at Level 1 and Level 2 (β00i ) was tested Eq. (1).
| (1) |
The significance of the random effects was of interest in this model as this indicates that there is sufficient variation in the dependent variable to warrant the inclusion of other explanatory variables in the model (Singer & Willett, 2003). The random effect of the Level 1 model determines whether there is a significant amount of within-person variation in the dependent variable. The random effect from the Level 2 model determines whether there is a significant amount of between-person variation in the dependent variable.
Next, an unconditional change model incorporating a measurement of time into the Level 1 model was tested. The Level 1 model contained three fixed effects: one representing pretreatment anxiety (π0i), the second representing the rate of change during therapy (π1i), and the third representing the rate of change during follow up (π2i) Eq. (2). Additional coefficients were used to create the distinct time periods, with a1t representing time during therapy and a2t representing time during follow-up (Table 1). For more information on piecewise coding schemes, refer to Raudenbush and Bryk (2002).
Table 1.
Coding scheme for the piecewise linear model
| Piece | Pretreatment | Midtreatment | Posttreatment | 6-month Follow-up | 12-month Follow-up |
|---|---|---|---|---|---|
| Treatment | 0 | 1 | 1.5 | 1.5 | 1.5 |
| Follow-up | 0 | 0 | 0 | 6 | 12 |
Note. Time is scaled in 1-month intervals.
| (2) |
The Level 2 model of the unconditional change model included only a single fixed and random effect for each coefficient Eq. (2). The Level 2 random effects ( ) indicate whether there is a significant amount of between-person variation within the respective coefficients. For example, a significant random effect for suggests that the rate at which people improved during the treatment varied across participants. This variation can then be predicted using between-person variables (i.e., outcome expectancy).
The final step added outcome expectancy for each time period (treatment and follow-up) in the Level 2 model Eq. (3). Through this multilevel approach, intra-individual variation over time can be assessed through the Level 1 model and interindividual variation on outcome expectancy can be simultaneously assessed through the Level 2 model.
| (3) |
Results
Retention rates for 6-and 12-month follow-up were 88% (n=64) and 76% (n=55), respectively. Missing follow-up data were considered missing at random, as participants who provided 6-and 12-month data did not significantly differ on age, ethnicity, expectancy and posttreatment QAF and FFI scores from those with missing data. Scores for the QAF and FFI indicate the mean item response, such that the possible range of scores on the QAF was 0 to 10, and the possible range of scores on the FFI was 0–8. The range of expectancy scores was 1 to 9. Table 2 shows that scores on the FOF measures decreased during treatment. All of the following analyses were conducted with the QAF and FFI, with identical results being obtained for both measures.
Table 2.
Descriptive statistics
| Mean | SD | |
|---|---|---|
| Expectancy | 6.97 | 1.58 |
| QAF Pretreatment | 5.88 | 1.65 |
| QAF Midtreatment | 4.81 | 1.69 |
| QAF Posttreatment | 4.06 | 1.73 |
| QAF 6-Month Follow-Up | 3.39 | 2.14 |
| QAF 12-Month Follow-Up | 3.49 | 1.99 |
| FFI Pretreatment | 3.50 | 1.39 |
| FFI Midtreatment | 3.52 | 1.49 |
| FFI Posttreatment | 3.03 | 1.32 |
| FFI 6-Month Follow-Up | 2.28 | 1.55 |
| FFI 12-Month Follow-Up | 2.38 | 1.50 |
Note. QAF=Questionnaire on Attitudes Towards Flying. FFI= Fear of Flying Inventory. N=72.
First, expectancy scores for participants randomly assigned to in vivo exposure therapy (n=36) or VRE (n=36) were compared to assess the potential confound of heterogeneous treatments. There were no significant differences in mean expectancy scores (Min vivo =7.14, SDin vivo =1.53; MVRE =6.84, SDVRE = 1.66) between the two groups, F(1, 71)=0.66, p=.42. Thus, data from both treatments were collapsed in all subsequent analyses. Also, there was no evidence that expectancy scores for participants varied as a function of diagnosis, F(2, 68)=0.88, p=.42.
