Abstract
Background
Women with breast or cervical cancer abnormalities can experience barriers to timely follow-up care, resulting in delays in cancer diagnosis. Patient navigation programs that identify and remove barriers to ensure timely receipt of care are proliferating nationally. The study used a systematic framework to describe barriers, including differences between African American and Latina women; to determine recurrence of barriers; and to examine factors associated with barriers to follow-up care.
Methods
Data originated from 250 women in the intervention arm of the Chicago Patient Navigation Research Program (PNRP). The women had abnormal cancer screening findings and navigator encounters. Women were recruited from a community health center and a publicly owned medical center. After describing proportions of African American and Latina women experiencing particular barriers, logistic regression was used to explore associations between patient characteristics, such as race/ethnicity, and type of barriers.
Results
The most frequent barriers occurred at the intrapersonal level (e.g., insurance issues and fear), while institutional-level barriers such as system problems with scheduling care were the most commonly recurring over time (29%). The majority of barriers (58%) were reported in the first navigator encounter. Latinas (81%) reported barriers more often than African American women (19%). Differences in race/ethnicity and employment status were associated with types of barriers. Compared to African American women, Latinas were more likely to report an intrapersonal level barrier. Unemployed women were more likely to report an institutional level barrier.
Conclusion
In a sample of highly vulnerable women, there is no single characteristic (e.g., uninsured) that predicts what kinds of barriers a woman is likely to have. Nevertheless, navigators appear able to easily resolve intrapersonal-level barriers, but ongoing navigation is needed to address system-level barriers. Patient navigation programs can adopt the PNRP barriers framework to assist their efforts in assuring timely follow-up care.
Introduction
African American and Latina women are more likely to be diagnosed with advanced breast cancer and to have poorer survival rates than non-Hispanic white (NHW) women.1–3 Minority women also have higher incidence and mortality rates for cervical cancer than NHW women.4 These observed mortality and survival disparities are attributed to a number of factors, including delayed follow-up to abnormal cancer screening.3,5–13 Studies have reported individual factors associated with delays, including minority ethnicity;5,11,14–19 lack of health insurance or limitations of public insurance;5,20–22 younger age;17,20,22 having less than a high school diploma;18,23,24 and lack of regular access to a healthcare provider.16 Medical-related factors associated with delay include absence of breast symptoms;15,25 less severe test findings;5,26 or previous abnormal test findings.13 Studies have also found delay-related psychosocial barriers, including fear of pain associated with follow-up exams or with fear of cancer.16,27–29 Interpersonal factors associated with delays include inadequate communication or dissatisfaction with providers on test results or procedures.27,28,30 System factors associated with delays include inconvenient appointment hours and long clinic waits;29,31 having to seek care at larger hospitals;32 first diagnostic appointment with radiology rather than a surgical consultancy;32 and variations in healthcare services/procedures from clinic to clinic.33
Increasingly, patient navigation programs have been used as a strategy to improve the timely receipt of needed healthcare services. The central focus of patient navigation programs is barrier identification and removal. In the effort to remove barriers, patient navigators connect patients to resources and support systems, assist in the healthcare provider interaction, and streamline appointments and paperwork.34 Several studies have found navigation to be efficacious in terms of improving both the timeliness of diagnostic resolution,22,35–37 and the stage at cancer diagnosis.38–40 The largest effort to date to examine the role and benefits of navigation (i.e., to assess the timeliness of diagnosis and treatment, patient satisfaction and quality of life, and cost effectiveness) is the Patient Navigation Research Program (PNRP), a 10-site study funded by the National Cancer Institute, with additional support from the American Cancer Society.41
Most studies, as discussed above, describe factors (e.g., age, race/ethnicity, sociodemographics) associated with delays in diagnosing breast or cervical cancer abnormalities. Fewer studies report on barriers experienced by women, and often these barrier reports are collected retrospectively and post-diagnosis. Patient navigation programs contain a unique feature designed to garner information on barriers experienced by women during the process of follow-up care for screening abnormalities.35,36,38,41–47 This allows navigators to identify barriers that might impede timely care in real time rather than retrospectively.
The aims of this study are to (1) describe barriers and identify differences between African American and Latina women in reported barriers, (2) determine the recurrence of barriers; and (3) examine factors associated with barriers to follow-up care. This study makes several important contributions to the literature. First, we apply a systematic framework to study barriers. Second, we report on barriers that were collected in real time. Third, we use data that were collected uniformly as part of a large federal initiative.
Materials and Methods
Setting and recruitment procedures of parent study
This study uses data from the intervention arm of a parent study, the Chicago PNRP. The parent study recruited participants for intervention and control groups from 2006 to 2010 from a Community Health Center network of clinics and a publicly owned medical center. The protocol for the Chicago PNRP was approved by the Institutional Review Boards at the University of Illinois at Chicago and Northwestern University.
Women were eligible to participate in the Chicago PNRP if they had breast or cervical cancer diagnoses without prior treatment; an abnormal breast or cervical cancer screening test; or an abnormal clinical breast exam. Women were excluded if they were pregnant, had a prior history of cancer, or had been previously navigated. From a list of qualifying patients assessed through medical records, navigators approached eligible patients in the clinics to enlist their participation. Those who agreed were enrolled in the study upon written consent. Of the 465 women who were invited to participate in the intervention, 89.1% agreed, 4.7% refused, and 6.2% failed to appear for their appointment or were missed by the navigator at the time of their appointment. Among participants, slightly over half (55%) entered the study due to a cervical cancer abnormality, while 45% entered due to a breast cancer abnormality.
Patient navigators
The Chicago PNRP navigator team consisted of two lay navigators and two clinical social workers. The African American social worker navigator managed a small caseload but served mostly in a supervisory capacity. In this managerial role this social worker oversaw two lay navigators (1 African American, 1 Latina), each of whom navigated patients at a single clinic site that served patients predominantly of one race/ethnicity matching that of the navigator. The second social worker navigator was Caucasian and worked solely in the medical center setting and almost exclusively with African American patients who had a cancer diagnosis. The navigators attended annual and biannual in-person and webinar PNRP training sessions that covered the role of navigators, cancer research, screening, culture and diversity, mapping health system resources, and more.34 Interactive role play and lecture provided all navigators a common set of tools with which to identify and remove barriers. All navigators received feedback and suggestions based on their role-play exchanges. Evaluation indicated that post-test training scores improved.34 Locally, Chicago PNRP project leaders observed the navigators' interaction with patients on a weekly basis; project leaders compared their observations on barriers with the navigators' documented barriers. Inconsistencies were discussed and reconciled with the navigator.
