Abstract
Femoroacetabular impingement is a recognized cause of hip pain and motion restrictions. Advancements in hip arthroscopy have allowed surgeons the ability to treat this condition more effectively. However, the learning curve is steep for osteochondroplasty of the femoral head-neck junction in the peripheral compartment. Therefore we present a reproducible technique that allows improved visualization of the peripheral compartment and treatment of the cam lesion with hip arthroscopy. Our technique uses the anterior portal as a viewing portal, a distal anterolateral accessory portal as a working portal, and the anterolateral portal for soft-tissue retraction.
Femoroacetabular impingement has recently been recognized as a source of hip pain and motion restrictions.1-3 There are multiple techniques, both open and arthroscopic, to treat this condition.4-7 In addition, femoroacetabular impingement is now widely recognized as a precursor to early osteoarthritis.3,8-11
Hip arthroscopy continues to be an evolving field of orthopaedics. Improved instrumentation and understanding of hip biomechanics have allowed orthopaedic surgeons to address hip and groin pain through minimally invasive arthroscopic techniques.12-14 However, arthroscopy of the hip joint is not an easy transition from the shoulder or the knee. The learning curve for hip arthroscopy is much steeper.15
One of the more difficult aspects of hip arthroscopy is visualization and treatment of increased femoral head-neck offset and cam lesions in the peripheral compartment.16-18 Visualization of the cam lesion and extent of resection can be difficult for an inexperienced hip arthroscopy surgeon. The purpose of this article is to detail our technique for exposure and 180° visualization of the femoral neck in the peripheral compartment (Video 1, Figs 1-5, Table 1).
Figure 1.
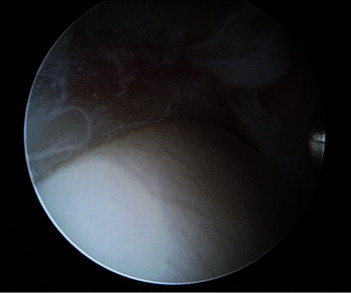
Peripheral-compartment view of anatomic labral refixation with arthroscope in anterior portal.
Figure 2.
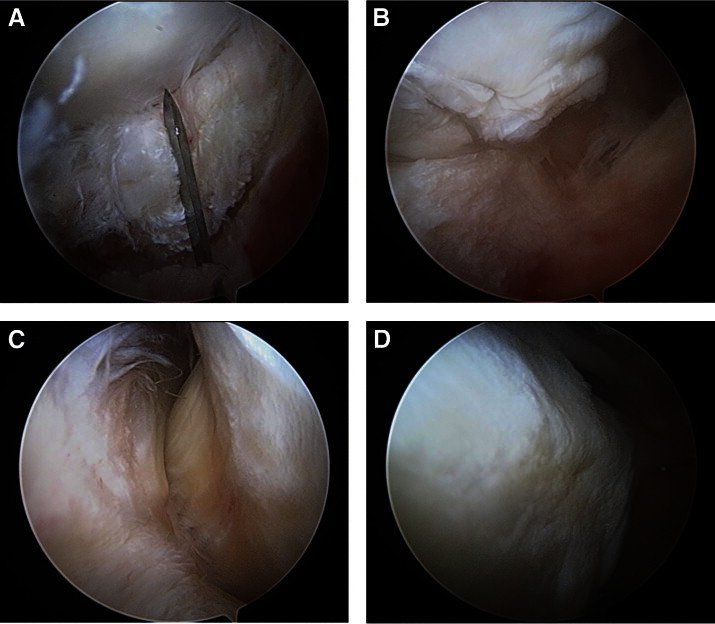
Expansile view of peripheral compartment with arthroscope in anterior portal, viewing distally and laterally. (A) Capsulotomy with arthroscopic scalpel through iliofemoral ligament between gluteus minimus and iliocapsularis muscles. (B) T capsulotomy down anterior aspect of femoral neck to intertrochanteric line. (C) View of lateral synovial folds. (D) View of medial synovial folds.
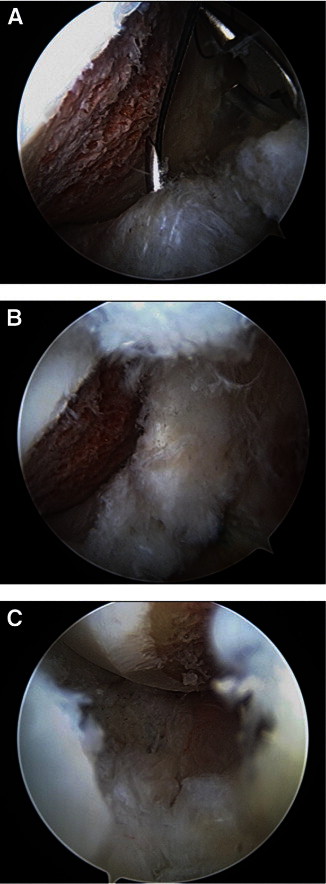
Figure 3.