A piecewise linear change model that assessed change during therapy (Piece 1) and change during follow-up (Piece 2) was fitted to the data using full maximum likelihood estimation (FML) (Singer & Willett, 2003).1 The Level 1 model that best approximated the data included both fixed and random effects for change during Piece 1 and Piece 2 (Table 3). The significant fixed effects indicate that anxiety ratings changed significantly during the course of therapy and during follow-up. Furthermore, the slopes for each piece suggest that anxiety declined at a greater rate during the course of therapy (QAF: β10i =−1.25; FFI: β10i =−0.34) than during follow-up (QAF: β20i =−0.05; FFI: β20i =−0.6). The significant random effects indicate that there was a significant amount of interindividual variation in the rate of change for both Piece 1 and Piece 2. This indicates that additional variables may be added to the Level 2 model (Singer & Willett, 2003).
Table 3.
Coefficients for models of anxiety change from pretreatment through 12-month follow-up
| Parameter | QAF
|
FFI
|
|||
|---|---|---|---|---|---|
| Unconditional Change Model | Fixed Effects (Expectancy) Model | Unconditional Change Model | Fixed Effects (Expectancy) Model | ||
| Level 1 | |||||
| Intercept | β00i | 5.95** (0.20) | 5.95** (0.20) | 3.25** (0.13) | 3.25** (0.13) |
| Piece 1 (Treatment) | β10i | −1.25** (1.3) | −1.25** (1.3) | −0.34** (0.12) | −0.34** (0.11) |
| Piece 2 (Follow-Up) | β20i | −0.05** (0.02) | −0.05** (0.02) | −0.06** (0.02) | −0.06** (0.02) |
| Level 2 | |||||
| Expectancy | β11i | – | −0.21** (0.05) | – | −0.14* (0.07) |
| Goodness of Fit | |||||
| Deviance | – | 1193.98 | 1183.29 | 1093.73 | 1089.81 |
| Deviance Δ | – | – | 10.69** | – | 3.93* |
Note. QAF=Questionnaire on Attitudes Towards Flying. FFI=Fear of Flying Inventory. N=72. Values represent betas and (standard errors).
p<.05.
p<.01.
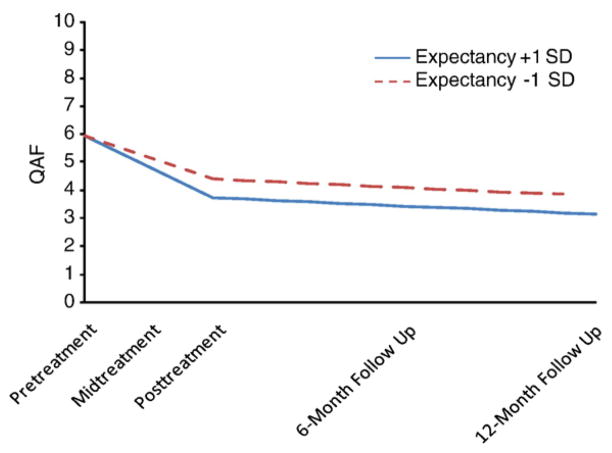
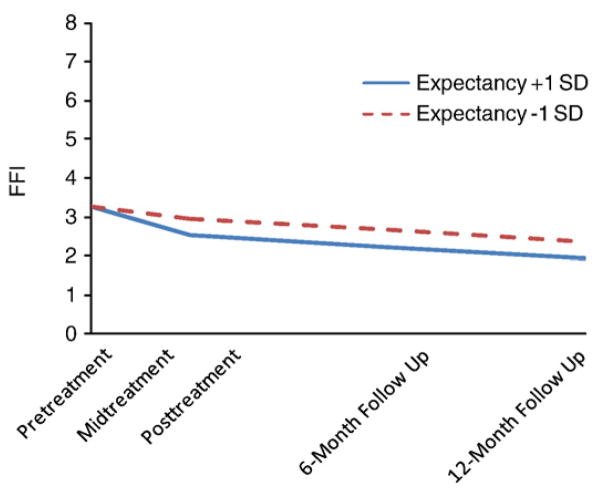
Expectancy was a significant predictor of change during treatment (QAF: Piece 1; β11i =−0.21, p < .01; FFI: Piece 1; β11i =−0.14, p < .05), but not during follow-up (QAF: Piece 2; β21i =−0.00, p =.92; FFI: Piece 2; β21i =−0.01, p =.36). Based on these results, the model was respecified using outcome expectancy as a predictor of Piece 1, but not Piece 2 (Table 3). This model fit equally well and was adopted on grounds of parsimony, QAF: χ2 Deviance Δ (1)=0.01, p=.94; FFI: χ2 Deviance Δ (1)=0.83, p=.39. A pseudo-R2 was calculated to determine the effect size of outcome expectancy on the rate of change during treatment. The pseudo-R2 is calculated in a similar manner to that of the R2 used in regression and has a similar interpretation (Singer & Willett, 2003). The pseudo-R2 for outcome expectancy was .28 for the QAF and .23 for the FFI, indicating that outcome expectancy explains 28% and 23% of the interindividual variation in treatment change during therapy in the QAF and FFI, respectively. Those with higher outcome expectancy showed a greater decline in anxiety during the course of therapy than those with lower outcome expectancy (see Figs. 1 and 2). Outcome expectancy was unrelated to the rate of change during follow-up.