Study procedures and data measures of the parent study
A common survey tool and a tracking log were developed and used by the multisite investigators participating in the PNRP. The measures for the survey were developed on the basis of guidelines from the medical literature or the consensus of the steering committee.41 The navigators administered the in-person survey at the time of study enrollment. Additionally, at each navigator encounter, the navigator used a tracking log to document information related to contact with the patient. A navigator encounter was defined as face-to-face meeting; telephone communication; or written communication. Navigators used the tracking log to document and categorize patient reported barriers using a list of 20 predefined barriers.
Women were considered lost to follow-up if they did not reach diagnostic resolution. Navigators attempted to contact participants at least 10 times if lost to follow-up was documented in the medical record. Study participants were followed from the time of their abnormal screening test through diagnostic resolution or through completion of initial cancer therapy. In some cases, navigator encounters continued after diagnostic resolution as a result of relationships established between the navigator and patient.
Inclusion/exclusion criteria for secondary analysis
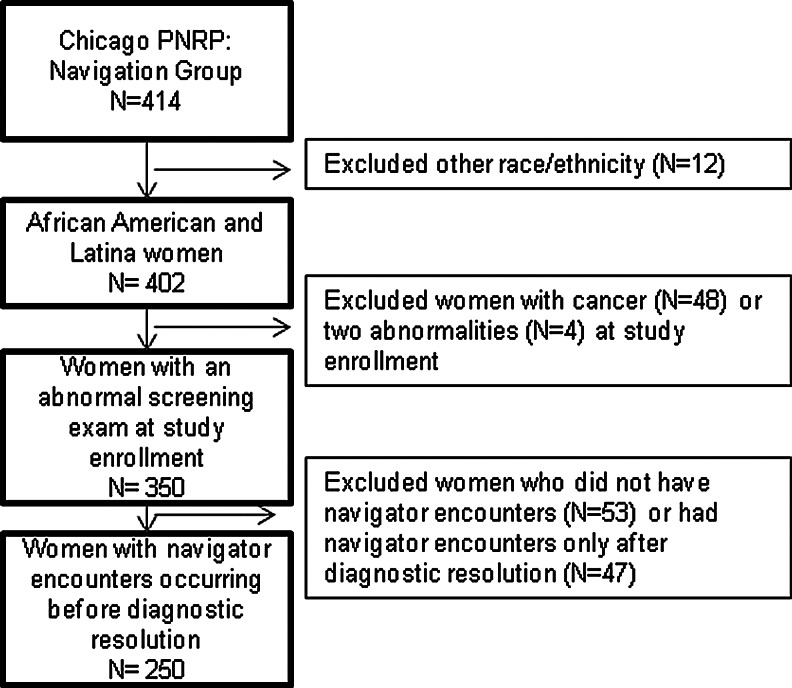
The 250 women included in this current study are from the intervention arm (i.e., assigned to receive navigation) of the Chicago PNRP; they are African American or Latina; and they had navigator encounters at any point after the abnormal screening test to before diagnostic resolution (Figure 1). Excluded from the study are white women or other ethnicity (N=12), whose small numbers rendered comparisons of these racial/ethnic categories impossible; women who had cancer at the time of study enrollment (N=48); women with both abnormal breast and cervical cancer screenings (N=4); women who had navigator encounters only after diagnostic resolution (N=47) that provided no information on the potential influence of barriers to delays in care; and women with no navigator encounters, as they did not provide information on barriers (N=53). Of the 53 women without encounters, 6 were lost to follow-up (i.e., they did not reach diagnostic resolution). Also lost to follow-up were 25 of the 250 women included in the current analysis; their inclusion is based on their navigator encounters and report of barriers, the purpose of our study.
FIG. 1.
The analytical sample for the current study includes data from 250 participants from the navigation arm of the parent study, Chicago Patient Navigation Research Program (PNRP).
Barriers framework
The National Cancer Institute PNRP group developed a framework that included 20 barriers41 with eight categories (Table 1). Drawing from the Social Ecological Theory,48,49 which divides factors into three levels of influence, we categorized the eight PNRP categories into intrapersonal, interpersonal, and institutional level barriers.
Table 1.
Barriers Framework
| Level | Category | 20 Individual barriers |
|---|---|---|
| Intrapersonal | 1. Finance | 1a. Health insurance issues |
| 1b. Financial problems | ||
| 1c. Housing | ||
| 2. Transportation | 2a. Location to healthcare facility | |
| 2b. Transportation | ||
| 2c. Out of town or country | ||
| 3. Beliefs | 3a. Fear of tests, treatment, or dying | |
| 3b. Attitudes toward provider | ||
| 3c. Perceptions/beliefs about tests or treatment | ||
| 4. Comorbidities | 4a. Medical and mental health comorbidity | |
| 4b. Patient disability | ||
| Interpersonal | 5. Family and employment issues | 5a. Employment issues |
| 5b. Childcare issues | ||
| 5c. Lack of social or practical support | ||
| 5d. Adult care | ||
| 6. Communication | 6a. Literacy | |
| 6b. Communication concerns with medical personnel | ||
| 6c. Language issues or interpreter needed | ||
| Institutional | 7. Logistical health system | 7a. System problems with scheduling care |
| Unknown | 8. Unknown | 8a. Other |
Intrapersonal-level barriers are defined as characteristics of the individual, such as knowledge, beliefs, attitudes, past experience, and skills.49 Four categories in this level are: (1) finance with barriers related to health insurance issues, financial problems, and housing; (2) transportation with barriers related to location of the healthcare facility, transportation, and being out of town or country; (3) beliefs with barriers related to issues of fear of tests, treatment, or dying, as well as attitudes toward provider (e.g., felt disrespected) and perceptions of medical tests or treatment that can affect receiving care; and (4) health-related comorbidities with barriers related to medical or mental health comorbidities and patient disability. We included transportation and finance barriers in the intrapersonal level because they affect the individual.
Interpersonal-level barriers are related to processes that involve other people, such as social support systems that may include family, friends, and peers.49 Two categories in this level are: (1) family and employment issues with barriers related to employment issues, childcare problems, lack of social or practical support, and adult care (e.g., a participant is not able to find support for other family when she needs medical care); and (2) communication with barriers related to literacy, communication concerns with medical personnel, and language or interpreter issues.
Institutional-level barriers are related to the characteristics and policies of organizations that can influence behaviors.49 One category in this level was system problems with scheduling care (e.g., long waits). The last category was termed “other” barriers, to be used when navigators could not characterize or detail the barrier. For this category we only described their occurrence using percentages.
Measures
The dependent variables for this study were from the PNRP tracking log, which included information on patient barriers. For each of the three levels—intrapersonal (finance, transportation, beliefs, and comorbidities), interpersonal (family and employment issues and communication), and institutional (logistical health system)—we created a binary category where 1 denoted having had any barrier in that category and 0 signified no barrier.
