Abstract
With an increasing understanding of femoroacetabular impingement (FAI) and advancement of the surgical treatment in patients with FAI, various techniques have been published. Successful outcome after arthroscopic hip surgery depends on appropriately reshaping the bony architecture to allow for improved range of motion before impingement symptoms occur, with special attention to preserve the labrum and restore its function. We present our surgical technique for the arthroscopic treatment of FAI.
Treatment of femoroacetabular impingement (FAI) has evolved significantly from open surgical dislocation to arthroscopic treatment. The goals of FAI surgery are to eliminate the pathologic contact between the femoral head and neck and the acetabular rim, to alleviate impingement symptoms, and to prevent further damage to the labrum and cartilage. Pincer impingement is caused by excess coverage of the anterosuperior acetabular rim, whereas cam impingement is caused by abnormal shape of the femoral head-neck junction. More commonly, FAI presents with combined pincer and cam lesions, which both need to be addressed for a successful outcome.1,2 Under-resection may result in continued impingement,3 whereas over-resection may result in iatrogenic instability or fracture. Equally as important as precise recontouring of bony architecture is restoring the anatomy of the labrum during an acetabuloplasty.4 Multiple studies have shown improvement in clinical outcomes with arthroscopic treatment of FAI.5-7 However, this surgery is not without significant risks and complications. Table 1 lists the pearls and pitfalls for arthroscopic FAI treatment. The purpose of this article is to detail the surgical technique for arthroscopic treatment of FAI, highlighting the method of precisely recontouring the bony architecture.
Table 1.
Pearls and Pitfalls of Arthroscopic FAI Surgery
| Pearls | Pitfalls |
|---|---|
|
|
Technique
The patient is placed supine on a hip traction table or fracture table with a large well-padded perineal post abutting the medial thigh of the operative extremity and the feet securely placed in well-padded boots. The operative extremity is placed in neutral abduction and slight flexion, with 15° of internal rotation of the foot. The hip is prepared in standard fashion with the proximal tibia included for possible semitendinosus tendon harvest in the case of labral insufficiency needing labral reconstruction. Access to the hip joint is performed as previously described by Domb et al.8 to minimize damage to the labrum and femoral head. We use the anterolateral portal and a modified anterior portal. A capsulotomy is performed with a beaver blade to connect the 2 portals, extending the capsulotomy medially and laterally as needed. A diagnostic arthroscopy is performed consisting of a circumferential examination of the entire labrum and central compartment (Video 1 at 20 seconds).
Acetabuloplasty
Before the procedure, preoperative templating is essential to successful execution in the operating room. For the rim resection, it is important to have an anteroposterior (AP) view of the pelvis that is not malrotated, with the coccyx superior to the symphyses, based on the acceptable range specific to the patient’s gender.2 The goal of surgery is to eliminate pathologic impingement. With this in mind, a correlation between imaging and intraoperative findings ultimately dictates the amount of resection. For example, the goal is not to reduce the center-edge angle unless there is a significant amount of lateral labral and chondral damage, the exception being a global pincer lesion with a negative Tönnis angle. In addition, if there is acetabular retroversion and a posterior wall sign, elimination of too much anterior rim to match the posterior rim to eliminate a crossover sign could result in instability. The templating process involves drawing the planned resection on the radiograph and extrapolating this to a clock face so that the planned amount of rim resection is performed in relation to each point on the clock face. A typical example may be resection of 2 mm at the 12-o’clock position, 4 mm at 1 o’clock, 4 mm at 2 o’clock, and 3 mm at 3 o’clock.
To begin the rim trimming, the capsule is elevated from the acetabular rim by use of electrocautery, with care to preserve the capsule on the acetabular side for later capsular closure. A 5.5-mm round burr is placed through the anterior portal, and fluoroscopy is used to delineate the precise location of bone resection9,10 (Fig 1, Video 1 at 29 seconds). To confirm the appropriate acetabular rotation, we rotate the C-arm to obtain an AP view of the operative hip that matches the preoperative AP view based on the obturator foramen and the ischial spine. If a large resection is planned such that the articular cartilage becomes redundant, a labral takedown will be performed to remove cartilage overlying the rim. If the planned resection is small, the rim trimming is performed without labral takedown. If the labrum becomes destabilized after the rim resection or had previous tearing, a labral refixation or repair is performed with suture anchors (Video 1 at 1 minute 38 seconds). A circumferential stitch is used when the labral tissue is thin or of poor quality, and a labral base fixation stitch with a small-diameter suture lasso (Arthrex, Naples, FL) is used when sufficient labral tissue is present.10 We commonly use a modified mid-anterior portal for anchor placement and use fluoroscopic guidance if needed (Fig 1C). After all necessary anchors and sutures are placed, final stability is checked with a probe. Any instruments and the arthroscope are pulled out of the central compartment, and traction is released. When viewed from the peripheral compartment, all parts of the labrum should be in contact with the femoral head, restoring labral function (Fig 1D). Although the treatment of chondral defects in FAI is beyond the scope of this article, we often perform chondroplasty whenever necessary, with the goal to preserve as much cartilage as possible, except in cases with grade IV lesions, which are treated with microfracture.