FIGURE 1.
Change trajectories for treatment outcome as measured by the Questionnaire on Attitudes Towards Flying (QAF).
FIGURE 2.
Change trajectories for treatment outcome as measured by the Fear of Flying Inventory (FFI).
To further evaluate the unique contribution of outcome expectancy to treatment outcome, several possible confounding variables were added to the Level 2 model. These variables included treatment type (VRE or in vivo exposure), ethnicity, and length of time participants had feared flying. These additions did not significantly improve model fit for the QAF, χ2 Deviance Δ (2)=0.79, p=ns, or FFI, χ2 Deviance Δ (2)=1.9, p=ns, and outcome expectancy remained a significant predictor of change during therapy (QAF: Piece 1; β11i =−0.20, p < .01; FFI: Piece 1; β11i =−0.12, p<.05).
Discussion
The primary finding of the current study suggests that higher outcome expectancy at the start of therapy is related to a greater rate of improvement during treatment. These results suggest that clinicians can potentially impact the rate at which a client will improve by facilitating positive outcome expectancy at the start of therapy. Future research should examine how outcome expectancies may be maximized; possible methods of improving outcome expectancy may include providing a strong rationale for treatment, addressing a client’s concerns about therapy, and setting appropriate goals (Holt & Heimberg, 1990). Unexpectedly, outcome expectancy was not related to symptom change during the follow-up period. Follow-up may be better conceptualized as a maintenance period. As such, expectations for treatment gains may be unrelated to changes in anxiety after the conclusion of the therapy. Variability during maintenance may be related to other factors and future work should attempt to discover these variables. One possibility is the frequency with which individuals continue to use the skills learned in treatment (Anderson et al., 2006).
The positive results of the current study are consistent with the findings of some recent studies (Dozois & Westra, 2005; Safren et al., 1997) and contrast the null findings of others (Borkovec et al., 2002; Chambless et al., 1997; Vogel et al., 2006), the majority of which used a regression approach (Chambless et al., 1997; Dozois & Westra, 2005; Safren et al., 1997; Vogel et al., 2006). The discrepancy of findings across the studies may be attributed to numerous factors, such as differences in therapy, measurement, diagnosis of the sample or, as highlighted in this study, the analytic approach. When assessing treatment gains, HLM has many technical advantages over a regression approach, including modeling interindividual and intraindividual variation, modeling distinct periods of change, and the lack of reliance on the assumption of independent observations. Furthermore, HLM is able to incorporate information from all measurement points to estimate slopes for change during treatment. Finally, HLM uses a better mechanism for missing data than listwise deletion, which traditionally is used in regression. All of these advantages may have improved the precision of the current study in assessing the relation between outcome expectancy and change during treatment.
HLM also has numerous conceptual advantages when used to assess longitudinal benefit from therapy. Conceptually, improvement over the course of therapy is a process of gradual improvement rather than a series of discrete changes. This is especially true for exposure therapies in which treatment gain is conceptualized as a gradual extinction of reactions towards a feared stimulus (Foa & Kozak, 1986). The change trajectory provided by HLM is more congruent with this gradual process. This trajectory also allows the follow-up period to be characterized as the entire duration that a client remains out of therapy, rather than a fixed amount of time after therapy has ended. Finally, HLM provides the flexibility to model the shape of change during therapy. Although the current study was limited to assess a linear change model, increasing the number of assessment points would allow researchers to examine higher-order polynomial trends.