The independent variables for this study were from the PNRP survey of patient demographics. We included variables commonly associated with follow-up care for abnormal cancer screening15,16,23,24 and available in our dataset. Demographic variables included age, race/ethnicity (African American or Latina), marital status (married vs. single, divorced, or widowed), language spoken most of the time (English, Spanish, or both), birthplace (the United States, Mexico, or other), and time (years) living in the United States. Variables related to socioeconomic status included education (≤high school or >high school), income (<$10,000; $10,000–$19,999; or ≥$20,000), employment (full/part-time or no employment), insurance status (uninsured, public, or private) and having a primary care provider (yes/no). Clinic included five sites participating in the PNRP study. We created a variable, lost to follow-up, to represent those women who did not reach diagnostic resolution (yes/no).
Statistical analysis
The characteristics of African American and Latina women were compared using chi squares, Fisher's Exact, or t-tests. To examine the association of participants' characteristics with type of barriers, we used logistic regression to estimate odds ratios. Our preliminary analysis showed that the number of navigator encounters per women ranged from 0 to 18, with a median of 2 (Table 2). There were a total of 250 women and 373 barriers in the first navigator encounter and 177 women with a total of 77 barriers in the second navigator encounter. As a result, we limit our analysis to the first navigator encounter. Logistic regression models did not include variables that were highly collinear with race/ethnicity, including clinic site, language, birthplace, and years living in the United States. After conducting regression models, we noted that none of the independent variables predicted two outcomes (interpersonal and institutional). In a consecutive regression model we excluded one of two correlated variables, either income or employment, to reassess predictors for these outcomes. Analyses were conducted using Stata version 11.2 (StataCorp LP).
Table 2.
Distribution of Navigator Encounters and Patient Barriers
| Number of navigator encounters N | Total number of women N=303 N (%) | Total number of barriers N=643 N (%) |
|---|---|---|
| 0 | 53 (17.5) | 0 (0.0) |
| 1 | 250 (82.5) | 373 (58.0) |
| 2 | 177 (58.4) | 77 (12.0) |
| 3 | 117 (38.6) | 71 (11.0) |
| 4 | 83 (27.4) | 31 (4.8) |
| 5 | 62 (20.5) | 21 (3.3) |
| 6 | 45 (14.9) | 25 (3.9) |
| 7 | 36 (11.9) | 15 (2.3) |
| 8 | 30 (9.9) | 10 (1.6) |
| 9 | 20 (6.6) | 4 (0.6) |
| 10 | 16 (5.3) | 3 (0.5) |
| 11 | 9 (3.0) | 1 (0.2) |
| 12 | 7 (2.3) | 4 (0.6) |
| 13 | 7 (2.3) | 2 (0.3) |
| 14 | 6 (2.0) | 3 (0.5) |
| 15 | 4 (1.3) | 0 (0.0) |
| 16 | 3 (1.0) | 2 (0.3) |
| 17 | 3 (1.0) | 1 (0.2) |
| 18 | 1 (0.3) | 0 (0.0) |
Results
Table 2 shows that 53 women did not have any navigator encounters. We explored potential explanations for their lack of encounters (data not shown). Among 45%, the medical record showed a date for a diagnostic resolution within two weeks after study enrollment, possibly leaving little time for a navigator encounter. For 43% of women, however, it is unclear why they did not have navigator encounters as the medical record showed that the date of diagnostic resolution occurred 15 to 336 days after study enrollment. Eleven-percent of women without navigator encounters were lost to follow-up (i.e., no diagnostic resolution date was available).
Table 3 presents demographic and healthcare characteristics for women who had a navigator encounter (N=250). The mean age of women was 36. High school diploma or less was the highest degree earned for nearly three-quarters of the sample. About half reported working in a part- or full-time job. Slightly over three-quarters reported income below $20,000. Nearly two-thirds were uninsured. More than two-thirds reported having a primary care provider. African American women were recruited from four clinics, and Latina women mainly were recruited from just one clinic. Ten percent of women did not reach diagnostic resolution (i.e., they were lost to follow-up). Compared to Latinas, a higher percentage of African American women were younger; had completed more than a high school education; were covered by public insurance; were unmarried; and were lost to follow-up. Most Latinas were Mexican born (78%), had lived in the United States for a median of 13 years (range 0–40), and their primary language was Spanish (78%).
Table 3.
Participant Characteristics (N=250)
| Total N=250 N (%)a | African American N=94 N (%)a | Latina N=156 N (%)a | Comparison test χ2 | |
|---|---|---|---|---|
| Age mean, (SD) | 35.5 (11.7) | 31.5 (11.6) | 37.8 (11.1) | <0.001b |
| Education | ||||
| ≤High school | 173 (72.4) | 53 (58.9) | 120 (80.5) | <0.001 |
| >High school | 66 (27.6) | 37 (41.1) | 29 (19.5) | |
| Employed | ||||
| Yes (part/full-time) | 118 (48.0) | 43 (46.7) | 75 (48.7) | 0.770 |
| No | 128 (52.0) | 49 (53.3) | 79 (51.3) | |
| Income | ||||
| Less than $10,000 | 112 (48.3) | 50 (60.2) | 62 (41.6) | 0.080 |
| $10–$19,999 | 65 (28.0) | 15 (18.1) | 50 (33.6) | |
| ≥$20,000 | 55 (23.7) | 18 (21.7) | 37 (24.8) | |
| Insurance | ||||
| Uninsured | 156 (63.2) | 20 (20.6) | 136 (90.7) | <0.001 |
| Public | 73 (29.6) | 64 (66.0) | 9 (6.0) | |
| Private | 18 (7.2) | 13 (13.4) | 5 (3.3) | |
| Marital status | ||||
| Married | 80 (32.4) | 9 (9.6) | 71 (46.4) | <0.001 |
| Single/divorced/widowed | 167 (67.6) | 85 (90.4) | 82 (53.6) | |
| Primary care provider | ||||
| Yes | 167 (69.6) | 66 (75.0) | 101 (66.5) | 0.170 |
| No | 73 (30.4) | 22 (25.0) | 51 (33.5) | |
| Clinic site | <0.001c | |||
| 1 | 45 (18.0) | 33 (35.1) | 12 (7.7) | |
| 2 | 15 (6.0) | 15 (16.0) | 0 (0.0) | |
| 3 | 36 (14.4) | 35 (37.2) | 1 (0.6) | |
| 4 | 141 (56.4) | 1 (1.1) | 140 (89.7) | |
| 5 | 13 (5.2) | 10 (10.6) | 3 (1.9) | |
| Lost to follow-upd | ||||
| Yes | 25 (10.0) | 21 (22.4) | 4 (2.6) | <0.001c |
| No | 225 (90.0) | 73 (77.7) | 152 (97.4) | |
| Birthplace | ||||
| United States | 111 (46.3) | 90 (100.0) | 21 (14.1) | <0.001c |
| Mexico | 116 (48.3) | 0 (0.0) | 116 (77.9) | |
| Other country | 13 (5.4) | 1 (1.1) | 12 (8.0) | |
| Years living in the United States among foreign born (median, range) | 13 (1–40) | 27 | 13 (1–40) | |
| Language | ||||
| English | 113 (45.4) | 93 (98.9) | 20 (12.8) | <0.001c |
| Spanish | 122 (78.2) | 0 (0.0) | 122 (78.2) | |
| English and Spanish | 14 (5.6) | 0 (0.0) | 14 (9.0) | |
Percentages are based on nonmissing values.