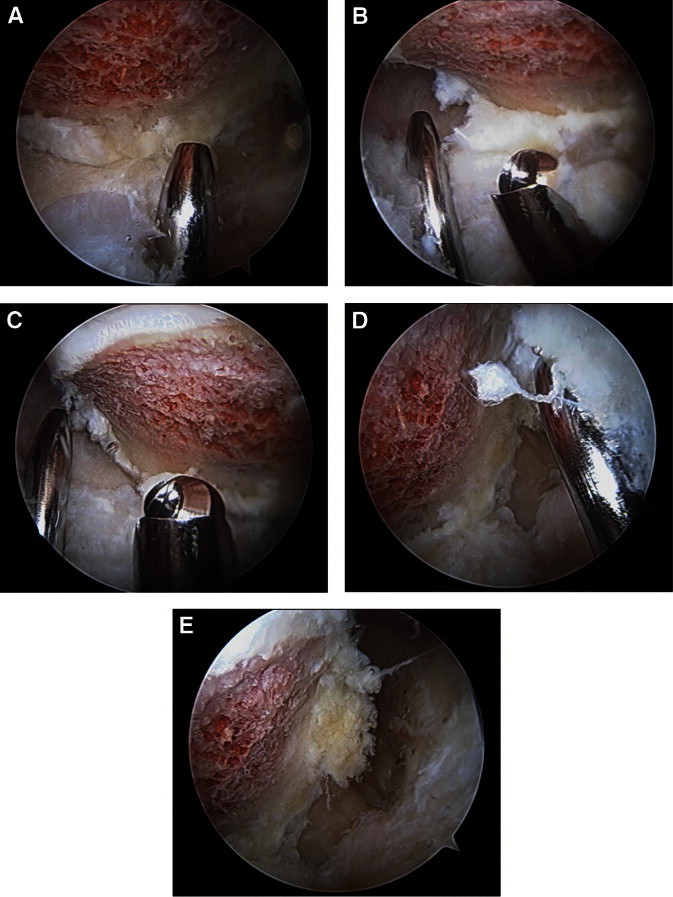
Capsular retraction. (A) Use of Wissinger rod in ALP to retract lateral leaflet of iliofemoral ligament. (B) Use of Wissinger rod to retract capsule to view anterolateral aspect of head-neck junction. (C) Arthroscopic bur positioned in DALA portal underneath Wissinger rod. (D) Retraction of medial leaflet of iliofemoral ligament with Wissinger rod to view anteromedial aspect of head-neck junction. (E) Retracted view of medial leaflet of iliofemoral ligament.
Figure 4.
Hip motion to enhance view. (A) Hip flexed at 45°. (B) Hip flexed at 60°.
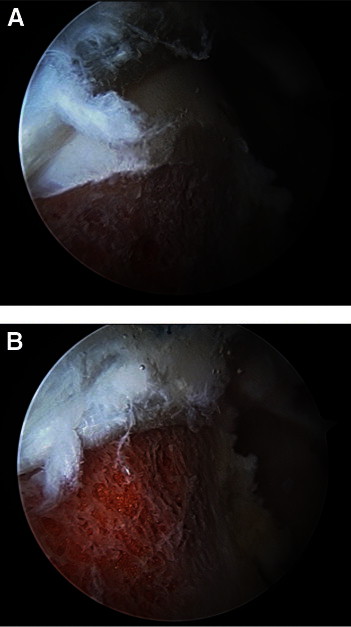
Figure 5.
Capsular closure. (A) Suture lasso through lateral leaflet of iliofemoral ligament and tissue penetrator through medial leaflet of iliofemoral ligament. (B) Closure of medial and lateral leaflets of iliofemoral ligament. (C) Closure of transverse aspect of capsulotomy, after closure of iliofemoral ligament to acetabulum.
Table 1.
