Abstract
Extrusion of the lateral meniscus has been reported after posterior root tear or radial tear, partial meniscectomy, and meniscoplasty of discoid meniscus. It has also been shown to be associated with the development of osteoarthritis. This technical note describes a new arthroscopic technique to centralize and stabilize the mid body of the lateral meniscus to restore and maintain the lateral meniscus function by repairing/preventing extrusion of the meniscus. A JuggerKnot Soft Anchor (Biomet, Warsaw, IN), loaded with a MaxBraid suture (Biomet), was placed on the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus, through a midlateral portal. A Micro Suture Lasso Small Curve with Nitinol Wire Loop (Arthrex, Naples, FL) was used to pass 2 limbs of the MaxBraid suture through the meniscus at the margin between the meniscus and the capsule. Another anchor was inserted on the lateral edge of the lateral tibial plateau, 1 cm anterior to the first anchor, and the same procedure was repeated. The sutures were then tied by use of a self-locking sliding knot, achieving centralization and secure stabilization of the lateral meniscus.
Extrusion of the lateral meniscus has been reported in patients with posterior root tear or radial tear,1 after partial meniscectomy,2 after meniscoplasty of discoid meniscus,3 and as a complication after meniscal transplantation.4 It has also been reported that extrusion of the meniscus is associated with development of osteoarthritis (OA)5,6 and knee pain7 in patients with OA. The posterior root tear or radial tear could be surgically repaired to the normal shape; however, meniscal transplantation has been the only surgical intervention for the extrusion of the lateral meniscus after meniscectomy or in patients with OA. This technical note describes a novel arthroscopic technique, centralizing and stabilizing the mid body of the lateral meniscus onto the rim of the lateral tibial plateau to restore and maintain the lateral meniscus function by repairing/preventing extrusion of the meniscus.
Surgical Technique
Centralization of the lateral meniscus was performed in cases with knee OA at the lateral compartment or after partial meniscectomy of the lateral meniscus, where extrusion of the mid body of the lateral meniscus was confirmed preoperatively on a coronal view of the magnetic resonance imaging study (Fig 1). This technique was also applicable to cases with discoid meniscus to prevent extrusion after meniscoplasty.
Figure 1.

Preoperative magnetic resonance imaging (left knee, coronal view) showed that the mid body of the lateral meniscus (arrow) was extruded after anterior cruciate ligament reconstruction and partial meniscectomy of the lateral meniscus at another hospital. In this case, the reconstructed anterior cruciate ligament was lax, and revision anterior cruciate ligament reconstruction was also planned.
A standard arthroscopic examination was performed through routine anteromedial and anterolateral portals (Video 1). Other injuries including osteochondral lesion were managed according to the injury status. Displacement of the lateral meniscus was confirmed by pushing the mid body of the meniscus out of the rim of the lateral tibial plateau by use of a probe (Fig 2A). The rim of the lateral tibial plateau, just anterior to the popliteal hiatus, was abraded by a motorized shaver to remove cartilage.
Figure 2.
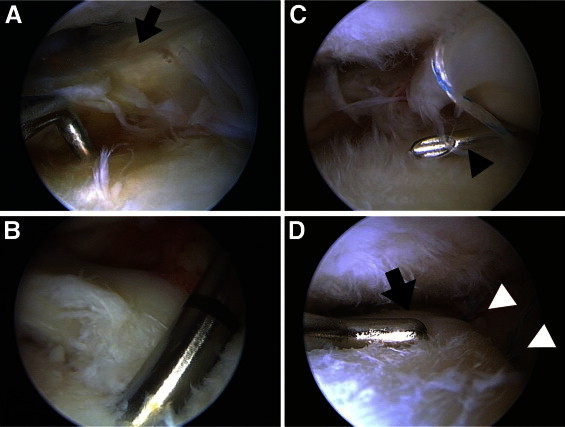
Arthroscopic findings. (A) Arthroscopic view of the lateral meniscus in a left knee from the anterolateral portal in the figure-of-4 position. Displacement of the lateral meniscus (arrow) was confirmed by pushing the mid body of the meniscus out of the rim of the lateral tibial plateau with a probe. (B) A JuggerKnot Soft Anchor was inserted on the lateral edge of the lateral tibial plateau. (C) A Micro Suture Lasso Small Curve (arrowhead) with Nitinol Wire Loop was inserted and penetrated the meniscus from superior to inferior at the margin between the meniscus and the capsule. (D) The displaced meniscus was centralized after stabilization of the mid body of the lateral meniscus (arrow) by 2 anchors (arrowheads).