P-value calculated using a t-test.
P-value calculated using a Fisher's exact test.
Women who were lost to follow-up did not reach diagnostic resolution.
Table 4 presents the number of women reporting barriers and the frequencies of specific barriers during the first two navigator encounters. Of the 250 women who experienced a first navigator encounter, 201 (80%) women reported 373 total barriers with a median of 1 among African American women and 2 reported among Latinas. Of the 177 women who experienced a second navigator encounter, 62 (35%) women reported 77 total barriers with a median of 0 in both groups.
Table 4.
Percent of Women Reporting Barriers to Follow-Up Care at the First and Second Navigator Encounter by Race/Ethnicity
| |
First navigator encounter |
Second navigator encountera |
|
||||
|---|---|---|---|---|---|---|---|
| Total women N=250N (%)c | African AmericanN=94N (%)c | LatinaN=156N (%)c | Total womenN=177N (%)c | African AmericanN=54N (%)c | LatinaN=123N (%)c | Recurring barriersbN=177N (%)c | |
| Total women reporting barriers, N(%) | 201 (80.0) | 61 (64.9) | 140 (89.7) | 62 (35.0) | 19 (35.2) | 43 (35.0) | 29 (11.6) |
| Total women reporting no barriers, N(%) | 49 (20.0) | 33 (35.1) | 16 (10.3) | 115 (65.0) | 35 (64.8) | 80 (65.0) | – |
| Barriers | |||||||
| Total barriers, N | 373 | 70 | 303 | 77 | 20 | 57 | 29 |
| Median, range | 1 (0–6) | 1 (0–4) | 2 (0–6) | 0 (0–3) | 0 (0–2) | 0 (0–3) | – |
| Intrapersonal-Level Barriers | |||||||
| Finance | |||||||
| Health insurance | 133 (53.2) | 9 (9.6) | 124 (79.5) | 12 (6. 8) | 4 (7.4) | 8 (6.5) | 10 (7.5) |
| Financial problems | 5 (2.0) | 2 (2.1) | 3 (1.9) | 0 | 0 | 0 | 0 |
| Housing barriers | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Transportation | |||||||
| Location to health care facility | 16 (6.4) | 1 (1.1) | 15 (9.6) | 4 (2.3) | 0 | 4 (3.3) | 0 |
| Transportation | 7 (2.8) | 3 (3.2) | 4 (2. 6) | 2 (1.1) | 1 (1.9) | 1 (0.8) | 0 |
| Out of town/country | 1 (0.4) | 0 | 1 (0.6) | 1 (0. 6) | 0 | 1 (0.8) | 0 |
| Beliefs | |||||||
| Fear of tests, treatment, or dying | 38 (15.2) | 4 (4.3) | 34 (21.8) | 1 (0. 6) | 0 | 1 (0.8) | 0 |
| Attitudes toward provider | 0 | 0 | 0 | 2 (1.1) | 1 (1.9) | 1 (0.8) | 0 |
| Perceptions/beliefs about test/treatment | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Comorbidities | |||||||
| Medical/mental comorbidity | 22 (8.8) | 6 (6.4) | 16 (10.3) | 5 (2.8) | 1 (1.9) | 4 (3.3) | 3 (13.6) |
| Patient disability | 4 (1.6) | 0 | 4 (2. 6) | 4 (2.3) | 2 (3.7) | 2 (1.6) | 0 |
| Interpersonal-Level Barriers | |||||||
| Family and employment Issues | |||||||
| Employment issues | 17 (6.8) | 0 | 17 (10.9) | 5 (2.8) | 1 (1.9) | 4 (3.3) | 2 (11.8) |
| Childcare issues | 4 (1.6) | 2 (2.1) | 2 (1.3) | 0 | 0 | 0 | 0 |
| Lack of social/practical support | 3 (1.2) | 1 (1.1) | 2 (1.3) | 3 (1.7) | 1 (1.9) | 2 (1.6) | 1 (33.3) |
| Adult care | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Communication | |||||||
| Literacy | 34 (13.6) | 0 | 34 (21.8) | 1 (0. 6) | 0 | 1 (0.8) | 1 (2.9) |
| Communication concerns with medical personnel | 24 (9.6) | 18 (19.2) | 6 (3.9) | 9 (5.1) | 2 (3.7) | 7 (5.7) | 1 (4.2) |
| Language/interpreter | 10 (4.0) | 1 (1.1) | 9 (5.8) | 0 | 0 | 0 | 0 |
| Institutional-Level Barriers | |||||||
| Logistical health system | |||||||
| System problems with scheduling care | 34 (13.6) | 5 (5.3) | 29 (18.6) | 27 (15.3) | 6 (11.1) | 21 (17.1) | 10 (29.4) |
| Other | 21 (8.4) | 18 (19.2) | 3 (1.9) | 1 (0. 6) | 1 (1.9) | 0 | 1 (4.8) |
Of the 250 women in the first navigator encounter, 177 of them had a second navigator.
The number of women whose barrier recurred from the first to the second navigator encounter.
Women could have reported more than one barrier during a navigator encounter; therefore, column percentages showing barriers will not add up to 100%.
The most commonly reported barriers were at the intrapersonal level (Table 4). Within the intrapersonal level, over half (53%) in the first navigator encounter experienced insurance-related barriers (e.g., un- or underinsured, high co-pays). The second most reported intrapersonal barrier (15%) in the first navigator encounter was fear-related (e.g., fear of dying or scared that test will hurt). At the interpersonal level, literacy and/or difficulty understanding written communication from the healthcare setting (14%) was the most common barrier, followed by communication concerns with medical providers (10%) and employment issues (7%). At the institutional level, issues related to system problems with scheduling care (e.g., the care provided was not efficient or convenient to the patient's needs) were reported by 14% of women. In the other category, navigators did not characterize 8% of barriers. The majority of barriers largely did not recur from the first to the second navigator encounter, except for system problems with scheduling care (29%). Furthermore, the majority of system problems recurred among Latina women.
In Table 5, the logistic regression models for each type of barrier reveal that few characteristics were significantly associated with the outcomes. In model 1, compared to African American women, Latinas were more likely to report an intrapersonal-level barrier (odds ratio [OR]: 17.39, confidence interval [CI: 7.62–39.68). No characteristics were statistically associated with interpersonal- (model 2) and institutional-level barriers. In a subsequent model (model 3) without the income variable, we found that for institutional barriers, employed women were more likely to report a barrier related to system problems with scheduling care (OR: 2.41, CI: 1.06–5.48).