The current study has several clinical implications. HLM offers the possibility of comparing an individual’s rate of change during therapy to a published rate of change of the same treatment. Receiving feedback about the rate of change relative to others may assist sufferers and clinicians in treatment planning. Knowing that one is progressing at a similar or better rate than others using the same treatment for a similar problem may be reinforcing. Alternatively, if a client is changing at a slower rate, it may present an opportunity to reassess the treatment plan. However, such a comparison is currently theoretical as much additional work must be done before this could be implemented appropriately. The finding should be replicated and the HLM analysis should contain multiple intra-session measurement points before making such a comparison. Lastly, HLM has the potential to determine which treatments are more effective for members of a particular gender, age, or ethnic group. The American Psychological Association multicultural guidelines (American Psychological Association, 2003) recommend that the cultural appropriateness of an intervention be evaluated to provide the best available care. HLM is a means by which the efficacy of intervention can be evaluated across various groups.
The current study had several limitations. In this study, a single item measured the construct of outcome expectancy. Future work on expectancy should use multi-item measures, such as the Treatment Expectancy Scale (Borkovec & Nau, 1972) and the Anxiety Change Expectancy Scale (Dozois & Westra, 2005). Additionally, the current study relied solely on self-report measures of anxiety, which are prone to bias. The FOF measures also do not have well-validated cutoff scores to distinguish between clinical populations and controls, which makes it difficult to assess the clinical relevance. Another weakness is the heterogeneity of diagnosis within the sample (mainly specific phobia, with a minority of participants with panic and agoraphobia). Finally, it is likely that other variables besides expectancy contribute to change over the course of therapy. For example, a recent study suggested that homework compliance mediated the relation between outcome expectancy and treatment outcome for individuals with generalized anxiety disorder and panic disorder (Westra, Dozois, & Marcus, 2007). Also, treatment credibility, a construct that is closely related to outcome expectancy, has been found to be a predictor of treatment outcome (Borkovec et al., 2002). Future research should evaluate these and other variables that may be related to change during treatment, such as motivation for participation, the working alliance, and treatment credibility and confidence (Greenberg et al., 2006).
The current study provides support for the relation between outcome expectancy and treatment change. The contribution of expectancy to treatment outcome presents a potentially useful tool for clinicians and presents new questions for researchers. Treatment outcome researchers should weigh the technical and conceptual advantages of HLM and other more commonly used analytic methods in deciding which analytic approach to use to address questions about predictors of treatment change.
Acknowledgments
This work was funded by a grant from the NIMH, R41MH58493-01, awarded to the second author.
Footnotes
Full maximum likelihood estimation has been shown to provide biased estimates of random effects with smaller samples (Singer & Willett, 2003). To determine the stability of the random effects, the model was also fitted using restricted maximum likelihood estimation (RML). RML has been shown to provide more accurate estimates of random effects, but it is unable to compare the fit of models with different fixed effects (Singer & Willett, 2003). The random effects estimated from RML were nearly identical to those obtained from FML for all of the models and so only the results of the FML are presented (Table 3). For more information on the use of FML and RML, refer to Singer and Willett (2003) and Raudenbush and Bryk (2002).
Disclosure statement: Dr. Rothbaum receives research funding and is entitled to sales royalty from Virtually Better, Inc., which is developing products alluded to in the research described in this article. In addition, she serves as a consultant to and owns equity in Virtually Better, Inc. The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict of interest policies.
Contributor Information
Matthew Price, Georgia State University.
Page Anderson, Georgia State University.