A midlateral portal was made with an arthroscopic view from the anterolateral portal, just proximal to the lateral meniscus and 1 cm anterior to the popliteal hiatus, to insert a suture anchor at the appropriate angle. A JuggerKnot Soft Anchor (Biomet, Warsaw, IN), loaded with a MaxBraid suture (Biomet), was inserted on the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus (Fig 2B). Extruded lateral meniscus was easily moved away and protected by use of a cannula for the anchor. A Micro Suture Lasso Small Curve with Nitinol Wire Loop (Arthrex, Naples, FL) was then inserted through the midlateral portal. The tip of the Micro Suture Lasso penetrated the meniscus from superior to inferior at the margin between the meniscus and the capsule (Fig 2C). The wire loop was advanced sufficiently into the knee joint, and the Micro Suture Lasso was retrieved. A suture grasper was inserted through the anteromedial portal, and a wire loop and 1 strand of MaxBraid suture were retrieved. The retrieved MaxBraid suture was passed into the wire loop, and the other limb of the wire loop was pulled to pass MaxBraid suture from inferior to superior. The same procedure was repeated for another strand of MaxBraid suture to create a mattress suture configuration.
Another JuggerKnot Soft Anchor was inserted on the lateral edge of the lateral tibial plateau, 1 cm anterior to the first anchor, and the same procedure was repeated. The passed sutures were then tied through the midlateral portal by use of a self-locking sliding knot (Figs 2D and 3).
Figure 3.

Magnetic resonance image at 3 months postoperatively showed that the mid body of the lateral meniscus (arrow) was well positioned without extrusion.
After surgery, the patient underwent a routine postoperative protocol. Namely, range-of-motion exercise without restriction was encouraged immediately after surgery. Full weight bearing with a knee immobilizer was allowed for the first 4 weeks. After 4 weeks, full weight bearing without the knee immobilizer was permitted. Deep squatting was allowed after 3 months (Table 1).
Table 1.
Tips and Pearls of Procedure
| Confirm extrusion of the lateral meniscus by coronal view of MRI study preoperatively, as well as by pushing the mid body of the meniscus out of the rim of the lateral tibial plateau with a probe during surgery |
| Make midlateral portal with an arthroscopic view from the anterolateral portal, just proximal to the lateral meniscus and 1 cm anterior to the popliteal hiatus, to insert a suture anchor at the appropriate angle |
| Insert the first anchor on the lateral edge of the lateral tibial plateau, just anterior to the popliteal hiatus, and the second anchor 1 cm anterior to the first anchor |
| Use a Micro Suture Lasso Small Curve with Nitinol Wire Loop to penetrate the meniscus, and use suture relay to create a mattress suture configuration |
Abbreviation: MRI, magnetic resonance imaging.
Discussion
The menisci have important roles in distributing loads and protecting the articular cartilage during joint loading in the knee joint. The lateral meniscus seems to contribute to the load bearing more than the medial meniscus, because the lateral meniscus bears 70% of the load transmitted across the lateral compartment, whereas the load bearing across the medial compartment is shared equally between the medial meniscus and articular cartilage.8 Therefore extrusion of the lateral meniscus leads to the loss of meniscal function, diminishing the effective load-bearing mechanism, and degeneration of articular cartilage will be accelerated.