Table 5.
Odds Ratios Between Types of Barriers to Follow-up Care and Participant Characteristics
| |
Model 1: Intrapersonal-level barriersa |
Model 2: Interpersonal-level barriersa |
Model 3: Institutional-level barriersa |
|||
|---|---|---|---|---|---|---|
| Characteristics | Reported barrier, Nb N=153 | OR (95% CI) | Reported barrier, Nb N=24 | OR (95% CI) | Reported barrier, Nb N=39 | OR (95% CI) |
| Age (years)c | 153 | 1.03 (1.00, 1.07) | 24 | 1.00 (0.97, 1.03) | 34 | 1.00 (0.96, 1.04) |
| Race | ||||||
| African American | 20 | ref | 3 | ref | 5 | ref |
| Latina | 133 | 17.39 (7.62, 39.68)*** | 21 | 1.67 (0.72, 3.88) | 29 | 2.06 (0.61, 7.01) |
| Education | ||||||
| ≤ High school | 113 | ref | 13 | ref | 23 | ref |
| > High school | 34 | 1.25 (0.52, 3.00) | 10 | 1.11 (0.57, 2.18) | 10 | 1.44 (0.58, 3.59) |
| Employed | ||||||
| No | 90 | ref | 6 | d | 13 | ref |
| Yes | 72 | 0.68 (0.30, 1.53) | 18 | 21 | 2.41 (1.05, 5.54)* | |
| Income | ||||||
| <$10,000 | 61 | ref | 10 | ref | 10 | e |
| $10,000–$19,999 | 50 | 1.99 (0.78, 5.03) | 10 | 1.41 (0.71, 2.82) | 15 | |
| >=$20,000 | 35 | 0.95 (0.36, 2.51) | 3 | 0.89 (0.40, 1.95) | 8 | |
| Marital status | ||||||
| Single/divorced/widow | 84 | ref | 16 | ref | 17 | ref |
| Married | 66 | 1.32 (0.53, 3.31) | 7 | 0.84 (0.43, 1.64) | 17 | 1.62 (0.7, 3.77) |
| Health insurance | ||||||
| Uninsured | 156 | d | 19 | ref | 29 | ref |
| Public | 13 | 4 | 0.76 (0.31, 1.83) | 5 | 0.68 (0.19, 2.34) | |
| Private | 3 | 1 | 1.30 (0.34, 4.95) | 0 | – | |
| Primary care Provider | ||||||
| No | 51 | ref | 4 | ref | 13 | ref |
| Yes | 99 | 0.76 (0.32, 1.77) | 19 | 21 | 0.74 (0.32,1.70) | |
| Lost to follow-up | ||||||
| No | 148 | ref | 21 | ref | 33 | ref |
| Yes | 5 | 0.13 (0.03, 0.69) | 3 | 1 | 0.40 (0.05,3.44) | |
p<.05; **p<.01; ***p<.001.
Each column represents a multivariate logistic regression model that includes independent variables listed in the first column.
Column totals within each characteristic do not add up to the total number of women reporting the barrier due to missing values.
Age included in model as a continuous variable.
Independent variable not included in regression due to its endogenous relationship with the outcome variable.
An initial model (not shown) included the income variable, resulting in no statistically significant predictors; therefore, we excluded this variable as it was correlated with employment. New estimates are presented in Model 3.
OR: Adjusted Odds Ratio, CI: Confidence Intervals.
Discussion
This study furthers the literature emerging from the field of patient navigation by reporting on barriers captured in real time by trained navigators. Arguably, the assessment of barriers reported as they are experienced (i.e., in real time) leads to increased accuracy in identifying and characterizing barriers. Accurate and specific information about barriers is necessary to prompt further action by the navigator to address the issues causing the delays to follow-up care. Timely diagnosis and treatment are essential to increase the chances of survival.
Our framework for categorizing barriers is novel and can easily be replicated by other patient navigation programs as a means of understanding the most frequent kinds of barriers, the origins of the barriers (individual level vs. institutional level), and the relationships between barriers. A focus on barrier removal has several advantages over simply offering more services. Identifying barriers allows navigators to focus on the issues that should yield more targeted and cost-effective service delivery. Also, identifying and resolving barriers is a patient-centered approach that strives for continued attachment to the medical system among patients who might otherwise become lost or falter. Another advantage to barrier removal is that resolving institutional-level barriers (i.e., system problems with scheduling care) can yield benefits for all patients receiving care in a system. The findings in our study provide information about the range of potential barriers that low-income African American and Latina women are likely to experience as they seek follow-up care. In this way our work may help inform the development of patient navigation programs tailored to the specific needs of low-income minority women.
In this study we attempted to determine whether specific personal characteristics were associated with certain kinds of barriers. We detected associations between types of barriers and race/ethnicity, as well as between types of barriers and employment status, but these relationships were not stable across the various barriers. Thus, no single characteristic (e.g., being uninsured) predicts what kinds of barriers a woman is likely to have. We attribute this result to our having a fairly homogeneous sample, which is made up of highly vulnerable women who all share enormous socioeconomic disadvantages. Recall, for instance, that we compared women with incomes below $10,000 to women with incomes between $10,000 and $20,000. Both income levels are very low. Future research should study the relationships between personal characteristics and barriers among a more heterogeneous sample.
We were interested in assessing when barriers were detected and when they were resolved. Our study showed that most of the barriers were detected in the first navigator encounter and that most of those barriers did not recur, suggesting that navigation was effective in removing barriers. The only type of barrier that recurred for significant numbers of women was institutional-level barriers, specifically those related to system problems with scheduling care. This suggests that helping patients to schedule care is an ongoing role for navigators. Navigators may be able to address intrapersonal-level barriers more efficiently, but may be less able to make permanent changes at the institutional level to completely remove system problems. Other navigation interventions have reported that system-level barriers exist,42,46,47 but our study is the first to show that these barriers persist.
In this study, Latina women reported more barriers than African American women. Specifically, Latina women experienced more intrapersonal-level barriers, including health insurance issues and fear. In previous studies, lack of insurance was reported to delay follow-up care.5,20–22 Whereas low-income African American women in this study may have access to Medicaid, immigration status may impede eligibility for Latina women. Navigators enrolled women in Stand Against Cancer, a state program that finances cancer screenings and treatment for uninsured, low-income women regardless of immigration status.