Technical Pearls
| Description | |
|---|---|
| Interportal capsulotomy | Adequate visualization and mobilization in the central compartment are provided. |
| T capsulotomy | Adequate visualization to fully evaluate the proximal femur is provided. |
| Arthroscope in anterior portal | Directing the light source down the femoral neck allows at least 180° visualization of the cam lesion. |
| Retraction | A switching stick is placed through the ALP and used to retract the superior and inferior leaves of the capsule for improved exposure. |
| DALA portal | Use of the DALA portal allows ergonomic osteochondroplasty of the femoral head-neck junction. |
Technique
The patient is anesthetized and placed on a traction table with a well-padded perineal post. Traction is established by adduction and cantilever force over the perineal post. Appropriate joint distraction is confirmed with an image intensifier. Under fluoroscopic visualization, a standard anterolateral portal (ALP) is used just proximal to the greater trochanter and anterior to the iliotibial band. Needle localization is used to establish an anterior portal with an outside-in technique. The ALP is approximately 1 cm lateral to the anterior superior iliac spine and in line with the ALP. A capsulotomy is then performed connecting the 2 portals. The reflected capsule on the superior acetabular rim is released from the level of the chondrolabral junction to the anterior inferior iliac spine and indirect head of the rectus femoris insertion proximally. The central compartment is visualized, and all indicated procedures are performed.
We routinely use a peritrochanteric distal anterolateral accessory (DALA) portal for anchor placement and later for peripheral-compartment work. The arthroscope is placed in the ALP, and needle localization is used to establish the DALA portal aiming for the acetabular rim. This portal is in line with the ALP and approximately 4 to 6 cm distal (Fig 1).
The arthroscope is switched to the anterior portal. The light source is directed distally and laterally along the femoral neck. The traction is released, and the hip is flexed approximately 30° to release tension on the anterior capsule and increase peripheral-compartment volume.
An arthroscopic beaver blade is introduced through the DALA portal. We use a Pivot Samurai blade (Pivot Medical, Sunnyvale, CA). The capsule undergoes a T-shaped incision from the femoral head-neck junction to the intertrochanteric line through the zona orbicularis (Fig 2). The capsular cut should be made through the iliofemoral ligament between the gluteus minimus and iliocapsularis along the center of the femoral neck. Skiving the blade in either direction can lead to injury to the femoral vessels.
Once the capsulotomy is complete, a switching stick is introduced in the ALP. The switching stick is used as a retractor of the superior and inferior leaves of the capsule to improve visualization of the cam lesion. Fluoroscopic images taken at a 45° angle to obtain a Dunn lateral view of the hip are frequently used to assess the extent of the cam lesion and retractor placement. The arthroscopic bur is inserted through the DALA portal for cam resection in a more ergonomic position (Fig 3).
Improved exposure superiorly and inferiorly can be obtained with repositioning of the switching stick either above or below the femoral neck. Increasing the hip flexion angle to 45° allows improved access to the distal femoral neck for larger cam lesions and visualization of the entire osteochondroplasty. Rotation of the hip in conjunction with fluoroscopic images helps improve access to the anterior and posterior extents of the cam lesion. This technique provides at least 180° visualization of the cam lesion and osteochondroplasty without extensive capsulectomy (Table 1).
After the femoral head-neck osteochondroplasty is complete, a dynamic arthroscopic examination of the hip is performed. The hip is flexed from 0° to 90° and rotated internally and externally, with the surgeon ensuring that there is no impingement on the labrum, liftoff, or subluxation of the femoral head. In addition, the proximal extent of the cam resection should not violate the suction seal of the hip joint. If the patient has pain with specific positions, these are also reproduced dynamically to ensure no further evidence of impingement (Fig 4). Fluoroscopic images are used to assess anatomic recontouring of the femoral head-neck junction.
We routinely repair the capsule after the capsulotomy. This is performed with the arthroscope in the anterior portal, by use of the same visualization as for cam osteochondroplasty. A cannula is introduced in the DALA portal. A tissue penetrator is introduced through the cannula, and a suture is passed through the inferior and superior capsule leaves. The knot is tied on the outside of the capsule through the DALA portal (Fig 5). We have found that it typically takes 3 to 4 passes to adequately close the capsule to the level of the interportal capsulotomy and cover the femoral osteochondroplasty. Another device that we have used successfully is the Pivot Injector (Pivot Medical) through the DALA portal for capsule closure. The interportal capsulotomy is left open. An alternative technique for capsular closure is to use a suture lasso technique. A suture passer is used through the DALA portal. The suture can be passaged through the ALP and then tied through the DALA portal.
Discussion
Hip arthroscopy is an expanding surgical practice with advanced techniques for evaluating and treating cam lesions in the peripheral compartment. Our technique of using the anterior portal as the viewing portal and the DALA portal as the working portal allows circumferential 180° visualization of the cam lesion. This allows ergonomic resection while one is performing a dynamic examination. The technique is reproducible with a T capsulotomy and use of a Wissinger rod through the ALP for retraction.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
Technique.