Fig 1.
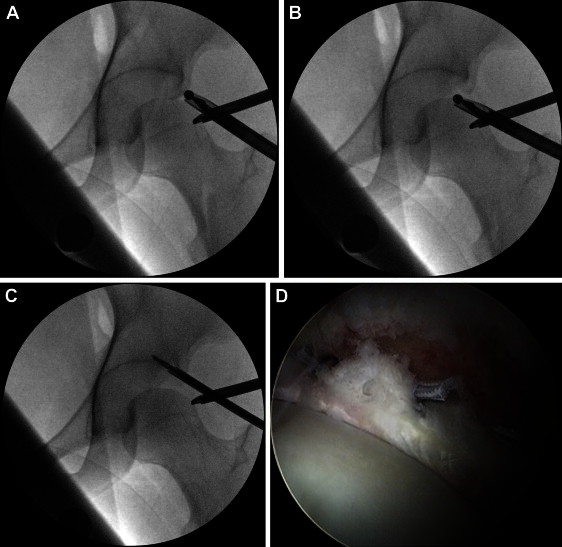
During rim trimming, the fluoroscope is used to ensure precise excision of the pincer lesion. (A) Fluoroscopic AP view of the distracted hip showing the burr on the lateral aspect of the pincer lesion. (B) Continual fluoroscopic images are taken with the burr on the edge of the acetabulum to visualize resection as it is being performed. Care is taken to ensure that no malrotation of the AP view of the pelvis occurs so as not to overestimate or underestimate the overhang. (C) Although not always necessary, fluoroscopy can be helpful to ensure accurate placement of suture anchors for labral refixation. (D) Bird’s-eye view of the acetabular rim and labrum after refixation by a labral base fixation technique. With traction released, the femoral head engages the labrum with no gapping, re-creating the suction seal.
Femoral Osteoplasty
The hip is flexed 45° and adducted to 0° as the post is removed. The C-arm is rotated 30° back to obtain a Dunn view of the proximal femur (Fig 2). If visualization is limited, the capsulotomy is extended down the femoral neck, with care taken not to extend through the zona orbicularis. Viewed from the anterolateral portal and confirmed with fluoroscopy, the proximal extent of the osteoplasty is demarcated with electrocautery. A 5.5-mm round burr is used for bony resection, working from distal to proximal, removing more bone distally than proximally to create the concave shape of the femoral neck and the convex shape of the head-neck junction (Video 1 at 2 minutes 49 seconds). Removing too much bone proximally can create a defect, which—when the hip is flexed—enters the acetabular dome and breaks the suction seal of the labrum (Fig 3). Throughout resection, care is taken to maintain high flow without stopping suction. This is important to decrease the risk of heterotopic ossification. The C-arm is brought to a straight AP view to ensure complete visualization, and the leg is then extended to address the superior neck. Care must be taken not to notch the femoral neck, specifically on the superior tension side. Frequent switching between portals can aid in visualization and orientation. When the procedure is complete, a dynamic examination should show elimination of the bony impingement. The capsule is closed with resorbable sutures for patients with any clinical signs of ligamentous laxity or radiographic indicators of instability.
Fig 2.
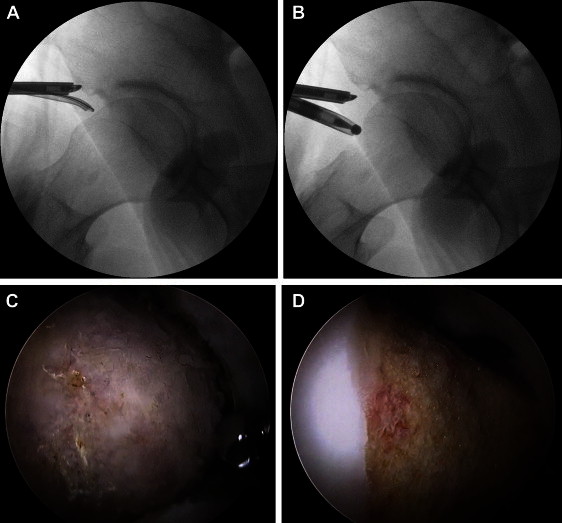
Dunn view of right hip with magnification. (A) Under fluoroscopic guidance, the proximal extent and distal extent of the cam lesion are demarcated with the electrocautery. (B) A burr is used to remove bone from distal to proximal, removing more bone distally than proximally to restore the natural concave shape of the femoral neck and the convex shape of the head-neck junction. (C) Arthroscopic image of the cam lesion after fibrocartilage is removed. (D) After cam resection, the convex curve of the head-neck junction and the concave shape of the femoral neck are obtained.
Fig 3.