In the beliefs category, fear was the sole barrier reported by women during the follow-up care period. Compared to African American women, a large percentage of Latina women were afraid of what certain tests entailed, what the findings might be, and how they would handle any bad news. Furthermore, the differences in beliefs related to fear between African American and Latina women may be due to experiential differences with the U.S. healthcare system. Latina women, the majority of whom were born in Mexico and speak mostly Spanish, may have less experience in seeking care in multiple sites of the healthcare system. Relatively fewer studies have reported associations between beliefs and delays to follow-up care.50–53 Studies showing associations between beliefs and delays cite poor health perceptions,50 misconceptions about screening,51 and fatalism.51 Other studies have proposed that such health beliefs as degree of worry52,53 do not influence adherence to recommendations or timely follow-up care, while patient-provider communication factors52 and demographic factors53 do impact timely care.
Furthermore, we found that employed women were more likely to report institutional-level barriers, such as system problems while scheduling care. One possible explanation is the lack of flexibility afforded to low-wage workers. The vulnerable women in our study mainly reported very low incomes, and time away from work leaves some women without pay. System-related problems when scheduling care was also a recurring problem experienced mostly by Latina women. For instance, the navigator who assisted Latina patients by calling the partnering hospital to schedule follow-up appointments found few available appointment slots within 30 days, the standard set by the Stand Against Cancer program. Additionally, the non–English-speaking Latina women reported difficulty communicating their needs with front office staff when scheduling follow-up appointments. Clinic hours may not explain why Latina women experienced more system-related barriers, as all five clinics had similar operating hours during the day, evenings, and weekends. Other studies also report that women experience system issues with regard to follow-up care including inconvenient scheduling times, long clinic waits, and variations in healthcare services/procedures from clinic to clinic.27,29,31,33,46,54
We did not find that women's characteristics were associated with interpersonal-level barriers, but it is important to note that the types interpersonal barriers slightly differed by ethnicity. African American women most commonly reported communication barriers related to not understanding information given to them by medical personnel. This is a concern as studies have reported that African Americans have poorer perceptions of communication with providers and/or information55–58; limited evidence shows that these barriers may influence adherence to medical recommendations or outcomes.56,59 Latina women exhibited low literacy levels such as difficulty understanding written medical communication. Low literacy poses a concern as studies have reported delays in diagnosis60 and lack of knowledge of the benefits of early cancer detection61 with low health literacy.
This study has several limitations. Although these findings may only be generalizable to low-income African American and Latina women attending similar health centers in urban settings, some findings may apply to others such as working patients. Another limitation is that as more than half of the participants were Latina and they reported more barriers, the caseload burden was greater for the Latina lay navigator than the lay navigator who worked with the African American women. The heavier caseload may help explain why more barriers persisted beyond the first navigator encounter among Latinas. Additionally, some of our odds ratios had wide confidence intervals due to small sample sizes. Nevertheless, despite the relatively low level of statistical power, we detected statistically significant differences. This study reports on barriers experienced by women during follow-up care for breast and cervical abnormalities; we did not assess whether these reported barriers influence delays in follow-up care. Future studies should examine whether barriers mediate the relationship between personal characteristics and delays to follow-up care. Future studies should also assess how the type of cancer abnormality (breast or cervical) influences reported barriers, as this study did not present barriers by type of cancer abnormality. Furthermore, there were 25 women who were lost to follow-up (i.e., did not reach diagnostic resolution) who had at least one or more navigator encounter. Our findings showed that there were no statistically significant differences in types of barriers reported between women who did not reach diagnostic resolution and those who did. Specifically, no observable differences emerged between these two groups at the initial navigator encounter with which to increase our understanding or detection of characteristics that may increase a woman's risk for failure to reach diagnostic resolution. Finally, we excluded 53 women without navigator encounters because they did not have the opportunity to report barriers and the purpose of our study was to describe barriers. We know that only 6 of the 53 women without navigator encounters failed to reach diagnostic resolution; this suggests that the other 47 women had less need for navigator assistance.
Conclusions
Our study informs healthcare providers in the development of navigation programs tailored to low-income African American and Latina women. Recently, the National Accreditation Programs for Breast Centers (NAPBC) and the American College of Surgeons Commission on Cancer (CoC) added the requirement that healthcare organizations complete both a community-based assessment and a navigation plan to obtain full accreditation. Our study shows that close examination of barriers with a framework developed by the National Cancer Institute PNRP can increase understanding of the population being served. Community assessments should include a review of the healthcare organization's procedures involved in scheduling care for women with abnormal cancer screening exams in order to identify the numerous appointments and locations of care needed to receive follow-up care. This assessment will help identify changes needed to prevent delays related to system issues as we found scheduling issues presented a recurring hindrance to advancing in the follow-up care process.
Resources should be focused on the initial patient contact because our study shows that most barriers are likely to occur at this time. A clear understanding of the frequency and type of barriers experienced by women in real time can help healthcare providers create programs that anticipate, target, and effectively manage the health and social needs of low-income women. For example, written and verbal medical communication from medical personnel should take into consideration its audience of low socioeconomic women through the use of language and style that are best understood by low literacy and ethnically diverse patients which requires the training of a culturally competent work force.
Changes and modifications in state and national policies are mandatory to meet the medical needs of women without insurance. Some healthcare organizations provide medical services regardless of the patient's ability to afford payment; federal and state funding is needed to employ navigators whose focus on identifying and removing barriers can lead to more cost-effective service delivery.