References
- 1.Ito K., Minka M.A., II, Leunig M., Werlen S., Ganz R. Femoroacetabular impingement and the cam-effect: A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. doi: 10.1302/0301-620x.83b2.11092. [DOI] [PubMed] [Google Scholar]
- 2.Murphy S., Tannast M., Kim Y.J., Buly R., Millis M.B. Debridement of the adult hip for femoroacetabular impingement: Indications and preliminary clinical results. Clin Orthop Relat Res. 2004:178–181. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 3.Lavigne M., Parvizi J., Beck M., Siebenrock K.A., Ganz R., Leunig M. Anterior femoroacetabular impingement: Part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004:61–66. [PubMed] [Google Scholar]
- 4.Byrd J.W., Jones K.S. Arthroscopic management of femoroacetabular impingement: Minimum 2-year follow-up. Arthroscopy. 2011;27:1379–1388. doi: 10.1016/j.arthro.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 5.Fabricant P.D., Heyworth B.E., Kelly B.T. Hip arthroscopy improves symptoms associated with FAI in selected adolescent athletes. Clin Orthop Relat Res. 2012;470:261–269. doi: 10.1007/s11999-011-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bedi A., Zaltz I., De La Torre K., Kelly B.T. Radiographic comparison of surgical hip dislocation and hip arthroscopy for treatment of cam deformity in femoroacetabular impingement. Am J Sports Med. 2011;39(Suppl):20S–28S. doi: 10.1177/0363546511412734. [DOI] [PubMed] [Google Scholar]
- 7.Byrd J.W., Jones K.S. Arthroscopic management of femoroacetabular impingement in athletes. Am J Sports Med. 2011;39(Suppl):7S–13S. doi: 10.1177/0363546511404144. [DOI] [PubMed] [Google Scholar]
- 8.Bedi A., Dolan M., Hetsroni I. Surgical treatment of femoroacetabular impingement improves hip kinematics: A computer-assisted model. Am J Sports Med. 2011;39(Suppl):43S–49S. doi: 10.1177/0363546511414635. [DOI] [PubMed] [Google Scholar]
- 9.Larson C.M., Giveans M.R., Taylor M. Does arthroscopic FAI correction improve function with radiographic arthritis? Clin Orthop Relat Res. 2011;469:1667–1676. doi: 10.1007/s11999-010-1741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barros H.J., Camanho G.L., Bernabé A.C., Rodrigues M.B., Leme L.E. Femoral head-neck junction deformity is related to osteoarthritis of the hip. Clin Orthop Relat Res. 2010;468:1920–1925. doi: 10.1007/s11999-010-1328-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ng V.Y., Arora N., Best T.M., Pan X., Ellis T.J. Efficacy of surgery for femoroacetabular impingement: A systemic review. Am J Sports Med. 2010;38:2337–2345. doi: 10.1177/0363546510365530. [DOI] [PubMed] [Google Scholar]
- 12.Stevens M.S., Legay D.A., Glazebrook M.A., Amirault D. The evidence for hip arthroscopy: Grading the current indications. Arthroscopy. 2010;26:1370–1383. doi: 10.1016/j.arthro.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 13.McCarthy J.C., Lee J.A. Hip arthroscopy: Indications, outcomes, and complications. Instr Course Lect. 2006;55:301–308. [PubMed] [Google Scholar]
- 14.Byrd J.W., Jones K.S. Hip arthroscopy in athletes: 10-Year follow-up. Am J Sports Med. 2009;37:2140–2143. doi: 10.1177/0363546509337705. [DOI] [PubMed] [Google Scholar]
- 15.Konan S., Rhee S.J., Haddad F.S. Hip arthroscopy: Analysis of a single surgeon's learning experience. J Bone Joint Surg Am. 2011;93(Suppl 2):52–56. doi: 10.2106/JBJS.J.01587. [DOI] [PubMed] [Google Scholar]
- 16.Ejnisman L., Philippon M.J., Lertwanich P. Femoroacetabular impingement: The femoral side. Clin Sports Med. 2011;30:369–377. doi: 10.1016/j.csm.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 17.Vaughn Z.D., Safran M.R. Arthroscopic femoral osteoplasty/chielectomy for cam-type femoroacetabular impingement in the athlete. Sports Med Arthrosc. 2010;18:90–99. doi: 10.1097/JSA.0b013e3181dfce63. [DOI] [PubMed] [Google Scholar]
- 18.Matsuda D.K. The case for cam surveillance: The arthroscopic detection of cam femoroacetabular impingement missed on preoperative imaging and its significance. Arthroscopy. 2011;27:870–876. doi: 10.1016/j.arthro.2010.12.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique.