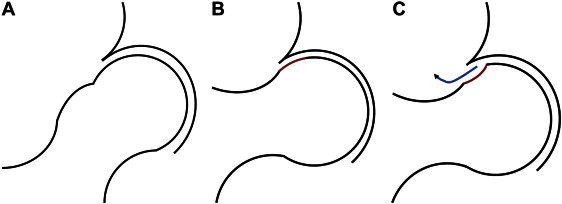
(A) With femoral osteoplasty, the goal is to create the convex shape of the femoral head-neck junction and the concave shape of the neck. (B) The head-neck convexity can appropriately engage the acetabular dome at higher flexion angles. (C) An “apple bite” creates a step-off at the head-neck junction that will break the seal with higher degrees of hip flexion, allowing joint fluid to escape.
Discussion
We have described a technique for the arthroscopic management of FAI. As with any technique, there are many subtleties and variations, and the exact technique used is at the discretion of the surgeon. Several studies have shown good clinical results after arthroscopic treatment.5-7 We believe that successful clinical outcomes are dependent on following some of the basic principles we have outlined in this article, including preoperative planning with appropriate imaging and physical examination, adequate resection but not over-resection of bony deformities, preservation of labral tissue, anatomic labral repair or refixation, minimization of iatrogenic damage to the cartilage and labrum, appropriate management of the capsule, fluoroscopic guidance during bone resection, and awareness of potential complications.
The anatomic restoration of the labrum is important to restore function to the labrum. The technique described aims to restore this relation of the labrum to the femoral head. The remodeling allows an increased physiological range of motion before impingement, preventing further impingement symptoms and chondrolabral damage. The balance between over- and under-resection of the bony architecture is important, especially when considering complications. The most devastating complications occur from over-resection, whereas one of the most common complications is caused by under-resection.1 Several cases of femoral neck fractures and hip dislocation have occurred because of overly aggressive resection.11 Careful use of the burr, fluoroscopic guidance, and preoperative planning can help decrease the risk of over-resection. Finding the balance between over and under-resection will lead to successful outcomes in patients undergoing arthroscopic decompression of FAI. This technique follows basic principles for arthroscopic femoroacetabular decompression so that surgeons can reliably reproduce good surgical outcomes.
Footnotes
The authors report the following potential conflict of interest or source of funding in relation to this article: American Hip Institute, Adventist Hinsdale Hospital, MedWest, and Arthrex, Inc.
Supplementary data
Arthroscopic treatment of FAI with acetabular and femoral osteoplasty. A step-by-step explanation of our preferred technique is shown for treatment of both cam and pincer impingement.
References
- 1.Philippon M.J., Schenker M.L., Briggs K.K. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 2.Siebenrock K.A., Kalbermatten D.F., Ganz R. Effect of pelvic tilt on acetabular retroversion: A study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. doi: 10.1097/00003086-200302000-00033. [DOI] [PubMed] [Google Scholar]
- 3.Bardakos N.V., Vasconcelos J.C., Villar R.N. Early outcome of hip arthroscopy for femoroacetabular impingement: The role of femoral osteoplasty in symptomatic improvement. J Bone Joint Surg Br. 2008;90:1570–1575. doi: 10.1302/0301-620X.90B12.21012. [DOI] [PubMed] [Google Scholar]
- 4.Larson C.M., Giveans M., Stone R.M. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: Mean 3.5-year follow-up. Am J Sports Med. 2012;40:1015–1021. doi: 10.1177/0363546511434578. [DOI] [PubMed] [Google Scholar]
- 5.Byrd J.W.T., Jones K.S. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39:7S–13S. doi: 10.1177/0363546511404144. [DOI] [PubMed] [Google Scholar]
- 6.Phillipon M.J., Briggs K.K., Yen Y.M., Kuppersmith D.A. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction. J Bone Joint Surg Am. 2009;91:16–23. doi: 10.1302/0301-620X.91B1.21329. [DOI] [PubMed] [Google Scholar]
- 7.Byrd J.W.T., Jones K.S. Arthroscopic management of femoroacetabular impingement: Minimum 2-year follow-up. Arthroscopy. 2011;27:1379–1388. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Domb B., Hanypsiak B., Botser I. Labral penetration rate in a consecutive series of 300 hip arthroscopies. Am J Sports Med. 2012;40:864–869. doi: 10.1177/0363546512437152. [DOI] [PubMed] [Google Scholar]
- 9.Larson C.M., Wulf C.A. Intraoperative fluoroscopy for evaluation of bony resection during arthroscopic management of femoroacetabular impingement in the supine position. Arthroscopy. 2009;25:1183–1192. doi: 10.1016/j.arthro.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Fry R., Domb B. Labral base refixation in the hip: Rationale and technique for an anatomic approach to labral repair. Arthroscopy. 2010;26:S81–S89. doi: 10.1016/j.arthro.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda D. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic treatment of FAI with acetabular and femoral osteoplasty. A step-by-step explanation of our preferred technique is shown for treatment of both cam and pincer impingement.