Acknowledgments
We thank the women for their participation in this study. We also thank clinic and research staff for their time and dedication, in particular Julia Shklovskaya and Olatokunbo S Adegboro. This work was supported by NIH grants P50 CA106743-07S1, R25 CA057699, and U01 CA116875.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Lantz PM. Keeton K. Romano L. DeGroff A. Case management in public health screening programs: The experience of the National Breast and Cervical Cancer Early Detection Program. J Public Health Manag Pract. 2004;10:545–555. doi: 10.1097/00124784-200411000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Jemal A. Clegg LX. Ward E, et al. Annual report to the nation on the status of cancer, 1975–2001, with a special feature regarding survival. Cancer. 2004;101:3–27. doi: 10.1002/cncr.20288. [DOI] [PubMed] [Google Scholar]
- 3.American Cancer Society. Cancer facts and figures for African Americans 2009–2010; Atlanta: 2009. [Google Scholar]
- 4.Watson M. Saraiya M. Benard V, et al. Burden of cervical cancer in the United States, 1998–2003. Cancer. 2008;113:2855–2864. doi: 10.1002/cncr.23756. [DOI] [PubMed] [Google Scholar]
- 5.Press R. Carrasquillo O. Sciacca RR. Giardina EGV. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Women's Health. 2008;17:923–930. doi: 10.1089/jwh.2007.0402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward E. Halpern M. Schrag N, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31. doi: 10.3322/CA.2007.0011. [DOI] [PubMed] [Google Scholar]
- 7.Freedman RA. He Y. Winer EP. Keating NL. Trends in racial and age disparities in definitive local therapy of early-stage breast cancer. J Clin Oncol. 2009;27:713–719. doi: 10.1200/JCO.2008.17.9234. [DOI] [PubMed] [Google Scholar]
- 8.Carey LA. Perou CM. Livasy CA, et al. Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA. 2006;295:2492–2502. doi: 10.1001/jama.295.21.2492. [DOI] [PubMed] [Google Scholar]
- 9.Bradley CJ. Given CW. Roberts C. Race, socioeconomic status, and breast cancer treatment and survival. J Natl Cancer Inst. 2002;94:490–496. doi: 10.1093/jnci/94.7.490. [DOI] [PubMed] [Google Scholar]
- 10.Benard VB. Johnson CJ. Thompson TD, et al. Examining the association between socioeconomic status and potential human papillomavirus-associated cancers. Cancer. 2008;113:2910–2918. doi: 10.1002/cncr.23742. [DOI] [PubMed] [Google Scholar]
- 11.Benard VB. Lawson HW. Eheman CR. Anderson C. Helsel W. Adherence to guidelines for follow-up of low-grade cytologic abnormalities among medically underserved women. Obstet Gynecol. 2005;105:1323–1328. doi: 10.1097/01.AOG.0000159549.56601.75. [DOI] [PubMed] [Google Scholar]
- 12.Swan J. Breen N. Coates RJ. Rimer BK. Lee NC. Progress in cancer screening practices in the United States. Cancer. 2003;97:1528–1540. doi: 10.1002/cncr.11208. [DOI] [PubMed] [Google Scholar]
- 13.Eggleston KS. Coker AL. Das IP. Cordray ST. Luchok KJ. Understanding barriers for adherence to follow-up care for abnormal Pap tests. J Women's Health. 2007;16:311–330. doi: 10.1089/jwh.2006.0161. [DOI] [PubMed] [Google Scholar]
- 14.Abercrombie PD. Improving adherence to abnormal Pap smear follow-up. J Obstet Gynecol Neonatal Nurs. 2001;30:80–88. [PubMed] [Google Scholar]
- 15.Wujcik D. Shyr Y. Li M, et al. Delay in diagnostic testing after abnormal mammography in low-income women. Oncol Nurs Forum. 2009;36:709–715. doi: 10.1188/09.ONF.709-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones BA. Dailey A. Calvocoressi L, et al. Inadequate follow-up of abnormal screening mammograms: Findings from the race differences in screening mammography process study (United States) Cancer Causes Control. 2005;16:809–821. doi: 10.1007/s10552-005-2905-7. [DOI] [PubMed] [Google Scholar]
- 17.Fox P. Arnsberger P. Zhang X. An examination of differential follow-up rates in cervical cancer screening. J Community Health. 1997;22:199–209. doi: 10.1023/a:1025125124926. [DOI] [PubMed] [Google Scholar]
- 18.Marcus AC. Crane LA. Kaplan CP, et al. Improving adherence to screening follow-up among women with abnormal Pap smears: Results from a large clinic-based trial of three intervention strategies. Med Care. 1992;30:216–230. doi: 10.1097/00005650-199203000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Paskett ED. Phillips KC. Miller ME. Improving compliance among women with abnormal papanicolaou smears. Obstet Gynecol. 1995;86:353–359. doi: 10.1016/0029-7844(95)00176-R. [DOI] [PubMed] [Google Scholar]
- 20.Engelstad LP. Stewart SL. Nguyen BH, et al. Abnormal Pap smear follow-up in a high-risk population. Cancer Epidemiol Biomarkers Prev. 2001;10:1015–1020. [PubMed] [Google Scholar]
- 21.Clark CR. Baril N. Hall A, et al. Case management intervention in cervical cancer prevention: The Boston REACH coalition women's health demonstration project. Prog Community Health Partnersh. 2011;5:235–247. doi: 10.1353/cpr.2011.0034. [DOI] [PubMed] [Google Scholar]
- 22.Battaglia TA. Roloff K. Posner MA. Freund KM. Improving follow-up to abnormal breast cancer screening in an urban population. Cancer. 2007;109:359–367. doi: 10.1002/cncr.22354. [DOI] [PubMed] [Google Scholar]
- 23.Yabroff KR. Breen N. Vernon SW, et al. What factors are associated with diagnostic follow-up after abnormal mammograms? Findings from a U.S. National Survey. Cancer Epidemiol Biomarkers Prev. 2004;13:723–732. [PubMed] [Google Scholar]
- 24.Strzelczyk J. Dignan M. Disparities in adherence to recommended followup on screening mammography: Interaction of sociodemographic factors. Ethn Dis. 2002;12:77–86. [PubMed] [Google Scholar]
- 25.Caplan L. Helzlsouer K. Shapiro S, et al. System delay in breast cancer in whites and blacks. Am J Epidemiol. 1995;142:804–812. doi: 10.1093/oxfordjournals.aje.a117719. [DOI] [PubMed] [Google Scholar]
- 26.Melnikow J. Chan B. Stewart G. Do follow-up recommendations for abnormal Papanicolaou smears influence patient adherence? Arch Fam Med. 1999;8:510–514. doi: 10.1001/archfami.8.6.510. [DOI] [PubMed] [Google Scholar]
- 27.Percac-Lima S. Aldrich LS. Gamba GB. Bearse AM. Atlas SJ. Barriers to follow-up of an abnormal Pap smear in Latina women referred for colposcopy. J Gen Intern Med. 2010;25:1198–1204. doi: 10.1007/s11606-010-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allen J. Shelton R. Harden E. Goldman R. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: Findings from a qualitative study. Patient Educ Couns. 2008;72:283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 29.Rojas M. Mandelblatt J. Cagney K. Kerner J. Freeman H. Barriers to follow-up of abnormal screening mammograms among low-income minority women. Ethn Health. 1996;1:221–228. doi: 10.1080/13557858.1996.9961790. [DOI] [PubMed] [Google Scholar]
- 30.McKee MD. Lurio J. Marantz P. Burton W. Mulvihill M. Barriers to follow-up of abnormal Papanicolaou smears in an urban community health center. Arch Fam Med. 1999;8:129–134. doi: 10.1001/archfami.8.2.129. [DOI] [PubMed] [Google Scholar]
- 31.Hunt L. de Voogd K. Akana L. Browner C. Abnormal Pap screening among Mexican-American women: Impediments to receiving and reporting follow-up care. Oncol Nurs Forum. 1998;25:1743–1749. [PubMed] [Google Scholar]