Christopher C. Henrich, Georgia State University
Barbara Olasov Rothbaum, Emory University School of Medicine.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author text revision; 2000. [Google Scholar]
- American Psychological Association. Guidelines on multi-cultural education, training, research, practice, and organizational change for psychologists. American Psychologist. 2003;58:377–402. doi: 10.1037/0003-066x.58.5.377. [DOI] [PubMed] [Google Scholar]
- Anderson P, Jacobs CH, Lindner GK, Edwards S, Zimand E, Hodges L, et al. Cognitive behavior therapy for fear of flying: Sustainability of treatment gains after September 11. Behavior Therapy. 2006;37:91–97. doi: 10.1016/j.beth.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Arnkoff DB, Glass CR, Shapiro SJ, Norcross JC. Expectations and preferences. In: Norcross J, editor. Psychotherapy relationships that work: Therapist contributions and responsiveness to patients. Oxford University Press; 2002. pp. 335–356. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Upper Saddle River, NJ: Prentice-Hall; 1986. [Google Scholar]
- Borkovec TD, Nau SD. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychaitry. 1972;3:257–260. [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. [PubMed] [Google Scholar]
- Chambless DL, Tran GQ, Glass CR. Predictors of response to cognitive-behavioral group therapy for social phobia. Journal of Anxiety Disorders. 1997;11:221–240. doi: 10.1016/s0887-6185(97)00008-x. [DOI] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Crits-Christoph P, de la Cruz C, Barber JP, Siqueland L, Gladis M. Pretreatment expectations, interpersonal functioning, and symptoms in the prediction of the therapeutic alliance across supportive-expressive psychotherapy and cognitive therapy. Psychotherapy Research. 2003;13:59–76. doi: 10.1093/ptr/kpg007. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Brotman MA, Gibbons CJ. A conceptual and methodological analysis of the nonspecifics argument. Clinical Psychology: Science and Practice. 2005;12:174–183. [Google Scholar]
- Dew SE, Bickman L. Client expectancies about therapy. Mental Health Services Research. 2005;7:21–33. doi: 10.1007/s11020-005-1963-5. [DOI] [PubMed] [Google Scholar]
- Dozois DJA, Westra HA. Development of the Anxiety Change Expectancy Scale (ACES) and validation in college, community, and clinical samples. Behaviour Research and Therapy. 2005;43:1655–1672. doi: 10.1016/j.brat.2004.12.001. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for the DSM-IV-TR. New York: Biometrics Research Department; 2002. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Glass CR, Arnkoff DB, Shapiro SJ. Expectations and preferences. Psychotherapy: Theory, Research, Practice, Training. 2001;38:455–461. [Google Scholar]
- Greenberg RP, Constantino MJ, Bruce N. Are patient expectations still relevant for psychotherapy process and outcome? Clinical Psychology Review. 2006;26:657–678. doi: 10.1016/j.cpr.2005.03.002. [DOI] [PubMed] [Google Scholar]
- Holt CS, Heimberg RG. The Reaction to Treatment Questionnaire: Measuring treatment credibility and outcome expectancies. The Behavior Therapist. 1990;13:213–214. 222. [Google Scholar]
- Howard WA, Murphy SM, Clarke JC. The nature and treatment of fear of flying: A controlled investigation. Behavior Therapy. 1983;14:557–567. [Google Scholar]
- Lambert MJ, Archer A, Goodheart CD, Kazdin AE, Sternberg RJ. Research findings on the effects of psychotherapy and their implications for practice. Washington, DC: American Psychological Association; 2006. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2. Thousand Oaks: Sage Publications; 2002. [Google Scholar]
- Rothbaum BO, Hodges LF, Smith S. Virtual reality exposure therapy abbreviated treatment manual: Fear of flying application. Cognitive and Behavioral Practice. 1999;6:234–244. [Google Scholar]
- Rothbaum BO, Anderson P, Zimand E, Hodges L, Lang D, Wilson J. Virtual reality exposure therapy and in vivo exposure therapy equally effective in the treatment of fear of flying. Behavior Therapy. 2006;37:80–90. doi: 10.1016/j.beth.2005.04.004. [DOI] [PubMed] [Google Scholar]
- Safren SA, Heimberg RG, Juster HR. Clients’ expectancies and their relationship to pretreatment symptomatology and outcome of cognitive-behavioral group treatment for social phobia. Journal of Consulting and Clinical Psychology. 1997;65:694–698. doi: 10.1037//0022-006x.65.4.694. [DOI] [PubMed] [Google Scholar]
- Scott W. Fear of flying inventory. In: Kellar P, Hayman S, editors. Innovations of clinical practice. Vol. 7. Sarasota, FL: Professional Resource Exchange; 1987. [Google Scholar]
- Shuman AL, Shapiro JP. The effects of preparing parents for child psychotherapy on accuracy of expectations and treatment attendance. Community Mental Health Journal. 2002;38:3–16. doi: 10.1023/a:1013908629870. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Vogel PA, Hansen B, Stiles TC, Gotestam KG. Treatment motivation, treatment expectancy, and helping alliance as predictors of outcome in cognitive behavioral treatment of OCD. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:247–255. doi: 10.1016/j.jbtep.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Westra HA, Dozois DJA, Marcus M. Expectancy, homework compliance, and initial change in cognitive-behavioral therapy for anxiety. Journal of Consulting and Clinical Psychology. 2007;75:363–373. doi: 10.1037/0022-006X.75.3.363. [DOI] [PubMed] [Google Scholar]