Past studies have shown that extrusion of the lateral meniscus is associated with development of OA5,6 and could often occur after posterior root tear or radial tear,1 partial meniscectomy,2 and meniscoplasty of discoid meniscus.3 Recently, surgical techniques for repair of the radial tear and posterior root tear have been developed, and good short-term results were reported.1 However, in cases with osteochondral injury or OA progression caused by extrusion of the lateral meniscus after partial meniscectomy, meniscal transplantation has been the only surgical intervention to regain meniscal function. This is also the case with discoid lateral meniscus, because extrusion of the meniscus and subsequent osteochondral injury could occur after meniscoplasty even in cases where sufficient margin of the discoid meniscus was preserved.3 Moreover, even after meniscal transplantation, extrusions of the mid body of grafted menisci have been reported, which were associated with development of OA after meniscal transplantation.4
Therefore we have developed the noble procedure to centralize and stabilize the mid body of the lateral meniscus to repair/prevent extrusion. The advantage of this technique is that the function of the lateral meniscus in distributing loads could be restored if only the mid body of the meniscus remains. Therefore it is applicable to cases with osteochondral injury or OA progression caused by extrusion of the lateral meniscus after partial meniscectomy, as well as cases with symptomatic lateral discoid meniscus where meniscoplasty is planned. On the other hand, this technique could have a risk to limit normal motion of the lateral meniscus during knee extension-flexion. Moreover, this is a preliminary report, and further follow-up will be necessary to investigate the long-term effect of meniscal centralization and clinical outcome. Nevertheless, arthroscopic centralization of the lateral meniscus can possibly repair/prevent extrusion and eventually prevent progression of OA.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary data
A case with lateral discoid meniscus in a right knee. Centralization of the lateral meniscus was performed after saucerization. Two JuggerKnot Soft Anchors, loaded with a MaxBraid suture, were inserted, and a Micro Suture Lasso Small Curve with Nitinol Wire Loop was used to penetrate the meniscus. Suture relay was used to create a mattress suture configuration. The saucerized lateral meniscus was centralized after stabilization of the mid body of the lateral meniscus.
References
- 1.Anderson L., Watts M., Shapter O. Repair of radial tears and posterior horn detachments of the lateral meniscus: Minimum 2-year follow-up. Arthroscopy. 2010;26:1625–1632. doi: 10.1016/j.arthro.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Kijowski R., Woods M.A., McGuine T.A., Wilson J.J., Graf B.K., De Smet A.A. Arthroscopic partial meniscectomy: MR imaging for prediction of outcome in middle-aged and elderly patients. Radiology. 2011;259:203–212. doi: 10.1148/radiol.11101392. [DOI] [PubMed] [Google Scholar]
- 3.Choi N.H. Radial displacement of lateral meniscus after partial meniscectomy. Arthroscopy. 2006;22:575.e1–575.e4. doi: 10.1016/j.arthro.2005.11.007. www.arthroscopyjournal.org [DOI] [PubMed] [Google Scholar]
- 4.Verdonk P.C., Verstraete K.L., Almqvist K.F. Meniscal allograft transplantation: Long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14:694–706. doi: 10.1007/s00167-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 5.Berthiaume M.J., Raynauld J.P., Martel-Pelletier J. Meniscal tear and extrusion are strongly associated with progression of symptomatic knee osteoarthritis as assessed by quantitative magnetic resonance imaging. Ann Rheum Dis. 2005;64:556–563. doi: 10.1136/ard.2004.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee D.H., Lee B.S., Kim J.M. Predictors of degenerative medial meniscus extrusion: Radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19:222–229. doi: 10.1007/s00167-010-1274-2. [DOI] [PubMed] [Google Scholar]
- 7.Wenger A., Englund M., Wirth W., Hudelmaier M., Kwoh K., Eckstein F. Relationship of 3D meniscal morphology and position with knee pain in subjects with knee osteoarthritis: A pilot study. Eur Radiol. 2012;22:211–220. doi: 10.1007/s00330-011-2234-z. [DOI] [PubMed] [Google Scholar]
- 8.Walker P.S., Erkman M.J. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A case with lateral discoid meniscus in a right knee. Centralization of the lateral meniscus was performed after saucerization. Two JuggerKnot Soft Anchors, loaded with a MaxBraid suture, were inserted, and a Micro Suture Lasso Small Curve with Nitinol Wire Loop was used to penetrate the meniscus. Suture relay was used to create a mattress suture configuration. The saucerized lateral meniscus was centralized after stabilization of the mid body of the lateral meniscus.