- 32.Bastani R. Mojica CM. Berman BA. Ganz PA. Low-income women with abnormal breast findings: Results of a randomized trial to increase rates of diagnostic resolution. Cancer Epidemiol Biomarkers Prev. 2010;19:1927–1936. doi: 10.1158/1055-9965.EPI-09-0481. [DOI] [PubMed] [Google Scholar]
- 33.Battaglia TA. Santana MC. Bak S, et al. Predictors of timely follow-up after abnormal cancer screening among women seeking care at urban community health centers. Cancer. 2010;116:913–921. doi: 10.1002/cncr.24851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Calhoun EA. Whitley EM. Esparza A, et al. A national patient navigator training program. Health Promot Pract. 2010;11:205–215. doi: 10.1177/1524839908323521. [DOI] [PubMed] [Google Scholar]
- 35.Ferrante J. Chen P-H. Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: A randomized controlled trial. J Urban Health. 2007;85:114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ell K. Vourlekis B. Lee P. Xie B. Patient navigation and case management following an abnormal mammogram: A randomized clinical trial. Prev Med. 2007;44:26–33. doi: 10.1016/j.ypmed.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 37.Ell K. Padgett D. Vourlekis B, et al. Abnormal mammogram follow-up: A pilot study in women with low income. Cancer Pract. 2002;10:130–138. doi: 10.1046/j.1523-5394.2002.103009.x. [DOI] [PubMed] [Google Scholar]
- 38.Gabram SG. Lund MJ. Gardner J, et al. Effects of an outreach and internal navigation program on breast cancer diagnosis in an urban cancer center with a large African-American population. Cancer. 2008;113:602–607. doi: 10.1002/cncr.23568. [DOI] [PubMed] [Google Scholar]
- 39.Oluwole S. Impact of a cancer screening program on breast cancer stage at diagnosis in a medically underserved urban community. J Am Coll Surg. 2003;196:180–188. doi: 10.1016/S1072-7515(02)01765-9. [DOI] [PubMed] [Google Scholar]
- 40.Battaglia TA. Bak SM. Heeren T, et al. Boston Patient Navigation Research Program: The impact of navigation on time to diagnostic resolution after abnormal cancer screening. Cancer Epidemiol Biomarkers Prev. 2012;21:1645–1654. doi: 10.1158/1055-9965.EPI-12-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freund KM. Battaglia TA. Calhoun E, et al. National Cancer Institute Patient Navigation Research Program. Cancer. 2008;113:3391–3399. doi: 10.1002/cncr.23960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hendren S. Chin N. Fisher S, et al. Patients' barriers to receipt of cancer care, and factors associated with needing more assistance from a patient navigator. J Natl Med Assoc. 2011;103:701–710. doi: 10.1016/s0027-9684(15)30409-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lobb R. Allen JD. Emmons KM. Ayanian JZ. Timely care after an abnormal mammogram among low-income women in a public breast cancer screening program. Arch Intern Med. 2010;170:521–528. doi: 10.1001/archinternmed.2010.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Crump SR. Shipp MP. McCray GG, et al. Abnormal mammogram follow-up: Do community lay health advocates make a difference? Health Promot Pract. 2008;9:140–148. doi: 10.1177/1524839907312806. [DOI] [PubMed] [Google Scholar]
- 45.Miller SM. Siejak KK. Schroeder CM, et al. Enhancing adherence following abnormal Pap smears among low-income minority women: A preventive telephone counseling strategy. J Natl Cancer Inst. 1997;89:703–708. doi: 10.1093/jnci/89.10.703. [DOI] [PubMed] [Google Scholar]
- 46.McCarthy BD. Yood MU. Janz NK, et al. Evaluation of factors potentially associated with inadequate follow-up of mammographic abnormalities. Cancer. 1996;77:2070–2076. doi: 10.1002/(SICI)1097-0142(19960515)77:10<2070::AID-CNCR16>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 47.Ell K. Vourlekis B. Muderspach L, et al. Abnormal cervical screen follow-up among low-income Latinas: Project SAFe. J Womens Health Gend Based Med. 2002;11:639–651. doi: 10.1089/152460902760360586. [DOI] [PubMed] [Google Scholar]
- 48.McLeroy KR. Bibeau D. Steckler A. Glanz K. An ecological perspective on health promotion programs. Health Educ Behav. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 49.National Cancer Institute. 2nd. U.S. Department of Health and Human Services; 2005. [Nov 10;12 ]. Theory at a glance: A guide for health promotion practice. [Google Scholar]
- 50.Kerner J. Realizing the promise of breast cancer screening: Clinical follow-up after abnormal screening among black women. Prev Med. 2003;37:92–101. doi: 10.1016/s0091-7435(03)00087-2. [DOI] [PubMed] [Google Scholar]
- 51.Nelson K. Geiger AM. Mangione CM. Effect of health beliefs on delays in care for abnormal cervical cytology in a multi-ethnic population. J Gen Intern Med. 2002;17:709–716. doi: 10.1046/j.1525-1497.2002.11231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Poon E. Haas J. Puopolo A, et al. Communication factors in the follow-up of abnormal mammograms. J Gen Intern Med. 2004;19:316–323. doi: 10.1111/j.1525-1497.2004.30357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haas JS. Cook EF. Puopolo AL. Burstin HR. Brennan TA. Differences in the quality of care for women with an abnormal mammogram or breast complaint. J Gen Intern Med. 2000;15:321–328. doi: 10.1046/j.1525-1497.2000.08030.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaplan CP. Eisenberg M. Erickson PI. Crane LA. Duffey S. Barriers to breast abnormality follow-up: Minority, low-income patients' and their providers' view. Ethn Dis. 2005;15:720–726. [PubMed] [Google Scholar]
- 55.Manfredi C. Kaiser K. Matthews AK. Johnson TP. Are racial differences in patient–physician cancer communication and information explained by background, predisposing, and enabling factors? J Health Commun. 2010;15:272–292. doi: 10.1080/10810731003686598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gordon HS. Street RL. Sharf BF. Kelly PA. Souchek J. Racial differences in trust and lung cancer patients' perceptions of physician communication. J Clin Oncol. 2006;24:904–909. doi: 10.1200/JCO.2005.03.1955. [DOI] [PubMed] [Google Scholar]
- 57.Kreling B. Figueiredo MI. Sheppard VL. Mandelblatt JS. A qualitative study of factors affecting chemotherapy use in older women with breast cancer: Barriers, promoters, and implications for intervention. Psychooncology. 2006;15:1065–1076. doi: 10.1002/pon.1042. [DOI] [PubMed] [Google Scholar]
- 58.Ayanian JZ. Zaslavsky AM. Guadagnoli E, et al. Patients' perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23:6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 59.Ashton C. Haidet P. Paterniti D, et al. Racial and ethnic disparities in the use of health services. J Gen Intern Med. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wolf MS. Knight SJ. Lyons EA, et al. Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer. Urology. 2006;68:89–93. doi: 10.1016/j.urology.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 61.Davis TC. Williams MV. Marin E. Parker RM. Glass J. Health literacy and cancer communication. CA Cancer J Clin. 2002;52:134–149. doi: 10.3322/canjclin.52.3.134. [DOI] [PubMed] [Google Scholar]